Abstract
We investigated the factors influencing ambulation prognosis after hip fracture in the elderly patient and examined whether it is possible to predict the ambulation status upon hospital discharge at the time of admission. Two hundred and five patients aged 60 or older with a hip fracture who were ambulant before injury were studied. The patients were divided into two groups according to their ability to walk at the time of discharge from hospital: the ambulatory group and the non-ambulatory group. We assessed the value of various predictive factors. At discharge, 136 patients (66.3%) were ambulatory while 69 patients (33.7%) were non-ambulatory. Factors significantly affecting walking ability at discharge were: (1) age, (2) dementia, (3) residence before injury, (4) anaemia, (5) electrolyte abnormality, (6) abnormal chest X-ray, and (7) chronic systemic disease. Each patient was scored on the basis of the above factors (1=yes, 0=no), and the total was used as the predictive score. The mean score was significantly higher (p<0.0005) in the non-ambulatory group. It is possible to predict ambulation prognosis after hip fracture using our scoring system at the time of admission.
Résumé
Nous avons analysé les facteurs influençant le pronostic de la marche après fracture de la hanche chez les patients âgés en nous posant la question de la possibilité de prévoir, lors de l’admission, le statut du patient après sa sortie de l’hôpital. Ont été étudiés 205 patients âgés de 60 ans ou plus, avec une fracture de la hanche, patients « marchant » avant le traumatisme. Ces patients ont été divisés en deux groupes selon leur statut ambulatoire à la sortie de l’hôpital. Un premier groupe de patient autonome sur le plan de la marche et un deuxième groupe non-autonome. Sont sortis de l’hôpital 136 patients: 66,3% étaient autonomes sur le plan de la marche pendant que 69 patients (33,7%) n’étaient pas autonomes. Les facteurs significatifs affectant l’autonomie de la marche après la sortie de l’hôpital étaient l’âge, la démence, le statut résidentiel avant le traumatisme, l’existence ou non d’une anémie, les anomalies électrolytiques, la radio anormale du poumon et une pathologie systémique chronique. Chaque patient a été sérié selon ces facteurs (1=présence du facteur, 0=pas de présence du facteur), le total des différents facteurs donnant le score prédictif. Le score moyen était hautement significatif dans le groupe des patients non-ambulatoires. Il est donc possible de prévoir le pronostic de marche après une fracture de la hanche en utilisant ce score au moment de l’admission du patient avant le traitement de sa fracture.
Introduction
The advancing age of society is accompanied by an increase in the incidence of hip fracture, which is also recognised as a causative factor for osteoporosis [10]. Fracture of the hip in this population most commonly occurs in patients who have become bedridden and is associated with a lowered prognosis of survival. Prevention and treatment of hip fracture have therefore, become topical and many reports have described factors that affect the functional prognosis after treatment for hip fracture [1–3, 5, 7–9]. To predict the prognosis of hip fracture, including functional recovery, it is necessary to assess many preoperative factors. However, there are few reports on tools or methods for such comprehensive assessment [4, 12–14], and no standard approach has been established. We have developed a scoring system to be used as a tool for comprehensive assessment. It uses various preoperative factors, the aims of which are to predict ambulation prognosis for patients with hip fractures at hospital discharge.
Patients and methods
Two hundred fifty-nine patients who sustained hip fracture were admitted to the Kofu National Hospital between 1 January 1997 and 31 December 2003. This hospital is a self-contained regional hospital with an Orthopaedic Department and rehabilitation facility to care for patients with acute injury. However, we do not have affiliated rehabilitation facilities or long-term-care facilities. The inclusion criteria in this study were patients who were able to walk and were independent in activities of daily living (ADL) before injury and who had sustained a non-pathological femoral neck or trochanteric hip fracture. A total of 205 patients that satisfied these criteria were recruited. The study was approved by the Ethical Committee of the National Kofu Hospital.
All patients were examined at the time of admission and were followed up. Information regarding pre-injury status was obtained by interview with the patient or a family member. Data on health status and discharge status were collected from clinical charts throughout their hospital stay and at discharge. There were 156 women (76.1%) and 49 men (23.9%). Fractures included 74 of the femoral neck (36.1%) and 131 involving the trochanter (63.9%). Mean patient age was 82.7 years (60–98). One hundred and eighty-three patients (61 with femoral neck fractures and 122 with trochanteric fractures) were treated operatively. The remaining 22 patients were treated conservatively, because the patient or family declined surgery or the patient had severe dementia. An endoprosthesis was most commonly used to treat femoral neck fractures (35 cases). Compression hip screw in 109 patients was the most common fixation method for trochanteric fractures (Table 1). In this study, the discharge policy was to discharge patients when they had recovered same level of ambulation as before injury or when their walking ability had reached a plateau.
Table 1.
Treatment modality in 205 patients with hip fracture
| Treatment type | Number of patients |
|---|---|
| Operative treatment | 183 |
| Prosthesis | 35 |
| Internal fixation | |
| Compression hip screw | 109 |
| Cannulated cancellous hip screw | 15 |
| Gamma nail | 11 |
| Hannson pin | 11 |
| Ender nail | 2 |
| Non-operative treatment | 22 |
Ambulation status at discharge, was recorded. Based on this, patients were divided into two groups: those who could walk independently or walk with aids (ambulatory group) and the remaining patients, who required a wheelchair or were bedridden or who died (non-ambulatory group).
Table 2 shows the 14 factors potentially affecting ambulation prognosis that were investigated in this study. Age was categorised as 60–84 or >85 years and gender as male or female. Cognitive level was graded using the revised version of Hasegawa’s Dementia Scale (HDS-R) [6]. Patients with scores less than 20 on HDS-R were recorded as having dementia. Fracture type was categorised as femoral neck or trochanteric. Residence before injury was either the patient’s own home or a nursing home/hospital. Anaemia was classified according haemoglobin level (cutoff: 12 g/dl in men, 11 g/dl in women). Liver function was classified according to serum glutamic oxaloacetic transaminase (cutoff: 40 IU/l) and glutamic pyruvic transaminase levels (cutoff: 35 IU/l). Renal function was classified according to blood urea nitrogen level (cutoff: 20 mg/dl). Serum electrolytes analised were sodium (normal range: 135–146 mEq/l), potassium (normal range: 3.4–5.1 mEq/l), and chlorine (normal range: 99–110 mEq/l) levels. Inflammatory status was based on C-reactive protein level (cutoff level: 0.5 mg/dl). Pancreatic function status was indicated by the presence or absence of urinary glucose. Lung function was classified according to plain chest radiographic findings (presence or absence of abnormality). Cardiac function was classified according to electrocardiographic findings (no abnormal findings or abnormal findings). General health status was defined by pre-existing significant comorbidities [11], including diabetes mellitus, congestive heart failure, cardiac arrhythmias, ischemic heart disease, previous cerebrovascular accident, renal disease, cancer, Parkinson’s disease, hypertension, chronic obstructive pulmonary disease, and the need for ongoing anticoagulant therapy. These comorbidities were selected based on the most important diseases that increase mortality risk after hip fractures reported in the literature [11]. Our patients were categorised as having either 0 or ≥1 comorbidity.
Table 2.
Analysis of factors affecting functional prognosis
| 1 | Age | Older than 85 years |
| 2 | Gender | Male |
| 3 | Dementia | Present |
| 4 | Fracture type | Femoral neck fracture |
| 5 | Residence before injury | Nursing home or hospital |
| 6 | Anaemia | Hb:≤12 g/dl in men, ≤11 g/dl in women |
| 7 | Liver function | GOT ≥40 IU/l, GPT ≥35 IU/l |
| 8 | Renal function | BUN ≥20 mg/dl |
| 9 | Electrolyte abnormality | Positive |
| 10 | Inflammation status | CRP ≥0.5 mg/dl |
| 11 | Urinary glucose | Positive |
| 12 | Lung function | Abnormal chest X-ray |
| 13 | Cardiac function | Abnormal ECG (arrhythmia, ischemic changes, etc) |
| 14 | Chronic systemic diseasea | Diabetes mellitus, congestive heart failure, ischemic heart disease, etc. |
GOT glutamic oxaloacetic transaminase, GPT glutamic pyruvic transaminase, BUN blood urea nitrogen, CRP C-reactive protein, ECG electrocardiogram
aEleven comorbid conditions according to J Richmond et al. (2003)
Ambulatory and non-ambulatory groups were compared for each variable. From the results, the factors associated with ambulation prognosis were extracted. Scores were assigned to each variable, and a prognostic scoring table was constructed. The validity of the table was examined by comparing total scores of the ambulatory and non-ambulatory groups.
Statistical analysis
Statistical analysis was performed using the Statcel software (OMS-publishing, Japan). Chi-square test, Fisher’s exact probability test, Mann–Whitney U test, and Fisher’s protected least squares difference (PLSD) were used for comparisons between groups. A p value less than 0.05 was considered to indicate a significant difference.
Results
At the time of discharge from hospital, 136 patients (66.3%) were in the ambulatory group and 69 patients (33.7%) were in the non-ambulatory group. The average duration between admission and discharge was 67.2 days for all subjects and was 74.8 days for the ambulatory group. Among the 69 patients in the non-ambulatory group, 19 were bedridden and eight died during hospital stay. Among the variables examined, significant differences were observed between the two groups in seven variables. They were age, dementia, place of residence before injury, anaemia, electrolyte abnormality, pulmonary function abnormality, and chronic systemic diseases (Table 3).
Table 3.
Result of analysis of predictors affecting functional prognosis
| Ambulatory (n=136) | Non-ambulatory (n=69) | P value | |
|---|---|---|---|
| n (%) | n (%) | ||
| Age (≥85 yr) | 50 (36.8) | 39 (56.5) | <0.01 |
| Male | 33 (24.3) | 16 (23.2) | N.S. |
| Dementia | 26 (19.1) | 42 (61.0) | <0.0001 |
| Femoral neck fracture | 49 (36.0) | 25 (36.2) | N.S. |
| Nursing home or hospital | 24 (17.6) | 36 (52.2) | <0.0001 |
| Anaemia | 64 (47.1) | 49 (71.0) | <0.005 |
| Abnormal liver function | 4 (2.9) | 6 (8.7) | N.S. |
| Abnormal renal function | 56 (41.2) | 37 (53.6) | N.S. |
| Electrolyte abnormality | 21 (15.4) | 19 (27.5) | <0.05 |
| Inflammation | 93 (68.4) | 52 (75.4) | N.S. |
| Glucosuria | 16 (11.8) | 7 (10.1) | N.S. |
| Abnormal lung function | 7 (5.1) | 9 (13.0) | <0.05 |
| Abnormal ECG | 43 (31.6) | 30 (43.5) | N.S. |
| Chronic systemic diseases | 51 (37.5) | 40 (58.0) | <0.01 |
Chi-square for independence test, Fisher’s exact probability test
N.S. not significant, ECG electrocardiogram
Components of an ambulation prognosis prediction scoring system
A functional prognostic predictive scoring system was constructed by assigning scores for each of the seven prognosis-related factors (1=yes, 0=no) with a total score of 7 (Table 4). In the table, the higher the score, the more problems the patient has and the higher the possibility of diminished walking ability compared with preinjury state.
Table 4.
Functional prognosis predictive score (FPPS)
| Score 1 | Score 0 | |
|---|---|---|
| Age | ≥85 years | <85 years |
| Dementia | Yes | No |
| Nursing home/hospital | Yes | No |
| Anaemia | ||
| Men: Hb≤12 g/dl, women: Hb≤11 g/dl | Yes | No |
| Electrolyte abnormality | Yes | No |
| Abnormal chest X-ray | Yes | No |
| Chronic systemic diseasesa (diabetes, congestive heart failure, etc.) | Yes | No |
The following items were scored 0 or 1 and the total score was used as the predictive score (maximum score=7)
aEleven comorbid conditions according to J Richmond et al. (2003)
Comparisons of ambulation prognosis predictive scores between groups
Ambulatory group versus non-ambulatory group
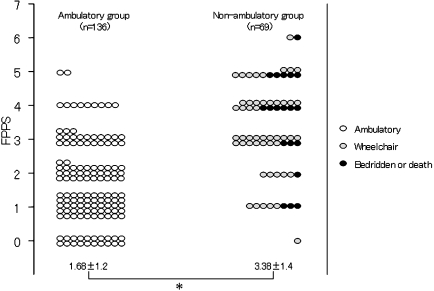
The ambulatory group (n=136) had a minimum score of 0 and a maximum of 5, with a mean score of 1.68. The non-ambulatory group (n=69) had a minimum score of 0 and a maximum of 6, with a mean score of 3.38. The non-ambulatory group had a significantly higher (p<0.0005) score than the ambulatory group (Fig. 1).
Fig. 1.
Comparison of functional prognosis predictive scores. Data are expressed as means ± SD. FPPS functional prognosis predictive score. *P<0.0005, Mann–Witney U test
Predictive score and walking ability
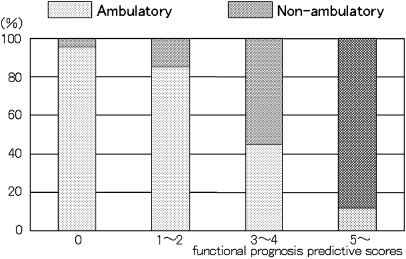
All patients were stratified into four subgroups by the predictive score: score 0, score 1−2, score 3−4, and score 5−6. The percentage of patients with walking ability was compared among four subgroups. The proportion of ambulatory patients was 95% (20 of 21 patients) in the score 0 subgroup and 85% (82 of 96 patients) in the score 1−2 subgroup compared with only 12% (2 of 17 patients) in the score 5−6 subgroup, showing a decrease in percentage of patients with walking ability as the score increases (Fig. 2). When a predictive score of 2 was chosen as the cutoff point, the sensitivity was 75% and specificity was 78.3%.
Fig. 2.
Preditive score and ambulatory status
Discussion
Various factors associated with functional outcome or walking ability after treatment for hip fracture have been proposed by various researchers. Age and preinjury walking were reported by Cheng et al. [1]; age, preinjury ambulation, American Society of Anesthesiologists score (ASA) and fracture type by Koval et al. [9]; age, preinjury ambulation, dementia and contralateral fracture by Kitamura et al. [8]; ADL, age, and mental state by Cree et al. [2]; and age, gender, preinjury residence, preinjury ambulation, dementia, neurological disease, and anemia by Ichimura et al. [5] On the other hand, Ishida et al. [7] reported that dementia was the only significant predictive factor for regaining walking ability. Furthermore, we reported in 2003 that the patient’s general condition before admission is predictive of the prognosis for walking after hip fracture. [3] To summarise the above reports, the factors that have the greatest influence on functional outcome are dementia, age, and preinjury walking ability. In this study, we identified seven preoperative factors affecting the ability to walk at the time of hospital discharge, namely: age, dementia, preinjury residence, anaemia, electrolyte abnormality, lung function abnormality, and chronic systemic diseases. However, since some patients have a good prognosis despite old age and medical conditions such as dementia and anaemia it is difficult to predict prognosis with these factors independently.
In this study, we limited our subjects to patients who were ambulant and independent in ADL before injury because patients who are not ambulant before injury are inevitably incapable of walking after injury. We consider it inappropriate to include this parameter as a predictive factor for ambulation prognosis. Based on these considerations, we examined the scores predicting ambulation prognosis after hip fracture in elderly patients who were ambulant and independent before injury. By designing a scoring system, we are able to predict with considerable accuracy the ambulation prognosis at the time of hospital discharge.
Hashmi et al. [4] and Svensson et al. [12] have reported a scoring system for predicting, before surgery, the postoperative functional prognosis. In that system, the three parameters of preinjury function in activities of daily living, absence of other medical conditions that would impair rehabilitation, and mental score were graded. The authors stated “early prediction of the outcome after hip fracture would allow better use of the resources of rehabilitation units. A patient with an excellent prognosis does not need the intensive treatment that may be very important for a patient who has an intermediate prognosis” [4, 12], emphasising the capability of their scoring system for early prediction of outcome and the usefulness of the system from the viewpoint of effective utilisation of limited rehabilitation resources. Our study differs from theirs in that we included not only surgical patients but also conservatively treated patients. Thus, the greatest characteristic of our predictive scoring system is that it can predict, even at the time of hospital admission, the ambulation prognosis of hip fracture, regardless of the treatment modality, for patients who are walking and independent in ADL before injury.
Statements
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article. This study was supported by the regular research fund of the Department of Orthopaedic Surgery, Faculty of Medicine, University of Yamanashi.
References
- 1.Cheng CL, Lau S, Hui PW, Chow SP, Pun WK, Ng J, Leong JC. Prognostic factors and progress for ambulation in elderly patients after hip fracture. Am J Phys Med Rehabil. 1989;68:230–233. doi: 10.1097/00002060-198910000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Cree AK, Nade S. How to predict return to the community after fractured proximal femur in the elderly. Aust N Z J Surg. 1999;69:723–725. doi: 10.1046/j.1440-1622.1999.01673.x. [DOI] [PubMed] [Google Scholar]
- 3.Hagino T, Harada J, Tonotsuka H, Ono T, Ishizuka K, Hamada Y. Preoperative general condition and clinical prognosis after hip fracture. J East Jpn Orthop Traumatol. 2003;15:189–193. [Google Scholar]
- 4.Hashmi MA, Tellisi N, Rigby AS, Wahab KH. The value of a prognostic scoring system in the rehabilitation of elderly patients with proximal femoral fractures. Int J Clin Pract. 2004;58:2–5. doi: 10.1111/j.1368-5031.2004.0016.x. [DOI] [PubMed] [Google Scholar]
- 5.Ichimura K, Ishii S. Walking ability after surgical treatment of hip fractures in elderly patients; the risk factor analyzed by logistic regression. Seikeigeka (Orthop Surg) 2001;52:1340–1342. [Google Scholar]
- 6.Imai Y, Hasegawa K. The revised Hasegawa’s dementia Scale (HDS-R) - Evaluation of its usefulness as a screening test for dementia. Hong Kong Coll Psychiatr. 1994;4:20–24. [Google Scholar]
- 7.Ishida Y, Tsuchida S, Murata H, Kawai S. Predictors of mortality and functional outcome of hip fractures in the elderly aged 90 years and over. Osteoporosis Jpn. 2003;11:219–223. [Google Scholar]
- 8.Kitamura S, Hasegawa Y, Suzuki S, Sasaki R, Iwata H, Wingstrand H, Thorngren KG (1998) Functional outcome after hip fracture in Japan. Clin Orthop 29–36 [PubMed]
- 9.Koval KJ, Skovron ML, Aharonoff GB, Meadows SE, Zuckerman JD (1995) Ambulatory ability after hip fracture. A prospective study in geriatric patients. Clin Orthop 150–159 [PubMed]
- 10.Orimo H, Hashimoto T, Sakata K, Yoshimura N, Suzuki T, Hosoi T. Trends in the incidence of hip fracture in Japan, 1987–1997: the third nationwide survey. J Bone Miner Metab. 2000;18:126–131. doi: 10.1007/PL00010636. [DOI] [PubMed] [Google Scholar]
- 11.Richmond J, Aharonoff GB, Zuckerman JD, Koval KJ. Mortality risk after hip fracture. J Orthop Trauma. 2003;17:53–56. doi: 10.1097/00005131-200301000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Svensson O, Stromberg L, Ohlen G, Lindgren U. Prediction of the outcome after hip fracture in elderly patients. J Bone Joint Surg Br. 1996;78:115–118. [PubMed] [Google Scholar]
- 13.Thomas M, Eastwood H. Re-evaluation of two simple prognostic scores of outcome after proximal femoral fractures. Injury. 1996;27:111–115. doi: 10.1016/0020-1383(95)00174-3. [DOI] [PubMed] [Google Scholar]
- 14.Wallace RG, Lowry JH, McLeod NW, Mollan RA. A simple grading system to guide the prognosis after hip fracture in the elderly. Br Med J (Clin Res Ed) 1986;293:665. doi: 10.1136/bmj.293.6548.665. [DOI] [PMC free article] [PubMed] [Google Scholar]