Abstract
The goal of this cadaver study was to compare the stability of anterior vertebral body screws after implantation in soft or cured kyphoplasty cement. Anterior vertebral body screws were inserted in a total of 30 thoracolumbar vertebrae of ten different human specimens: ten screws were implanted in non-augmented vertebrae (group 1), ten screws were placed in soft cement (group 2), and ten screws were placed in cured cement (group 3). The screws were then tested for biomechanical axial pullout resistance. Mean axial pullout strength was 192 N (range: 10–430 N) in group 1, 364 N (range: 65–875 N) in group 2, and 271 N (range: 35–625 N) in group 3. The paired Student’s t-test demonstrated a significant difference between pullout strength of groups 1 and 2 (p= 0.0475). No significant difference was seen between pullout strength of groups 1 and 3 (p= 0.2646) and between groups 2 and 3 (p= 0.3863). We achieved a 1.9 times higher pullout strength with kyphoplasty augmentation of osteoporotic vertebrae compared with the pullout strength of non-augmented vertebrae. Implantation of anterior vertebral body screws in cured cement is a satisfactory method. With this method we found a 1.4 times higher pullout strength than non-augmented vertebrae.
Résumé
Le but de cette étude est de comparer la stabilité de vis implantées dans le corps vertébral de sujets cadavériques avec ou sans kyphoplastie par ciment. Méthode : 30 vertèbres thoraciques et lombaires sur dix sujets ont été ainsi implantées, 10 vis dans des vertèbres non traitées. Groupe 1 : 10 vis ont été placées dans du ciment mou et 10 vis (groupe 2) et 10 vis (groupe 3) dans du ciment dur. Les vis ont été évaluées sur le plan bio-mécanique et sur la résistance à l’arrachage. Résultat : la résistance à l’arrachage a été de 192 N dans le groupe 1, 1 364 N dans le groupe 2 et 271 N dans le groupe 3. Le test de Student a démontré une différence significative entre groupes 1 et 2 et les groupes 1 et 3, par contre, entre les groupes 2 et 3 il n’a pas été observé de différences significatives. Conclusion : la Kyphoplastie multiplie 1,9 fois la résistance des vertèbres ostéoportiques. Cette technique par inclusion de vis dans le corps vertébral, des vertèbres ainsi traitées est une méthode expérimentale suffisante.
Introduction
Anterior vertebral body screw systems are used commonly to rigidly stabilise the spine during fusion procedures. Rigid fixation systems place high requirements on the load-carrying capacity of the screw-bone interface. Poor bone quality decreases the integrity of this interface, increasing screw micromotion and reducing stability and possible fusion success. In severely osteoporotic bone, anterior vertebral body screw use, without supplementary instrumentation, may be precluded completely [8, 9].
Also augmentation of vertebrae with cement is used to improve the chances of successful fixation of anterior vertebral body screws in osteopoenic bone. Augmentation of vertebrae can significantly increase screw pullout strength [1].
Kyphoplasty is being used with increasing frequency to treat painful vertebral compression fractures [4, 7]. This treatment offers the advantage of realigning the spinal column and restoring height of the fractured vertebra. It involves injecting cement into the compressed vertebral body to stabilise the fracture mechanically [5]. In our study the combination of kyphoplasty and screw implantation was used to stabilise unstable osteoporotic fractures for which isolated treatment with instrumentation or kyphoplasty was not sufficient.
It might be necessary to insert anterior vertebral body screws in augmented vertebrae in cases of unstable vertebrae. In this context stability of anterior vertebral body screws, inserted after kyphoplasty in cured cement, was not examined.
The purpose of this cadaveric study was to compare the axial anterior vertebral body screw pullout strength after kyphoplasty in soft and cured cement with that of screw implantation in vertebrae without cement augmentation.
Methods
Specimens
Ten formalin-fixed human cadaveric spines were obtained from the University of Regensburg Department of Anatomy. All specimens were examined for a history of disease. The spines were evaluated radiographically for tumours and metabolic or structural disease that would compromise bone integrity. Specimens were then assessed for osteopoenia by using quantitative computed tomography (CT) scanning. Spines were freed of all soft tissue and the pedicles were exposed unilaterally.
Of all ten spine specimens, five were randomly instrumented in three thoracic vertebrae and the other five in three lumbar vertebrae.
Bone mineral density
Measurement of bone mineral density (BMD) was performed using quantitative CT (Somatom Sensation 16, Siemens). A 10-mm thick transverse slice was scanned in the midline of vertebral bodies T11 for testings of the thoracic and L3 for testings of the lumbar spine.
Group 1
Ten anterior vertebral body screws were inserted by an experienced spine surgeon in one vertebral body of each specimen using a common technique. The screws were inserted parallel to the coronal plane in the middle of the vertebral body through one cortex and midway between the end plates under fluoroscopic control without cement augmentation.
Group 2
Ten anterior vertebral body screws were inserted after kyphoplasty whilst the cement was still soft in ten vertebrae of different specimens.
Group 3
Group 3 consisted of ten vertebrae of different specimens. After kyphoplasty in each vertebra we waited 60 min at 73°F (23°C) until the cement was cured. Then a 5.0-mm diameter drill channel was created through the hardened cement and the appropriate anterior vertebral body screw was inserted.
Kyphoplasty
Vertebrae in groups 2 and 3 were treated by the kyphoplasty technique under fluoroscopic guidance. For kyphoplasty treatment and anterior screw implantation we used the same lateral approach. A drill channel was created for placement of the inflatable tamp (Kyphon, Inc.) by passing a 5.0-mm diameter bit (Kyphon, Inc.) parallel to the coronal plane in the middle of each vertebral body. The tamp was centered in each drill channel between the anterior and posterior walls of the vertebral bodies and then inflated with 3 ml radiopaque contrast medium. Realigning the spinal column and regaining height of the vertebra was not required in our study as there where no fractures. The maximum pressure was recorded for each increment of contrast volume using the gauge on the inflation device. Inflation endpoints were cortical contact, maximum inflation volume (4.0 ml per tamp), or maximum inflation pressure (220 psi) without pressure decay. Cortical contact was the limiting point because additional inflation might have induced cortical fracture. The volume and pressure limits were based on the manufacturer’s recommendations for safe use of the balloons. The tamps were deflated and removed. An 11-gauge spinal needle was then inserted into the vertebral body through the hole, and its position was verified with radiographs. Bone substitute [polymethylmethacrylate (PMMA) cement Vertebroplastic, DePuy] was rapidly mixed until consolidation and was then injected under manual pressure through the needle.
Implantation of the screws
The screws were inserted through one cortex in the pre-existing 5.0-mm diameter drill channel having used an awl to extend the channel in the cement. The screws were inserted parallel to the coronal plane in the middle of the vertebral body and midway between the end plates under fluoroscopic control.
The implants used were titanium monoaxial pedicle screws 5.5×40 mm in the thoracic and 7.0×60 mm in the lumbar spine, Moss Miami-System (DePuy) (Fig. 1).
Fig. 1.
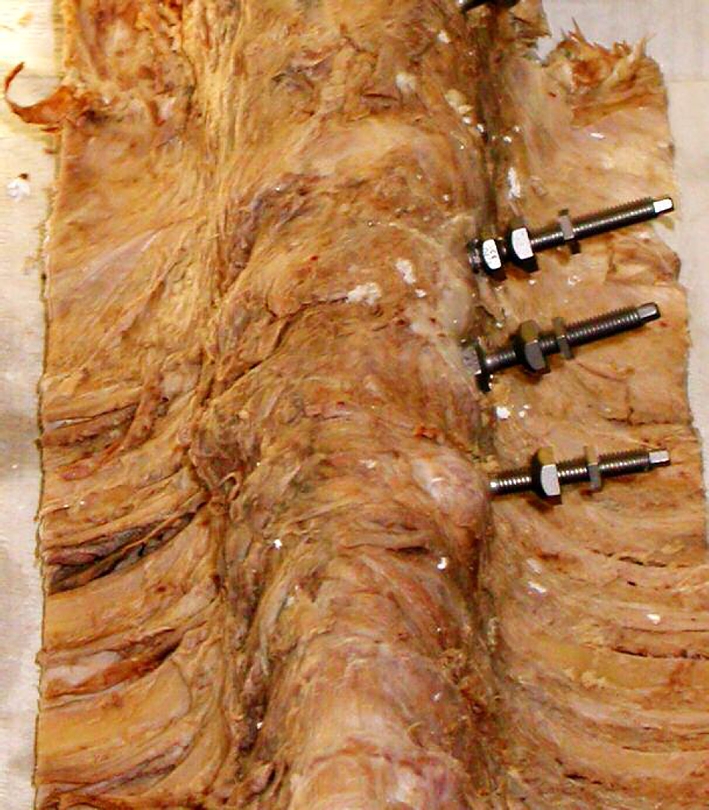
Human cadaveric spine with implanted anterior vertebral body screws T9-11. Upper screw: non-augmented vertebra; middle screw: screw implantation in soft cement; lower screw: screw implantation in cured cement
Mechanical test
Each vertebral column specimen was secured in a steel fixation device allowing a three-dimensional alignment in both the axial and the tangential plane and mounted on a material testing machine (Type 1442, Zwick Inc., Ulm, Germany). The screw heads were attached to a steel rod by using the AO Universal Fitter. A linear displacement force was applied along the long axis of the screw at a rate of 10 mm/min (Fig. 2). Load values were constantly recorded by a uniaxial load cell and arranged graphically on a printer until the force of pullout resistance peaked, declined, and the screw had been displaced.
Fig. 2.

Steel fixation device. The screw head was attached by using an AO Universal Instrument
Statistics
The maximum pullout strength of anterior vertebral body screws was analysed using Student’s t-test.
Results
Specimens
There were five male and five female vertebrae with an average age at the time of death of 77.1 (in a range from 56 to 94).
Bone mineral density
An average BMD of 56.4 mg hydroxylapatite/ml (range: 37.2–82.3 mg hydroxylapatite/ml, SD 17.2) was calculated for all specimens (Table 1).
Table 1.
BMD of each specimen: mean results with range and standard deviation
| Specimen number | BMD (mg hydroxylapatite/ml) |
|---|---|
| 1 | 38.6 |
| 2 | 66.4 |
| 3 | 62.0 |
| 4 | 69.2 |
| 5 | 82.3 |
| 6 | 39.8 |
| 7 | 51.6 |
| 8 | 39.7 |
| 9 | 37.2 |
| 10 | 77.0 |
| Mean (range) | 56.4 (37.2–82.3) |
| SD | 17.2 |
Cement application
A mean volume of 4.2 ml (thoracic spine: 4.0 ml, lumbar spine: 4.4 ml) (range: 3.0–4.9 ml) of cement was injected into each vertebra based on the maximum filling of the vertebra. In groups 2 and 3 the same volume of cement was injected.
Specimen preparation
On X-ray pictures, all screws in all groups were correctly placed without damage of the adjacent vertebral body cortex. Cement leakage was not seen.
Mechanical test
During axial pullout testing of the control group (group 1), in all cases screws stripped through the trabecular bone of the vertebral body.
Of the vertebrae with anterior vertebral body screw fixation in soft cement (group 2), the screw, cement, and surrounding trabecular bone were extracted en bloc. For statistical analysis, the force measured at the time of cortical failure was recorded as the maximum pullout force because the recorded axial forces declined after cortical failure.
Anterior vertebral body screws fixed in cured cement stripped out of the cement during pullout testing.
Results of pullout strength are summarized in Table 2. The mean axial pullout strength was 192 N (range: 10–430 N) in group 1, 364 N (range: 65–875 N) in group 2, and 271 N (range: 35–625 N) in group 3. The mean pullout strength of group 2 was 1.9 times and of group 3 1.4 times higher than group 1. Group 2 had a 1.3 times higher pullout strength than group 3. The paired Student’s t-test demonstrated a significant difference between pullout strength of groups 1 and 2 (p=0.0475). No significant difference was seen between pullout strength of groups 1 and 3 (p=0.2646) and between groups 2 and 3 (p=0.3863) (Table 2).
Table 2.
Pullout strength of all groups: mean results with range and standard deviation; Student’s paired t-test between all groups
| Specimen number | Vertebrae | Pullout strength of group 1 (N) | Pullout strength of group 2 (N) | Pullout strength of group 3 (N) |
|---|---|---|---|---|
| 1 | T9, T11, T12 | 250 | 225 | 120 |
| 2 | T11, T12, T9 | 125 | 250 | 620 |
| 3 | T8, T9, T10 | 430 | 430 | 625 |
| 4 | T12, T10, T11 | 30 | 600 | 250 |
| 5 | T10, T12, T8 | 250 | 250 | 205 |
| 6 | L1, L3, L4 | 100 | 105 | 50 |
| 7 | L2, L4, L5 | 150 | 200 | 430 |
| 8 | L3, L5, L1 | 10 | 65 | 35 |
| 9 | L4, L1, L2 | 325 | 875 | 240 |
| 10 | L5, L2, L3 | 250 | 635 | 130 |
| Mean (range) | 192 (10–430) | 364 (65–875) | 271 (35–625) | |
| SD | 133 | 263 | 217 |
Student’s paired t-test: pullout strength
Group 1 versus group 2: p=0.0475, significant
Group 1 versus group 3: p=0.2646, nonsignificant
Group 2 versus group 3: p=0.3863, nonsignificant
Discussion
In this study, we compared the pullout strength of anterior vertebral body screws implanted in non-augmented and kyphoplasty-augmented osteoporotic vertebrae.
According to the WHO definition of osteoporosis, a BMD of <80 mg hydroxylapatite/ml was considered osteoporotic [17]. Thus, the mean BMD of our specimens (56.4 mg hydroxylapatite/ml) was classified as osteoporotic. Obviously, the influence of formalin fixation on specimens explains the decreased BMD [6]. Another possible reason for osteoporotic bone structure is the age of most specimens at the time of the patients’ death.
It was known from experience that vertebral osteoporosis played a major role in pullout force. There have been several cadaveric studies in which investigators have found a correlation between anterior vertebral body screw failure and the decreased BMD osteoporosis [8, 9, 11]. This is the reason for inferior mean axial pullout strength of non-augmented and augmented specimens in our study.
The effectiveness of anterior screw-fixated instrumentation is critically dependent on the bone-screw interface [9]. Poor bone quality decreases the integrity of this interface, increasing screw micromotion and reducing stability reducing the possibility of fusion [13].
Bai et al. [1] found that pressurised injection of PMMA into the cancellous bone of the vertebral body increased the mean pullout force of anterior vertebral body screws 2.8 times compared with similar non-augmented osteoporotic vertebrae.
Our results (1.9 times increased mean pullout force) were inferior for screws implanted in soft cement and relates to the poor bone quality.
In summary, this injection method may be crucial for anterior vertebral body screw implantation in osteoporotic vertebrae or revision of failed screws.
The stability of anterior vertebral body screws implanted in cured cement after kyphoplasty have not yet been reported. In our experience, implanting anterior vertebral body screws in cured cement is a satisfactory method by which it is possible to stabilise augmented and adjacent vertebrae after kyphoplasty. With this method we achieved a 1.4 times higher pullout strength than non-augmented vertebrae. A reason for this is the more stable cement-screw interface of augmented vertebrae. In contrast to augmented vertebrae with soft cement, 0.3 times less stability without significant difference was seen. This may be explained by the less stable cement-screw interface in cases of pedicle screw implantation in cured cement.
Cured cement in living vertebrae is exposed to physiological effects for some time and, therefore, not comparable to recently cured cement in cadaveric specimens. This could explain lower stability of augmented pedicle screws in vivo [10].
There is a correlation between volume of cement injected and the augmentation effect [12]. In our study the same volume of cement was injected in groups 2 and 3. Therefore, the volume of cement had no influence on pullout strength in either groups.
In two previous studies [3, 15] the average injection volume of PMMA in the thoracolumbar region was between 9.4 and 5.0 ml. In our study, injection volume averaged 4.2 ml in the thoracic and lumbar regions. Thus the smaller cement volumes used in the current study may explain the reduced pullout values compared with other studies.
According to Cohen et al. [2] vertebroplasty constitutes a relatively simple and cheap alternative with a very high rate of success. In our study we used the kyphoplasty technique because it is widely used for vertebral augmentation and associated with fewer complications and has a better potential to restore vertebral height, although more cement is used in the kyphoplasty technique improving the stability of the pedicle screws [15,16].
In our study we used PMMA cement for vertebral augmentation. Renner et al. [14] have shown calcium phosphate to be highly biocompatible and able to be fully replaced by new and healthy bone and it may be a good alternative to PMMA for the augmentation of anterior vertebral body screw fixation.
Conclusion
This study demonstrated that kyphoplasty of osteoporotic vertebrae with PMMA cement could significantly (1.9 times) increase anterior vertebral body screw pullout strength compared with the pullout strength of nonaugmented vertebrae.
Also implantation of anterior vertebral body screws in cured cement is sufficient since we achieved a 1.4 times higher pullout strength than in non-augmented vertebrae.
References
- 1.Bai Bo, Kummer J, Spivak J. Augmentation of anterior vertebral body screw fixation by an injectable, biodegradable calcium phosphate bone substitute. Spine. 2001;26(24):2679–2683. doi: 10.1097/00007632-200112150-00009. [DOI] [PubMed] [Google Scholar]
- 2.Cohen JE, Lylyk P, Ceratto R, Kaplan L, Umanskyt F, Gomori JM. Percutaneous vertebroplasty: technique and results in 192 procedures. Neurol Res. 2004;26(1):41–49. doi: 10.1179/016164104773026516. [DOI] [PubMed] [Google Scholar]
- 3.Cotten A, Boutry N, Cortet B. Percutaneous vertebroplasty: state of the art. Radiographics. 1998;18:311–323. doi: 10.1148/radiographics.18.2.9536480. [DOI] [PubMed] [Google Scholar]
- 4.Gangi A, Kastler BA, Dietemann JL. Percutaneous vertebroplasty guided by a combination of CT and fluoroscopy. Am J Neuroradiol. 1994;15:83–86. [PMC free article] [PubMed] [Google Scholar]
- 5.Garfin S, Hansen A, Reiley M. New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine. 2001;26:1511–1515. doi: 10.1097/00007632-200107150-00002. [DOI] [PubMed] [Google Scholar]
- 6.Gertzbein SD, Robbins SE. Accuracy of pedicular screw placement in vivo. Spine. 1990;15:11–14. doi: 10.1097/00007632-199001000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Jensen ME, Evans AJ, Mathis JM. Percutaneous polymethylmethacrylate vertebroplasty in the treatment of osteoporotic vertebral body compression fractures: technical aspects. Am J Neuroradiol. 1997;18:1897–1904. [PMC free article] [PubMed] [Google Scholar]
- 8.Kaneda K, Fujiya N, Satoh S. Results with Zielke instrumentation for idiopathic thoracolumbar and lumbar scoliosis. Clin Orthop. 1986;205:195–203. [PubMed] [Google Scholar]
- 9.Kostuik JP, Carl A, Ferron S. Anterior Zielke instrumentation for spinal deformity in adults. J Bone Joint Surg Am. 1989;71:898–912. [PubMed] [Google Scholar]
- 10.Kostuik JP, Errico TJ, Gleason TF. Techniques of internal fixation for degenerative conditions of the lumbar spine. Clin Orthop. 1986;203:219–231. [PubMed] [Google Scholar]
- 11.Moe JH, Purcell GA, Bradford DS. Zielke instrumentation (VDS) for the correction of spinal curvature: analysis of results in 66 patients. Clin Orthop. 1983;180:133–153. [PubMed] [Google Scholar]
- 12.Molloy S, Mathis JM, Belkoff SM. The effect of vertebral body percentage fill on mechanical behavior during percutaneous vertebroplasty. Spine. 2003;28:1549–1554. doi: 10.1097/00007632-200307150-00014. [DOI] [PubMed] [Google Scholar]
- 13.Pfeifer BA, Krag MH, Johnson C. Repair of failed transpedicular screw fixation: a biomechanical study comparing polymethylmethacrylate, milled bone, and matchstick bone reconstruction. Spine. 1994;19:350–353. doi: 10.1097/00007632-199402000-00017. [DOI] [PubMed] [Google Scholar]
- 14.Renner S, Lim T, Kim W, Katolik L, An H, Andersson G. Augmentation of pedicle screw fixation strength using an injectable calcium phosphate cement as a function of injection timing and method. Spine. 2004;29(11):212–216. doi: 10.1097/00007632-200406010-00020. [DOI] [PubMed] [Google Scholar]
- 15.Sarzier JS, Evans AJ, Cahill DW. Increased pedicle screw pullout strength with vertebroplasty augmentation in osteoporotic spines. J Neurosurg Spine. 2002;96(3):309–312. doi: 10.3171/spi.2002.96.3.0309. [DOI] [PubMed] [Google Scholar]
- 16.Tomita S, Molloy Sean M, Jasper L, Abe M, Belkoff S. Biomechanical comparison of kyphoplasty with different bone cements. Spine. 2004;29(11):1203–1207. doi: 10.1097/00007632-200406010-00009. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organisation Technical report (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis, series 843 [PubMed]


