Abstract
This study compared the accuracy of lag screw placement between extracapsular femoral fractures fixed with sliding hip screw plate systems and those fixed with cephalocondylic nails. It involved 75 retrospective radiographs of fractures fixed with either a cephalocondylic nail (32) or a sliding hip screw plate system (43). Postoperative anteroposterior and lateral radiographs of the hip were scanned using a digital X-ray scanner and measured using computer software. Measurements were conducted by two independent observers, and the radiographs were calibrated to correct for magnification. Accuracy of lag screw placement was determined by “tip apex distance,” described by Baumgaertner et al., and by the ratio method described by Parker. The mean tip apex distance was 24.0 mm in sliding hip screw plate systems and 21.1 mm in cephalocondylic nails. This was found to be statistically significant. Lag screw placement through cephalocondylic nails is more accurate and therefore has less chance of cut-out compared with sliding hip screw plate systems. There was no statistically significant difference using Parker’s ratio method because this method quantifies the direction of the screw rather than the depth of penetration.
Résumé
Le but de cette étude est de comparer les avantages de la position de la vis cervicale dans les fractures extra capsulaires du col du fémur fixées par une vis plaque ou un clou type γ. L’étude a inclus 75 radiographies rétrospectives de fractures fixées, 32 fois par clou et 43 fois par vis plaque. Les radiographies post-opératoires de la hanche ont été analysées à l’aide d’un scanner. Les mesures ont été conduites par des observateurs indépendants. Les radiographies ont été recalibrées avec le même agrandissement. La bonne position de la vis a été déterminée par la distance «extrémité de la vis Apex» décrite par Baumgaertner et la méthode décrite par Parker. La moyenne de cette distance a été de 24 mm avec la vis plaque et de 21,1 mm avec le clou centro-médullaire plaque, ceci est statistiquement significatif. La position de la vis avec un clou type γ est plus performante et a moins de chance de balayage si on la compare à une vis plaque. Il n’y a pas de différences significatives si l’on utilise la méthode et le ratio de Parker. Cette méthode permet de quantifier la direction de la vis et l’importance de la pénétration de celle-ci.
Introduction
Hip implants provide excellent fixation for fractures in the neck of the femur, but they can, in some patients, lead to unwanted outcomes. The main implant-related complications are implant failure and infection. Failure of fixation of an extracapsular fracture has been reported to have an incidence of between 5.3% and 16.8% [4]. Of these failures, cutting out of the implant within the femoral head has been shown to be the most common cause of failure. Cut-out can be defined as collapse of the neck-shaft angle into the varus, leading to extrusion of the screw from the femoral head [2].
Few studies have demonstrated the importance of implant placement in relation to cutting out of the implant within the femoral head [2, 5]. Not only is quantification of implant placement an indicator to predict future fixation failure following surgery, but it can easily be used for audit and research purposes.
Aim
Our aim was to identify any radiographic differences in the accuracy of lag screw placement between sliding hip screws and cephalocondylic nails. The null hypothesis was that there are no differences between them.
Accuracy was determined by the concept of “tip apex distance” [2] and also by the recommendations of Parker [4], who favours lag screw positioning centrally or inferiorly on the anteroposterior (AP) view and centrally on the lateral view.
Materials and methods
The study involved 75 radiographs of patients with an extracapsular fracture that was fixed with either a cephalocondylic nail or a sliding hip screw plate system. The radiographs were traced via theatre records for the previous year in our institution. Thirty-two had been treated with a cephalocondylic nail (15 intramedullary hip screws and 17 intertrochanteric subtrochanteric devices) and 43 with a sliding hip screw plate system. A total of 90 radiographs were originally identified. Fifteen radiographs were missing from the system (six nails and nine sliding hip screws) because they were unavailable for measurement.
The postoperative AP and lateral radiographs of the proximal femur/hip joint were scanned using a Vidar digital X-ray scanner (Vidar Systems Corporation, Herndon, VA, USA) and Imagika (ViewTec, Zurich, Switzerland). Calibration was possible because the diameter of the lag screw of each implant was known. The calibration facility was selected in the software, and the on-screen diameter of the lag screw was measured. The software allowed the true value of the diameter to be entered in order to calibrate a particular X-ray. Once each digital X-ray image was calibrated, any measurements on the computer were then corrected for magnification. This calibration process was performed for each view.
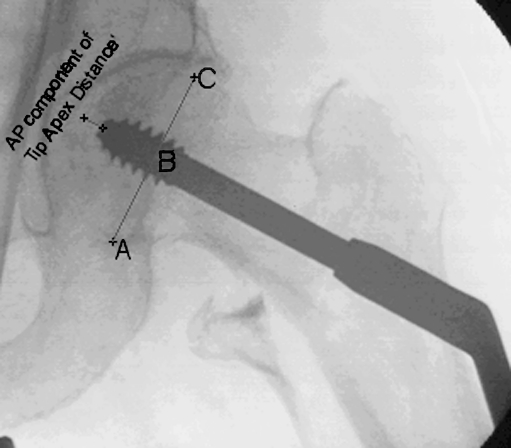
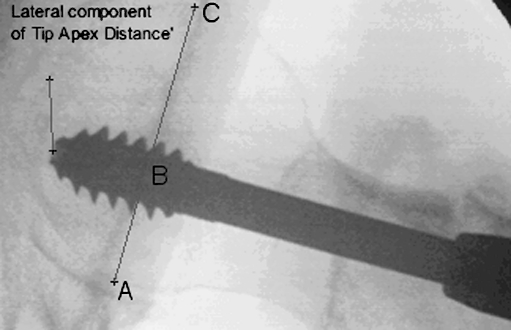
The following measurements were made on each of the postoperative AP and lateral X-ray images for each patient (see Figs. 1 and 2):
Tip of the lag screw of the implant to the apex of the femoral head in AP and lateral views
AB: Distance from the inferior/posterior border of the femoral head to the centre of the lag screw
AC: Diameter of the femoral head in the AP and lateral views
Fig. 1.
X-ray measurements conducted on anteroposterior radiographs
Fig. 2.
X-ray measurements conducted on lateral radiographs
Results
All measurements were entered into SPSS statistical software (version 12.01) to allow for further statistical analysis. The values obtained from each of two independent observers were combined to derive a mean value (Table 1). The measurements of the tip of the lag screw of the implant to the apex of the femoral head in both the AP and the lateral view allowed calculation of the tip apex distance for each fixed fracture. The accuracy of lag screw placement of each implant was also determined using Parker’s ratio method [4].
Table 1.
Measurements from X-ray analysis (standard deviation given in parentheses)
| Sliding hip screw and plate | Cephalocondylic nail | |||||
|---|---|---|---|---|---|---|
| Mean tip apex distance (mm) | Mean Parker’s ratio | Mean tip apex distance (mm) | Mean Parker’s ratio | |||
| Anteroposterior | Lateral | Anteroposterior | Lateral | |||
| Observer 1 | 26.2 (7.2) | 46.4 (9.7) | 49.3 (7.7) | 22.9 (6.3) | 49.3 (9.7) | 47.9 (8.1) |
| Observer 2 | 21.3 (6.8) | 48.1 (8.5) | 46.4 (7.0) | 19.3 (6.6) | 50.7 (8.6) | 47.8 (7.3) |
| Combined | 24.0 (6.1) | 47.3 (8.3) | 47.9 (5.9) | 21.1 (6.1) | 50.0 (8.8) | 47.9 (7.1) |
An independent t-test was conducted, demonstrating a significant difference in the tip apex distance between those extracapsular fractures fixed with a cephalocondylic nail and those fixed with a sliding hip screw plate system (p=0.047; Table 2).
Table 2.
Summary of statistical analysis
| t-test | p-value |
|---|---|
| Tip apex distance between cephalocondylic nail and sliding hip screw and plate | 0.047 |
| Anteroposterior component of tip apex distance between cephalocondylic nail and sliding hip screw and plate | 0.206 |
| Lateral component of tip apex distance between cephalocondylic nail and sliding hip screw and plate | 0.024 |
Subanalysis of the AP and lateral components of the tip apex distance showed a statistical difference in the lateral component only (p=0.024).
The results also showed that 50% of those fractures fixed with an intramedullary nail complied with the recommendation by Pervez et al. [5] (less than 20 mm), but only 25% of the sliding hip screw plate systems in this study fulfilled this criteria.
Analysis using Parker’s ratio method revealed no statistically significant difference between the groups.
The power of this study was retrospectively calculated as 82%.
Discussion
Cutting out of the lag screw from the femoral head is the most common cause of fixation failure in an extracapsular fracture of the femur neck [4]. The two main methods described to quantify lag screw placement are the tip apex distance described by Baumgaertner et al. [2] and the ratio method described by Parker [4]. Baumgaertner et al. also showed that an increase in the tip apex distance was found to be the strongest predictor of lag screw cut-out, and they recommended that the tip apex distance be less than 25 mm to reduce the risk of cut-out. A subsequent study has shown that a tip apex distance of less than 20 mm improves the results [5].
Other authors have also tried to quantify lag screw placement to establish a relationship to cut-out [3], proposing a cut-out index as a predictor of lag screw cut-out. But this was described for the Asiatic gamma nail, and the authors believe the results may not be applicable to the general population.
Previous studies have given contradictory results with regard to the cut-out rate of intramedullary devices. A meta-analysis of implant-related complications of dynamic hip screw plates versus intramedullary devices showed a decreased cut-out rate with intramedullary devices [1]. In Baumgaertner et al.'s original series, there was no statistically significant difference between the cut-out rates of the sliding screw plate system and that of intramedullary devices [2].
In this study, both methods described above for quantifying the lag screw placement in cephalocondylic nails and the sliding screw plate system were used. It showed that the cephalocondylic group achieved a better lag screw placement compared with the sliding screw and plate device and that this difference is statistically significant (p=0.047). Further analysis showed that the main reason for this difference was in the lateral component of the tip apex distance (p=0.029). An explanation for the improved accuracy of placement is that it is due to the intramedullary position achieved by the nail (when viewed from the lateral side), preventing AP translation of the guide wire entry point during insertion. AP translation is more likely to occur during the guide wire insertion for a sliding hip screw plate system because the entry site of the guide wire into the femur is determined by the surgeon (Figs. 3, 4, 5, 6, 7, 8).
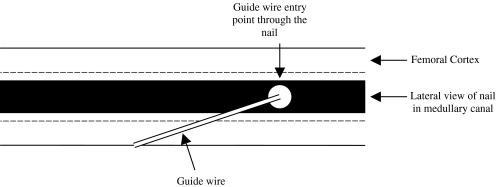
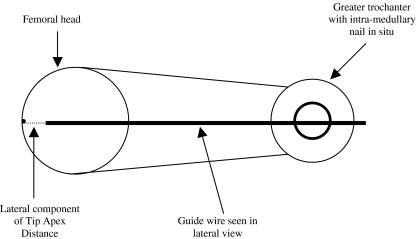
Fig. 3.
Line diagram showing lateral view of the femur during guide wire insertion through an intramedullary nail. The medullary canal prevents anteroposterior translation of the nail and guide wire
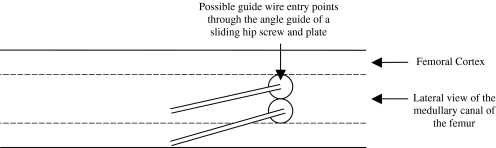
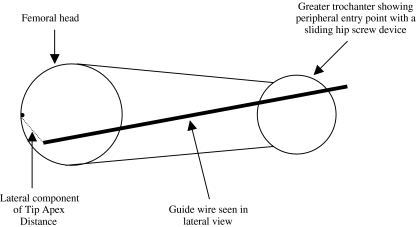
Fig. 4.
Line diagram showing lateral view of the femur during guide wire insertion during sliding hip screw and plate insertion. Anterior/posterior translation of the entry point can occur because there is no restriction of the entry point by the medullary canal, as in an intramedullary device
Fig. 5.
Line diagram of the lateral view of the femoral head and neck during guide wire insertion through an intramedullary nail
Fig. 6.
Line diagram of the lateral view of the femoral head and neck during guide wire insertion of a sliding hip screw and plate system. Note that the guide wire may follow an increased angle to the neck and hence may not achieve optimum tip apex distance
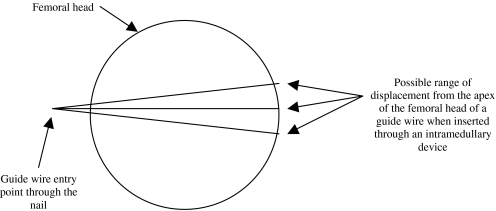
Fig. 7.
Close-up of the femoral head with the guide wire when passed through an intramedullary nail
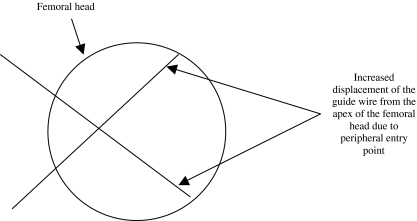
Fig. 8.
Close-up of the femoral head with the guide wire when a sliding hip screw device is inserted. Note the possibility of increased tip apex distance, which can occur because of anteroposterior translation of the entry point
No statistically significant difference between the two groups was found using Parker’s ratio method, but this method quantifies the direction of the screw rather than the depth of penetration.
Conclusion
Lag screws inserted through cephalocondylic nails achieve a more accurate position in the femoral head compared with the sliding screw plate system for extracapsular fractures of the neck of the femur. This paper provides an explanation for the difference in tip apex distance measurement between the two devices, complementing the current literature.
References
- 1.Audige L, Hanson B, Swiontkowski MF. Implant-related complications in the treatment of unstable intertrochanteric fractures: meta-analysis of dynamic hip screw plate versus dynamic screw-intramedullary devices. Int Orthop. 2003;27(4):197–203. doi: 10.1007/s00264-003-0457-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995;77(7):1058–1064. doi: 10.2106/00004623-199507000-00012. [DOI] [PubMed] [Google Scholar]
- 3.Kawaguchi S, Sawada K, Nabeta Y. Cutting out of the lag screw after internal fixation with the Asiatic gamma nail. Injury. 1998;29(1):47–53. doi: 10.1016/S0020-1383(97)00158-7. [DOI] [PubMed] [Google Scholar]
- 4.Parker MJ. Cutting-out of the dynamic hip screw related to its position. J Bone Joint Surg Br. 1992;74(4):625. doi: 10.1302/0301-620X.74B4.1624529. [DOI] [PubMed] [Google Scholar]
- 5.Pervez H, Parker MJ, Vowler S. Prediction of fixation failure after sliding hip screw fixation. Injury. 2004;35:994–998. doi: 10.1016/j.injury.2003.10.028. [DOI] [PubMed] [Google Scholar]