Abstract
Data from 44 patients (23 males, 21 females) with a median age of 39 (range 13–80) years who underwent total hip arthroplasty for proximal femoral tumours (1994–2004) were analysed. The histological diagnoses included 14 metastases, six osteosarcomas, six chondrosarcomas, four Ewing’s sarcomas, four giant cell tumours, three malignant fibrous histiocytomas, two parosteal and two periosteal osteosarcomas, and one each primary neuroectodermal tumour, myeloid disease, and aneurysmal bone cyst. Twenty-one patients (48%) had pathological fractures. The cause of the pathological fracture was metastasis in 12 patients (57%). Twenty-eight patients (64%) had soft tissue invasion. Complications observed in 17 patients (37%) were local recurrence in two, postoperative haematoma in two, dislocation of prosthesis in five, deep infection in six, and one patient died of myocardial infarction in the early postoperative period. During our midterm survival analysis, functional results were excellent in 25% of patients, good in 57%, fair in 12%, and poor in 6%.
Résumé
Entre 1994 et 2004, nous avons récolté les données de 44 patients (23 hommes et 21 femmes), dont l’âge moyen était de 39 ans (de 13 à 80), qui ont bénéficié d’une prothèse totale de hanche pour une tumeur de l’extrémité proximale du fémur 4. Le diagnostic étiologique a inclus, chez ces patients, 14 métastases, 6 ostéosarcomes, 6 chondrosarcomes, 4 sarcomes d’Ewing, 4 tumeurs à cellules géantes, 4 histiocytomes malins, 2 sarcomes paraosteal, 2 sarcomes périosters et une tumeur neuroectodermique, un myélome un kyste anévrismal. 21 patients (48%) présentaient une fracture pathologique. La fracture pathologique était une métastase chez 12 patients (soit 57%). Pour 28 patients (64%) avaient un envahissement des parties molles. Des complications ont été observées chez 17 patients (37%) avec 2 récidives locales de la tumeur, 2 hématomes post-opératoires, 5 luxations de prothèse, 6 infections profondes et un patient décédé d’infarctus du myocarde en post opératoire précoce. Le résultat fonctionnel a été noté excellent à moyen terme chez 25 patients, bon chez 57%, moyen pour 12% et mauvais pour 6% des patients.
Introduction
For many decades, disarticulation of the hip joint was the method of choice for proximal femoral tumours. A great deal of attention has been focused on malignant bone tumours in recent years because of the great progress made in the multidisciplinary management of the more common tumours, including osteogenic sarcoma and Ewing’s sarcoma. Nowadays, femoral tumour resection with endoprosthetic replacement is one of the most commonly used treatment methods [7, 8]. However, it has several technical difficulties, including reconstruction of abductor mechanism, soft tissue coverage, and hip joint bio mechanics [13]. Although endoprosthetic replacement has its own complications, such as dislocation, periprosthetic infections, and aseptic loosening, the tumour endoprosthesis allows removal of all affected parts of the femur and assures a good functional recovery [2, 7, 10]. The purpose of this retrospective study was to evaluate the midterm survival and functional outcome as well as surgical and technical complications in patients who had an endoprosthetic replacement for primary malignant and metastatic tumours of the proximal femur.
Patients and methods
Between 1994 and 2004, 44 patients underwent resection of the proximal femur with endoprosthetic replacement in the Department of General Oncology (bone and soft tissue tumours), N.N. Blokhin Russian Cancer Research Center and in the Department of Orthopaedics & Traumatology, Moscow Regional Clinical Research Institute (MONIKI), Moscow, Russian Federation. There were 23 males and 21 females. The mean age of the patients was 39 years, but there was a bimodal distribution to the age range spanning from 13 to 80 years. Follow-up ranged from 1 to 10 years. In all cases, we performed a limb salvage procedure (endoprosthetic hip replacement) with different custom-made prostheses, such as Poldi, Beznoska, Prospon (Czech Rebuplic), Link (Germany), Mathys (Switzerland), and Sivasha (Russia).
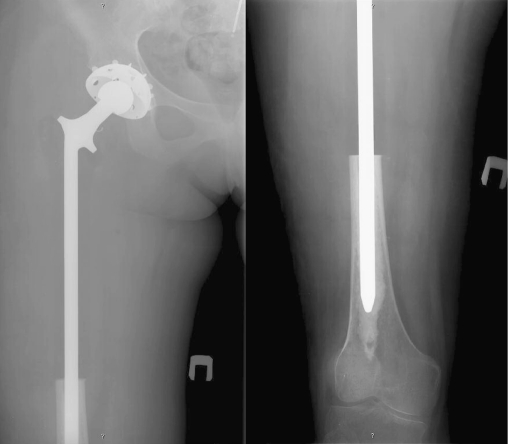
Preoperative work-up was standard and consisted of history and clinical examination, routine laboratory tests and anaesthetic assessment, plain radiography of the limb, computed tomography (CT) scan of the limb and chest, technetium-99m bone scan, and, in most cases, magnetic resonance imaging (MRI) of the affected limb (Fig. 1). A patient receiving intra-arterial chemotherapy was given an angiogram of the affected leg (Fig. 2). Preoperative antibiotics were given prior to surgery. Open biopsy was used to obtain material for histopathological examination. Chemotherapy commenced 6 weeks prior to surgery in those cases diagnosed as osteosarcoma, Ewing’s sarcoma, and dedifferentiated chondrosarcoma. The patients were staged according to the Enneking’s staging system [1, 18]. Twenty-one patients presented with pathological fracture, and 28 patients had soft issue invasion of the tumour. Adjuvant chemotherapy was given to 24 patients, preoperative irradiation was given to nine patients, and 25 patients received neoadjuvant chemotherapy.
Fig. 1.
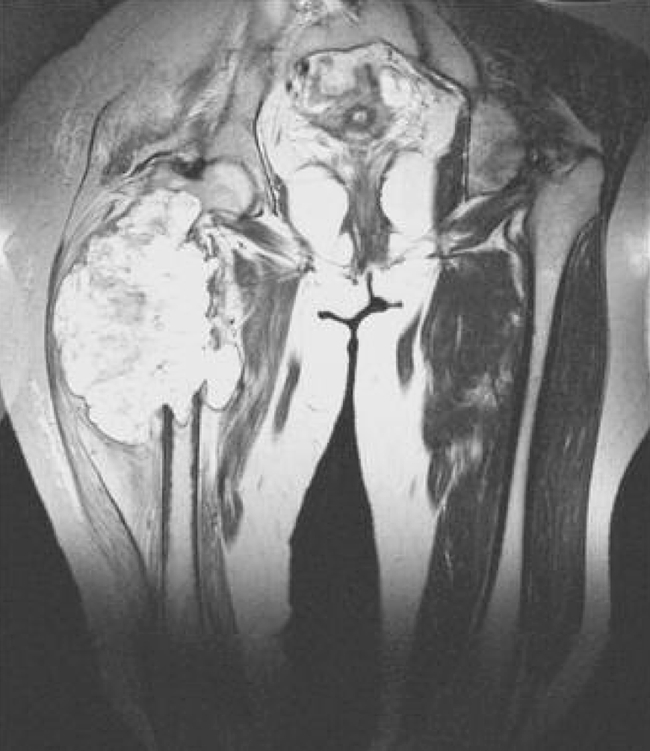
Magnetic resonance imaging of a patient with osteosarcoma of the right femur
Fig. 2.

Arteriography of the right hip joint of the same patient with osteosarcoma
Prostheses used were specially ordered and customised for each patient. The required dimensions were estimated using X-rays in all patients. The tumour was resected using oncological principles with the intention of preserving an intact layer of normal tissue over the tumour to obtain a wide margin. The hip capsule was divided as close to the femur as was considered safe for tumour resection and subsequently repaired using a nonabsorbable purse-string suture around the neck of the prosthesis to prevent dislocation. In cases where the tumour extended into the femoral neck, very little capsule could be left, and no repair was possible. Special care was taken to reattach the abductors and psoas muscle to the prostheses. Patients were allowed to walk with crutches 2 weeks after operation and were advised to attend the clinic every 3 months during the first year after operation and every 6 months thereafter. Radiographic data were obtained from anteroposterior and lateral views of the hip and femur taken at the latest follow-up (Fig. 3).
Fig. 3.
Post operative X-ray of the femur: anteroposterior view
Results
Oncological outcome
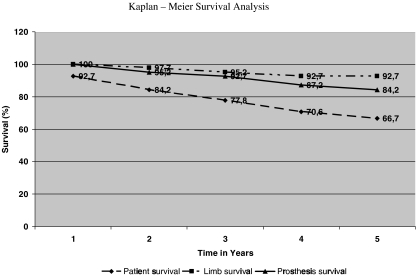
Overall survival rate was 66.7% at 5 years. Two (4.5%) patients had local recurrence. Twelve (27.7%) patients had metastases after surgery, and 11 (25%) died. There was no evidence of disease in 32 patients.
Limb survival
In three patients, we performed disarticulation of the hip joint because of the local recurrence. The overall survival rate was 92.7% at 5 years.
Prosthetic survival
The overall survival rate of prostheses survival was 84.2% at 5 years. One patient required revision hip replacement. In one patient, the acetabular cup and in one patient the stem of the endoprosthesis alone were replaced. All the survival analyses were done using Kaplan – Meier survivorship analysis method (Fig. 4).
Fig. 4.
Forty-four cases with tumour prosthesis for proximal femoral tumours. X axis time in years; Y axis survival in percentage
Functional outcome
Functional outcome was estimated using Enneking’s evaluation criteria [5], an assessment that evaluates pain, functional limitation, walking distance, use of support, gait, and emotional acceptance as parameters. At the latest follow-up, functional results were excellent in 11 (25%) patients, good in 25 (57%), fair in five (12%), and poor in three (6%).
Complications
In our experience, periprosthetic infection was the most common complication. Out of 44, six (13.6%) patients had late infection; four 9.1%) were treated conservatively with antibiotics and in two (4.5%), we performed a revision endoprosthetic hip replacement to treat the infection. Staphylococcusaureus was the most common pathogen identified. Results were excellent after the treatment, i.e, no recurrence of infection. In five patients, dislocation of the endoprosthesis occurred in the postoperative period. The dislocation was reduced with satisfactory functional results. In two patients, haematoma was observed in the postoperative period. The endoprosthesis was unstable in six patients. Local tumour recurrence occurred in two patients, and three showed evidence of lung metastases. One patient died of myocardial infarction in the early postoperative period.
Discussion
The popularity of limb salvage procedures in the treatment of aggressive benign and malignant musculoskeletal neoplasms increased markedly in the 1980s as a result of improved operative techniques, better patient selection, and advances in prosthetic design. Limb salvage now is considered the standard procedure for treatment of malignant bone tumours in many centres [2, 3, 6, 7, 12, 10]. According to several authors, dislocation of the endoprosthesis is the most frequent complication [14, 15, 17]. But in our experience, infection rate (13.6%) was slightly higher than dislocation (9%). Preservation of hip-joint capsule and capsulorraphy over the prosthetic head are the major factors in prevention of dislocation. Stability is also enhanced by reattaching the abductor mechanism to the endoprosthesis.
It is generally accepted that limb salvage surgery leads to an increased risk of local recurrence, but there is no convincing evidence that this leads to decreased survival [15, 16]. In our experience, only two patients had local recurrence, denoting the oncological adequacy of the resections.
Another option when replacing the proximal femur is to use an allograft or allograft prosthesis composite. The advantage of an allograft is that it allows for direct reattachment of soft tissues to bone and theoretically will provide a more functional hip. The integration of the graft into the host bone may provide a more secure long-term reconstruction. A specimen of the appropriate size and shape is easy to obtain, and this facilitates reconstruction [9, 19].
The management of malignant bone tumours of the proximal femur remains a surgical challenge, and this study showed that successful midterm results can be obtained with massive endoprostheses despite the incidence of recognised complications, including polyethylene wear and aseptic loosening. Preoperative evaluation and planning, meticulous surgical technique, and adequate postoperative management are essential. Though the extent of the muscle and bone resection is large, there is no doubt that endoprosthetic replacement of the proximal femur provides a good functional and oncological outcome when compared with the various other reconstructive operations.
References
- 1.Bacci G, Longhi A, Fagioli F, Briccoli A, Versari M, Picci P. Adjuvant and neoadjuvant chemotherapy for osteosarcoma of the extremities: 27 year experience at Rizzoli Institute, Italy. Eur J Cancer. 2005;41(18):2836–2845. doi: 10.1016/j.ejca.2005.08.026. [DOI] [PubMed] [Google Scholar]
- 2.Bickels J, Meller I, Henshaw RM, Malawer MM. Reconstruction of hip stability after proximal and total femur resections. Clin Orthop Relat Res. 2000;375:218–230. doi: 10.1097/00003086-200006000-00027. [DOI] [PubMed] [Google Scholar]
- 3.Capanna R, Ruggeri P, Decristofaro R et al (1991) Complications, their treatment and outcome in 257 cementless megaprostheses. In: Brown KLB (ed) Complications of limb salvage. Prevention, management and outcome. International Symptosium on Limb Salvage, Montreal, pp 147–150
- 4.Chang DW, Weber KL. Use of a vascularized fibula bone flap and intercalary allograft for diaphyseal reconstruction after resection of primary extremity bone sarcomas. Plast Reconstr Surg. 2005;116(7):1918–1925. doi: 10.1097/01.prs.0000189203.38204.d5. [DOI] [PubMed] [Google Scholar]
- 5.Enneking WF, Dunham W, Gebherdt MC, Malawar N, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumours of the musculoskeletal system. Clin Orthop. 1993;286:241–246. [PubMed] [Google Scholar]
- 6.Ferrapie AL, Brunel P, Besse W, Altermatt E, Bontoux L, Richard I. Lower limb proximal amputation for a tumour: a retrospective study of 12 patients. Prosthet Orthot Int. 2003;27(3):79–185. doi: 10.1080/03093640308726680. [DOI] [PubMed] [Google Scholar]
- 7.Grimer RJ, Bielack S, Flege S, Cannon SR, Foleras G, Andreeff I, Sokolov T, Taminiau A, Dominkus M, San-Julian M, Kollender Y, Gosheger G. Periosteal osteosarcoma - a European review of outcome. Eur J Cancer. 2005;41(18):2806–2811. doi: 10.1016/j.ejca.2005.04.052. [DOI] [PubMed] [Google Scholar]
- 8.Kabukcuoglu Y, Grimer RJ, Tillman RM, Carter SR. Endoprosthetic replacement for primary malignant tumours of the proximal femur. Clin Orthop. 1999;358:8–14. doi: 10.1097/00003086-199901000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Lobo Gajiwala A, Agarwal M, Puri A, D’Lima C, Duggal A. The use of irradiated allografts in reconstruction of tumor defects - the tata memorial hospital experience. Cell Tissue Bank. 2003;4(2–4):125–132. doi: 10.1023/B:CATB.0000007025.14614.42. [DOI] [PubMed] [Google Scholar]
- 10.Malawer MM, Chou LB. Prosthetic survival and clinical results with use of large-segmental replacements in the treatment of high-grade bone sarcomas. J Bone Joint Surg Am. 1995;77:1154–1165. doi: 10.2106/00004623-199508000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Malkani AL, Settecerri JJ, Sim FH, Chao EYS, Wallrichs SL. Long-term results of proximal femoral replacement for non-neoplastic disorders. J Bone Joint Surg Br. 1995;77:351–356. [PubMed] [Google Scholar]
- 12.Ogilvie CM, Wunder JS, Ferguson PC, Griffin AM, Bell RS. Functional outcome of endoprosthetic proximal femoral replacement. Clin Orthop Relat Res. 2004;426:44–48. doi: 10.1097/01.blo.0000136840.67864.78. [DOI] [PubMed] [Google Scholar]
- 13.Ozaki T, Kaneko S, Kunisada T, Kawai A, Dan’ura T, Naito N, Inoue H. Reconstruction of the hip abductors after resection of the proximal femur. Int Orthop. 1999;23(3):182–183. doi: 10.1007/s002640050342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Renard AJ, Veth RP, Schreuder HW, Loon CJ, Koops HS, Horn JR. Function and complications after ablative and limb-salvage therapy in lower extremity sarcoma of bone. J Surg Oncol. 2000;73(4):198–205. doi: 10.1002/(SICI)1096-9098(200004)73:4<198::AID-JSO3>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 15.Rougraff BT, Simon MA, Kneisl JS, Greenberg DB, Mankin HJ. Limb salvage compared with amputation for osteosarcoma of the distal end of the femur. J Bone Joint Surg Am. 1994;76:649–656. doi: 10.2106/00004623-199405000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Tunn PU, Delbruck H, Schlag PM. Ablative procedures in surgical treatment of malignant bone tumors. Orthopade. 2003;32(11):955–964. doi: 10.1007/s00132-003-0547-6. [DOI] [PubMed] [Google Scholar]
- 17.Ward WG, Dorey F, Eckardt JJ. Total femoral endoprosthetic reconstruction. Clin Orth. 1995;316:195–206. [PubMed] [Google Scholar]
- 18.Wolf RE, Enneking WF. The staging and surgery of musculoskeletal neoplasms. Orthop Clin North Am. 1996;27:473–481. [PubMed] [Google Scholar]
- 19.Zehr RJ, Enneking WF, Scarborough MT. Allograft-prosthetic composite versus megaprosthesis in proximal femoral reconstruction. Clin Orth. 1996;322:207–223. doi: 10.1097/00003086-199601000-00026. [DOI] [PubMed] [Google Scholar]