Abstract
We examined the incidence of avascular necrosis (AVN) of the healthy femoral head in unilateral hip dysplasia at the end of the use of the Pavlik harness. The evaluation of AVN was done with the help of standardised roentgenograms. Between 1974 and 1982, 1,064 dysplastic hips (869 children) were treated with the Pavlik harness at the Orthopaedic Department of Semmelweis University. Of these, 674 children who had unilateral hip dysplasia were chosen for this study. In the period of our investigation, ultrasonography was not yet used routinely, so in some cases the hip was mistakenly diagnosed as dysplastic. The average patient age was 3.2 months, and the average length of treatment was 4.9 months. We found no correlation between the appearance of AVN in the healthy hips at the end of treatment with the Pavlik harness and the age of the child at the start of treatment. On the other hand, there was a strong significant correlation between the appearance of AVN and the length of treatment.
Résumé
Nous avons examiné l’incidence de la nécrose avasculaire de la tête fémorale dans les dysplasies unilatérales de hanches à la fin du traitement utilisant le harnais de Pavlik. L’évaluation de cette nécrose avasculaire a été déterminée à l’aide des radiographies standards. Entre 1974 et 1982, 1064 hanches dysplasiques (869 enfants) ont été traitées par harnais de Plavik au Département de l’Université Semmelweis. Parmi cette population, 674 enfants, présentant une lésion unilatérale de la hanche ont été choisis pour cette étude. Au moment de cette étude l’écho doppler de la hanche n’était pas utilisé en routine, ainsi certaines hanches ont été, à tort, diagnostiquées comme dysplasiques. L’âge moyen des patients était de 3,2 mois et la durée moyenne du traitement a été de 4,9 mois. Nous n’avons pas trouvé de corrélation entre l’aspect de la nécrose avasculaire de la hanche à la fin du traitement de l’harnais de Pavlik et de l’âge de l’enfant au moment du début du traitement. Par contre, il existe une corrélation significative entre l’existence de la nécrose avasculaire et la durée du traitement.
Introduction
Avascular necrosis (AVN) occurs with every form of hip splintage. Forceful reduction and passive abduction in the Lorenz position involve an unacceptably high risk of AVN [3].
Since Pavlik first reported on the effectiveness of his orthotic device 60 years ago, his harness has been used to manage congenital dislocation and dysplasia of the hip [6]. The harness allows spontaneous movements in the safe zone of the lower extremity and prevents flexion and adduction. This should lead to physiological and gentle reduction of the hip joint [8]. The Pavlik harness works by shifting the femoral head from the superior position to the posterior rim of the acetabulum, which is indicated by the flexion of the hip joint. The abducted position stretches the adductor muscles with the help of the weight of the lower extremity. This procedure helps the dislocated femoral head to slide anteriorly back into the acetabulum. This movement of the femoral head is more effective during deep sleep, because of the decreased muscle tone [4]. The most serious complication of the treatment is AVN of the proximal femoral epiphysis, which is mostly iatrogenic [8]. Early recognition and functional treatment of congenital dislocation and dysplasia of the hip greatly decreases the appearance of AVN [3]. In this retrospective study, we examined the incidence of AVN of the healthy femoral head in unilateral hip dysplasia treated with the Pavlik harness.
Materials and methods
Between 1974 and 1982, 1,064 dysplastic hips (869 children) were treated with the Pavlik harness at the Orthopaedic Department of Semmelweis University in Budapest. Of these, 674 children with unilateral hip dysplasia were chosen for this study. The period of investigation coincides with the time when the diagnosis of the dysplastic hip was, mistakenly, made more frequently than it should have been because at that time ultrasonography of the hip was not routinely done. The average age of the patients treated with the Pavlik harness was 3.2 months (range 1–7 months), and the average length of the treatment was 4.9 months (range 1–9 months). The position of the femoral head and the state of the acetabulum were checked at the end of treatment by standardised anteroposterior radiographs. These were made with the infant in supine position, with both lower extremities extended, parallel, and maintained in neutral position between external and internal rotation.
The Tönnis classification was used to evaluate AVN of the proximal femoral epiphysis [10]. Tönnis divided AVN types into four grades. The first is the mildest. The rim of the ossific nucleus is blurred, and the substance is mildly granular. After treatment, the hip joint will recover totally. In grade II, Tönnis described the rim of the ossific nucleus as being more irregular and the substance more granular than in the first grade. In some cases a cyst can be seen in the proximal epiphysis of the femur. After treatment in this grade also, the hip joint will recover totally, with no late consequences of AVN. In grade III, the ossific nucleus is seriously damaged, and only smaller pieces or strips are recognisable. Recovery of the femoral head is possible, but if the growth plate is damaged by the AVN, deformity in the femoral head or in the neck of the femur may ensue. In grade IV, the growth plate is damaged, and the proximal metaphysis of the femur may be involved, which can disturb the normal rhythm of growing. These changes usually become visible too late, when the shortening or varus or valgus deformity of the femoral neck is recognisable. We used this classification to evaluate the state of the femoral head at the end of treatment.
The chi square test and the chi square test for trend were used for the statistical analysis. The calculations were done with the help of the Open Office 1.1. program.
Results
The overall incidence of AVN in our series was 11.7% (125 of the 1,064 hips). The appearence of AVN in unilateral hip dysplasia after treatment with the Pavlik harness was 9.9% (66 of the 674 hips). These patients (hips) were split into two groups: dysplastic hips and healthy but treated hips (Table 1). Of the dysplastic hips, 5.2% AVN were graded Tönnis I, 0.6% Tönnis II, and 1.2% Tönnis III. Of the healthy but treated hips, 2.7% had Tönnis I AVN, and 0.2% had grade II.
Table 1.
The appearance of avascular necrosis (AVN) in unilateral hip dysplasia after the use of the Pavlik harness on the dysplastic and the normal contralateral sides
| Incidence of AVN on the dysplastic side | Incidence of AVN on the normal contralateral side | |||
|---|---|---|---|---|
| Results | Hips (n) | Results | Hips (n) | |
| Tönnis I | 5.2% | 35 | 2.7% | 18 |
| Tönnis II | 0.6% | 4 | 0.2% | 1 |
| Tönnis III | 1.2% | 8 | 0 | 0 |
Because the difference in outcome between the first and second groups of Tönnis classification is small, these two grades were combined for evaluation of the results.
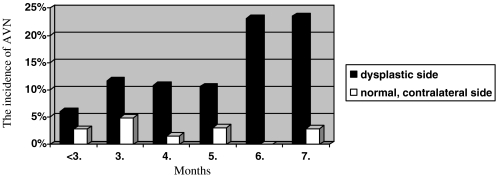
First we grouped the patients according to their ages at the start of treatment, and we examined the incidence of AVN in the dysplastic and in the normal contralateral hips. In the dysplastic hip group, we found that under 3 months of age, 6% of the hips showed signs of AVN; at 3 months, 11.7%; at 4 months, 10.8%; at 5 months, 10.6%; at 6 months, 23.1%; and at 7 months, 23.5% (Table 2). When we examined the group of healthy but treated hips, the incidence of AVN was 2.8% under 3 months of age, 4.9% at 3 months, 1.5% at 4 months, 3% at 5 months, 0% at 6 months, and 2.9% at 7 months (Fig. 1, Table 3).
Table 2.
The incidence of avascular necrosis (AVN) on the dysplastic side; the patients (hips) were grouped according to patient age at the start of treatment
| Months | <3 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|
| Hips with AVN | 19 | 12 | 14 | 7 | 6 | 8 |
| Number of hips | 317 | 102 | 129 | 66 | 26 | 34 |
| Incidence of AVN | 6% | 11.7% | 10.8% | 10.6% | 23.1% | 23.5% |
Fig. 1.
The incidence of avascular necrosis (AVN) in unilateral hip dysplasia. Patients were grouped according to their ages at the start of treatment. The x-axis shows the patient age at the start of treatment, and the y-axis shows the incidence of AVN
Table 3.
The appearance of avascular necrosis (AVN) in unilateral hip dysplasia after the use of the Pavlik harness on the normal contralateral side; the patients (hips) were grouped according to their ages at the start of treatment
| Months | <3 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|
| Hips with AVN | 9 | 5 | 2 | 2 | 0 | 1 |
| Number of hips | 317 | 102 | 129 | 66 | 26 | 34 |
| Incidence of AVN | 2.8% | 4.9% | 1.6% | 3% | 0% | 2.9% |
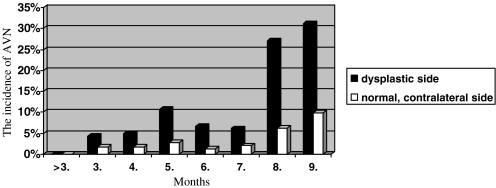
Then we regrouped the patients according to the length of treatment. We found that when the Pavlik harness was used less than 3 months, no AVN developed on either the affected or the normal contra-lateral side. After this, the incidence of AVN was as follows: 3 months, 4.2%; 4 months, 4.9%; 5 months, 10.8%; 6 months, 6.6%; 7 months, 6.1%; 8 months, 27.1%; and after 9 months, 31.1% (Table 4). When we evaluated these results in the healthy but treated hips, the AVN incidence after 3 months was 1.7%; 4 months, 1.6%; 5 months, 2.7%; 6 months, 1.3%; 7 months, 2%; 8 months, 6.25%; and after 9 months, 9.8% (Fig. 2, Table 5).
Table 4.
The appearance of avascular necrosis (AVN) in unilateral hip dysplasia after the use of the Pavlik harness on the dysplastic side; the patients (hips) were grouped according to the length of treatment
| Months | <3 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|
| Hips with AVN | 0 | 5 | 9 | 12 | 5 | 3 | 13 | 19 |
| Number of hips | 30 | 118 | 182 | 111 | 75 | 49 | 48 | 61 |
| Incidence of AVN | 0% | 4.2% | 4.9% | 10.8% | 6.6% | 6.1% | 27.1% | 31.1% |
Fig. 2.
The incidence of avascular necrosis (AVN) in unilateral hip dysplasia. The patients were grouped according to the length of treatment. The x-axis shows the length of the treatment, and the y-axis shows the incidence of AVN
Table 5.
The appearance of avascular necrosis (AVN) in unilateral hip dysplasia after the use of the Pavlik harness on the normal contralateral side; the patients (hips) were grouped according to the length of treatment
| Months | <3 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|
| Hips with AVN | 0 | 2 | 3 | 3 | 1 | 1 | 3 | 6 |
| Number of hips | 30 | 118 | 182 | 111 | 75 | 49 | 48 | 61 |
| Incidence of AVN | 0% | 1.7% | 1.6% | 2.7% | 1.3% | 2% | 6.25% | 9.8% |
To evaluate the relationship between patient age at the start of treatment and the appearance of AVN in the normal healthy hips, we used the chi square test. It showed that the age at the start of treatment did not influence the development of AVN (p=0.67833). We used the same test to correlate the length of treatment and the incidence of AVN. It showed significant difference between the subgroups (p=0.0245). Finally, the chi square test for trend showed that the longer the treatment, the higher the probability that AVN will develop (p=0.0011).
Discussion
The incidence of AVN after treatment with the Pavlik harness has been examined by several authors. Grill et al. found AVN at the end of the treatment in 2.38% of affected hips [3], Iwasaki found it in 7.2% [4], and Suzuki et al. [9] in 8%. When we grouped our patients (hips) according to their ages at the start of treatment, we found a close relationship between age and incidence of AVN on the dysplastic side, which matches the findings of several other authors in the international orthopaedic literature. Grill et al. reported that if the treatment is started within the first 3 months of life, the rate of AVN is only 50% of that which occurs if treatment begins between the 3rd and 6th months of life [3]. Kruczynski et al. found that if treatment is started after the 6th month of life, the appearance of AVN in the affected hip is significantly higher than under that age [5].
Esteve noted in 1960 that in one of his patients, AVN developed in the healthy hip at the end of treatment of congenital hip dislocation [1]. Salter et al. [7], Gore [2], and Westin and Ilfeld [11] noticed the same phenomenon. Iwasaki found roentgenographic changes referring to AVN in two normal contra-lateral hips out of 193 during treatment of the dislocated hip [4].
Our study demonstrated that during the treatment of unilateral hip dysplasia, AVN could be detected on the normal contra-lateral side. We found only mild changes in the proximal epiphysis of the femurs. Only the first and second grades of the Tönnis classification were detected, at an incidence of 2.7% for Tönnis I and 0.2% for Tönnis II. We found no relationship between the appearance of AVN in the healthy hips at the end of treatment with the Pavlik harness and the child’s age at the start of treatment. On the other hand, there was a highly significant correlation between the appearance of AVN and the length of treatment. These results were proven by statistical analysis.
During and after the treatment of unilateral hip dysplasia and dislocation, the appearance of AVN on the dysplastic, dislocated side is a well-known complication. Based on our results, we have established that mild AVN (Tönnis grades I and II) can also develop in the normal contra-lateral side. We found no severe AVN (Tönnis grade III) that could cause lasting damage in the proximal femoral epiphysis. The development of AVN mainly depends on the length of use of the Pavlik harness.
Footnotes
An erratum to this article can be found at http://dx.doi.org/10.1007/s00264-006-0262-0
References
- 1.Esteve R (1960) Congenital dislocation of the hip. A review and assessment of results of treatment with special reference to frame reduction as compared with manipulative reduction. J Bone Joint Surg Br 42:253–263 [DOI] [PubMed]
- 2.Gore DR (1974) Iatrogenic avascular necrosis of the hip in young children. A review of six cases. J Bone Joint Surg Am 56:493–502 [PubMed]
- 3.Grill F, Bensahel H, Canadell J, Dungl P, Matasovic T, Vízkelety T. The Pavlik harness in the treatment of congenital dislocating hip: report on a multicenter study of the European Paediatric Orthopaedic Society. J Pediatr Orthop. 1988;8:1–8. doi: 10.1097/01241398-198801000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Iwasaki K (1983) Treatment of the congenital dislocation of the hip by the Pavlik harness: mechanism of reduction and usage. J Bone Joint Surg Am 65:760–767 [PubMed]
- 5.Kruczynski J. Avascular necrosis of the proximal femur in developmental dislocation of the hip. Acta Orthop Scand. 1996;67(Suppl 268):7–12. [PubMed] [Google Scholar]
- 6.Mubarak S, Garfin S, Vance R, McKinnon B, Sutherland D (1981) Pitfalls in the use of the Pavlik harness for treatment of congenital dysplasia, subluxation, and dislocation of the hip. J Bone Joint Surg Am 63:1239–1248 [PubMed]
- 7.Salter RB, Kostuik J, Dallas S. Avascular necrosis of the femoral head as a complication of treatment for congenital dislocation of the hip in young children: clinical and experimental investigation. Can J Surg. 1969;12:44–61. [PubMed] [Google Scholar]
- 8.Song K, Lapinsky A. Determination of hip position in the Pavlik harness. J Pediatr Orthop. 2000;20:317–319. doi: 10.1097/00004694-200005000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Suzuki S, Kashiwagi N, Kasahara Y, Seto Y, Futami T (1996) Avascular necrosis and the Pavlik harness: the incidence of avascular necrosis in three types of congenital dislocation of the hip as classified by ultrasound. J Bone Joint Surg Br 78:631–635 [PubMed]
- 10.Tönnis D (1984) Die angeborene Hüftdysplasie und Hüftluxation. Springer-Verlag, Berlin Heidelberg New York, pp 208–209
- 11.Westin GW, Ilfeld FW. Total avascular necrosis of capital femoral epiphysis in congenital dislocated hips. Clin Orthop. 1976;119:93–98. [PubMed] [Google Scholar]