Abstract
We evaluated the mid-term clinical and radiographical performance of a cohort of patients who underwent primary total hip replacement with a modern, forged cobalt–chrome, polished cemented femoral stem with proximal and distal centralisation. Sixty-seven patients with 73 hybrid total hip replacements were followed up clinically and radiographically for an average of 6.1 years (4–8.5). No patient was lost. No hips required revision, and all stems are radiographically well-fixed. Four hips developed localised osteolysis: one at the site of a proximal periprosthetic fracture, another at the level of a lateral femoral window of a previous core decompression, the third at the mid third of the femoral component, and the fourth on the greater trochanter, associated with accelerated polyethylene wear. This modern polished stem yielded excellent, predictable clinical and radiographic results at an intermediate follow-up.
Résumé
Nous évaluons à moyen terme un groupe de patients après arthroplastie totale primaire de la hanche avec une tige cimentée, en chrome cobalt poli, a centralisation proximale et distale. Soixante sept patients avec 73 prothèses hybrides étaient suivis cliniquement et radiologiquement pendant une durée moyenne de 6,1 ans (4–8,5), sans perdu de vue. Aucune hanche n’avait eu de révision chirurgicale, et toutes les tiges étaient radiologiquement bien fixées. Quatre hanches avaient, une ostéolyse localisée : au niveau d’une fracture péri-prothétique proximale, au niveau de la fenêtre corticale d’un précédent forage, à hauteur du tiers moyen de la tige et au niveau du grand trochanter associé à une usure précoce du PE. Cette tige fémorale donne un excellent résultat à moyen terme.
Introduction
Two of the first successful cemented femoral components were highly polished stems: the flatblack Charnley [9], and the double-tapered Exeter [3, 7, 8, 14, 26, 38]. The survivorship, free of revision for aseptic loosening, for the Charnley stem ranged from 90 to 98%, after a follow-up of 20 to 30 years [3, 7, 8, 38]. The long-term results of the original Exeter stem, demonstrated femoral aseptic loosening in seven of 374 patients (1.8%) after a follow-up of 11 to 16 years [14].
Poor metallurgy led to plastic deformation [24] and stem fracture [10], which was reported in 0.23% [10] to 11% [27] of the first-generation stainless steel, or cast cobalt–chrome cemented stems. In addition, inconsistent stem centralisation and finger-packing of the cement led to areas of incomplete cement mantle, which were considered detrimental to the long-term survivorship of the arthroplasty [1, 21, 23].
The senior author (EAS) has implanted a modern, forged cobalt-chromium, polished, tapered cemented femoral stem, with proximal and distal centralisation (VerSys CT, Zimmer, Warsaw, IN) since December 1996 (Fig. 1). The aim of study is to analyse the midterm clinical and radiographic performance of a cohort of patients who underwent primary total hip replacement with this femoral stem.
Fig. 1.

Anteroposterior view of the polished VerSys CT stem utilized in the present study
Materials and methods
Between December 1996 and February 1998, 67 patients underwent 73 primary hybrid total hip replacements (six of them one-stage bilateral) by the senior author (EAS) utilizing a polished cemented femoral stem (VerSys CT, Zimmer, Warsaw, IN). The main features of the stem included an anatomic design, tapered in the frontal plane, with rounded corners, a micro-collar and highly polished surface finish (radius, 0.5 μm). It was made of forged cobalt–chromium in six standard sizes (12 to 17), and with a high offset for the sizes 13 to 16. It had a 12/14 Morse taper and rectangular neck geometry, minimised in the anteroposterior dimension to maximise range of motion. The head sizes were provided in 22, 26, 28 and 32 mm, and the lengths in −3.5 mm, 0, +3.5, +7, and +10.5 (the latter two with a skirt). It was cemented in place with proximal and distal polymethylmethacrylate centralisers.
The operation was performed through a posterolateral approach under hypotensive epidural anaesthesia [33]. All stems were implanted utilizing modern cementing technique which included a cement restrictor (Kinamed, Amarillo, CA, USA) and vacuum-mixed Simplex P bone cement, which was injected in a retrograde fashion with a cement gun. Prior to cementation, the femoral canal was irrigated copiously and aspirated until it was dry. During cement injection and after the proximal femur had been filled, the surgeon occluded the proximal femoral opening and continued to inject cement under pressure. During insertion of the stem, the assistant’s thumb was placed in the medial aspect of the proximal femoral opening to prevent cement extrusion. The femoral component and the polymer were heated to 40°C to decrease polymerisation time and interface porosity [4, 12, 20, 29]. A cobalt–chromium modular head was used in all patients, with a 28 mm diameter in 64 hips (87.67%), 22 mm diameter in seven hips (9,59%), and 32 mm and 26 mm diameter in one hip each (1,37%). The 22 mm heads were implanted in young patients with a small acetabular diameter to maximise polyethylene thickness. A Trilogy (Zimmer, Warsaw, IN, USA) cementless acetabular cup was implanted in all patients, and the mid-term follow-up study of the acetabular component has been recently published [16].
None of the patients was lost to follow-up. Of the original group of 67 patients (73 hips), three patients (three hips) died of causes unrelated to surgery three, four and five years after surgery with an intact total hip arthroplasty. Thus, the study group consisted of 64 patients (44 women, 20 men) with 70 hips (27 right hips, 31 left hips and 6 bilateral). The mean age of the patients at the time of surgery was 69 years (range 40–86, SD 10.3). The average height was 1.63 meters (range 1.44–1.85, SD 9.8) and the average weight was 69 kilograms (range 44–115, SD 12.3). Preoperative diagnosis was osteoarthritis in 61 hips, osteonecrosis in five, post-traumatic arthritis in two and dysplasia and rheumatoid arthritis in one hip each. Nine patients (nine hips, 12%) could not return for the last follow-up, and were evaluated by telephone with a detailed questionnaire. No recent radiographs of these patients were available, and they were excluded from the radiographic analysis, leaving 55 patients (61 hips) with a minimum 4-year radiographic follow-up (mean 6.2 years, range 4.2–8.5).
Patients were scored according to the Hospital for Special Surgery (HSS) hip scoring system [30], which was calculated at the last follow-up by two of the authors (AGDV, AZ). The score rates pain, walking ability, motion, and function from 0–10 for a maximum of 40 points. Scores greater than 31 were considered excellent, 31–22 good, 21–16 fair, and 15 or less poor. The differences in the four categories of the HSS hip score before and after surgery were compared using the paired t-test.
On the 6-week postoperative radiographs we measured the alignment of the stem in the frontal plane in degrees [positive (+) for varus alignment and negative (−) for valgus alignment]. The cement mantle was classified according to Barrack et al. [2] On the radiographs obtained at the last follow-up, we determined the radiographic fixation of the femoral stem according to Harris and McGann [19]. The presence, extent, and location of progressive radiolucent lines measuring more than 1 mm, and the areas of femoral osteolysis were evaluated according to the zones defined by Gruen et al. [18]. Radiographic osteolysis was defined as punched-out areas devoid of trabecular bone, usually with a sclerotic border. All radiographs were evaluated and measured by a single observer (AGDV) who was not involved in the surgery, to avoid inter-observer variation and outcome bias.
Results
Clinical results
None of the patients developed aseptic loosening of the femoral component or required revision for any reason. The HSS hip score improved from an average of 16.7 points (range 12–32) preoperatively to 37.8 points (range 28–40) postoperatively at an average follow-up of 6.13 years (range 4–8.5) (P<0.0001) (Table 1). The clinical results at the last follow-up in the 64 living patients was excellent in 61 patients, and good in three. Two patients (2.8%) had a dislocation of the prosthesis at four and seven years after primary surgery. They both had 28-millimeter heads. They were treated with closed reduction and instructed to follow dislocation precautions, without recurrence.
Table 1.
Average, minimum, maximum, and standard deviation values for HSS Hip Scoring system preoperatively and postoperatively
| Preoperative | Postoperative | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Pain | Gait | ROM | Function | Total | Pain | Gait | ROM | Function | Total |
| 4.1 | 3.9 | 4 | 4 | 16.7 | 9.9 | 9.6 | 8.9 | 9.4 | 37.8 |
| 3 | 3 | 3 | 3 | 12 | 8 | 4 | 4 | 6 | 28 |
| 8 | 8 | 8 | 8 | 56 | 10 | 10 | 10 | 10 | 40 |
| 1 | 1 | 1 | 1 | 6.2 | 0.5 | 1.1 | 1.5 | 1.2 | 2.9 |
All differences are significant (P<0.0001)
Radiographic results
The average alignment of the stem was 0.04° (range: −3 to +2). The cement mantle was classified as type A in 12 hips, B in 40, C1 in 16, and C2 and D in one hip each. At an average follow-up of 6.2 years (range 4.2–8.5), all 55 femoral components were radiographically well fixed. There were no progressive radiolucent lines.
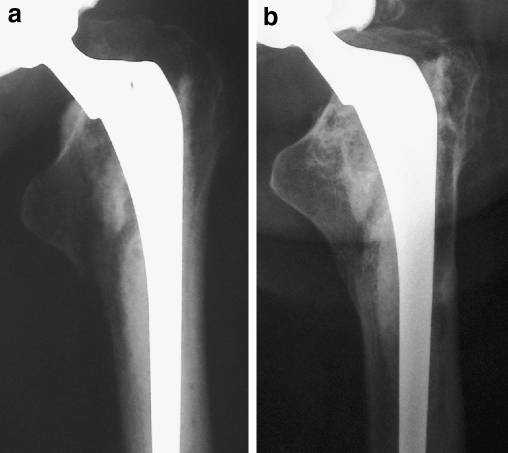
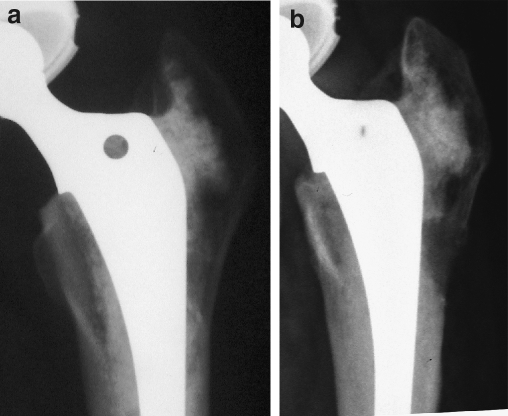
Four hips (7.2%) demonstrated osteolytic lesions. The first patient was a 61-year-old female who sustained a periprosthetic fracture in a skiing accident 26 months after surgery. The fracture occurred in the proximal femur, at the level of the lesser trochanter (Type B1 of the Vancouver Classification [5]); it was minimally displaced, but the fracture extended through the proximal cement mantle (Fig. 2a). The mid and distal stem remained well-fixed. The patient was treated conservatively, with an uneventful healing of the fracture. Five years after the fracture, she developed an osteolytic lesion in Gruen zone 2, where the cement fracture had occurred (Fig. 2b). The second patient was a 40-year-old female who underwent total hip replacement after a failed core decompression for osteonecrosis (Fig. 3a). Eight years after THA, she presented with an osteolytic lesion at the level of the femoral window in the lateral femoral cortex (Fig. 3b). The third patient was a 66-year-old male who developed a 10×5 mm osteolytic lesion in Gruen zone 6, five and a half years after surgery. The fourth patient was a 74-year-old male with osteolysis in the greater trochanter, in association with accelerated polyethylene wear (0.26 mm/year). These four patients have well-fixed stems, are asymptomatic, and the osteolytic areas are under observation with radiographic follow-up every 6 months. They are treated with calcium, vitamin D and diphosphonates and have been advised to avoid strenuous activities.
Fig. 2.
a Non-displaced periprosthetic fracture. There is a fracture of the cement mantle at the level of the lesser trochanter. The stem remains well fixed. b Five years latter, osteolysis developed in the lateral cortex of the femur at the site of the cement fracture
Fig. 3.
a Postoperative radiograph of a total hip arthroplasty with the VerSys CT stem after a failed core decompression for osteonecrosis of the femoral head. b Eight years later, osteolysis developed at the site of the lateral femoral opening. The stem remains well fixed
Discussion
In this study, we report the mid-term clinical and radiographical results of a cemented polished tapered stem for total hip arthroplasty. The design of the stem is inspired by the original Charnley stem, with the addition of proximal and distal centralisation to achieve a homogeneous, circumferential cement mantle. The stems were implanted with modern cementing technique[26].
At 4.2 to 8.5 years of follow-up, the results have been excellent, with no mechanical failures. Low rates of aseptic loosening and osteolysis have been also reported for other modern, polished tapered stems at intermediate follow-up (Table 2). These findings contrast with the high rates of revision for aseptic loosening observed by us [15], and reported by several surgeons, with rough or precoated stems at similar follow-up (Table 3).
Table 2.
Mid-term results of other polished stems
| Author | Year of publication | Femoral stem | Number of hips | Mean age at surgery (years old) | Revisions for femoral aseptic loosening | Radiolucent lines/osteolysis (%) | Follow-up (years) |
|---|---|---|---|---|---|---|---|
| Wroblewski et al. [39] | 2001 | C-Stem | 500 | 53.7 | 0% | NA (*) | 3.5 |
| Williams et al. [37] | 2002 | Exeter Universal | 325 | 67.5 | 0% | 8.9 | 10 to 12 |
| Yates et al. [40] | 2002 | CPT | 76 | 65 | 0% | 7.9 | 5 |
| Present study | – | VerSys CT | 70 | 69 | 0% | 7.2 | 6.1 |
(*) NA: not available. No stem was considered to be at risk of loosening
Table 3.
Series reporting failures with different roughened or precoated stems
| Author | Year | Femoral stem | # of hips | Mean age at surgery (years old) | Revisions for femoral aseptic loosening | Follow-up (years) |
|---|---|---|---|---|---|---|
| Callaghan et al. [7] | 1996 | Iowa Precoat | 131 | 68 | 6.1% | 8 to 9 |
| Sporer et al. [34] | 1998 | Iowa Precoat | 45 | <50 | 18% | 5 to 10 |
| Dowd et al. [13] | 1998 | Harris Precoat | 154 | 70 | 13.6% | 6.3 |
| Kawate et al. [25] | 1999 | Harris Precoat | 55 | 67 | 5.5% | 8 |
| Sylvain et al. [35] | 2001 | Centralign Precoat | 84 | 61.4 | 11% | 2.9 |
| Ong et al. [28] | 2002 | Harris Design-2 | 192 | 59 | 4.16% | 13.5 |
| Ong et al. [28] | 2002 | Harris Precoat | 429 | 55 | 10% | 8.4 |
| Sanchez-Sotelo et al. [31] | 2002 | Harris Design-2 | 249 | 66 | 7% | 10 to 20 |
| Grose et al. [17] | In press | Spectron EF | 20 | 62 | 25% | 5.2 |
| Datir et al. [41] | 2005 | Harvard | 51 | 66 | 16% | 10 |
During the first three months of this study, the senior author implanted two other versions of the cemented VerSys femoral stem : one was collared, proximally textured, with a rough surface finish (Ra 1.4–2 μm), and the other was identical but with a satin finish (Ra 0.4–0.5 μm). They were implanted according to availability, with identical cementing techniques and with the same acetabular component (Trilogy). All patients have been followed up for a minimum of four years (range: 4 to 6.8), or until death or failure. The clinical results have been recently reported [15] and serve as a historical control. Among 64 rough VerSys stems, eight (12.5%) developed aseptic loosening to date. Among 138 satin VerSys stems, none developed aseptic loosening. The femoral bone cement interface revealed progressive radiolucent lines or osteolysis in ten of 64 rough stems (15.6%) and in three of 138 satin stems (2.2%).
In the current study, osteolysis occurred in four patients (7.2%) with well-fixed cemented femoral stems. In three of these patients, osteolysis could be related to the following factors: a proximal periprosthetic fracture compromising the cement integrity in one (Fig. 2a), the site of a previous core decompression in another (Fig. 3a), and accelerated polyethylene wear in the third. No clear explanation for the small osteolytic lesion in the fourth patient could be established.
Several authors have observed a communication of the stem–cement interface with the bone–cement interface in well-functioning and failed total hip replacements [22, 32]. Such communication can be present from the time of implantation, if the cement mantle is not circumferential and homogenous; or if there are cement voids [22], or cracks occuring before or after stem loosening [22, 36]. When such communication exists, osteolysis may develop [1, 23, 32]. Anthony et al. [1] described the flow of particle-loaded fluid at the stem–cement interface as a possible cause of femoral osteolysis in Exeter cemented femoral stems. He postulated that polyethylene loaded synovial fluid can flow at the stem–cement interface when there is no bond between the metal and the cement. In addition, in areas of incomplete cement mantle or at the site of cement cracks, the synovial fluid is forced by the cyclical local loads into the biological interface, generating osteolysis.
In conclusion, there were no mechanical failures in this series and in the satin historical controls. Despite the relatively small series presented in this study, these favourable results are significantly better than our experience with the rough VerSys stem, in which there were eight (12.5%) mechanical failures, requiring revision (p=0.03) (Table 4). We continue to follow up our patients prospectively to determine if the favourable mid-term results persist over time. Based on our experience [11, 15] and that of others (Tables 2 and 3), we believe that the surface finish of cemented femoral stems should be satin or polished.
Table 4.
Comparative analysis between the present study and our historic control groups
| Stem design | Ra (μm) | Number of hips | Average followup (years) | Osteolysis/radiolucent lines (number of cases and %) | Revisions for aseptic loosening (number of cases and %) | |
|---|---|---|---|---|---|---|
| Present study | VerSys CT | 0.05 | 54 | 6.1 | 4 (7.2%) | 0 (0%) |
| Historic control groups | VerSys Satin (25) | 0.4–0.5 | 138 | 5.2 | 3 (2.2%) | 0 (0%) |
| VerSys Rough (25) | 1.4–2 | 64 | 5.7 | 10 (15.6%) | 8 (12.5%) |
Footnotes
One or more of the authors has received research funding from the Zimmer Corp
References
- 1.Anthony PP, Gie GA, Howie CR, Ling RS. Localised endosteal bone lysis in relation to the femoral components of cemented total hip arthroplasties. J Bone Joint Surg Br. 1990;72:971–979. doi: 10.1302/0301-620X.72B6.2246300. [DOI] [PubMed] [Google Scholar]
- 2.Barrack RL, Mulroy RD, Jr, Harris WH. Improved cementing techniques and femoral component loosening in young patients with hip arthroplasty. A 12-year radiographic review. J Bone Joint Surg Br. 1992;74:385–389. doi: 10.1302/0301-620X.74B3.1587883. [DOI] [PubMed] [Google Scholar]
- 3.Berry DJ, Harmsen WS, Cabanela ME, Morrey BF. Twenty-five-year survivorship of two thousand consecutive primary Charnley total hip replacements: factors affecting survivorship of acetabular and femoral components. J Bone Joint Surg Am. 2002;84:171–177. doi: 10.2106/00004623-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Bishop NE, Ferguson S, Tepic S. Porosity reduction in bone cement at the cement-stem interface. J Bone Joint Surg Br. 1996;78:349–356. [PubMed] [Google Scholar]
- 5.Brady OH, Garbuz DS, Masri BA, Duncan CP. Classification of the hip. Orthop Clin North Am. 1999;30:215–220. doi: 10.1016/S0030-5898(05)70076-6. [DOI] [PubMed] [Google Scholar]
- 6.Callaghan JJ, Tooma GS, Olejniczak JP, Goetz DD, Johnston RC. Primary hybrid total hip arthroplasty: an interim followup. Clin Orthop. 1996;333:118–125. doi: 10.1097/00003086-199612000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Callaghan JJ, Albright JC, Goetz DD, Olejniczak JP, Johnston RC. Charnley total hip arthroplasty with cement. Minimum twenty-five-year follow-up. J Bone Joint Surg Am. 2000;82:487–497. doi: 10.2106/00004623-200004000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Callaghan JJ, Templeton JE, Liu SS, Pedersen DR, Goetz DD, Sullivan PM, Johnston RC. Results of Charnley total hip arthroplasty at a minimum of thirty years. A concise follow-up of a previous report. J Bone Joint Surg Am. 2004;86:690–695. doi: 10.2106/00004623-200404000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Charnley J. Arthroplasty of the hip. A new operation. Lancet. 1961;7187:1129–1132. doi: 10.1016/S0140-6736(61)92063-3. [DOI] [PubMed] [Google Scholar]
- 10.Charnley J. Fracture of femoral prostheses in total hip replacement. A clinical study. Clin Orthop. 1975;111:105–120. doi: 10.1097/00003086-197509000-00014. [DOI] [PubMed] [Google Scholar]
- 11.Comba F, Gonzalez Della Valle A, Salvati EA. The role of surface finish on the survivorship of cemented femoral stems for total hip arthroplasty. Minerva Ortopedica e Traumatologica. 2005;56:65–79. [Google Scholar]
- 12.Dall DM, Miles AW, Juby G. Accelerated polymerization of acrylic bone cement using preheated implants. Clin Orthop. 1986;211:148–150. [PubMed] [Google Scholar]
- 13.Dowd JE, Cha CW, Trakru S, Kim SY, Yang IH, Rubash HE. Failure of total hip arthroplasty with a precoated prosthesis. 4- to 11-year results. Clin Orthop. 1998;355:123–136. doi: 10.1097/00003086-199810000-00013. [DOI] [PubMed] [Google Scholar]
- 14.Fowler JL, Gie GA, Lee AJ, Ling RS. Experience with the Exeter total hip replacement since 1970. Orthop Clin North Am. 1988;19:477–489. [PubMed] [Google Scholar]
- 15.González Della Valle A, Zoppi A, Peterson MG, Salvati EA. A rough surface finish adversely affects the survivorship of a cemented femoral stem. Clin Orthop. 2005;436:158–163. doi: 10.1097/00003086-200507000-00024. [DOI] [PubMed] [Google Scholar]
- 16.González Della Valle A, Zoppi A, Peterson MG, Salvati EA. Clinical and radiographic results associated with a modern, cementless modular cup design in total hip arthroplasty. J Bone Joint Surg Am. 2004;86:1998–2003. doi: 10.2106/00004623-200409000-00019. [DOI] [PubMed] [Google Scholar]
- 17.Grose A, Gonzalez Della Valle A, Tomek I, Bullough P, Pellici P (2006) High failure rate of a proximally roughen cemented femoral stem for total hip arthroplasty. Int Orthop (in press) [DOI] [PMC free article] [PubMed]
- 18.Gruen TA, McNeice GM, Amstutz HC. “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop. 1979;141:17–27. [PubMed] [Google Scholar]
- 19.Harris WH, McGann WA. Loosening of the femoral component after use of the medullary-plug cementing technique. Follow-up note with a minimum five-year follow-up. J Bone Joint Surg Am. 1986;68:1064–1066. [PubMed] [Google Scholar]
- 20.Iesaka K, Jaffe WL, Kummer FJ. Effects of preheating of hip prostheses on the stem-cement interface. J Bone Joint Surg Am. 2003:;85:421–427. doi: 10.2106/00004623-200303000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Jasty M, Burke D, Harris WH. Biomechanics of cemented and cementless prostheses. Chir Organi Mov. 1992;77:349–358. [PubMed] [Google Scholar]
- 22.Jasty M, Jiranek W, Harris WH. Acrylic fragmentation in total hip replacements and its biological consequences. Clin Orthop. 1992;285:116–128. [PubMed] [Google Scholar]
- 23.Jasty MJ, Floyd WE, 3rd, Schiller AL, Goldring SR, Harris WH. Localized osteolysis in stable, non-septic total hip replacement. J Bone Joint Surg Am. 1986;68:912–919. [PubMed] [Google Scholar]
- 24.Johanson NA, Callaghan JJ, Salvati EA, Merkow RL. 14-year follow-up study of a patient with massive calcar resorption. A case report. Clin Orthop. 1986;213:189–196. [PubMed] [Google Scholar]
- 25.Kawate K, Ohmura T, Hiyoshi N, Natsume Y, Teranishi T, Tamai S. Thin cement mantle and osteolysis with a precoated stem. Clin Orthop. 1999;365:124–129. doi: 10.1097/00003086-199908000-00017. [DOI] [PubMed] [Google Scholar]
- 26.Malchau H, Herberts P, Eisler T, Garellick G, Soderman P. The Swedish total hip replacement register. J Bone Joint Surg Am. 2002;84(Suppl 2):2–20. doi: 10.2106/00004623-200200002-00002. [DOI] [PubMed] [Google Scholar]
- 27.Martens M, Aernoudt E, Meester P, Ducheyne P, Mulier JC, Langh R, Kestelijn P. Factors in the mechanical failure of the femoral component in total hip prosthesis. Report of six fatigue fractures of the femoral stem and results of experimental loading tests. Acta Orthop Scand. 1974;45:693–710. doi: 10.3109/17453677408989679. [DOI] [PubMed] [Google Scholar]
- 28.Ong A, Wong KL, Lai M, Garino JP, Steinberg ME. Early failure of precoated femoral components in primary total hip arthroplasty. J Bone Joint Surg Am. 2002;84:786–792. doi: 10.2106/00004623-200205000-00014. [DOI] [PubMed] [Google Scholar]
- 29.Parks ML, Walsh HA, Salvati EA, Li S. Effect of increasing temperature on the properties of four bone cements. Clin Orthop. 1998;355:238–248. doi: 10.1097/00003086-199810000-00025. [DOI] [PubMed] [Google Scholar]
- 30.Salvati EA, Wilson PD., Jr Long-term results of femoral-head replacement. J Bone Joint Surg Am. 1973;55:516–524. [PubMed] [Google Scholar]
- 31.Sanchez-Sotelo J, Berry GS, Harmsen S. Long-term results of use of a collared matte-finished femoral component fixed with second-generation cementing techniques. A fifteen-year-median follow-up study. J Bone Joint Surg Am. 1996;84:1636–1641. doi: 10.2106/00004623-200209000-00018. [DOI] [PubMed] [Google Scholar]
- 32.Schmalzried TP, Jasty M, Harris WH. Periprosthetic bone loss in total hip arthroplasty. Polyethylene wear debris and the concept of the effective joint space. J Bone Joint Surg Am. 1992;74:849–863. [PubMed] [Google Scholar]
- 33.Sharrock NE, Salvati EA. Hypotensive epidural anesthesia for total hip arthroplasty: a review. Acta Orthop Scand. 1996;67:91–107. doi: 10.3109/17453679608995620. [DOI] [PubMed] [Google Scholar]
- 34.Sporer SM, Callaghan JJ, Olejniczak JP, Goetz DD, Johnston RC. Hybrid total hip arthroplasty in patients under the age of fifty: a five- to ten-year follow-up. J Arthroplasty. 1998;13:485–491. doi: 10.1016/S0883-5403(98)90045-6. [DOI] [PubMed] [Google Scholar]
- 35.Sylvain GM, Kassab S, Coutts R, Santore R. Early failure of a roughened surface, precoated femoral component in total hip arthroplasty. J Arthroplasty. 2001;16:141–148. doi: 10.1054/arth.2001.20541. [DOI] [PubMed] [Google Scholar]
- 36.Willert HG, Ludwig J, Semlitsch M. Reaction of bone to methacrylate after hip arthroplasty: a long-term gross, light microscopic, and scanning electron microscopic study. J Bone Joint Surg Am. 1974;56:1368–1382. [PubMed] [Google Scholar]
- 37.Williams HD, Browne G, Gie GA, Ling RS, Timperley AJ, Wendover NA. The Exeter universal cemented femoral component at 8 to 12 years. A study of the first 325 hips. J Bone Joint Surg Br. 1999;84:324–334. doi: 10.1302/0301-620X.84B3.12261. [DOI] [PubMed] [Google Scholar]
- 38.Wroblewski BM, Fleming PA, Siney PD. Charnley low-frictional torque arthroplasty of the hip. 20-to-30 year results. J Bone Joint Surg Br. 1999;81:427–430. doi: 10.1302/0301-620X.81B3.9521. [DOI] [PubMed] [Google Scholar]
- 39.Wroblewski BM, Siney PD, Fleming PA. Triple taper polished cemented stem in total hip arthroplasty: rationale for the design, surgical technique, and 7 years of clinical experience. J Arthroplasty. 2001;16:37–41. doi: 10.1054/arth.2001.28374. [DOI] [PubMed] [Google Scholar]
- 40.Yates P, Gobel D, Bannister G. Collarless polished tapered stem: clinical and radiological follow-up over 5 years. J Arthroplasty. 2002;17:189–195. doi: 10.1054/arth.2002.30292. [DOI] [PubMed] [Google Scholar]
- 41.Datir SP, Wynn-Jones CH. Staged bilateral total hip arthroplasty using rough and smooth surface femoral stems with similar design. Acta Orthopaedica. 2005;76:809–814. doi: 10.1080/17453670510045417. [DOI] [PubMed] [Google Scholar]