Abstract
One hundred and eleven total knee replacements without patellar resurfacing were followed-up for a minimum of 48.8 months (range 48.8–108.2 months; average 78.2 months). Evaluation was performed using the Knee Society Clinical Rating System (KS-CRS). Preoperatively, the mean knee score was 34.3 points and the mean function score was 42.2 points. Postoperatively, this knee score improved to a mean of 91.1 points and the function score improved to mean of 89.6 points at the most recent follow-up. There were no significant differences among the knees with mild, moderate, or severe degenerative change to the patella with regard to the preoperative (p=0.83) and postoperative (p=0.39) knee pain score. It seems likely that the postoperative knee pain is not related to the severity of degenerative change to the patella in total knee arthroplasties performed without patellar resurfacing, and none of those patients required patellar resurfacing to achieve knee pain relief.
Résumé
Une série de 111 prothèse totales de genou sans resurfaçage patellaire a été suivi un minimum de 48 mois (de 48,8 à 108,2 mois avec une moyenne de 78,2 mois). L’évaluation a été faite selon le score clinique de la Knee Society (KS-CRS). Le score du genou est passé de 34,3 à 91,1 points et le score fonctionnel de 42,2 à 89,6 points entre l’état pré-opératoire et le plus récent recul. Il n’y avait pas de différence significative selon l’état dégénératif de la rotule. Il semble que les douleurs post-opératoires ne sont pas en relation avec l’atteinte de la rotule. Aucun des patients n’a eu besoin d’un resurfaçage rotulien en raison de douleurs du genou.
Introduction
Patellofemoral complications frequently compromise the outcome of total knee arthroplasies, which have a reported incidence of patellar complications ranging from 1 to 50% [3, 10, 16–20, 25, 26]. These complications have included osteonecrosis [22, 33, 36], patellar fracture [12, 17, 19–22, 28, 35–37, 39], component wear, loosening, and extensor mechanism problem [5, 7, 8] and chronic pain [5, 8, 9, 12, 23, 27, 31, 40].
Although some researchers concluded that resurfacing should be performed, others did not recommend its routine implementation [1, 3, 11, 31].
Complications related to patellar resurfacing have revived interest in performing the procedure without resurfacing.
Postoperative anterior knee pain is probably clinically important, but the aetiology is often unclear. A review of the literature reveals that the prevalence of patellofemoral pain when the patella was not resurfaced ranged between 5 and 45%, but these studies were usually retrospective and described implants poorly designed to deal with the patellofemoral joint. Anterior knee pain is related to component design or to details of the surgical technique, such as component rotation, rather than to whether or not the patellar is resurfaced [5, 40].
Herein, we report the results of a randomised, prospective study of 111 knees replaced with the NexGen prosthesis with no resurfacing of the patella that were followed for a minimum of 4 years. The Nex-Gen femoral component has a deep patellar groove and a smoother femoral surface with a curved anterolateral flange surface to provide full support of the lateral patellar facet. The secondary purpose of this study was to determine whether there was any correlation between the degree of severity of degenerative change in the patella and anterior knee pain.
Materials and methods
Between February 1995 and March 2000, 142 total knee arthroplasties (NexGen, Zimmer, Warsaw, IN, USA) were performed without patellar resurfacing in 89 patients. The NexGen femoral component has a slightly smaller intercondylar notch and also has a smoother femoral surface with a curved anterolateral flange surface to provide full support of the lateral patellar facet (Fig. 1). Of these, 31 knees (21 patients) were lost to follow-up, leaving 111 knees (68 patients) for review at a minimum 4 years’ follow up. All the operations were performed by a single surgeon (I.S.O.) and patellar resurfacing was not performed, regardless of the state of the patellar articular cartilage.
Fig. 1.
This photograph shows the Nex-Gen femoral component. The patellar groove is deepened and extended further posteriorly. The lateral femoral flange surface was extended further to provide full support of the lateral patellar facet
The mean duration of follow-up was 78.2 months (range 48.8–108.2). There were 8 men and 60 women, with an average age of 68.3 years (range 59.2–80.6) at the time of operation. There were 42 right knees and 69 left knees. The diagnosis was degenerative arthritis in 98 knees, rheumatoid arthritis in 10 knees, and avascular necrosis in 3 knees.
Pre- and postoperative evaluations were performed using the Knee Society Clinical Rating System (KS-CRS) [16, 23, 24], which assesses knee score and patient function score separately. The KS-CRS uses only three main parameters in assessing the knee score: pain, stability, and range of motion. Flexion contracture, extension lag, and malalignment cause deductions to be made from the scores. A well-aligned knee with no pain, 125° of motion, and negligible anteroposterior and mediolateral instability would score 100 points. The patient functional score takes into consideration only walking distance and stair climbing, with deductions made for use of walking aids. Patients who can walk unlimited distances and go up and down stairs normally score 100 points.
We used a simple clinical anterior knee pain rating, which indicated whether anterior knee pain was present (Table 1) [40].
Table 1.
Clinical anterior knee pain rating
| Rating | Description |
|---|---|
| I | Mild pain that does not intrude on daily activities |
| II | Moderate pain that is a nuisance; patient not considering further surgery |
| III | Severe pain; patient considering further surgery |
Postoperative anterior knee pain was assessed without knowledge of the severity of the degenerative change to the patella.
The degenerative condition of the patellar cartilage at the time of operation was classified using a visual grading system as “mild,” “moderate,” or “severe.” “Mild” degeneration was defined as the presence of cartilage softening, “moderate” as the presence of fibrillation and erosion less than 1 cm in diameter, and “severe” as the presence of exposed bone greater than 1 cm in diameter. The degrees of patellar cartilage degeneration in our study group were classified as “mild” to “moderate” (58 knees) and “severe” (53 knees). At the time of operation, osteophytes were removed and fibrillated cartilage smoothed, in the 53 severely involved patellae, but no other treatment was performed on the exposed subchondral bones of the patellae. In moderate cases, only smoothing of fibrillated cartilage was performed. In mild cases, neither osteophyte removal nor cartilage smoothing was performed. We debrided the parapatellar synovium in moderate and severe degenerative changes to the patella using the knife to excise the hypertrophied synovium and the patellofemoral tracking was assessed intraoperatively in all of the knees.
We assessed preoperative and postoperative anterior knee pain scores between mild to moderate and severe degenerative changes to the patellae using the KS-CRS system. The ability to climb stairs and to rise from a chair were specifically assessed, as was the presence or absence of anterior knee pain as a means of identifying symptoms related to the patella.
Statistical analysis was performed using the SPSS for Windows statistical package (version 10.0).
The Student’s t test was used to analyse differences between the knees with mild to moderate and severe degenerative changes in the patella with regard to the pre- and postoperative anterior knee pain score.
Results
Knee society clinical score
At follow-up (mean 78.2 months, range 48.8–108.2), none of the 111 cases of total knee replacement arthroplasty without patellar resurfacing had any patellar complications such as fracture, dislocation, subluxation or rupture of the patellar tendon. However, there were three cases with complications: one case of infection and two cases of supracondylar fracture of the femur. The infection was caused by staphylococcus aureus and developed 1 year postoperatively. It was treated with debridement, component retention, and parenteral antibiotics. The two cases of supracondylar fracture of the femur occurred due to injuries from falls during the 4th month and the 17th month postoperatively, and were treated by intramedullary fixation of the fracture.
According to the KS-CRS preoperative knee evaluations, 3 knees (2.7%) scored 60–69 points, 11 (9.9%) scored 50–59 points, 21 (18.9%) scored 40–49 points, 30 (27.0%) scored 30–39 points, 26 (23.4%) scored 20–29 points, 12 (10.8%) scored 10–19 points, and 8 (7.2%) scored 0–9 points. The mean preoperative knee score was 34.3 points (range 5.6–63.2). In the postoperative knee evaluations, 48 knees (43.2%) scored 90–100 points, 51 (45.9%) scored 80–89 points, 9 (8.1%) scored 70–79 points, and 3 (2.7%) scored 60–69 points. The mean postoperative knee score was 91.1 points (range 65.5–98.3). In the preoperative function evaluations, 3 knees (2.7%) scored 60–69 points, 4 (3.6%) scored 50–59 points, 50 (45.0%) scored 40–49 points, 44 (39.6%) scored 30–39 points, 7 (6.3%) scored 20–29 points, and 3 (2.7%) scored 10–19 points. The mean preoperative function score was 42.2 points (range 10.6–61.3). In the postoperative patient function evaluations, 55 knees (49.5%) scored 90–100 points, 46 (41.4%) scored 80–89 points, 8 (7.2%) scored 70–79 points, and 2 (1.8%) scored 60–69 points. The mean postoperative patient function score was 89.6 points (range 63.2–100.0).
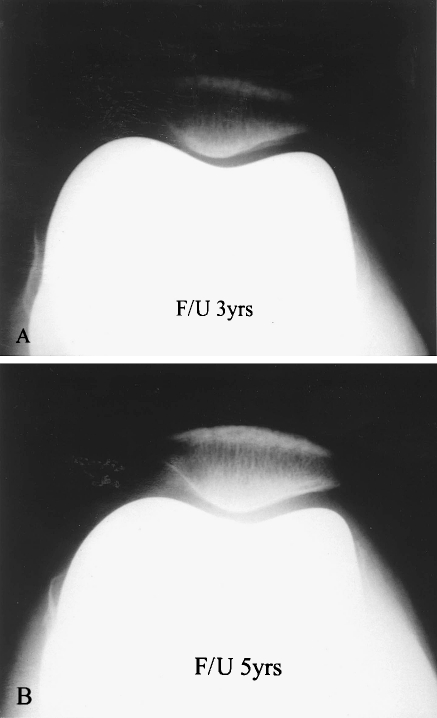
The patellofemoral joints were radiographically observed at the time of follow-up examination (mean duration of follow-up was 78.2 months) using the Merchant view; there were no gross findings of misalignment, dislocation or subluxation of the patellae. The patellofemoral joint spaces were well preserved, based on radiographs taken postoperatively; at 1 year in 111 cases, at 3 years in 93 cases, and at 5 years in 88 cases. These results reflect the preservation of cartilage integrity and the fact that the lateral patellar facet is well supported (Fig 2).
Fig. 2.
The patellofemoral joint was well preserved based on radiographs at a 3 and b 5 years’ follow-up and the lateral patellar facet is well supported
Knee pain score
According to the KS-CRS: 50 points are allotted for no pain, 45 points for mild or occasional pain, 40 points for pain on stairs only, 30 points for pain when walking and on stairs, 20 points for moderate occasional pain, 10 points for continual pain, and 0 points for severe pain.
The mean preoperative pain score was 10.0 points, but at the time of follow-up the mean postoperative pain score was 47.9 points.
Eighty-five knees (76.5%) were not painful, 12 (10.8%) were mildly or occasionally painful, 11(9.9%) were painful on stairs only, and 3 (2.7%) were painful when walking and on stairs, and none was moderately or severely painful at the time of follow-up examination.
The mean preoperative pain score was 9.8 points in 53 cases of severe degenerative changes to patellae. The mean preoperative pain score was 10.2 points in 58 cases of mild to moderate degenerative changes to patellae. There was no statistical difference in the mean preoperative pain score between the knees with mild to moderate degenerative changes to the patellae and those with severe degenerative changes to the patellae (p=0.83).
The mean postoperative pain score was 47.5 points in 53 severe cases of degenerative changes in the patellae and the mean postoperative pain score was 48.3 points in 58 mild to moderate cases of degenerative changes in the patellae. There was also no significant difference in the mean postoperative pain score between the knees with mild to moderate degenerative changes to the patellae and those with severe degenerative changes in the patellae (p=0.39).
Anterior knee pain
The overall prevalence of anterior knee pain was 11.7% (13 out of 111 knees; Table 2).
Table 2.
Anterior knee pain rating (number of knees)
| Severe (53 knees) | Mild to moderate (58 knees) | Prevalence of anterior knee pain (%) | |
|---|---|---|---|
| Grade I (mild) | 3 | 4 | 6.3 |
| Grade II (moderate) | 4 | 2 | 5.4 |
| Grade III (severe) | 0 | 0 | 0 |
| Percentage | 12.1 | 11.3 |
According to the clinical anterior knee pain score [40], 7 knees (6.3%) were grade I, 6 (5.4%) were grade II, and none was grade III. None of the patients underwent further surgery to the patellofemoral joint with patellar resurfacing.
The prevalence of anterior knee pain in the 53 knees with severe degenerative changes in the patella was 12.1% (7 out of 53 knees) and the pain in the 58 mild to moderate degenerative changes was 11.3% (6 out of 58 knees).
Four knees (6.9%) with mild to moderate degenerative changes at the time of surgery had mild anterior knee pain and 2 (3.4%) with mild to moderate changes had moderate anterior knee pain. None of those with mild to moderate changes had severe anterior knee pain.
Three knees (5.6%) with severe changes had mild anterior knee pain and 4 knees (7.5%) with severe changes had moderate anterior knee pain. None of those with severe changes had severe anterior knee pain.
There was no significant difference between the mild to moderate and severe degenerative changes in the patella with regard to the anterior knee pain (p=0.73).
Range of movement
The mean preoperative flexion contracture was 8° (range 0∼20°) in the mild to moderate group and 12° (range 0∼35°) in the severe group, and the mean preoperative flexion was 122° ( range 100∼130°) in mild to moderate group and 118° (range 95∼140°) in the severe group.
The mean postoperative flexion contracture was 2° (range 0∼5°) in the mild to moderate and severe groups, and the mean postoperative flexion was 120° (range 95∼130°) in the mild to moderate group and 116° (range 90∼135°) in the severe group.
There was no statistical significance in the mean postoperative flexion between the mild to moderate and the severe degenerative changes in the patella (p=0.095).
Walking
Preoperatively, 15 knees (13.5%) were not able to walk, 56 knees (50.5%) could walk a distance of less than one block, 22 knees (19.8%) could walk one to five blocks, and 18 knees (16.2%) could walk five to ten blocks. Postoperatively, 103 knees (92.8%) could walk an unlimited distance without pain, five (4.5%) could walk more than ten blocks without pain, and three (2.7%) could walk five to ten blocks without pain.
Discussion
Possible patellar complications following total knee replacement arthroplasty include osteonecrosis, fracture [12, 17, 19–21, 28, 35–39], subluxation [12, 29], patellofemoral instability [4, 6–8, 10, 18], rupture of the quadriceps or patellar tendons [3, 15, 20, 28, 32], patellar component failure [12, 22, 23, 28, 36], soft tissue impingement [7], patellar pain [4, 8, 9, 12, 27, 31], and malrotation of the femoral or tibial component [2, 11, 30, 39]. The reported rates of these complications have ranged from 1 to 50% when patellar resurfacing is performed [3, 10, 11, 17–21, 25, 26, 30, 34].
It seems clear that anterior knee pain remains an important clinical issue following total knee arthroplasty.
Barrack et al. [5] reported that anterior knee pain will develop postoperatively regardless of whether patellar resurfacing is performed. In osteoarthritic knees without patellar resurfacing, Insall et al. reported patellofemoral pain in 6 out of 33 knees (18.2%) and a decreased clinical score [23]. Barrack et al. also reported that there was no significant difference between the groups treated with or without resurfacing with regard to the overall Knee Society score or the pain and function subscores, and suggested that postoperative anterior knee pain is related to the component design or to details of the surgical technique, such as component rotation, rather than to whether or not the patella is resurfaced [4, 5].
Unresurfaced patellae function well over 10 years when applied to a femoral surface that is designed to minimize articular pressure, but they function poorly when applied to a femoral component with a high, wide intercondylar notch and a shallow patellar groove [40].
Soudry et al. [38] also found no correlation between cartilage integrity and the degree of pain, with 82% of patients denying any patellofemoral pain at all. Patellofemoral pain syndromes are derived from cartilage degeneration and from soft tissue change, including tendinitis [12, 13]. These authors concur with Soudry et al. [38], finding no correlation between patellar erosion seen intraoperatively and patellar pain in the non-resurfaced patellae. Whiteside [41] also reported that with appropriate femoral surface contours, patellofemoral function can be excellent, with the unresurfaced patella articulating against the smooth metal component, and found no relationship between the severity of patellar wear found at the time of surgery and the incidence of anterior knee pain. In our prospective study of patients treated with the NexGen prosthesis, the incidence of anterior knee pain in knees without patellar resurfacing was not related to the severity of degenerative changes to the patella.
Furthermore, in our total knee arthroplasties without patellar resurfacing, revision surgery was not required for the treatment of chronic patellar pain in any of our cases.
In 111 cases of total knee arthroplasties without patellar resurfacing, the mean postoperative knee score was 91.1 points (range 65.5–98.3) and the mean postoperative function score was 89.6 points (range 63.2–100.0), according to the KS-CRS system. There were no patellar complications, in contrast to total knee arthroplasty with patellar resurfacing, which has a reported complication rate of 4% [10]. The authors conclude that routine patellar resurfacing provides no advantage, and in fact leads to more complications than not resurfacing the patella. Our results also indicate that there is no correlation between the severity of degenerative changes in the patella and anterior knee pain.
Conclusions
According to the KS-CRS system, the mean preoperative knee score was 34.3 points and the mean postoperative score was 91.1 points. The mean preoperative function score was 42.2 points and the mean postoperative function score was 89.6 points.
Knee pain after total knee arthroplasty without patellar resurfacing was not correlated with the severity of degenerative changes in the patella, and the pain was so mild that none of those patients required patellar resurfacing to achieve pain relief. Patellar complications that can occur in a resurfaced patella were completely avoided.
The authors have found that the patellofemoral joint can function without patellar resurfacing.
Acknowledgement
This work was supported by an INHA University Research Grant.
References
- 1.Abraham W, Buchanan JR, Daubert H, Greer RB, III, Keefer J. Should the patella be resurfaced in total knee arthroplasty? Clin Orthop Relat Res. 1988;236:128–134. [PubMed] [Google Scholar]
- 2.Anouchi YS, Whiteside LA, Kaiser AD, Milliano MT. The effects of axial rotational alignment of the femoral component on knee stability and patellar tracking in total knee arthroplasty demonstrated on autopsy specimens. Clin Orthop Relat Res. 1993;287:170–177. [PubMed] [Google Scholar]
- 3.Arciero RA, Toomey HE. Patellofemoral arthroplasty. Clin Orthop Relat Res. 1988;236:60–71. [PubMed] [Google Scholar]
- 4.Barrack RL, Wolfe MW, Waldman DA, Milicic M, Bertot AJ, Myers L. Resurfacing of the patella in total knee arthroplasty. J Bone Joint Surg Am. 1997;79:1121–1131. doi: 10.2106/00004623-199708000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Barrack RL, Bertot AJ, Wolfe MW, Waldman DA, Milicic M, Myers L. Patellar resurfacing in total knee arthroplasty. J Bone Joint Surg Am. 2001;83-A:1376–1381. [PubMed] [Google Scholar]
- 6.Bayne O, Cameron HU. Total knee arthroplasty following patellectomy. Clin Orthop Relat Res. 1984;186:112–114. [PubMed] [Google Scholar]
- 7.Beight JL, Yao B, Hozack WJ, Hearn SL, Booth RE., Jr The patellar “Clunk” syndrome after posterior stabilized total knee arthroplasty. Clin Orthop Relat Res. 1994;299:139–142. [PubMed] [Google Scholar]
- 8.Bindelglass DF, Cohen JL, Dorr LD. Patellar tilt and subluxation in total knee arthroplasty. Clin Orthop Relat Res. 1993;286:103–109. [PubMed] [Google Scholar]
- 9.Bourne RB, Rorabeck CH, Kramer J, Hardie R, Robertson D. Resurfacing versus not resurfacing the patella during total knee replacement. Clin Orthop Relat Res. 1995;321:156–161. [PubMed] [Google Scholar]
- 10.Boyd AD, Ewald FC, Thomas WH, Poss R, Sledge CB. Long-term complications after total knee arthroplasty with or without resurfacing of the patella. J Bone Joint Surg Am. 1993;75:674–681. doi: 10.2106/00004623-199305000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Brick GW, Scott RD. The patellofemoral component of total knee arthroplasty. Clin Orthop Relat Res. 1988;231:163–178. [PubMed] [Google Scholar]
- 12.Cameron HU, Fedorkow DM. The patella in total knee arthroplasty. Clin Orthop Relat Res. 1982;165:197–199. [PubMed] [Google Scholar]
- 13.Chrisman OD. The role of articular cartilage in patellofemoral pain. Orthop Clin North Am. 1986;17:231–234. [PubMed] [Google Scholar]
- 14.Clayton ML, Thirupathi R. Patellar complication after total condylar arthroplasty. Clin Orthop Relat Res. 1982;170:152–155. [PubMed] [Google Scholar]
- 15.Emerson RH, Jr, Head WC, Malinin TI. Reconstruction of patellar tendon rupture after total knee arthroplasty with an extensor mechanism allograft. Clin Orthop Relat Res. 1990;260:154–161. [PubMed] [Google Scholar]
- 16.Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;248:9–12. [PubMed] [Google Scholar]
- 17.Goldberg VM, Figgie HE, III, Inglis AE, Figgie MP, Sobel M, Kelly M, Kraay M. Patellar fracture type and prognosis in condylar total knee arthroplasty. Clin Orthop Relat Res. 1988;236:115–122. [PubMed] [Google Scholar]
- 18.Grace JN, Rand JA. Patellar instability after total knee arthroplasty. Clin Orthop Relat Res. 1988;237:184–189. [PubMed] [Google Scholar]
- 19.Grace JN, Sim FH. Fracture of the patella after total knee arthroplasty. Clin Orthop Relat Res. 1988;230:168–175. [PubMed] [Google Scholar]
- 20.Healy WL, Wasilewski SA, Takei R, Oberlander M. Patellofemoral complication following total knee arthroplasty: correlation with implant design and patient risk factors. J Arthroplasty. 1995;10:197–201. doi: 10.1016/S0883-5403(05)80127-5. [DOI] [PubMed] [Google Scholar]
- 21.Hozack WJ, Goll SR, Lotke PA, Rothman RH, Booth RE., Jr The treatment of patellar fractures after total knee arthroplasty. Clin Orthop Relat Res. 1988;236:123–127. [PubMed] [Google Scholar]
- 22.Hsu HP, Walker PS. Wear and deformation of patellar components in total knee arthroplasty. Clin Orthop Relat Res. 1989;246:260–265. [PubMed] [Google Scholar]
- 23.Insall JN, Ranawat CS, Aglietti P, Shine J. A comparison of four models of total knee-replacement prostheses. J Bone Joint Surg Am. 1976;58:754–765. [PubMed] [Google Scholar]
- 24.Insall JN, Dorr Lawrence DD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 25.Kayler DE, Lyttle D. Surgical interruption of patellar blood supply by total knee arthroplasty. Clin Orthop Relat Res. 1988;229:221–227. [PubMed] [Google Scholar]
- 26.Keblish PA, Varma AK, Greeneald AS. Patellar resurfacing or retention in total knee arthroplasty. A prospective study of patients with bilateral replacements. J Bone Joint Surg Br. 1994;76:930–937. [PubMed] [Google Scholar]
- 27.Levai JP, McLeod HC, Freeman MA. Why not resurface the patella? J Bone Joint Surg Br. 1983;65:448–451. doi: 10.1302/0301-620X.65B4.6874718. [DOI] [PubMed] [Google Scholar]
- 28.Lombardi AV, Jr, Engh GA, Voltz RG, Albrigo JL, Virginia A, Brainard BJ. Fracture/dissociation of the polyethylene in metal-backed patellar components in total knee arthroplasty. J Bone Joint Surg Am. 1988;70:675–679. [PubMed] [Google Scholar]
- 29.Mochizuki RM, Schurman DJ. Patellar complications following total knee arthroplasty. J Bone Joint Surg Am. 1979;61:879–883. [PubMed] [Google Scholar]
- 30.Nagamine R, Whiteside LA, White SE, McCarthy DS. Patellar tracking after total knee arthroplasty. Clin Orthop Relat Res. 1994;304:262–271. [PubMed] [Google Scholar]
- 31.Picetti GD, III, McGann WA, Welch RB. The patellofemoral joint after total knee arthroplasty without patellar resurfacing. J Bone Joint Surg Am. 1990;72:1379–1382. [PubMed] [Google Scholar]
- 32.Rand JA, Morrey RF, Bryan RS. Patellar tendon rupture after total knee arthroplasty. Clin Orthop Relat Res. 1986;244:233–238. [PubMed] [Google Scholar]
- 33.Reuben JD, McDonald CL, Woodard PL, Hennington LJ. Effect of patella thickness on patella strain following total knee arthroplasty. J Arthroplasty. 1991;6:251–258. doi: 10.1016/s0883-5403(06)80172-5. [DOI] [PubMed] [Google Scholar]
- 34.Ritter MA, Campbell ED. Postoperative patellar complications with or without lateral release during total knee arthroplasty. Clin Orthop Relat Res. 1987;219:163–168. [PubMed] [Google Scholar]
- 35.Roffman M, Hirsh DM, Mendes DG. Fracture of the resurfaced patella in total knee replacement. Clin Orthop Relat Res. 1980;148:112–116. [PubMed] [Google Scholar]
- 36.Rosenberg AG, Andriacchi TP, Barden R, Galante JO. Patellar component failure in cementless total knee arthroplasty. Clin Orthop Relat Res. 1988;236:106–114. [PubMed] [Google Scholar]
- 37.Scott RD, Turoff N, Ewald FC. Stress fracture of the patella following duopatellar total knee arthroplasty with patellar resurfacing. Clin Orthop Relat Res. 1982;170:147–151. [PubMed] [Google Scholar]
- 38.Soudry M, Mestriner LA, Binazzi R, Insall JN. Total knee arthroplasty without patellar resurfacing. Clin Orthop Relat Res. 1986;205:166–170. [PubMed] [Google Scholar]
- 39.Tria AJ, Harwood DA, Alicea JA, Cody RP. Patellar fractures in posterior stabilized knee arthroplasties. Clin Orthop Relat Res. 1994;299:131–138. [PubMed] [Google Scholar]
- 40.Waters TS, Bentley G. Patellar resurfacing in total knee arthroplasty. J Bone Joint Surg Am. 2003;85:212–217. doi: 10.2106/00004623-200302000-00005. [DOI] [PubMed] [Google Scholar]
- 41.Whiteside LA, Nakanwra T. Effect of femoral component design on unresurfaced patellas in knee arthroplasty. Clin Orthop Relat Res. 2003;410:189–198. doi: 10.1097/01.blo.0000063605.67412.4d. [DOI] [PubMed] [Google Scholar]