Abstract
We studied the relationship between stem subsidence and improvement in the initial radiolucency at the bone–cement interface in polished- and rough-surface stems. Stem subsidence was seen in 34 of 42 hips (81.0%), and improvement in the initial radiolucency was seen in 15 hips (35.7%) in collarless polished tapered stems at 1 year after operation. In polished stems, stem subsidence in cases with improvement in the initial radiolucency was significantly greater than in those with no change (average 1.12 mm and 0.48 mm, P<0.005). In rough-surface stems partially coated with polymethylmethacrylate (VerSys Cemented Plus), no stem subsidence and no improvement in the initial radiolucency was seen. In polished stems, stem subsidence leads to cement creep and compressive force on the bone–cement interface and can improve the initial radiolucency.
Résumé
Nous avons étudié les relations entre la migration de la pièce fémorale et l’augmentation des liserés à l’interface ciment-os lors de la mise en place de prothèse fémorale avec une pièce fémorale soit polie, soit rugueuse. La migration de la pièce fémorale a été observée dans 34 des 42 hanches (81%) et l’aggravation du liseré dans 15 hanches (35,7%) dans les pièces fémorales polies (CPT) à un an post opératoire. La migration de la pièce fémorale est beaucoup plus importante dans les cas où le liseré est important si on le compare aux pièces fémorales polies sans migration (moyenne de migration entre 1,12 et 0,48 mm, P<0,005). Lorsque la pièce fémorale est rugueuse avec un ciment polyméthylmethacrylate (VerSys Cemented Plus), il n’y a pas de migration de la queue et pas d’aggravation des liserés Les pièces fémorales polies avec migration de la queue entraînent un fluage du ciment et des forces de compression à l’interface ciment-os qui peuvent être la cause d’aggravation dans l’apparition des liserés.
Introduction
Studies have reported that polished-surface stems provide better long-term survival than the same design of rough-surface stems in cemented femoral implants such as Exeter, T-28, and Iowa stems [4, 5, 11, 18]. However, the reason for better survival is unknown. In polished-surface tapered stems, stem subsidence into cement without cement destruction or loosening is often reported [1, 5, 7, 18]. In addition, Wroblewski et al. have described that the cement-bone interface of the femur in a polished tapered stem showed progressive improvement, with the cancellous bone taking on a more dense appearance, indicating proximal load transfer, in 20% of cases [17]. Improvement in the radiolucency is considered to be a good sign in contrast to stem loosening, and elucidation of this mechanism may lead to improved long-term survival of polished stems. In this study, we investigated the relationship between stem subsidence and improvement in the initial radiolucency in polished tapered stems at early term within 1 year of operation compared with rough-surface stems.
Materials and methods
We reviewed the cases that had undergone primary total hip arthroplasty (THA) using collarless polished tapered (CPT) stems (Zimmer, Warsaw, IN, USA) and VerSys Cemented Plus (VerSys) stems. A CPT stem has a highly polished double-tapered surface. A VerSys stem has a collar and different geometry from the CPT stem, with a tapered rough surface coated with polymethylmethacrylate (PMMA) on the upper one-third of the stem.
Subjects for the CPT group were 42 consecutive hips in 38 patients in a series. In this group, seven patients representing seven hips were male, and 31 patients representing 35 hips were female. The patients' ages at surgery ranged from 51 to 79 years (average 69.1). Their heights ranged from 135 to 168 cm (average 148.4) and their weights from 42 to 68 kg (average 53.1). The diagnoses were osteoarthritis (OA) secondary to developmental dysplasia of the hip (DDH) in 26 hips, degenerative joint disease (DJD) with less deformity of the femoral head and neck in eight hips, osteonecrosis of the femoral head (ONF) in four hips, post-traumatic OA in two hips, rheumatoid arthritis (RA) in two hips, and rapidly destructive arthrosis in one hip. The sizes of the CPT stems were number 0 in 19 hips, number 1 in 20 hips, and numbers 2, 3, and 4 in one hip each. According to the classification of Barrack et al. [2], the cementing grades were grade A in 13 hips, B in 18, C-1 in five, C-2 in six, and D in none.
Subjects for the VerSys group were 36 consecutive hips in 31 patients in a series. In this group, two patients representing two hips were male, and 29 patients representing 34 hips were female. The patients' ages at surgery ranged from 57 to 81 years (average 70.5). Their heights ranged from 133 to 172 cm (average 148.3) and their weights from 36 to 76 kg (average 49.3). The diagnoses were OA secondary to DDH in 21 hips, DJD in three hips, ONF in two hips, post-traumatic OA in two hips, RA in seven hips, and rapidly destructive arthrosis in one hip. The cementing grades were grade A in eight hips, B in 11, C-1 in 12, C-2 in five, and D in none.
Although the patients' weights were heavier in the CPT group, there was no significant difference in height, gender, diagnoses, or cementing grades between the two groups. All cases in both groups had poor quality of the femoral bone because of osteoporosis due to aging or underlying diseases. The acetabular cups were fixed without cement in all cases. Trilogy cups (Zimmer, Warsaw, IN, USA) were used for all cases in the CPT group and for 15 hips in the VerSys group, and Harris/Galante Porous II cups (Zimmer, Warsaw, IN, USA) were used in 19 hips in the VerSys group. Two or three screws were used to fix the cup in all cases. A 26-mm zirconia ceramic head was used in all cases. Simplex-P cement (Stryker Howmedica Osteonics, Allendale, NJ, USA) was used in eight hips in the VerSys group, and CMW Endurance cement (DePuy International, Blackpool, UK) was used in the other hips. The cement was mixed under negative pressure and delivered with a cement gun. Using a bone plug, the cement was compressed manually.
After the drain was removed, patients started walking with a walker or cane within the limits of pain. There was no infection in either group. One patient in the VerSys group fell whilst walking and had dislocation of the hip, but that happened only once. There were no complications such as ectopic ossification or pulmonary embolism.
The follow-up observations were available over more than 1 year after operation in all cases. Postoperative stem subsidence and changes in the radiolucency were reviewed using the anteroposterior views of three X-rays taken within 2 months and at 6 months and 1 year after operation. The X-rays were taken in a uniform manner at one institution, and the rotational angles of the X-ray films selected for evaluation were confirmed to be almost equivalent. The change in the initial radiolucency at the cement–bone interface was judged by two orthopaedic surgeons as one of three categories: improvement, no change, and spread on each zone, as described by Gruen et al. [6] (Fig. 1). Improvement in the radiolucency at the cement–bone interface was defined as blurring or fading of a slight radiolucent line between the cement and the femoral inner cortex seen in the X-ray taken within 2 months of operation. The measurement of stem subsidence was taken by digitizing X-ray images and measuring the distance from the top of the greater trochanter to the top of the stem and calibrating the data by the femoral head along the lines of Braud and Freeman [3]. This measurement was performed by an orthopaedic surgeon who did not judge improvement of radiolucency and was unaware of the study's purpose. The statistical analysis was performed using t-tests.
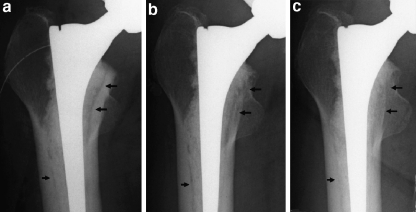
Fig. 1.
Initial radiolucency was seen on X-ray immediately after surgery (a) at zones 2 and 7 (black arrows). Radiolucency gradually reduced with the time course on X-rays at 6 months (b) and 1 year (c) after surgery. These findings were judged as improvement of the initial radiolucency
Results
The average Harris hip score rose from 40.1 points preoperatively to 86.4 points 1 year postoperatively in the CPT group, and from 39.6 to 86.6 in the VerSys group. There was no significant difference between the two groups. In the CPT group, stem subsidence was seen in 34 hips of 31 cases (81.0%) and averaged 0.72 mm (range 0.00–2.52 mm) at 1 year after operation. Twenty-four hips had subsidence within 1 mm, seven hips with 1–2 mm, and three hips with 2–3 mm. On the other hand, in the VerSys group, there was no case of measurable stem subsidence except for one case showing mechanical failure. Improvement in the initial radiolucency was seen in 15 hips (35.7%) in the CPT group and none in the VerSys group (Fig. 2). In 13 hips of 15 cases (86.7%) with improvement in the radiolucency in the CPT group, this finding was observed 6 months after operation. In the other two hips, improvement was seen at 1 year after operation.
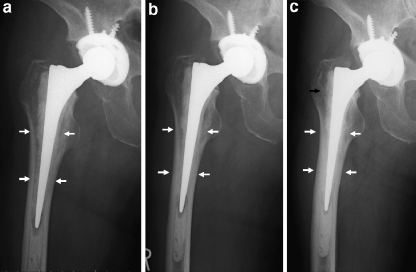
Fig. 2.
A 70-year-old woman with stem subsidence and decrease in the initial radiolucency. Initial radiolucency on the X-ray at 1 month after operation (a; white arrows) had already decreased at 6 months after operation (b) with stem subsidence. Stem subsidence of 2.52 mm had occurred by 1 year after operation (c), and radiolucency decreased more at zones 2, 3, 5, and 6. In addition, the border of cement and cancellous bone at zone 1 became indistinct (black arrow)
Spread in the radiolucency was observed in one hip each in both groups. In the VerSys group, the case showing spread had a stem debonding from the cement in zone 1 and cement cracking in zone 2, and was therefore considered to be due to mechanical failure. This was the only case of stem subsidence in the VerSys group, with 0.65 mm at 1 year and 3.54 mm at 3 years after surgery. In the CPT group, the case of spread in radiolucency showed that the radiolucency cleared slightly at the 6-month X-ray compared with the X-ray taken immediately postoperatively; however, there was no further expansion of the radiolucency on the X-ray film at 1 year after operation. No cement cracking was considered as loosening. No change in the radiolucency was seen in the other 26 hips (61.9%) in the CPT group or 35 hips (97.2%) in the VerSys group.
The average stem subsidence in the cases with improvement in radiolucency was 1.12 mm (range 0.46–2.52), and in the cases with no change it was 0.48 mm (range 0.00–1.91). Stem subsidence was significantly greater in the cases with improvement in the initial radiolucency (P<0.005; Table 1). Improvement in the initial radiolucency was seen in three, three, five, four, seven, two, and nine hips in zones 1 to 7, respectively, and more frequently in the medial side, such as zones 5 and 7 (Table 2). Improvement in the radiolucency was seen in more than two zones in eight of 15 hips. The frequency in each diagnosis was five of 26 hips (19.2%) with OA secondary to DDH, five of seven hips (71.4%) with DJD, four of four hips (100%) with ONF, and one of two hips (50%) with post-traumatic OA. There was no significant difference in improvement in the initial radiolucency with regard to other factors such as height, weight, stem size, cup size, neck length, cement type, and cementing grade.
Table 1.
Radiolucency and stem subsidence in collarless polished tapered stem group
| Radiolucency | |||
|---|---|---|---|
| No change | Improvement | P-value | |
| Hips (n) | 26 | 15 | |
| % | 61.9 | 35.7 | |
| Stem subsidence (mm)a | 0.48±0.49 | 1.12±0.69 | <.005 |
aValues are average ± standard deviation
Table 2.
Improvement in the initial radiolucency at each zone according to Gruen et al. [6]
| Zone | Number | % |
|---|---|---|
| 1 | 3 | 20.0 |
| 2 | 3 | 20.0 |
| 3 | 5 | 33.3 |
| 4 | 4 | 26.7 |
| 5 | 7 | 47.7 |
| 6 | 2 | 13.3 |
| 7 | 9 | 60.0 |
Percentages are calculated by number in each zone divided by 15, the total number of improvement in the initial radiolucency
Discussion
Progressive development of radiolucent lines around the stem in THA is generally considered a sign of implant failure. Therefore, if development of radiolucency could be prevented, mechanical implant failure also could be prevented. For this purpose, it is better to reduce the shear stress between the bone and cement and to increase the horizontal compressive stress. With its geometric properties, a polished tapered stem is likely to distribute the vertical stress caused by load in the horizontal direction and to increase the compressive stress [5, 9]. In addition, having a tendency to cause taper slip and stress relaxation, a polished tapered stem has less shear stress at the cement–bone interface [5, 9, 10, 13–16] and causes stem subsidence without cement fracture. It is presumed that if stem subsidence occurs without cement destruction or loosening, the cement moves in the femoral canal [5, 9, 16]. Basic experiments have found that PMMA cement moves, or creeps, after polymerization [8, 9, 12, 15]. Some reports describe the possibility of cement creep in polished tapered stems to explain stem subsidence [5, 9, 14].
In this study, stem subsidence was significantly greater in the cases with improvement in the initial radiolucency than the cases without improvement. Similar improvement in the radiolucency was not observed in the VerSys group, which had no stem subsidence apart from the case of loosening. We considered that although the VerSys Cemented Plus was a tapered stem, it had a rough surface partially coated with PMMA tightly bonding with cement, preventing the horizontal compressive stress [9, 15]. These results suggest that improvement in the initial radiolucency was caused by stem subsidence.
How did improvement in radiolucency in the CPT group occur? Wroblewski et al. reported that the same improvement in radiolucency as in our study was seen in 20% of the cases using a polished triple tapered stem [17], and they reported that the cancellous bone takes on a more dense appearance, indicating proximal load transfer from the implant to the bone. We also found that improvement in radiolucency was more frequently seen on the medial side of the canal. This may be associated with the load transfer that is likely to pass through the medial side of the femur. On the other hand, stem subsidence and improvement in the radiolucency were already visible in 86.7% of cases at the 6-month X-ray, early in the postoperative period. It is unlikely that only bone condensation by the stress transfer would lead to improvement in the radiolucency by 6 months. It may be caused not only by bone condensation due to load transfer, but also to so-called cement creep, and transposition of cement into the canal after polymerization, due to hoop stress in the femoral canal. Some reports have demonstrated that cement creep and stem subsidence are often seen in an early stage [1, 5, 12, 18].
In addition, the average of stem subsidence was greater in the cases that improved than in the other cases in this study. Because the moving cement volume caused by stem subsidence was considered insufficient to fill the initial radiolucency, both the concept of bone condensation and cement creep were used to explain the mechanism of improvement in the initial radiolucency. Although the existence of many other issues, such as the material property of cement over the long term, fretting wear by the stem, and so on make this a complex issue, continuous improvement in radiolucency is a good sign contrary to loosening and may lead to improved long-term results in polished stems.
References
- 1.Alfaro-Adrian J, Gill HS, Murray DW. Should total hip arthroplasty femoral components be designed to subside? A radiostereometric analysis study of the Charnley Elite and Exeter stems. J Arthroplasty. 2001;16:598–606. doi: 10.1054/arth.2001.23576. [DOI] [PubMed] [Google Scholar]
- 2.Barrack RL, Mulroy RD, Jr, Harris WH. Improved cementing techniques and femoral component loosening in young patients with hip arthroplasty. A 12-year radiographic review. J Bone Joint Surg Br. 1992;74:385–389. doi: 10.1302/0301-620X.74B3.1587883. [DOI] [PubMed] [Google Scholar]
- 3.Braud P, Freeman MA. The effect of retention of the femoral neck and of cement upon the stability of a proximal femoral prosthesis. J Arthroplasty. 1990;5(Suppl):S5. doi: 10.1016/s0883-5403(08)80018-6. [DOI] [PubMed] [Google Scholar]
- 4.Collis DK, Mohler CG. Comparison of clinical outcomes in total hip arthroplasty using rough and polished cemented stems with essentially the same geometry. J Bone Joint Surg Am. 2002;84:586–592. doi: 10.2106/00004623-200204000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Fowler JL, Gie GA, Lee AJ, Ling RS (1988) Experience with the Exeter total hip replacement since 1970. Orthop Clin North Am 19:477–489. Erratum in Orthop Clin North Am (1989) 20(4):preceding 519 [PubMed]
- 6.Gruen TA, McNeice GM, Amstutz HC. “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop. 1979;141:17–27. [PubMed] [Google Scholar]
- 7.Howie DW, Middleton RG, Costi K. Loosening of matt and polished cemented femoral stems. J Bone Joint Surg Br. 1998;80:573–576. doi: 10.1302/0301-620X.80B4.8629. [DOI] [PubMed] [Google Scholar]
- 8.Lee AJC, Perkins RD, Ling RSM. Time-dependent properties of polymethylmethacrylate bone cement. In: Older J, editor. Implant bone interface. Berlin Heidelberg New York: Springer Verlag; 1990. p. 85. [Google Scholar]
- 9.Lee AJC. The time-dependent properties of polymethylmethacrylate bone cement: the interaction of shape of femoral stems, surface finish and bone cement. In: Learmonth ID, editor. Interfaces in total hip arthroplasty. Berlin Heidelberg New York: Springer Verlag; 2000. p. 11. [Google Scholar]
- 10.Lu Z, McKellop H. Effects of cement creep on stem subsidence and stresses in the cement mantle of a total hip replacement. J Biomed Mater Res. 1997;34:221–226. doi: 10.1002/(SICI)1097-4636(199702)34:2<221::AID-JBM11>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 11.Meding JB, Nassif JM, Ritter MA. Long-term survival of the T-28 versus the TR-28 cemented total hip arthroplasties. J Arthroplasty. 2000;15:928–933. doi: 10.1054/arth.2000.9319. [DOI] [PubMed] [Google Scholar]
- 12.Pal S, Saha S. Stress relaxation and creep behaviour of normal and carbon fibre reinforced acrylic bone cement. Biomaterials. 1982;3:93–96. doi: 10.1016/0142-9612(82)90040-0. [DOI] [PubMed] [Google Scholar]
- 13.Shen G. Femoral stem fixation. An engineering interpretation of the long-term outcome of Charnley and Exeter stems. J Bone Joint Surg Br. 1998;80:754–756. doi: 10.1302/0301-620X.80B5.8621. [DOI] [PubMed] [Google Scholar]
- 14.Verdonschot N, Huiskes R. Subsidence of THA stems due to acrylic cement creep is extremely sensitive to interface friction. J Biomech. 1996;29:1569–1575. doi: 10.1016/0021-9290(96)00077-2. [DOI] [PubMed] [Google Scholar]
- 15.Verdonschot N, Huiskes R. Acrylic cement creeps but does not allow much subsidence of femoral stems. J Bone Joint Surg Br. 1997;79:665–669. doi: 10.1302/0301-620X.79B4.7173. [DOI] [PubMed] [Google Scholar]
- 16.Verdonschot N, Huiskes R. Surface roughness of debonded straight-tapered stems in cemented THA reduces subsidence but not cement damage. Biomaterials. 1998;19:1773–1779. doi: 10.1016/S0142-9612(98)00088-X. [DOI] [PubMed] [Google Scholar]
- 17.Wroblewski BM, Siney PD, Fleming PA. Triple taper polished cemented stem in total hip arthroplasty: rationale for the design, surgical technique, and 7 years of clinical experience. J Arthroplast. 2001;16(8 Suppl 1):37–41. doi: 10.1054/arth.2001.28374. [DOI] [PubMed] [Google Scholar]
- 18.Yates P, Gobel D, Bannister G. Collarless polished tapered stem: clinical and radiological follow-up over 5 years. J Arthroplasty. 2002;17:189–195. doi: 10.1054/arth.2002.30292. [DOI] [PubMed] [Google Scholar]