Abstract
Background
Desire for death is not generally considered a harbinger of more severe suicidal behavior and is not routinely included in suicide research and assessment interviews. We aimed to compare desire for death and suicidal ideation as clinical markers for suicide attempts.
Methods
Using data from two nationally representative surveys (n=42,862 and n=43,093 respectively), we examined whether desire for death predicts suicide attempts. We compared the odds ratio (OR) and “Number Needed to be Exposed for one additional person to be Harmed” [NNEH] for lifetime suicide attempts among those with desire for death but no suicidal ideation; those with suicidal ideation but no desire for death, and those with both desire for death and suicidal ideation, compared to those with neither desire for death nor suicidal ideation.
Results
The risk for lifetime suicide attempt was similar among those with lifetime desire for death with no suicidal ideation and those with lifetime suicidal ideation with no desire for death. Respondents with both lifetime desire for death and suicidal ideation had the highest risk for lifetime suicide attempts.
Limitations
Cross-sectional design; self-reported suicidal ideation/attempts.
Conclusions
Querying individuals on desire for death has the same value as assessing suicidal ideation to examine risk for suicide attempt. A combination of desire for death and suicidal ideation is the best predictor for suicide attempts. This is of high clinical relevance since we suggest that desire for death should be included as a potential clinical marker of suicidality in clinical assessments.
Keywords: Attempted suicide, suicidal ideation, desire for death
Introduction
In the last two decades there have been approximately 30,000 suicide deaths per year in the United States (Centers for Disease Control and Prevention, 2009). Furthermore, the lifetime prevalence of suicide attempts in the US has remained stable over the past decade (Baca-Garcia et al., 2010), while the yearly age-adjusted rate of suicide has slightly increased between 1997 and 2007 (Centers for Disease Control and Prevention, 2009). These observations suggest that suicide prevention and treatment strategies are not working and provide good reason to question current views regarding risk factors for suicidal behavior. Ongoing debate about the adequacy of the assessment of suicidal behavior in current diagnostic frameworks has led to the suggestion that suicidal behavior be included as a separate diagnostic entity in DSM-V (Oquendo et al., 2008). Moreover, the rate and quality of treatment received for depression, even in patients at high risk for suicidal behavior, is still suboptimal and often does not adhere to published guidelines (Hasin et al., 2005; Kessler et al., 2003; Oquendo et al., 2002; Oquendo et al., 1999; Wang et al., 2005; Young et al., 2001). This is striking given that depression is one of the major risk factors for suicide attempts and suicide (APA, 2003). An additional factor that may have had an effect on antidepressant treatment is the media coverage of the FDA black box warning to antidepressants regarding increased risk of suicidality in children (Barry and Busch, 2010), which has been shown to have an impact on prescription trends (Nemeroff et al., 2007).
Desire for death, often conceptualized as passive suicidal ideation, is a core element of the definition of suicide attempts put forth by the U.S. National Institute of Mental Health (O’Carroll et al., 1996) and suicidal individuals often experience an internal struggle between wanting to live and wanting to die (Brown et al., 2005; Kovacs and Beck, 1977). However, desire for death is not generally considered a harbinger of more severe suicidal behavior. Research on suicidal behavior has primarily focused on individuals with suicidal ideation or suicide attempts, and the prevalence of desire for death has not been reported in any analyses of the major epidemiologic surveys that have examined suicidal behaviors (Kessler et al., 2005; Kessler et al., 1999; Moscicki et al., 1988). Similarly, several major psychiatry textbooks (Carroll-Ghosh et al., 2003; Sadock and Sadock, 2007) and the recommendations of the UK National Institute for Clinical Excellence for the psychological management and secondary prevention of self-harm in primary and secondary care do not recommend the inclusion of questions about desire for death as part of an assessment of suicide risk (Health, 2004).
A recent review of the complex nomenclature for suicide and suicidal behaviors (Silverman et al., 2007) observed that multiple synonyms exist for suicidal ideation, some of which were related to passive desire for death, and highlighted the need to investigate the association of desire for death and risk for suicide attempt.
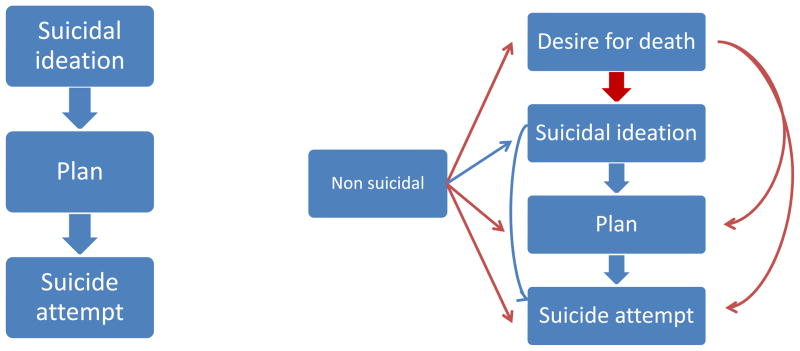
Process models of suicide attempt propose a continuum of risk for attempting suicide that starts with suicidal ideation (see Figure 1). According to this model, only a small percentage of individuals with suicidal ideation progress to making a plan, and only a small proportion of individuals with a plan progress to attempting suicide (Crosby et al., 1999; Kessler et al., 1999; LeMaster et al., 2004). The few studies based on this model which also considered desire for death imply a severity gradient, with desire for death usually labeled as “lower severity”, suicidal ideation as “intermediate severity”, and suicide attempts representing “high severity” (Linden and Barnow, 1997; Yip et al., 2003).
Figure 1.
Traditional continuum model (left) versus multiple pathways model (right) for risk of suicide attempta
aThe blue arrows represent transitions between stages that have been previously analyzed in the literature. The red arrows represent transitions between stages that have not been previously studied.
There are indications that this conceptualization may not provide an adequate description of the relationship among different suicidal thoughts and behaviors. In one study, rates of suicide attempts were greater than rates of suicidal ideation (LeMaster et al., 2004). In a survey of the US population, at least one third of adults reporting previous suicide attempts denied making a plan (Crosby et al., 1999). Such attempts were interpreted as being impulsive, carried out on the spur of the moment without prior suicidal ideation and/or planning (Crosby et al., 1999; LeMaster et al., 2004). However, an alternative explanation may be that desire for death, unexamined in those studies, is a key risk factor for attempting suicide for a high percentage of individuals, including those without previous planning.
Some evidence suggests that the assumption that desire for death does not significantly increase the risk for attempting suicide is questionable. First, although few studies have focused on the impact of desire for death on the risk for future suicidal behavior, some report that desire for death may be an important predictor of future completed suicide (Palacio et al., 2007; Suokas et al., 2001). In addition, when the desire for death is greater than the wish to live, the seriousness of suicidal intent during a suicide attempt may be greater (Kovacs and Beck, 1977). In a study of older women, the strength of desire for death distinguished those who more actively wished to end their lives from those who did not (Rao et al., 1997). Taken together, these findings suggest that the emergence of desire for death may be an alternative onset point that influences whether an individual will progress towards a suicide attempt.
In this study we used data from two recent large epidemiological surveys of the general population in the US. We examined whether desire for death is a marker of suicide attempt in the National Institute on Alcohol Abuse and Alcoholism (NIAAA) National Longitudinal Alcohol Epidemiologic Survey (NLAES) dataset and conducted the same analysis using National Epidemiologic Survey of Alcohol and Related Conditions (NESARC) data to verify that the findings were consistent across studies.
Methods
Samples
The 1991–1992 NLAES (n=42,862) and its successor the 2001–2002 NESARC (n=43,093), are nationally representative samples of the adult population of the United States, as described previously (Grant et al., 2004a; Grant et al., 1992; Grant et al., 2003; Grant et al., 1994; Grant et al., 2004b). The purpose of both surveys was to provide nationally representative data on the distribution and correlates of alcohol use disorders and associated conditions. The sample design and field methods were nearly identical, as described previously (Compton et al., 2004). The target population for both surveys was the U.S. general population, 18 years and older. The NESARC and NLAES overall response rates were 81% and 90%, respectively. Fieldwork was carried out by the United States Bureau of the Census under NIAAA staff supervision.
NLAES and NESARC respondents were informed in writing about the nature of the survey, the statistical uses of the survey data, the voluntary aspect of participation, and the federal laws that rigorously provided for the strict confidentiality of the identifiable survey information. Those respondents who gave written informed consent to participate after receiving this information were interviewed. The research protocols, including informed consent procedures, received full ethical review and approval from the US Census Bureau and US Office of Management and Budget. As noted previously (Compton et al., 2004), there were minor differences in the mode of administration of the surveys, for example whether interviewers recorded the information on paper or directly into a computer. In both surveys, data were adjusted to account for oversampling and respondent and household response and to be representative of the US population on a range of sociodemographic characteristics at the time of the study.
Diagnostic Assessment of Suicidal behaviors
The NLAES and NESARC included exactly the same questions to assess lifetime suicidal behaviors. NLAES and NESARC respondents were asked the following questions: “During that time when your mood was at its lowest/you enjoyed or cared the least about things, did you: 1) think about committing suicide?; 2) attempt suicide?” We used the first question to assess a lifetime history of suicidal ideation, and the second to assess a lifetime history of suicide attempt. A relevant difference between the NLAES and the NESARC is that the questions related to suicidal ideation and suicide attempt were asked only to those who screened into the major depressive episode section in the NESARC survey, whereas all respondents in the NLAES were assessed for suicidal ideation and suicide attempt. To screen into the major depressive episode section, subjects had to answer yes to one of these two questions: 1) “In your entire life, have you ever had a time when you felt sad, blue, depressed, or down most of the time for at least 2 weeks?”; or 2) “In your entire life, have you ever had a time, lasting at least 2 weeks, when you didn’t care about the things that you usually cared about, or when you didn’t enjoy the things you usually enjoyed?”. To ensure equality of measurement across the NLAES and NESARC, the present study focused on suicide-related behaviors of individuals who screened into the depression section of the AUDADIS-IV interview in either survey. In the NLAES survey, 33.8% of respondents screened into the depression section of the interview; in the NESARC survey, 31.7% of respondents screened in.
Statistical analysis
We analyzed the conditional rates of lifetime suicide attempt among different subgroups. We hypothesized that, according to the process models of suicide attempt, the rates of lifetime suicide attempt would be lowest among those with neither desire for death nor suicidal ideation (Subgroup 0), followed by those with desire for death but no suicidal ideation (Subgroup 1), those with suicidal ideation but no desire for death (Subgroup 2), and those with both suicidal ideation and desire for death (Subgroup 3).
We also estimated the lifetime rates of desire for death, suicidal ideation and suicide attempt, and the conditional rates of lifetime suicidal ideation among those with desire for death.
For all analyses, we present the percentage and 95% confidence interval (95% CI), and the Odds Ratio for suicide attempts in each subgroup (OR) compared to those with no desire for death and no suicidal ideation. The findings obtained in the NLAES were compared to those found in the NESARC. Because the combined standard error of two means (or percents) is always equal or less than the sum of the standard errors of those two means, we consider two confidence intervals (CIs) that do not overlap to be significantly different from one another (Agresti, 2002).
To assess the utility of querying individuals on the presence of desire for death and suicidal ideation, we calculated the “Number Needed to be Exposed for one additional person to be Harmed” (NNEH) (Bender and Blettner, 2002), where harm was defined as suicide attempt, and exposure as desire for death and suicidal ideation respectively. The NNEH is an extension to epidemiological studies of the Number Needed to Treat (NNT) concept. It is described as “the analogous definition of the NNT measure when the considered agent is exposure rather than treatment”, and can be used to compare exposed and unexposed subjects in epidemiological studies (Bender and Blettner, 2002).
All analyses were conducted with SUDAAN, a statistical software package that is suitable for analyses of studies with complex survey designs.
Results
The lifetime rates of desire for death, suicidal ideation and suicide attempt, and the conditional rates of lifetime suicidal ideation among those with desire for death in the NLAES and NESARC are shown in Table 1.
Table 1.
Lifetime rates of desire for death, suicide ideation and suicide attempt, and conditional rates of lifetime suicidal ideation among those with desire for death in the National Longitudinal Alcohol Epidemiologic Survey (NLAES) and the National Epidemiologic Survey of Alcohol and Related Conditions (NESARC).
| NLAES(n=42,862) | NESARC (n=43,093) | |||
|---|---|---|---|---|
| % | 95% CI | % | 95% CI | |
| Desire for death | 11.3 | 10.90–11.63 | 10.2 | 9.63–10.75 |
| Suicidal ideation among those with desire for death | 70.5 | 68.92–72.05 | 70.4 | 68.44–72.26 |
| Suicide ideation | 9.7 | 9.32–10.01 | 8.4 | 7.82–8.93 |
| Suicide attempt | 2.4 | 2.26–2.59 | 2.4 | 2.16–2.56 |
The conditional rates of lifetime suicide attempts among those without desire for death and without suicidal ideation (Subgroup 0), those with desire for death without suicidal ideation (Subgroup 1), those with suicidal ideation without desire for death (Subgroup 2), and those with both suicidal ideation and desire for death (Subgroup 3) in the NLAES and NESARC are shown in Table 2.
Table 2.
Conditional rates of lifetime suicide attempts in the National Longitudinal Alcohol Epidemiologic Survey (NLAES) and the National Epidemiologic Survey of Alcohol and Related Conditions (NESARC) among those with neither desire for death nor suicidal ideation (Subgroup 0), those with desire for death without suicidal ideation (Subgroup 1), those with suicidal ideation without desire for death (Subgroup 2), and those with both suicidal ideation and desire for death (Subgroup 3). ORs and NNEH were calculated using Subgroup 0 as the reference category.
| Subgroups | Neither Desire for Death nor Suicidal Ideation (0) | Desire for Death with no Suicidal Ideation (1) | Suicidal Ideation with no Desire for Death(2) | Desire for Death and Suicidal Ideation (3) | |
|---|---|---|---|---|---|
| Desire for death | − | + | − | + | |
| Suicidal ideation | − | − | + | + | |
| NLAES * | % (95% CI) | 0.14 (0.10–0.19) | 5.41 (4.16–7.00) | 2.75 (1.60–4.71) | 25.9 (24.22–27.67) |
| OR (95% CI) | 1.00 | 46.87 (31.17–70.47) | 18.63 (10.83–32.02) | 255.51 (173.49–376.31) | |
| NNEH(95% CI) | − | 18.56 (12.59–27.70) | 46.69 (26.97–82.94) | 4.17 (3.15–5.67) | |
| NESARC ** | % (95% CI) | 0.07 (0.04–0.11) | 2.39 (1.59–3.57) | 6.11 (3.82–9.64) | 30.0(28.12–31.89) |
| OR (95% CI) | 1.00 | 37.37 (19.09–73.53) | 99.75 (47.83–208.03) | 655.42 (376.20–1141.86) | |
| NNEH(95% CI) | − | 48.69 (24.91–96.87) | 18.56 (9.38–38.04) | 3.65 (2.52–5.62) |
In the NLAES: Among those that reported a suicide attempt (N=1,086), 150 individuals (13.2%) reported no suicidal ideation, and 68 (6.7%) individuals reported no desire for death. Among those that reported suicidal ideation (N=4,321), 716 (17.8%) reported no desire for death.
In the NESARC: Among those that reported a suicide attempt (N=1,074), 62 individuals (5.8%) reported no suicidal ideation, and 55 individuals (5.1%) reported no desire for death. Among those that reported suicidal ideation, (N=3,566), 491 (13.8%) reported no desire for death.
In the NLAES, the highest rate of lifetime suicide attempt was found among respondents with both lifetime desire for death and suicidal ideation (Subgroup 3, 25.9%, 95% CI=24.22–27.67). The rate of lifetime suicide attempt among those with lifetime desire for death but no suicidal ideation (Subgroup 1, 5.41%, 95% CI=4.16–7.00) was higher but not significantly different from the rate found among respondents with lifetime suicidal ideation but no desire for death (Subgroup 2, 2.75%, 95% CI=1.60–4.71). The lowest rate of lifetime suicide attempt was found among respondents with neither desire for death nor suicidal ideation (Subgroup 0, 0.14%, 95% CI= 0.10–0.19) (Table 2).
In the NESARC, the highest rate of lifetime suicide attempt was found among respondents with both lifetime desire for death and suicidal ideation (Subgroup 3, 30.0%, 28.11–31.89). The rate of lifetime suicide attempts was significantly lower among respondents with lifetime desire for death but no suicidal ideation (Subgroup 1, 2.39%, 95% CI=1.59–3.57) than among respondents with lifetime suicidal ideation but no desire for death (Subgroup 2, 6.11%, 95% CI=3.82–9.64). The lowest rate of lifetime attempts was found among respondents with neither desire for death nor suicidal ideation (Subgroup 0, 0.07%, 95% CI=0.04–0.11) (Table 2).
In the NLAES, among those with a past suicide attempt, 13.2% reported no suicidal ideation, whereas 6.7% reported no desire for death. In the NESARC, among those who reported a past suicide attempt, 5.8% reported no suicidal ideation, and 5.1% reported no desire for death.
The ORs and NNEHs for lifetime suicide attempts for all the subgroups are presented in Table 2.
In the NLAES and NESARC, the highest OR and the lowest NNEH for lifetime suicide attempts was found among those with both desire for death and suicidal ideation (Subgroup 3). The OR for this subgroup was significantly higher and the NNEH was significantly lower than among those with lifetime desire for death with no suicidal ideation (Subgroup 1) or those with lifetime suicidal ideation with no desire for death (Subgroup 2). There were no significant differences in the ORs and NNEHs for lifetime suicide attempts among those with lifetime desire for death with no suicidal ideation (Subgroup 1) compared to lifetime suicidal ideation with no desire for death (Subgroup 2). (Table 2).
Discussion
In two large community samples, the combination of desire for death and suicidal ideation was the best marker for lifetime suicide attempts, whereas there were no significant differences in the probability of lifetime suicide attempt between individuals with lifetime desire for death with no suicidal ideation and those with lifetime suicidal ideation but no desire for death.
In both surveys, the ORs for lifetime suicide attempts among those with both desire for death and suicidal ideation were very large, and significantly higher than among those with lifetime desire for death but no suicidal ideation and those with lifetime suicidal ideation but no desire for death. The NNEHs for lifetime suicide attempts among those with both desire for death and suicidal ideation (4.17 and 3.65 in the NLAES and NESARC respectively) were significantly lower than among those with lifetime desire for death but suicidal ideation and those with lifetime suicidal ideation but desire for death. This indicates that four individuals need to report both desire for death and suicidal ideation for one additional case of suicide attempt to be reported, compared to individuals with neither desire for death nor suicidal ideation. The ORs and NNEHs for lifetime suicide attempts were similar between those with lifetime desire for death but no suicidal ideation and those with lifetime suicidal ideation but no desire for death.
There is little guidance on the acceptable NNEH threshold to warrant a preventive intervention in the general population (Cheng, 2007). However, for comparison purposes, the number needed to screen (NNS) for 5 years using a lipid profile to prevent one death was 418; the NNS for 5 years using mammography in women aged 40 to 49 years to prevent 1 breast cancer death was 8,054 (Rembold, 1998). Given the relatively high estimated prevalence of desire for death (11.3% NLAES; 10.2% NESARC) and suicidal ideation (9.7% NLAES, 8.4% NESARC), these low NNEH demonstrate the high risk for suicide attempts among individuals in the general population.
Of note, the lifetime prevalence of suicide attempts among those experiencing neither desire for death nor suicidal ideation is extremely low (0.14 %, 95% CI 0.10–0.19 in the NLAES and 0.07%, 95% CI 0.04–0.11 in the NESARC) compared to those with desire for death and/or suicidal ideation. This suggests that impulsive suicide attempts without prior passive or active suicidal ideation may be much less frequent in the general population than previous studies have suggested (Baca-Garcia et al., 2001).
Taken together, these findings suggest that suicidal ideation is not the only starting point on the trajectory to making a suicide attempt, and thus assessing desire for death in people who deny suicidal thoughts would be clinically useful. Querying individuals on desire for death has the same value as assessing suicidal ideation to examine the risk for suicide attempts, whereas the combination of desire for death and suicidal ideation is the best marker for detecting lifetime suicide attempts.
This is the first study to analyze the rates of reported lifetime desire for death in relation to rates of suicide attempt in two nationally representative samples. The large sample size of both surveys, their national representativeness and the consistency of the findings across both samples are important strengths of the present study. However, our findings should be viewed with two main limitations in mind. First, the NLAES and the NESARC, like all large-scale surveys, rely on lay interviewers and on self-reported rates of suicide attempts. Second, the cross-sectional design of the NLAES and Wave I of the NESARC makes it impossible to study the temporal progression from desire for death to suicidal ideation or suicide attempts, and only allows for identification of associations. An additional limitation is that suicide related questions were only asked of respondents who screened into the depression module in the NESARC.
In summary, our findings suggest that the conceptualization of the trajectory of a suicide attempt as a continuum, starting with suicidal ideation, followed by making a plan, and finally attempting suicide (Crosby et al., 1999; Kessler et al., 1999; LeMaster et al., 2004) may require revision in order to include desire for death, and to acknowledge the fact that not all stages in the continuum proposed in the literature are always evident prior to a suicide attempt. In addition, other factors such as having fewer reasons for living, which has been identified as a risk factor for suicide attempts (Galfalvy et al., 2006; Lizardi et al., 2007; Oquendo et al., 2007), may precede the onset of desire for death, and should be routinely assessed when evaluating the risk for suicide. Clinical evaluation of the risk for suicide may need to undergo change, and scales to assess suicide risk may also need revision (Mann et al., 2005; Maris, 2002). A recent study on the prevalence of suicidal behaviors, calculated a “Composite Measure for Suicidal ideation” that reflected the scores for each individual on measures of suicidal ideation, attempt, wish, and plan to die (Haggarty et al., 2008). We suggest that desire for death should be included as a potential clinical marker of suicidal risk in the repositioning of suicide as a separate diagnostic entity that is currently being advocated for DSM-V (Oquendo et al., 2008). Future clinical and epidemiological studies examining suicide risk should include questions about desire for death and examine its relationship with suicidal ideation and attempts.
Footnotes
Location of work
The work was conducted at the Department of Psychiatry at Columbia University, New York, NY, USA.
The work has not been previously presented.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Agresti A. Categorical data analysis. Wiley; New York, NY: 2002. [Google Scholar]
- APA. Practice guideline for the assessment and treatment of patients with suicidal behaviors. American Psychiatric Association; Arlington, Virginia: 2003. [PubMed] [Google Scholar]
- Baca-Garcia E, Diaz-Sastre C, Basurte E, Prieto R, Ceverino A, Saiz-Ruiz J, de Leon J. A prospective study of the paradoxical relationship between impulsivity and lethality of suicide attempts. J Clin Psychiatry. 2001;62:560–564. doi: 10.4088/jcp.v62n07a11. [DOI] [PubMed] [Google Scholar]
- Baca-Garcia E, Perez-Rodriguez MM, Keyes KM, Oquendo MA, Hasin DS, Grant BF, Blanco C. Suicidal ideation and suicide attempts in the United States: 1991–1992 and 2001–2002. Mol Psychiatry. 2010;15:250–259. doi: 10.1038/mp.2008.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry CL, Busch SH. News coverage of FDA warnings on pediatric antidepressant use and suicidality. Pediatrics. 2010;125:88–95. doi: 10.1542/peds.2009-0792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bender R, Blettner M. Calculating the “number needed to be exposed” with adjustment for confounding variables in epidemiological studies. J Clin Epidemiol. 2002;55:525–530. doi: 10.1016/s0895-4356(01)00510-8. [DOI] [PubMed] [Google Scholar]
- Brown GK, Steer RA, Henriques GR, Beck AT. The internal struggle between the wish to die and the wish to live: a risk factor for suicide. Am J Psychiatry. 2005;162:1977–1979. doi: 10.1176/appi.ajp.162.10.1977. [DOI] [PubMed] [Google Scholar]
- Carroll-Ghosh T, Victor BS, Bourgeois JA. Suicide. In: Hales REYS, editor. Textbook of Clinical Psychiatry. American Psychiatric Publishing Inc; Washington: 2003. [Google Scholar]
- Centers for Disease Control and Prevention, C; National Center for Injury Prevention and Control, CDC (producer) Web-based Injury Statistics Query and Reporting System (WISQARS) [Online] 2009. [Google Scholar]
- Cheng H. The number needed to be exposed: a potential use for quantifying the strength of an individual risk factor including a protective factor in a cohort study. Arch Intern Med. 2007;167:1690. doi: 10.1001/archinte.167.15.1690-a. author reply 1690–1691. [DOI] [PubMed] [Google Scholar]
- Compton WM, Grant BF, Colliver JD, Glantz MD, Stinson FS. Prevalence of marijuana use disorders in the United States: 1991–1992 and 2001–2002. JAMA. 2004;291:2114–2121. doi: 10.1001/jama.291.17.2114. [DOI] [PubMed] [Google Scholar]
- Crosby AE, Cheltenham MP, Sacks JJ. Incidence of suicidal ideation and behavior in the United States, 1994. Suicide Life Threat Behav. 1999;29:131–140. [PubMed] [Google Scholar]
- Galfalvy H, Oquendo MA, Carballo JJ, Sher L, Grunebaum MF, Burke A, Mann JJ. Clinical predictors of suicidal acts after major depression in bipolar disorder: a prospective study. Bipolar Disord. 2006;8:586–595. doi: 10.1111/j.1399-5618.2006.00340.x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug Alcohol Depend. 2004a;74:223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Grant BF, Harford TC, Dawson DA, Chou SP, Dufour M, Pickering RP. Prevalence of DSM-IV alcohol abuse and dependence: United States, 1992. Alcohol Health Res World. 1992;18:243–248. [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Kaplan K, Shepard J, Moore T. Source and Accuracy Statement for Wave 1 of the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions. National Institute on Alcohol Abuse and Alcoholism; Bethesda, MD: 2003. [Google Scholar]
- Grant BF, Peterson A, Dawson DA, Chou SP. Source and Accuracy Statement for the National Longitudinal Alcohol Epidemiologic Survey (NLAES) National Institute on Alcohol Abuse and Alcoholism; Bethesda, MD: 1994. [Google Scholar]
- Grant BF, Stinson FS, Hasin DS, Dawson DA, Chou SP, Anderson K. Immigration and lifetime prevalence of DSM-IV psychiatric disorders among Mexican Americans and non-Hispanic whites in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004b;61:1226–1233. doi: 10.1001/archpsyc.61.12.1226. [DOI] [PubMed] [Google Scholar]
- Haggarty JM, Cernovsky Z, Bedard M, Merskey H. Suicidality in a sample of Arctic households. Suicide Life Threat Behav. 2008;38:699–707. doi: 10.1521/suli.2008.38.6.699. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry. 2005;62:1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- Health, N.C.C.f.M. Self-harm: the short-term physical and psychological management and secondary prevention of self-harm in primary and secondary care. NICE clinical guideline National Institute for Clinical Excellence (NICE); London (UK): 2004. [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Borges G, Nock M, Wang PS. Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990–1992 to 2001–2003. JAMA. 2005;293:2487–2495. doi: 10.1001/jama.293.20.2487. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, Wang PS. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999;56:617–626. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- Kovacs M, Beck AT. The wish to die and the wish to live in attempted suicides. J Clin Psychol. 1977;33:361–365. doi: 10.1002/1097-4679(197704)33:2<361::aid-jclp2270330207>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- LeMaster PL, Beals J, Novins DK, Manson SM. The prevalence of suicidal behaviors among Northern Plains American Indians. Suicide Life Threat Behav. 2004;34:242–254. doi: 10.1521/suli.34.3.242.42780. [DOI] [PubMed] [Google Scholar]
- Linden M, Barnow S. 1997 IPA/Bayer Research Awards in Psychogeriatrics. The wish to die in very old persons near the end of life: a psychiatric problem? Results from the Berlin Aging Study. Int Psychogeriatr. 1997;9:291–307. doi: 10.1017/s1041610297004456. [DOI] [PubMed] [Google Scholar]
- Lizardi D, Currier D, Galfalvy H, Sher L, Burke A, Mann J, Oquendo M. Perceived reasons for living at index hospitalization and future suicide attempt. J Nerv Ment Dis. 2007;195:451–455. doi: 10.1097/NMD.0b013e3180522661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann JJ, Apter A, Bertolote J, Beautrais A, Currier D, Haas A, Hegerl U, Lonnqvist J, Malone K, Marusic A, Mehlum L, Patton G, Phillips M, Rutz W, Rihmer Z, Schmidtke A, Shaffer D, Silverman M, Takahashi Y, Varnik A, Wasserman D, Yip P, Hendin H. Suicide prevention strategies: a systematic review. JAMA. 2005;294:2064–2074. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- Maris RW. Suicide. Lancet. 2002;360:319–326. doi: 10.1016/S0140-6736(02)09556-9. [DOI] [PubMed] [Google Scholar]
- Moscicki EK, O’Carroll P, Rae DS, Locke BZ, Roy A, Regier DA. Suicide attempts in the Epidemiologic Catchment Area Study. Yale J Biol Med. 1988;61:259–268. [PMC free article] [PubMed] [Google Scholar]
- Nemeroff CB, Kalali A, Keller MB, Charney DS, Lenderts SE, Cascade EF, Stephenson H, Schatzberg AF. Impact of publicity concerning pediatric suicidality data on physician practice patterns in the United States. Arch Gen Psychiatry. 2007;64:466–472. doi: 10.1001/archpsyc.64.4.466. [DOI] [PubMed] [Google Scholar]
- O’Carroll PW, Berman AL, Maris RW, Moscicki EK, Tanney BL, Silverman MM. Beyond the Tower of Babel: a nomenclature for suicidology. Suicide Life Threat Behav. 1996;26:237–252. [PubMed] [Google Scholar]
- Oquendo MA, Baca-Garcia E, Mann JJ, Giner J. Issues for DSM-V: suicidal behavior as a separate diagnosis on a separate axis. Am J Psychiatry. 2008;165:1383–1384. doi: 10.1176/appi.ajp.2008.08020281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oquendo MA, Bongiovi-Garcia ME, Galfalvy H, Goldberg PH, Grunebaum MF, Burke AK, Mann JJ. Sex differences in clinical predictors of suicidal acts after major depression: a prospective study. Am J Psychiatry. 2007;164:134–141. doi: 10.1176/appi.ajp.164.1.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oquendo MA, Kamali M, Ellis SP, Grunebaum MF, Malone KM, Brodsky BS, Sackeim HA, Mann JJ. Adequacy of antidepressant treatment after discharge and the occurrence of suicidal acts in major depression: a prospective study. Am J Psychiatry. 2002;159:1746–1751. doi: 10.1176/appi.ajp.159.10.1746. [DOI] [PubMed] [Google Scholar]
- Oquendo MA, Malone KM, Ellis SP, Sackeim HA, Mann JJ. Inadequacy of antidepressant treatment for patients with major depression who are at risk for suicidal behavior. Am J Psychiatry. 1999;156:190–194. doi: 10.1176/ajp.156.2.190. [DOI] [PubMed] [Google Scholar]
- Palacio C, Garcia J, Diago J, Zapata C, Lopez G, Ortiz J, Lopez M. Identification of suicide risk factors in Medellin, Colombia: a case-control study of psychological autopsy in a developing country. Arch Suicide Res. 2007;11:297– 308. doi: 10.1080/13811110600894223. [DOI] [PubMed] [Google Scholar]
- Rao R, Dening T, Brayne C, Huppert FA. Suicidal thinking in community residents over eighty. Int J Geriatr Psychiatry. 1997;12:337–343. [PubMed] [Google Scholar]
- Rembold CM. Number needed to screen: development of a statistic for disease screening. BMJ. 1998;317:307–312. doi: 10.1136/bmj.317.7154.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadock BJ, Sadock VA, editors. Kaplan and Sadock’s Comprehensive Textbook of Psychiatry. Lippincott Williams; Philadelphia: 2007. [Google Scholar]
- Silverman MM, Berman AL, Sanddal ND, O’Carroll PW, Joiner TE. Rebuilding the tower of Babel: a revised nomenclature for the study of suicide and suicidal behaviors. Part 1: Background, rationale, and methodology. Suicide Life Threat Behav. 2007;37:248–263. doi: 10.1521/suli.2007.37.3.248. [DOI] [PubMed] [Google Scholar]
- Suokas J, Suominen K, Isometsa E, Ostamo A, Lonnqvist J. Long-term risk factors for suicide mortality after attempted suicide--findings of a 14-year follow-up study. Acta Psychiatr Scand. 2001;104:117–121. doi: 10.1034/j.1600-0447.2001.00243.x. [DOI] [PubMed] [Google Scholar]
- Wang PS, Schneeweiss S, Brookhart MA, Glynn RJ, Mogun H, Patrick AR, Avorn J. Suboptimal antidepressant use in the elderly. J Clin Psychopharmacol. 2005;25:118–126. doi: 10.1097/01.jcp.0000155819.67209.e5. [DOI] [PubMed] [Google Scholar]
- Yip PS, Chi I, Chiu H, Chi Wai K, Conwell Y, Caine E. A prevalence study of suicide ideation among older adults in Hong Kong SAR. Int J Geriatr Psychiatry. 2003;18:1056–1062. doi: 10.1002/gps.1014. [DOI] [PubMed] [Google Scholar]
- Young AS, Klap R, Sherbourne CD, Wells KB. The quality of care for depressive and anxiety disorders in the United States. Arch Gen Psychiatry. 2001;58:55–61. doi: 10.1001/archpsyc.58.1.55. [DOI] [PubMed] [Google Scholar]