1. DISEASE CHARACTERISTICS
1.1 Name of the disease (synonyms)
Hypertrophic cardiomyopathy (HCM CMH), familial HCM CMH, ventricular hypertrophy, hereditary asymmetric septal hypertrophy, hypertrophic obstructive cardiomyopathy (HOCM), and hypertrophic subaortic stenosis.
1.2 OMIM# of the disease
192600 Cardiomyopathy, familial hypertrophic; CMH.
115195 Cardiomyopathy, familial hypertrophic, 2; CMH2.
115196 Cardiomyopathy, familial hypertrophic, 3; CMH3.
115197 Cardiomyopathy, familial hypertrophic, 4; CMH4.
600858 Cardiomyopathy, familial hypertrophic, 6; CMH6.
+191044 Cardiomyopathy, familial hypertrophic, 7; CMH7.
608751 Cardiomyopathy, familial hypertrophic, 8; CMH8.
+191044 Cardiomyopathy, familial hypertrophic, 9; CMH9.
608758 Cardiomyopathy, familial hypertrophic, 10; CMH10.
612098 Cardiomyopathy, familial hypertrophic, 11; CMH11.
612124 Cardiomyopathy, familial hypertrophic, 12; CMH12.
613243 Cardiomyopathy, familial hypertrophic, 13; CMH13.
613251 Cardiomyopathy, familial hypertrophic, 14; CMH14.
613243 Cardiomyopathy, familial hypertrophic, 15; CMH15.
1.3 Name of the analysed genes or DNA/chromosome segments
1. Sarcomeric protein genes:
a. Cardiac myosin-binding protein-C gene (MYBPC-3) locus 11p11.2.
b. Cardiac beta-myosin heavy chain gene (MYH7) locus 14q11.2-q12.
c. Troponin T gene (TNNT2) locus 1q32.
d. Troponin I gene (TNNTI3) locus 19q13.4.
e. Alpha tropomyosin gene (TPM1) locus 15q22.1.
f. Essential light-chain gene (MYL3) locus 3p21.2-p21.3.
g. Alpha-cardiac myosin heavy chain (MYH6) locus 14q11.2-q12.
h. Alpha-cardiac actin (ACTC) locus 15q11-q14.
i. Titin (TTN) locus 2q31.
j. Regulatory myosine light chain (MYL2) locus 12q23-q.24.3.
k. Cardiac troponin C (TNNC1) locus 3p21.3-p14.3.
2. Z-disc genes:
a. LIM-binding domain 3 (LBD3) locus 10q22.2-q23.3.
b. Muscle LIM protein (CSRP3) locus 11p15.1.
c. Telethonin (TCAP) locus 17q12-q21.1.
d. Vinculin (VCL) locus 10q22.1-q23.
e. Alpha-actinin 2 (ACTN2) locus 1q42-q43.
f. Myozenin 2 (MYOZ2) locus 4q26-q27.
3. Calcium-handling genes:
a. Junctophilin-2 (JPH2) locus 20q12.
b. Phospholamban (PLN) locus 6q21.1.
Phenocopies/syndromes with only cardiac manifestation possible.
a. AMP-activated protein kinase (PRKAG2) locus 7q35-q36.36 → Wolff–Parkinson–White syndrome, with or without HCM CMH.
b. Mitochondrial oxidative phosphorylation (OXPHOS) mtDNA.
c. Alpha-galactosidase A (GLA) locus Xq22 → Fabry's disease.
d. Lysosome-associated membrane protein 2 (LAMP2) locus Xq24 → Danon's disease/Wolff–Parkinson–White syndrome.
1.4 OMIM# of the gene(s)
1. Sarcomeric protein genes:
*600958 Cardiac myosin-binding protein-C gene (MYBPC-3) locus 11p11.2.
+160760 Cardiac beta-myosin heavy chain gene (MYH7) locus 14q11.2-q12.
*191045 Troponin T gene (TNNT2) locus 1q32.
+191044 Troponin I gene (TNNTI3) locus 19q13.4.
*191010 Alpha tropomyosin gene (TPM1) locus 15q22.1.
*160790 Essential light-chain gene (MYL3) locus 3p21.2-p21.3.
+160710 Alpha-cardiac myosin heavy chain (MYH6) locus 14q11.2-q12.
+102540 Alpha-cardiac actin (ACTC) locus 15q11-q14.
+188840 Titin (TTN) locus 2q31.
*160781 Regulatory myosine light chain (MYL2) locus 12q23-q.24.3.
*191040 Cardiac troponin C (TNNC1) locus 3p21.3-p14.3.
2. Z-disc genes:
*605906 LIM domain-binding 3 (LDB3) locus 10q22.2-q23.3.
*600824 Muscle LIM protein (CSRP3) locus 11p15.1.
*604488 Telethonin (TCAP) locus 17q12-q21.1.
*193065 Vinculin (VCL) locus 10q22.1-q23.
*102573 Alpha-actinin 2 (ACTN2) locus 1q42-q43.
*605602 Myozenin 2 (MYOZ2) locus 4q26-q27.
3. Calcium-handling genes:
*605267 Junctophilin-2 (JPH2) locus 20q12.
*172405 Phospholamban (PLN) locus 6q21.1.
Phenocopies/syndromes with only cardiac manifestation possible.
*602743 AMP-activated protein kinase (PRKAG2) locus 7q35-q36.36 → Wolff–Parkinson–White syndrome, with our without HCM CMH.
Mitochondrial oxidative phosphorylation (OXPHOS) mtDNA.
*300644 Alpha-galactosidase A (GLA) locus Xq22 → Fabry's disease.
*309060 Lysosome-associated membrane protein 2 (LAMP2) locus Xq24 → Danon's disease/Wolff–Parkinson–syndrome.
1.5 Mutational spectrum
Many genes are involved in HCM. For practically all genes, all types of mutations have been reported (missense, frameshift, nonsense, splice site, and small deletions and insertions).
1.6 Analytical methods
Direct sequencing and DHPLC (only for MYBPC3 until the end of 2010). MLPA is also being used.
1.7 Analytical validation
Sequencing of both strands. When a mutation is identified, one should validate the mutation in an independent experiment by direct sequencing using a freshly prepared DNA dilution.
1.8 Estimated frequency of the disease
(incidence at birth (‘birth prevalence') or population prevalence)
Estimated that one in 500 individuals is phenotypically affected in the general population worldwide.1, 2, 3, 4, 5
1.9 If applicable, prevalence in the ethnic group of investigated person
There seems to be no clear differences in the HCM prevalence between different ethnicities.
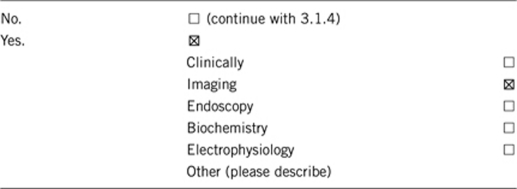
1.10 Diagnostic setting

Comment: The two most frequently mutated genes are MYBPC3 and MYH7.6 Most of the HCM CMH patients are heterozygous for a mutation, but in 3–5% of the cases, patients carry two mutations in the same gene (compound heterozygous or homozygous), or in different genes (digenic). In general, this is associated with a more severe phenotype with younger age of onset and more adverse events, suggesting a gene-dosage effect.6, 7, 8, 9, 10
2. TEST CHARACTERISTICS
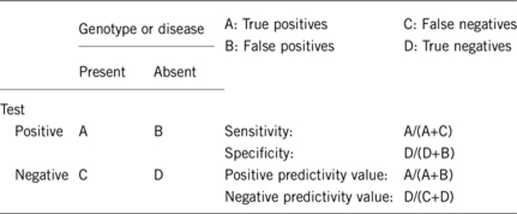
2.1 Analytical sensitivity
(proportion of positive tests if the genotype is present)
Almost 100%. Preferential amplification of one allele can happen when one of the primers is located on a SNP. We try to minimise this by checking the primers in SNP databases every other year.
2.2 Analytical specificity
(proportion of negative tests if the genotype is not present)
Almost 100%.
2.3 Clinical sensitivity
(proportion of positive tests if the disease is present)
The clinical sensitivity can be dependent on variable factors such as age or family history. In such cases, a general statement should be given, even if a quantification can only be made case by case.
Many genes involved with mutation frequencies ranging between 30% and rare (local data and literature). On average, the mutation detection rate for the most obvious set of five candidates is about 56% (MYBPC3:20–30% MYH7:20–30% TNNT2:3–5% TNNI3:3–5% TPM1:1–3%).11, 12, 13
2.4 Clinical specificity
(proportion of negative tests if the disease is not present)
The clinical specificity can be dependent on variable factors such as age or family history. In such cases, a general statement should be given, even if a quantification can only be made case by case.
Probably 100%, but no data available for this measure. Might be a little bit less because of the reduced penetrance of HCM.
2.5 Positive clinical predictive value
(life-time risk to develop the disease if the test is positive).
Almost 100% in advanced age. HCM has an age-related pentrance. This penetrance is depending on the individual mutation and/or the gene that is affected and is, in general, steadily increasing until advanced age; see ref. 13 for a review.
2.6 Negative clinical predictive value
(probability not to develop the disease if the test is negative).
Assume an increased risk based on family history for a non-affected person. Allelic and locus heterogeneity may need to be considered.
Index case in that family had been tested:
If a pathogenic mutation is found in the index and this mutation was not found in another family member, then this member has a <5% change of carrying another HCM-causing mutation.
Index case in that family had not been tested:
If the patient has a clinical diagnosis of HCM he/she has a >90% chance of having a genetic mutation. Therefore, the chance that another family member will develop HCM once in his/her life will be close to 50%.
3. CLINICAL UTILITY
3.1 (Differential) diagnosis: the tested person is clinically affected
(To be answered if in 1.10, ‘A' was marked)
3.1.1 Can a diagnosis be made other than through a genetic test?
Comment: The diagnosis of HCM CMH is a clinical one, made on the basis of an increased ventricular wall thickness (15 mm or more, or 13 mm or more in relatives of an HCM patient) in the absence of abnormal-loading conditions (arterial hypertension, valve disease), sufficient to cause the observed abnormality.14 Wall thickness is assessed using echocardiography or cardiac magnetic resonance imaging. Owing to age-dependant penetrance, a negative clinical test does not exclude the possibility of developing HCM CMH at a later age.
3.1.2 Describe the burden of alternative diagnostic methods to the patient
Echocardiography and magnetic resonance imaging are non-invasive procedures with negligible risks and little inconvenience to the patient.
3.1.3 How is the cost effectiveness of alternative diagnostic methods to be judged?
When a disease-causing mutation is identified in the index patient, genetic testing can be offered to apparently healthy relatives within the family to determine whether they carry the same mutation and are at risk of developing the disease in the future. If the relative carries the mutation, then regular medical follow-up is required to detect early cardiac disease, and thereby improve their management. Specific advice to gene carriers might include restriction of physical activity (especially competitive sport), avoidance of specific careers, and reproductive counselling.
If a relative does not carry the mutation then they can be reassured and cardiological follow-up discontinued (provided that severity of the phenotype in any family member does not suggest multiple genetic events). Recent evidence indicates that this strategy is highly cost-effective.15 An important feature highlighted by this study is the potential for molecular genetic testing to discharge those without a disease-causing mutation who may have had an ambiguous, or even false positive clinical tests requiring ongoing clinical surveillance. It is estimated that by introducing genetic testing, 13% of patients will be discharged from routine follow-up care.
3.1.4 Will disease management be influenced by the result of a genetic test?

3.2 Predictive setting: the tested person is clinically unaffected, but carries an increased risk based on family history
(To be answered if in 1.10, ‘B' was marked)
3.2.1 Will the result of a genetic test influence lifestyle and prevention?
If the test result is positive, regular cardiological evaluation is advised to detect clinical signs of HCM CMH and to estimate the risk of sudden cardiac death. Intense physical activity (eg, burst activities, sprinting), or systematic isometric exercise (eg, heavy lifting) will be discouraged.
If the test result is negative (please describe), relatives without the mutation can be discharged form cardiological follow-up. Carriers of mutations will receive reproductive counselling on the risk of transmission to their own offspring.
3.2.2 Which options in view of lifestyle and prevention do a person at-risk have if no genetic test has been done (please describe)?
Advice given will be the same as with a positive genetic test.
3.3 Genetic risk assessment in family members of a diseased person
(To be answered if in 1.10, ‘C' was marked)
Predictive genetic testing of relatives is only possible if a pathogenic mutation has been identified in an affected person in the family. Autosomal dominant inheritance implies a 50% risk of being a carrier of the pathogenic mutation in first-degree relatives of a person with the disease.
3.3.1 Does the result of a genetic test resolve the genetic situation in that family?
This is only possible if the mutation in the affected proband is detected (35–65%).16, 17 Otherwise, relatives are advised to undergo regular cardiological evaluation.
3.3.2 Can a genetic test in the index patient save genetic or other tests in family members?
Yes, it will be cost effective. A negative test result in the index patient does not mean the disease is not hereditary. On the other hand, a positive genetic test result implies the possibility of predictive genetic testing in relatives. Relatives being non-carrier of the pathogenic mutation can be excluded from repeated cardiological follow-up and this will mean saving the costs of ECG and echocardiography. In case of a negative genetic test in the index patient, all relatives are advised to continue regular cardiological follow-up.
3.3.3 Does a positive genetic test result in the index patient enable a predictive test in a family member?
Yes, when a pathogenic mutation is detected.
3.4 Prenatal diagnosis
(To be answered if in 1.10, ‘D' was marked)
Prenatal genetic diagnosis in HCM is rarely performed,10 and is not actively offered to parents, in common, with other late-onset genetic diseases. Prenatal diagnostics in HCM is only possible when a pathogenic mutation has been detected in the family.
3.4.1 Does a positive genetic test result in the index patient enable a prenatal diagnostic?
Yes, but prenatal diagnostics is not actively offered.
4. If applicable, further consequences of testing
Please assume that the result of a genetic test has no immediate medical consequences. Is there any evidence that a genetic test is nevertheless useful for the patient or his/her relatives? (Please describe)
Acknowledgments
This work was supported by the EuroGentest, an EU-FP6 supported NoE, contract number 512148 (EuroGentest unit 3: ‘Clinical genetics, community genetics, and public health', Workpackage 3.2).
The authors declare no conflict of interest.
References
- Hada Y, Sakamoto T, Amano K, et al. Prevalence of hypertrophic cardiomyopathy in a population of adult Japanese workers as detected by echocardiographic screening. Am J Cardiol. 1987;59:183–184. doi: 10.1016/s0002-9149(87)80107-8. [DOI] [PubMed] [Google Scholar]
- Maron BJ, Peterson EE, Maron MS, et al. Prevalence of hypertrophic cardiomyopathy in an outpatient population referred for echocardiographic study. Am J Cardiol. 1994;73:577–580. doi: 10.1016/0002-9149(94)90337-9. [DOI] [PubMed] [Google Scholar]
- Maron BJ, Gardin JM, Flack JM, et al. Prevalence of hypertrophic cardiomyopathy in a general population of young adults echocardiographic analysis of 4111 subjects in the CARDIA study. Coronary artery risk development in (young) adults. Circulation. 1995;92:785–789. doi: 10.1161/01.cir.92.4.785. [DOI] [PubMed] [Google Scholar]
- Zou Y, Song L, Wang Z, et al. Prevalence of idiopathic hypertrophic cardiomyopathy in China: a population-based echocardiographic analysis of 8080 adults. Am J Med. 2004;116:14–18. doi: 10.1016/j.amjmed.2003.05.009. [DOI] [PubMed] [Google Scholar]
- Morita H, Larson MG, Barr SC, et al. Single-gene mutations and increased left ventricular wall thickness in the community: the Framingham Heart Study. Circulation. 2006;113:2697–2705. doi: 10.1161/CIRCULATIONAHA.105.593558. [DOI] [PubMed] [Google Scholar]
- Richard P, Charron P, Carrier L, et al. Hypertrophic cardiomyopathy: distribution of disease genes, spectrum of mutations, and implications for a molecular diagnosis strategy. Circulation. 2003;107:2227–2232. doi: 10.1161/01.CIR.0000066323.15244.54. [DOI] [PubMed] [Google Scholar]
- Richard P, Isnard R, Carrier L, et al. Double heterozygosity for mutations in the beta-myosin heavy chain and in the cardiac myosin binding protein C genes in a family with hypertrophic cardiomyopathy. J Med Genet. 1999;36:542–545. [PMC free article] [PubMed] [Google Scholar]
- Ho CY, Lever HM, DeSanctis R, et al. Homozygous mutation in cardiac troponin T: implications for hypertrophic cardiomyopathy. Circulation. 2000;102:1950–1955. doi: 10.1161/01.cir.102.16.1950. [DOI] [PubMed] [Google Scholar]
- Richard P, Charron P, Leclercq C, et al. Homozygotes for a R869G mutation in the beta-myosin heavy chain gene have a severe form of familial hypertrophic cardiomyopathy. J Mol Cell Cardiol. 2000;32:1575–1583. doi: 10.1006/jmcc.2000.1193. [DOI] [PubMed] [Google Scholar]
- Lekanne Deprez RH, Muurling-Vlietman JJ, Hruda J, et al. Two cases of severe neonatal hypertrophic cardiomyopathy caused by compound heterozygous mutations in the MYBPC3 gene. J Med Genet. 2006;43:829–832. doi: 10.1136/jmg.2005.040329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marian AJ. Hypertrophic cardiomyopathy: from genetics to treatment. Eur J Clin Invest. 2010;40:360–369. doi: 10.1111/j.1365-2362.2010.02268.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Langen Im, Arens Y, Baars H, et al. Genetic diagnostics and genetic counselling in hypertrophic cardiomyopathy (HCM) Neth Heart J. 2010;18:144. doi: 10.1007/BF03091753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keren A, Syrris P, McKenna WJ. Hypertrophic cardiomyopathy: the genetic determinants of clinical disease expression. Nat Clin Pract Cardiovasc Med. 2008;5:158–168. doi: 10.1038/ncpcardio1110. [DOI] [PubMed] [Google Scholar]
- Elliott PM, Andersson B, Arbustini E, et al. Classification of the cardiomyopathies: a position statement from the European Society Of Cardiology Working Group on myocardial and pericardial diseases. Eur Heart J. 2008;29:270–276. doi: 10.1093/eurheartj/ehm342. [DOI] [PubMed] [Google Scholar]
- Wordsworth S, Leal J, Blair E, et al. DNA testing for hypertrophic cardiomyopathy: a cost-effectiveness model. Eur Heart J. 2010;31:926–935. doi: 10.1093/eurheartj/ehq067. [DOI] [PubMed] [Google Scholar]
- Marian AJ, Roberts R. The molecular genetic basis for hypertrophic cardiomyopathy. J Mol Cell Cardiol. 2001;33:655–670. doi: 10.1006/jmcc.2001.1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Driest SL, Ommen SR, Tajik AJ, et al. Sarcomeric genotyping in hypertrophic cardiomyopathy. Mayo Clin Proc. 2005;80:463–469. doi: 10.1016/S0025-6196(11)63196-0. [DOI] [PubMed] [Google Scholar]


