Abstract
Restrictions in ankle dorsiflexion range of motion (ROM) have been associated with decreased posterior talar glide in individuals with an acute lateral ankle sprain. Talocrural joint mobilizations may be used to restore joint arthrokinematics. Our purpose was to examine the effects of a single bout of anterior to posterior (AP) talocrural joint mobilization on self-reported function, dorsiflexion ROM, and posterior talar translation in individuals with an acute lateral ankle sprain. This single-blinded, randomized controlled trial utilized 17 volunteers (nine treatment and eight control) with an acute lateral ankle sprain (grade I/II) who were immobilized for a period of 1–7 days. The treatment group received a single 30-second bout of grade III AP talocrural joint mobilization the day their immobilization device was removed, while the control group did not receive any intervention. Active dorsiflexion ROM and posterior talar translation were assessed before, immediately after, and 24 hours after receipt of the treatment or control interventions. Self-reported function and pain were assessed before and 24 hours after the receipt of the treatment or control interventions using the foot and ankle disability index. Collectively all groups demonstrated improved dorsiflexion ROM and self-reported function. There was a significant decrease in pain perception at 24-hour follow-up for the treatment group. A single bout of AP talocrural joint mobilizations may not have an immediate effect on ankle dorsiflexion ROM, posterior talar translation, or self-reported function; however, they may have an immediate effect on pain perception in individuals with an acute lateral ankle sprain.
Keywords: Arthrokinematics, Ankle sprain, Talocrural joint mobilization, Dorsiflexion, Self-reported function
Introduction
Decreased ankle dorsiflexion range of motion (ROM) is a common lingering impairment following lateral ankle sprains1–3 which can impact both walking2 and running gait patterns.2 This impairment may also increase susceptibility to re-injury. Limited ankle dorsiflexion ROM may be due to osteokinematic or arthrokinematic restrictions. Although osteokinematic ankle dorsiflexion ROM may be restored following lateral ankle sprains, arthrokinematic restrictions may still be present.4 Altered joint arthrokinematics can ultimately impact gait and are thought to be associated with increased risk of ankle osteoarthritis.5–7 Following a lateral ankle sprain, it has been reported that participants present with decreased dorsiflexion ROM2 and posterior talar glide.8 Limited dorsiflexion ROM has been associated with a lack of posterior glide of the talus on the tibia in participants suffering from ankle sprain.3,8
It has been hypothesized that the lack of posterior talar glide may be associated with a positional fault, specifically anterior positioning of the talus, following lateral ankle sprains due to the disruption of the ligaments restraining anterior talus translation.3,8,9 These individuals would demonstrate decreased ankle dorsiflexion ROM and would be thought to benefit from joint mobilization. When applied to an injured joint, joint mobilizations can be used to reduce pain and improve joint arthrokinematics.10 Previous studies have used a grade III anterior to posterior (AP) talocrural joint mobilization to increase dorsiflexion ROM in participants with a history of lateral ankle sprain and to reduce pain.2,3,11 Increases in dorsiflexion ROM and decreases in self-reported pain following a grade II AP talocrural joint mobilization have been reported after 1 week of treatment in participants recovering from acute ankle sprain; however, there is not a clear understanding of mechanisms by which joint mobilizations influence these changes.
The immediate effects of grade III AP talocrural mobilization on dorsiflexion ROM have been examined in participants with recurrent ankle sprain and other lower extremity injuries.3,11 It was reported that following grade III AP talocrural joint mobilizations participants in the treatment group demonstrated increases in posterior talar glide when measured manually and improvements in dorsiflexion ROM.1–3 Similarly, a single 30-second bout of grade III AP joint mobilizations in patients with a variety of foot and ankle injuries who were immobilized for at least 10 days resulted in immediate improvements in dorsiflexion ROM.9 These changes were accompanied by a reduction in the magnitude of posterior talar glide, as assessed with an ankle arthrometer, suggesting a correction of an anterior positional fault of the talus after AP mobilization.9 There is no such research to date on patients recovering from acute ankle sprains.9
While the effects of AP talocrural joint mobilizations on dorsiflexion ROM have been previously assessed, there has been no prior research conducted on the immediate mechanistic effects of AP talocrural joint mobilizations in acute lateral ankle sprain patients. Understanding the immediate effects of grade III AP talocrural joint mobilizations on patients with acute ankle sprains may be of particular importance to sports medicine clinicians who are concerned about returning injured athletes quickly, but safely, for return to play. Therefore, the purpose of this study was to examine the immediate effects of a single bout of grade III AP talocrural joint mobilizations on ankle dorsiflexion ROM, posterior talar translation, self-reported function and pain in individuals with an acute lateral ankle sprain.
Methods
Study design
This was a single blinded randomized controlled trial with two levels of independent variables, group at two levels (treatment or control) and time at three levels (baseline, post-treatment, and 24-hour follow-up). Four dependent variables were measured: ankle dorsiflexion ROM, posterior talar translation, self-reported function, and pain.
Participants
Seventeen individuals (nine treatment and eight control) with an acute lateral ankle sprain (grade I/II), who had previously been immobilized in a walking boot, participated in this study. Inclusion criteria for this study required that the participants be between the ages of 18 and 45 years, incur a lateral ankle sprain (grade I/II) requiring immobilization for a minimum of 24 hours and a maximum of 7 days, and present with a 5° deficit in dorsiflexion ROM. Participants were excluded from the study if they had a history of ankle surgery that involved intra-articular fixation, suffered from a syndesmotic ankle sprain, had a history or signs of reflex sympathetic dystrophy, or had received manual therapy for the ankle sprain prior to enrollment. All participants signed consent forms approved by the university institutional review board for health sciences research.
Procedures
Participants were randomly assigned to the control group or the treatment group, using sealed envelope allocation. A computer-generated randomization schedule was made by the senior author and the sealed envelopes were given to the clinician who administered the treatments. All participants remained in the same allocation throughout the study and the examiner who measured all outcomes was blinded to the group assignment of subjects. Each participant underwent three testing sessions (baseline, immediate post-treatment, and 24-hour follow-up). Each session included measurements of ankle dorsiflexion ROM in a non-weight bearing seated position and posterior talar translation assessed using an ankle arthrometer. Participants also completed the foot and ankle disability index (FADI) and foot and ankle disability index – sport (FADI-sport) prior to the removal of the immobilization device and at 24-hour follow-up.
Dorsiflexion ROM
The dorsiflexion ROM measurement was taken with the participant seated; the knee in terminal extension, and the bubble inclinometer placed over the fifth metatarsal using a Velcro strap (see Fig. 1).8 The participant was instructed to actively dorsiflex the talocrural joint maximally. Once the participant was at their reported end range, the angle of dorsiflexion was recorded. The mean of three measurements was used an outcome variable.4 Measurement of dorsiflexion in this position has been reported to have excellent intraclass correlation coefficients (0·96–0·98).8
Figure 1.
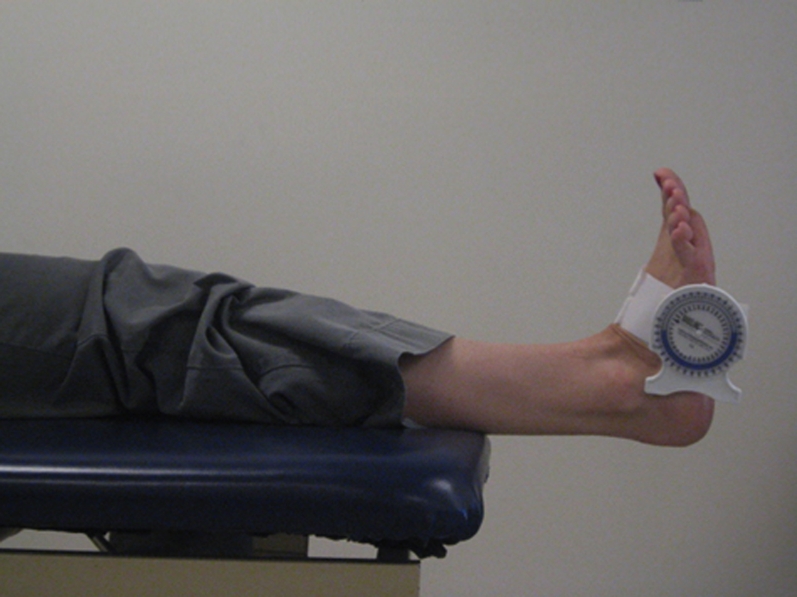
Straight knee measurement of active dorsiflexion ROM with bubble inclinometer.
Posterior talar translation
Testing was conducted using a portable ankle arthrometer (Blue Bay Research Inc., Navarre, FL, USA). A computer with an analog-to-digital converter was used to simultaneously record and calculate translation (mm) and load (N). A custom software program written in LabView (National Instruments Corp., Austin, TX, USA) was used for data collection. Participants were placed in a supine position with a styrofoam bolster placed under the knee of the test limb to standardize knee flexion angle between all participants. Adhesive spray was applied to the test ankle as well as the arthrometer to minimize foot movement during testing. With the ankle in a neutral position, a posteriorly directed force of 170 N was applied to the talus (Fig. 2). Posterior translation of the talus was measured in millimeters (mm) and the mean of three measures was used for data analysis.11
Figure 2.

Measurement of posterior talar translation using the instrumented ankle arthrometer (170 N).
Self-reported function
Self-reported function and pain were measured using the FADI and FADI-sport.12 Measurements were taken at baseline and at 24-hour follow-up. Pain perception was measured using the pain subscale within the foot and ankle disability index – activities of daily living (FADI-ADL). The minimally clinically important differences (MCIDs) for the ADL and sport subscales have been reported to be 8 and 9%, respectively.13 The FADI has 26 items, and the FADI-sport has eight. Each item is scored from 0 (unable to do) to 4 (no difficulty at all). The four pain questions of the FADI are scored from 0 (none) to 4 (unbearable), with lower scores within this subscale indicating decreased pain perception.13 The FADI has a total point value of 104 points, whereas the FADI-sport has a total point value of 32 points. The FADI and FADI-sport are scored separately as percentages, with 100% representing no dysfunction.12 The FADI and FADI-sport have good to excellent intersession reliability, with intraclass correlation coefficients of 0·85–0·98 and 0·67–0·98, respectively.12
Intervention
Following arthrometer testing, a physical therapist, with over 5 years of experience in performing joint mobilizations, entered the treatment area to provide the randomly allocated treatment for each participant. The intervention group received a 30-second bout of grade III AP talocrural joint mobilizations performed at a rate of ∼1 mobilization/second. Control participants were given no treatment and received no physical contact from the treating clinician.
Following the intervention, the examiner returned and a second series of measurements were obtained in the same manner and order as baseline measures. The participant was then instructed to return to activities of daily living without the immobilization device. Each participant and their treating clinician were instructed to exclude AP talocrural joint mobilizations from their treatment protocol. Participants in both groups were allowed to receive the standard of care, which included: rest, ice, compression, and elevation;2 and also participated in ankle strengthening and proprioceptive exercises.
Twenty-four-hour follow-up
Following 24 hours of unrestricted ambulation, the participant returned, was asked to complete the FADI and FADI-sport, and underwent a final series of ROM and arthrometer testing.
Statistical analysis
The five dependent variables were ankle dorsiflexion ROM, posterior talar translation, and self-reported function as measured by the FADI-ADL, FADI-sport, and foot and ankle disability index – pain (FADI-pain) subscales. The independent variables were treatment group (control and treatment), and time (baseline, post-treatment, and 24-hour follow-up). For dorsiflexion ROM and posterior talar translation, a 2×3 mixed model analysis of variance (ANOVA) was run to determine the influence of a single bout of grade III AP talocrural joint mobilizations. For self-reported function, a 2×2 repeated measures ANOVA was run because these measures were only taken at baseline and 24-hour follow-up. A separate 2×2 repeated measures ANOVA was run to determine the immediate effects of grade III AP talocrural joint mobilizations on pain perception, using the pain subscale components of the FADI-ADL. In the event of a significant interaction or main effect, Tukey’s post hoc tests were computed to identify specific differences. Cohen’s d effect measures were determined by calculating the mean difference between and within groups immediately after the intervention and at 24-hour follow-up, and dividing it by the reference SD (control group or baseline measures). The strength of the effect size was interpreted as trivial (<0·20), small (0·21–0·40), moderate (0·41–0·7), and large (⩾0·71). All analyses were performed using SPSS 17·0 (SPSS Inc., Chicago, IL, USA), and the alpha level was set a priori at P⩽0·05.
Results
Seventeen individuals completed the study and had a mean age of 19·76±1·35 years, mean height of 69·10±4·31 cm, and mean mass of 71·34±16·45 kg. Descriptive statistics and effect sizes for each outcome measure are presented in Tables 1 and 2, respectively. For the dorsiflexion ROM, there was not a significant group by time interaction (F2,30 = 0·17, P = 0·85, 1-beta = 0·07) or group main effect (F2,30 = 0·21, P = 0·66, 1-beta = 0·07); however, there was a significant main effect for time (F2,30 = 3·67, P = 0·04, 1-beta = 0·63). When both groups were pooled together, there was a significant improvement in dorsiflexion ROM from baseline to 24-hour follow-up; however, there was not a significant improvement in dorsiflexion ROM attributable to the joint mobilization treatment (Fig. 3).
Table 1. Ankle dorsiflexion ROM, posterior talar translation, and self-reported function (mean±SD).
| Control group |
Treatment group |
P value |
|||||||
| Baseline | Post-treatment | 24-hour follow-up | Baseline | Post-treatment | 24-hour follow-up | Time | Group | Time×group | |
| Dorsiflexion ROM* (°) | 7·36±6·38 | 8·5±4·02 | 9·94±4·0 | 6·49±6·43 | 6·62±7·34 | 8·82±7·29 | 0·04* | 0·65 | 0·85 |
| Posterior talar translation (mm) | 5·86±2·81 | 5·34±2·98 | 6·95±3·64 | 7·09±3·54 | 6·86±3·69 | 7·06±2·99 | 0·43 | 0·51 | 0·57 |
| FADI-ADL* (%) | 72·76±18·7 | … | 82·09±9·99 | 62·29±17·63 | … | 75·85±15·15 | 0·004 | 0·24 | 0·52 |
| FADI-sport (%) | 14·06±6·33 | … | 20·13±5·72 | 14·93±5·96 | … | 19·79±5·72 | 0·15 | 0·99 | 0·85 |
| FADI-pain (%) | 81·25±14·94 | … | 80·47±7·04 | 72·22±10·87 | … | 84·03±14·36 | 0·03 | 0·96 | 0·03†† |
Note: FADI-ADL = foot and ankle disability index – activities of daily living; FADI-pain = foot and ankle disability index – pain; FADI-sport = foot and ankle disability index – sport; mm = millimeters; ROM = range of motion.
*Significant time main effect for dorsiflexion and FADI-ADL, P<0·05.
†Significant group by time interaction for pain.
Table 2. Between group and time Cohen’s d effect sizes, with 95% CI*.
| Control group time effect (95% CI) |
Treatment group time effect (95% CI) |
Between group effect size (95% CI) |
||||
| Baseline–post-treatment | Baseline–24-hour follow-up | Baseline–post-treatment | Baseline–24-hour follow-up | Post-treatment | 24-hour follow-up | |
| Dorsiflexion ROM† (°) | 0·18 (−0·80, 1·16) | 0·40 (−0·59, 1·39) | 0·02 (−0·90, 0·94) | 0·36 (−0·57, 1·29) | 0·26 (−0·70, 1·21) | −0·28 (−1·24, 0·68) |
| Posterior talar translation (mm) | −0·19 (−1·17, 0·80) | 0·39 (−0·60, 1·38) | −0·06 (−0·99, 0·86) | −0·01 (−0·93, 0·92) | 0·51 (−0·46, 1·48) | 0·03 (−0·92, 0·98) |
| FADI-ADL† (%) | … | 0·50 (−0·50, 1·49) | … | 0·77 (−0·19, 1·73) | … | −0·62 (−1·60, 0·35) |
| FADI-sport (%) | … | 0·96 (−0·08, 1·99) | … | 0·82 (−0·15, 1·78) | ... | −0·06 (−1·01, 0·89) |
| FADI-pain (%) | … | −0·05 (−1·03, 0·93) | … | 1·09† (0·10, 2·08) | … | 0·51 (−0·46, 1·47) |
Note: CI = confidence interval; FADI-ADL = foot and ankle disability index – activities of daily living; FADI-pain = foot and ankle disability index – pain; FADI-sport = foot and ankle disability index – sport; mm = millimeters; ROM = range of motion.
*Group effect sizes were calculated from baseline to immediately after treatment and from baseline to 24-hour follow-up. Time effect sizes were calculated from baseline to immediately after treatment and from baseline to 24-hour follow-up for both groups.
†Large effect size where 95% CIs do not cross zero.
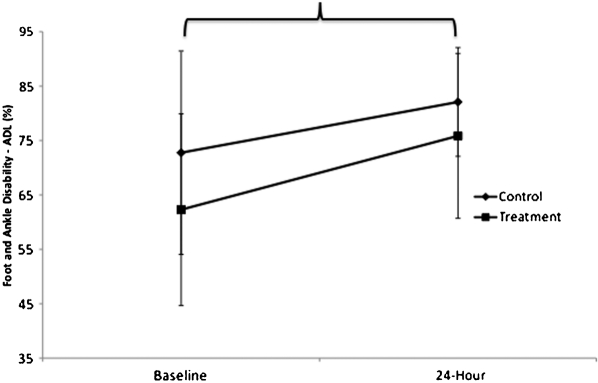
Figure 3.
Dorsiflexion ROM means (±SE) for both groups at each testing session. There was a significant main effect for time (P = 0·037), indicating that when the groups were pulled together they had increases in their ROM regardless of group assignment.
For the posterior talar translation measures, there was not a significant group by time interaction (F2,30 = 0·58, P = 0·57, 1-beta = 0·14), group main effect (F2,30 = 0·45, P = 0·51, 1-beta = 0·10), or time main effect (F2,30 = 0·86, P = 0·43, 1-beta = 0·18). These results indicate that there was no significant change in talar translation immediately following the intervention or at 24-hour follow-up.
For the FADI-ADL and FADI-sport, there were no significant group by time interactions (F1,15 = 0·43, P = 0·52, 1-beta = 0·09; F1,15 = 0·04, P = 0·85, 1-beta = 0·05, respectively) or group main effects (F1,15 = 1·51, P = 0·24, 1-beta = 0·21; F1,15 = 0·00, P = 0·99, 1-beta = 0·05). There was a significant main effect for time for the FADI-ADL (F1,15 = 11·28, P = 0·004, 1-beta = 0·88), but not for the foot and ankle ability measure – sport (F1,15 = 2·25, P = 0·15, 1-beta = 0·29). When both groups were pooled together, there was a significant increase in the self-reported function on the FADI-ADL subscale at the 24-hour follow-up (Fig. 3). There was a significant group by time interaction (F1,15 = 5·58, P = 0·04, 1-beta = 0·60) for the FADI-ADL pain subscale (Fig. 4). Paired samples t-tests revealed a 20% reduction in pain (t8 = −3·74, P = 0·006) for the treatment group following a single bout of grade III AP talocrural joint mobilizations at 24-hour follow-up when compared to the control group (t7 = 0·00, P = 1·0).
Figure 4.
FADI-ADL means (±SE) for both groups at each testing session. There was a significant main effect for time (P = 0·004), indicating that when the groups were pooled together, they had improvements in their self-reported function regardless of group assignment.
Figure 5.
FADI-pain subscale means (±SE) for both groups at each testing session. There was a significant group×time interaction (P = 0·04), indicating a decrease in pain perception following the intervention in the experimental group. *Significant improvement in pain from baseline to 24-hour follow-up for the treatment group.
Discussion
In this study of acute ankle sprain participants who were recently removed from ankle immobilization, a single bout of a grade III AP talocrural joint mobilizations did not significantly alter dorsiflexion ROM, posterior talar translation, or self-reported function immediately following the intervention or at 24-hour follow-up. Following the removal of the immobilization device, both the treatment and control groups had improvements in dorsiflexion ROM and self-reported function as measured by the FADI-ADL subscale at 24-hour follow-up.
In our study, both groups had increases in their dorsiflexion ROM at 24-hour follow-up; however, there was no difference in the change of dorsiflexion ROM between the treatment group who received the joint mobilization and the control group. The results of this study are in contrast to previous literature, which have reported significant differences between ankle-injured individuals who received grade III AP talocrural joint mobilizations and those who did not;2,11 however, methodological differences may explain this discrepancy. The mean baseline dorsiflexion ROM for the control group was approximately 7·36±6·38° and for treatment group was 6·62±6·43°, which is consistent with previous reported research where the observed baseline dorsiflexion values were ∼7 and 9° for the control and treatment group, respectively and used an acute lateral ankle sprain population.2 It has been reported that following a single bout and multiple bouts of a grade III AP talocrural joint mobilization observed greater changes in dorsiflexion ROM following the application of the joint mobilization in the treatment group when compared to injured controls.2,11 We did not observe differences between groups in dorsiflexion ROM following the application of the joint mobilization in this study. This finding may suggest that a single bout of AP talocrural joint mobilizations when applied to the talocrural joint may not restore a positional fault and may not be enough to cause improvements in dorsiflexion ROM in an acute lateral ankle sprain population. This finding can be supported by the trivial to small effect sizes that were observed between (0·26, −0·28) and within (0·02–0·40) the groups at each follow-up period (Table 2). Multiple bouts of grade III AP talocrural joint mobilizations in patients with acute lateral ankle sprains have been reported to increase dorsiflexion ROM and to return individuals to activity quicker than those in the control group.2 These results suggest that in order to improve dorsiflexion ROM, multiple bouts of AP talocrural joint mobilizations may be needed to improve dorsiflexion ROM in the acute lateral ankle sprain population.2
There was no change in posterior talar translation immediately post-treatment or following 24 hours of ambulation. These results are consistent with previous literature11 which observed a trend towards a decrease in posterior talar translation following a single 30-second bout of an AP joint mobilization. We hypothesized that following a single bout of grade III AP talocrural joint mobilization, posterior talar glide would be decreased. If an anterior positional fault at the talocrural joint was present in this particular group of participants decreases in posterior talar translation following a grade III AP talocrural joint mobilization could be as a result of the talus being more anterior prior to the treatment and being repositioned following a single bout of grade III AP talocrural joint mobilization, thus resulting in less posterior translation.11 Several studies have identified an anterior positional fault at the talocrural joint following lateral ankle sprain;3,4,11 however, none of these studies have used an acute lateral ankle sprain population. Factors that could have played a role in the lack of differences between the treatment and control groups in this study include muscle spasm, increased muscle activity in the lower leg, pain, and the dose and length of the treatment being administered. It has been reported that multiple bouts of joint mobilizations are effective at increasing dorsiflexion ROM; the results of this study suggest that improvements in dorsiflexion ROM do not occur within one session and that the dose and the length of the treatment may need to be longer to observe mechanical differences between the treatment and control groups.2
To our knowledge, this is the first study to examine the immediate effects of joint mobilizations on self-reported function in individuals with acute lateral ankle sprains. It has been reported in the ankle literature that following rehabilitation individuals suffering from chronic ankle instability reported improvements in self-reported function as measured by the foot and ankle ability measure – activities of daily and sport subscales.7–9,14 The MCID has been reported to be 8 and 9% on the ADL and sport subscales, respectively.13 At 24-hour follow-up participants in the treatment and control group surpassed the MCID for the ADL subscale, with the control group reporting improvement by 10% and the treatment group reporting a 15% improvement (Table 1). The improvement of self-reported function as measured by the ADL subscale can be potentially explained by improvements in motion following the removal of the immobilization device.
Changes in self-reported function as measured by the sport subscale were not significant and did not meet the MCID of 8%, with the control group improving by 6% and the treatment group reporting a 5% improvement. The FADI-sport subscale values for this particular group of ankle injured participants at baseline and 24-hour follow-up are lower than previously reported values in an acutely ankle injured population.15 The sports subscale consists of eight questions related to cutting, jumping, and running and other sports related activities. Participants in this study, following the removal of the immobilization device could have still been in the acute or subacute phase of healing; therefore, it is highly unlikely that they would be confident in their ability to perform such sport related activities. Therefore, differences or changes in the sport subscale were not expected to change in such a short follow-up time. It has been reported at 8-week follow-up that scores on the FADI-ADL and FADI-sport were significantly lower in patients with acute lateral ankle sprains when compared to healthy patients.15 The results of this study suggest that more time may be needed to observe improvements in self-reported function as measured with the foot and ankle ability measure – sport subscale.
When examining the four pain questions embedded in the FADI-ADL subscale, we did observe a significant group by time interaction. These results are similar to previous joint mobilization literature2 in patients with acute lateral ankle sprains, which found a significant decrease in pain perception following the intervention. In the present study, a single 30-second bout of a grade III AP talocrural joint mobilization was not enough to produce a change in dorsiflexion ROM; however, our findings suggest that a single 30-second bout of grade III AP talocrural joint mobilizations was effective at improving pain perception by eliciting a neurophysiologic response at the talocrural joint in the intervention group. Clinically, a single bout of a grade III AP talocrural joint mobilization may allow clinicians a small window of opportunity to restore ROM while working in pain free environment. The effect size for the baseline to 24-hour change for the treatment group on the pain questions within the FADI was 1·09, which suggests that the clinical magnitude of a single bout of AP talocrural joint mobilizations was strong.
A limitation of this study was that it only examined the effects of a single bout of joint mobilizations over a 24-hour period. Additional research should examine long-term effects, including both mechanistic properties and participant functional outcomes, of multiple applications of joint mobilizations in individuals recovering from an acute lateral ankle sprain. Second, the use of a clinical test to quantify posterior talar glide following lateral ankle sprain was not used in this study. The posterior talar glide test has been used to quantify changes in posterior talar glide following a lateral ankle sprain or a joint mobilization treatment.3,8 These authors were able to detect changes in talar glide in individuals who had suffered from a lateral ankle sprain and received a mobilization treatment using the posterior talar glide test. Future research should examine the intra- and intertester reliability and examine the relationships between posterior talar glide as measured with the instrumented ankle arthrometer and the posterior talar glide test. Third, we acknowledge that the sample size for the control and treatment groups was relatively small, increasing the risk of a type II error; however, the magnitude of change for dorsiflexion ROM and posterior talar translation as represented with effect size was trivial to small; therefore, the risk of a type II error is unlikely.
Conclusion
A single bout of a grade III AP talocrural joint mobilization was not effective at increasing ankle dorsiflexion ROM, decreasing posterior talar glide, or improving self-reported function in individuals with an acute lateral ankle sprain when compared to controls. Following the removal of the immobilization device, dorsiflexion ROM improved for both groups at 24-hour follow-up, and there was an improvement in self-reported function as reported by the ADL subscale of the FADI. These results suggest that there was a restoration of function and ROM at the ankle joint when participants were allowed to ambulate for 24 hours. While there were no immediate changes in motion, individuals in the treatment group did demonstrate decreased pain over 24 hours.
References
- 1.Collins N, Teys P, Vicenzino B. The initial effects of a Mulligan’s mobilization with movement technique on dorsiflexion and pain in subacute ankle sprains. Man Ther 2004;9(2):77–82 [DOI] [PubMed] [Google Scholar]
- 2.Green T, Refshauge K, Crosbie J, Adams R. A randomized controlled trial of a passive accessory joint mobilization on acute ankle inversion sprains. Phys Ther 2001;81(4):984–94 [PubMed] [Google Scholar]
- 3.Vicenzino B, Branjerdporn M, Teys P, Jordan K. Initial changes in posterior talar glide and dorsiflexion of the ankle after mobilization with movement in individuals with recurrent ankle sprain. J Orthop Sports Phys Ther 2006;36(7):464–71 [DOI] [PubMed] [Google Scholar]
- 4.Denegar CR, Hertel J, Fonseca J. The effect of lateral ankle sprain on dorsiflexion range of motion, posterior talar glide, and joint laxity. J Orthop Sports Phys Ther 2002;32(4):166–73 [DOI] [PubMed] [Google Scholar]
- 5.Gross P, Marti B. Risk of degenerative ankle joint disease in volleyball players: study of former elite athletes. Int J Sports Med 1999;20(1):58–63 [DOI] [PubMed] [Google Scholar]
- 6.Valderrabano V, Hintermann B, Horisberger M, Fung TS. Ligamentous posttraumatic ankle osteoarthritis. Am J Sports Med 2006;34(4):612–20 [DOI] [PubMed] [Google Scholar]
- 7.Harrington KD. Degenerative arthritis of the ankle secondary to long-standing lateral ligament instability. J Bone Joint Surg Am 1979;61(3):354–61 [PubMed] [Google Scholar]
- 8.Denegar CR, Hertel J, Fonseca J. The effect of lateral ankle sprain on dorsiflexion range of motion, posterior talar glide, and joint laxity. J Orthop Sports Phys Ther 2002;32(4):166–73 [DOI] [PubMed] [Google Scholar]
- 9.Mulligan GM. Manual therapy: ‘NAGS’, ‘SNAGS’, ‘MWMS’, ETC. 3rd ed. Wellington: Plane View Services; 1995 [Google Scholar]
- 10.Maitland GD. Peripheral manipulation. 3rd ed. Oxford: Butterworth-Heinemann; 1991 [Google Scholar]
- 11.Landrum EL, Kelln CB, Parente WR, Ingersoll CD, Hertel J. Immediate effects of anterior-to-posterior talocrural joint mobilization after prolonged ankle immobilization: a preliminary study. J Man Manip Ther 2008;16(2):100–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hale SA, Hertel J. Reliability and sensitivity of the foot and ankle disability index in subjects with chronic ankle instability. J Athl Train 2005;40(1):35–40 [PMC free article] [PubMed] [Google Scholar]
- 13.Martin RL, Irrgang JJ, Burdett RG, Conti SF, Van Swearingen JM. Evidence of validity for the foot and ankle ability measure (FAAM). Foot Ankle Int 2005;26(11):968–83 [DOI] [PubMed] [Google Scholar]
- 14.van Rijn RM, van Os AG, Bernsen RM, Luijsterburg PA, Koes BW, Bierma-Zeinstra SM. What is the clinical course of acute ankle sprains? A systematic literature review. Am J Med 2008;121(4):324–31 [DOI] [PubMed] [Google Scholar]
- 15.Hubbard TJ, Cordova M. Mechanical instability after an acute lateral ankle sprain. Arch Phys Med Rehabil 2009;90(7):1142–6 [DOI] [PubMed] [Google Scholar]