Abstract
Testing for outcome or performance can take many forms; including multiple iterations of self-reported measures of function (an assessment of the individual’s perceived dysfunction) and/or clinical special tests (which are primarily assessments of impairments). Typically absent within these testing mechanisms is whether or not one can perform a specific task associated with function. The paper will operationally define function, discuss the construct of function within the disablement model, will overview the multi-dimensional nature of ‘function’ as a concept, will examine the current evidence for functional testing methods, and will propose a functional testing continuum. Limitations of functional performance testing will be discussed including recommendations for future research.
Keywords: Functional testing, International Classification of Functioning, Physical performance tests, Physical therapy
Introduction
Through the assessment of changes in pain and movement, and corresponding improvements that arise from these changes, manual therapists routinely evaluate within the disablement process at the levels of impairment, functional limitation, and disability. Impairment has previously been defined as ‘anatomical, physiological, mental or emotional abnormalities or loss’, whereas functional limitation is defined as ‘limitation in performance at the level of the whole organism or person’. In contrast, disability is considered a ‘limitation in performance of society defined roles and tasks within a sociocultural and physical environment’1 or more succinctly as ‘any restriction or lack of ability to perform a task or an activity in the manner considered normal for a person’.2 The disablement model refers to ‘various impact(s) of chronic and acute conditions on the functioning of specific body systems, on basic human performance, and on people’s functioning in necessary, usual, expected, and personally desired roles in society’.1,3,4 Therefore, this model is used to determine the consequences of disease and injury ‘both at the level of the person and at the level of society’.1
In contrast to disablement models such as the Nagi model,1 the International Classification of Impairments, Disabilities, and Handicaps Disablement Model (ICF)2 does not discriminate between functional limitation and disability. The domains described within the ICF model are classified from body, individual, and societal perspectives by means of two lists: (1) a list of body functions and structure; and (2) a list of domains of activity and participation. Activity and participation are influenced by contextual factors, including personal and environmental. The ICF differs most dramatically from the disablement model in that the definition of functioning (or activity) is highly complex and multi-dimensional, and likely differs from person to person.
The purpose of this clinical perspective involves examination of the concept of function, how this concept can be assessed, as well as its suggested implementation and limitations in the current literature. Additionally, we propose an examination continuum, incorporating a more comprehensive functional testing system.
Key Point #1: There are a Number of Current Measures of Functional Assessment
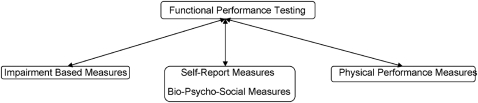
Function is measured in a number of different ways, including through the use of impairment measures, self-report measures, and physical performance measures (PPMs). The current measures of function all have unique contributions and dedicated limitations.
Impairment-based measures
Impairments are defined as a dysfunction or a significant structural abnormality in a specific body part or system.4 Findings of impaired joint mobility, motor function, muscle performance, range-of-motion (ROM), and sensation are considered problems that are limited to the impairment level.1 These impairments, alone or in combination, can contribute to limited function and ultimately may have consequences for physical functioning.3 For example, impaired humeral head inferior translation can contribute to the inability of a person to comb their hair due to mechanical shoulder impingement pain. Restricted ROM at the hip may lead to a limp during gait.
Clinical special tests are used to determine the tissue source of pain and are impairment-based assessments. It has been previously suggested5 that clinical examination testing has demonstrated an over-reliance on these clinical special tests despite multiple psychometric and performance deficiencies.6–9 The majority of stand-alone clinical tests do not demonstrate high levels of sensitivity and/or specificity,6–9 thus questioning the validity of use. Additionally, several clinical practice guidelines state that the tissue source of many forms of musculoskeletal pain cannot be specified in the majority of patients.10–13
Lastly, a clinical examination finding of an impairment does not always correspond to a functional loss. Using the previous examples of restricted inferior glide and a limp originating from a lack of range of the hip helps represent the precarious relationship. Limited humeral head inferior glide may not always directly correlate with the actual concept of physical function (combing hair), as the patient may compensate by side-bending their head towards the involved extremity or through use of the opposite extremity. Poor ROM and a limp may be sub-threshold for patients whose activity levels are low, thus do not compromised the individual to the point where their expectations are altered.
Self-report measures
Self-report measures are common methods of having the patient assess their pain and function. Self-report measures involve careful evaluation of instrument reliability, responsiveness, and validity and much work has been dedicated towards the development of these tools. Nearly all body regions or conditions have dedicated self-report functional measures that have been created.
Indeed, self-report measures are valuable in defining the patient’s perspective of their change but have been shown to differ substantially from PPMs that involve quantification of output, and are dramatically influenced by changes in pain.14–21 A reduction in pain after total joint arthroplasty has been associated with patients’ self-reported improvements in their functional ability, even though their time to complete performance tasks had doubled.22 In other words, patient’s perception of their functional ability was inflated in instances of decreased pain for these patients.
The relationship between self-reports of pain level and function has frequently been investigated in patients with low back pain (LBP), demonstrating low to moderate levels of association between self-report measures of LBP and PPMs.15,23 Patients systematically and significantly overestimate LBP at preferred and fastest speeds of movement with sit-to-stand tasks. There was also a trend towards underestimating expected pain at slow speeds of movement with the sit-to-stand tasks.24 An additional concern of self-report measures is that these measures do not always differentiate between whether or why a specific task is not done or cannot be done.25 Clearly, self-report measures are important, but should be utilized cautiously, and serve only as one component of the assessment of function.
PPMs
PPMs have become increasingly popular methods of measuring specific characteristics of function, especially in post-injury assessment,15,26–37 determining fall risks38–41 and sports performance/injury prediction.42–44 Although several authors45 have described these tests as functional tests, a more accurate depiction of these testing methods is that they are measures of physical performance. While some of these tests have demonstrated causal relationships for both post-injury15,26–37 and pre-injury risk assessments,38–44 they are often just one test and measure just one parameter of function. Additionally, the depth of investigation into these relationships is lacking.
Of particular concern for the spine manual clinician is the dearth of investigation regarding trunk endurance/capacity with reference to function. While trunk endurance testing has been investigated in healthy individuals for normative values,46–50 as well as post-surgical individuals with correlation to fear avoidance behavior,51 its incorporation into function has not been investigated. Therefore, the value of such testing in patients with LBP is currently uncertain.
As previously mentioned, a limitation of PPMs is their use to predict successful return to function and prediction of future injury. Unfortunately, this is a limitation with all current testing means, and an unsettled area of investigation. Reasoning for limited evidence support in this realm is multiple. Different medical and performance enhancement disciplines examine different components of function. Some of these disciplines are rooted in anecdotal evidence as the highest form of substantiation. Other disciplines have just begun to investigate this type of testing. The type of testing that is truly necessary to verify these tests are long-term longitudinal, prospective, and retrospective studies.
Key point #2: There is a Need for Functional Performance Testing (FPT)
Presently used methods of assessing function in clinical practice are incomplete. Much like the difficulty in, and complexity of, measuring function, there is the obstacle of defining function and the definitive assessment process for it.
FPT defined
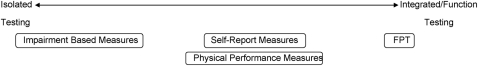
‘Testing’ is defined as using a set of problems to assess abilities. Therefore, we have previously termed FPT to mean using a set of tests to determine performance abilities or functional limitations.45 In other words, FPT is not impairment or PPM testing (Table 1). In simplified terms, impairments and PPM are typically more isolated findings while function is a more global concept incorporating the entire extremity, body, or person.
Table 1. PPMs compared to isolated components of functional tests utilized in musculoskeletal testing.
| Impairment tests (isolated components) | PPMs (integrating components of impairment testing) |
|
|
Note: PPMs = physical performance measures; ROM = range-of-motion.
Pain perception and movement, both integral elements in assessment of manual therapy interventions, are mediated by contextual elements such as cognitive, emotional, and social factors.45 Consequently, an expanded conceptual model of patient management and assessment at a functional, rather than impairment or PPM level, is necessary to fully evaluate all the elements associated with functioning.45 This expanded conceptual model (FPT), ventures to capture the multiple dimensions of function through clustered physical performance movements.
FPT can therefore be more complexly defined as using a variety of physical skills and tests to determine: (1) one’s ability to participate at the desired level in sport, occupation, and recreation or to return to participation in a safe and timely manner without functional limitations; and (2) one’s ability to move through up to three planes of movement as determined via non-traditional testing that provides qualitative and quantitative information related to specialized motions involved in sport, exercise, and occupations.45 The clinician should understand that FPT is an aspect of everyday life, whether for the elite athlete, the industrial worker, or the homemaker. The commonality among all groups is that some aspect of performance is needed for each individual to be successful in performing their respective skills or duties.45
Compared to clinical assessment with special tests, assessments with FPTs test the ability of the person to put together a series of movements (rather than isolated single joint and planar movements) to safely and efficiently complete a task. In other words, assessment at the functional level assesses function of the person rather than function of the part of the person.24 For example, the fact that a person has full hip, knee, and ankle ROM does not ensure successful return to basketball. If this same person has normal joint play, full strength, and full neuromuscular control and additionally is able to achieve an excellent score on jumping/hopping and anaerobic endurance tests without adverse symptoms, there should be much more confidence about the prospect of a safe return. Many FPTs closely approximate the activities that people need or wish to do.
We recommend the expansion of these recommendations to state that measurement of an individual’s ability to properly function should be along a continuum, and should include multiple measures (Figs. 1 and 2 and Table 2). To achieve this objective, the measurement of function demands careful individual consideration and investigations of the interactions among various examination methods.
Figure 1.
Conceptual model of comprehensive assessment of function.
Figure 2.
Proposed examination continuum. FPT = functional performance testing.
Table 2. Proposed levels for assessment of function in an individual.
| Levels for the assessment of function | Assessment examples |
| Level I Assessment primarily at the level of subjective report (patient and clinician) |
|
| Level II Assessment primarily at the level of impairment |
|
| Level III Assessment primarily at the level of static observation/posture/balance |
|
| Level IV Assessment primarily at the level of dynamic posture, general movement patterns, and single plane dynamic balance |
|
| Level V Assessment primarily at the level of movement patterns encountered during higher level tasks and/or multi-planar dynamic balance |
|
| Level VI Assessment primarily at the level of specific movement patterns |
|
| Level VII Assessment of the individual primarily at the level of performance-based measures (PPM) occurring predominantly in one plane of movement |
|
Level VIII Assessment primarily at the level of PPM occurring predominantly in one plane of movement, but requiring one or more of the following:
|
|
| Level IX Assessment primarily at the level of PPM occurring predominantly in multiple planes of movement and/or requiring explosive movement |
|
| Level X Assessment primarily at the level of PPM in multiple planes and/or explosive type of movement with the quality of the performance also assessed |
|
| Level XI Assessment primarily at the level of replication of the specific tasks performed during the individual’s sport/occupation/daily activity and/or clustering of PPM that replicate component(s) of the sport/occupation/daily activity |
|
| Level XII Cumulative assessment (FPT) including performance assessment (quantitative and qualitative) with self-report and bio-psycho-social measures |
|
Note: ROM = range-of-motion; PPM = physical performance measure; 1RM = one repetition maximum BEAST90 = ball-sport endurance and sprint test; FPT = functional performance testing.
Traditional thought regarding the examination process might suggest that the normal assessment ‘procedures’ progress from self-report measures to examination (including observation) followed by special testing (with use of clinical measures or other tests). FPT, if employed, would then be implemented at the very end stage of the rehabilitation process. It is our contention that the measurement of function requires assessment of combinations of these measures (Fig. 1) throughout the rehabilitation process. Examination of a patient’s function requires assessment of the entire disablement model.
The conceptual model illustrated in Fig. 1 suggests this comprehensive approach to measuring function. It should also be pointed out that this conceptual model advocates multi-directional flow along the assessment continuum. There are levels of function assessment (Table 2). Lower levels of function assessment can be implemented earlier in the examination process when warranted. In the above example, the use of functional movement and Rockport walk test could be utilized even prior to jumping/hopping and/or isokinetic testing in some dysfunctions. Functional movement could be utilized to screen for normal joint mobility in many early stage rehabilitation programs assuming safety. Additionally, the use of the deep squat assessment component of the Functional Movement Screen™ (Functional Movement Systems, Danville, VI, USA)43 could be used to determine restricted mobility of the hip joint (impairment). Lack of sufficient hip mobility would not allow the patient to perform a proper deep squat. Performing this assessment early in the examination process would allow the clinician to complete the necessary impairment assessments in order to ascertain the reason(s) for improper deep squatting. Another example of multi-directional flow examination may have a patient perform the firefighting ‘ability test’52 (as long as not contraindicated), allowing the clinician to assess for potential restricted abilities, whether they exist at the PPM or impairment level. An unsuccessful attempt at a specific component of this test does not specifically uncover the limitation, but it can allow the clinician to converge on identifiable areas of interest (impaired joint mobility, decreased muscle performance, etc.). Use of higher levels of testing in this fashion can prove beneficial in determining the limiting factors of function in these patients. The following articles in this series plan to use an algorithmic approach to demonstrate such examples of the integration of the multiple types of testing that we suggest in the comprehensive examination conceptual model. The combination of all of these testing approaches measures the concept of function.
Key Point #3: Limitations of FPT and Future Directions in the Assessment of Function
Not unlike normal objective and clinical special tests for musculoskeletal dysfunction, FPT has limitations. Since it is our suggestion that FPT is a comprehensive compilation of various assessment methods (each with their own respective limitations), the limitations of this assessment method are ample. The same limitations described above for each respective domain of FPT are applicable.
Incorporating clusters of PPMs, or specific aspects of an individual patient’s functional requirements, presumably more accurately indicates their current level of function. While these types of tests do exist, their worth is uncertain. Functional capacity evaluations are measurement tools created to assist in determining safe, tolerable levels of function and for predicting when an individual is ready to return to work duties.53 Manual handling, including lifting and carrying, has been described as the primary determinant for rating a job’s physical demands.54 It has been argued though that lifting capacity may not have much to do with subsequent injury or even job success.55 Additionally, the findings of spine ROM and muscle strength have little relationship with future LBP.47,56,57 Trunk muscle endurance, on the other hand, has demonstrated some predictive value of future episodes of back pain, suggesting that the capacity to perform repetitive prolonged work may be more closely linked to muscle endurance and actual job demands.46,47 Trunk endurance testing, as described above, is more likely an assessment of physical performance versus function as it does not mimic any movement of function in sport or the work place.
Other investigations have utilized more practical PPM's for LBP.15,23,58,59 However, comparisons to normal individuals without LBP are lacking. Therefore, assessment of the most appropriate test(s) for the pre- and post-injury LBP patient, whether they are impairment, PPM's self-report measure, or some combination thereof, are overdue.
Combining various examination methods for the purpose of evaluating function has recently been suggested with the use of the Delaware Osteoarthritis profile to include subjective and objective measures in post-surgical total knee arthroplasty patients.60 Expansion of this model is suggested (Figs. 1 and 2 and Table 2) for all orthopedic and sports-related patients as it does not entirely encapsulate the convolution of function. Determining the most efficacious combination of these multiple measures will require diligent investigation.
A final suggestion regarding the future investigation of function and the use of FPT is to investigate the entire concept of function assessment as proposed to determine which combination of these assessments is most predictive of function success and future injury prediction. Deficiencies exist in each examination procedure of function outlined in Fig. 1. The psychological and social effects of a patient’s function have increasingly warranted investigation. One potential suggestion for investigation is determining if the potential exists for clustering of FPT scores, similar to what is currently investigated with special testing, in order to define those athletes/patients at greater risk. Determining the relationship among these different variables is a complex task, one that will most likely require interaction among multiple disciplines.
Conclusion
Capturing a patient’s capabilities is a complex undertaking. Integrating current testing methods into an assessment continuum will provide the best determination of the patient’s current status. The use of various forms of testing is necessary to ascertain the patient’s abilities. The use of these various tests should be on a continuum that allows for movement in all directions. Limiting our examination process to self-report measures and assessment of specific impairments is not conclusive. FPT provides the best medium to mimic the patient’s actual functional activity. As with each form of examination, FPT is not without its limitations. Increased emphasis on research with necessary long-term studies is required to determine its best applicability. Despite its limitations, FPT is the best ‘big picture’ testing mechanism that we have.
References
- 1.American Physical Therapy Association Guide to physical therapist practice. Phys Ther 2001;81:9–746 [PubMed] [Google Scholar]
- 2.WHO International Classification of Impairments, Disabilities, and Handicaps. Geneva, Switzerland: World Health Organization; 1980 [Google Scholar]
- 3.Jette AM. Physical disablement concepts for physical therapy research and practice. Phys Ther 1994;74:380–6 [DOI] [PubMed] [Google Scholar]
- 4.Verbrugge L, Jette A. The disablement process. Soc Sci Med 1994;38:1–14 [DOI] [PubMed] [Google Scholar]
- 5.Cook C. The lost art of the clinical examination: an overemphasis on clinical special tests. J Man Manip Ther 2010;18:3–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rubinstein SD, van Tulder M. A best-evidence review of diagnostic procedures for neck and low back pain. Best Pract Res Clin Rheumatol 2008;22:471–82 [DOI] [PubMed] [Google Scholar]
- 7.Hegedus EJ, Cook C, Hasselblad V, Goode A, McCrory DC. Physical examination tests for assessing a torn meniscus in the knee: a systematic review with meta-analysis. J Orthop Sports Phys Ther 2007;37:541–50 [DOI] [PubMed] [Google Scholar]
- 8.Hegedus EJ, Goode A, Campbell S, Morin A, Tamaddoni M, Moorman CT, 3rd, et al. Physical examination tests of the shoulder: a systematic review with meta-analysis of individual tests. Br J Sports Med 2008;42:80–92 [DOI] [PubMed] [Google Scholar]
- 9.Liebold MR, Huijbregts PA, Jensen R. Concurrent criterion-related validity of physical examination tests for hip labral lesions: a systematic review. J Man Manip Ther 2008;16:E24–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Childs JD, Cleland JA, Elliott JM, Teyhen DS, Wainner RS, Whitman JM, et al. Neck pain: clinical practice guidelines linked to the International Classification of Functioning, Disability, and Health from the Orthopedic Section of the American Physical Therapy Association. J Orthop Sports Phys Ther 2008;38:A1–34 [DOI] [PubMed] [Google Scholar]
- 11.Cibulka MT, White DM, Woehrle J, Harris-Hayes M, Enseki K, Fagerson TL, et al. Hip pain and mobility deficits–hip osteoarthritis: clinical practice guidelines linked to the international classification of functioning, disability, and health from the Orthopaedic Section of the American Physical Therapy Association. J Orthop Sports Phys Ther 2009;39:A1–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pincus T, Santos R, Breen A, Burton AK, Underwood M; Multinational Musculoskeletal Inception Cohort Study Collaboration. A review and proposal for a core set of factors for prospective cohorts in low back pain: a consensus statement. Arthritis Rheum 2008;59:14–24 [DOI] [PubMed] [Google Scholar]
- 13.Chou R, Qaseem A, Snow V, Casey D, Cross JT, Jr, Shekelle P, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med 2007;147:478–91 [DOI] [PubMed] [Google Scholar]
- 14.Lee CE, Simmonds MJ, Novy DM, Jones SC. A comparison of self-report and clinician measured physical function among patients with low back pain. Arch Phys Med Rehabil 2000;82:227–31 [DOI] [PubMed] [Google Scholar]
- 15.Reneman MF, Jorritsma W, Schellekens JMH, Göeken LNH. Concurrent validity of questionnaire and performance-based disability measurements in patients with chronic nonspecific low back pain. J Occup Rehabil 2002;12:119–29 [DOI] [PubMed] [Google Scholar]
- 16.Bellamy N, Kirwan J, Boers M, Brooks P, Strand V, Tugwell V, et al. Recommendations for a core set of outcome measures for future phase III clinical trials in knee, hip, and hand osteoarthritis. Consensus development at OMERACT III. J Rheumatol 1997;24:799–802 [PubMed] [Google Scholar]
- 17.Terwee CB, van der Slikke RM, van Lummel RC, Benink RJ, Meijers WG, de Vet HC. Self-reported physical functioning was more influenced by pain than performance-based physical functioning in knee-osteoarthritis patients. J Clin Epidemiol 2006;59:724–31 [DOI] [PubMed] [Google Scholar]
- 18.Maly MR, Costigan PA, Olney SJ. Determinants of self-report outcome measures in people with knee osteoarthritis. Arch Phys Med Rehabil 2006;87:96–104 [DOI] [PubMed] [Google Scholar]
- 19.Stratford PW, Kennedy DM, Maly MR, MacIntyre NJ. Quantifying self-report measures’ overestimation of mobility scores postarthroplasty. Phys Ther 2010;90:1288–96 [DOI] [PubMed] [Google Scholar]
- 20.Stratford PW, Kennedy DM, Woodhouse LJ. Performance measures provide assessments of pain and function in people with advanced osteoarthritis of the hip or knee. Phys Ther 2006;86:1489–96 [DOI] [PubMed] [Google Scholar]
- 21.Parent E, Moffett H. Comparative responsiveness of locomotor tests and questionnaires used to follow early recovery after total knee arthroplasty. Arch Phys Med Rehabil 2002;83:70–80 [DOI] [PubMed] [Google Scholar]
- 22.Stratford PW, Kennedy DM. Performance measures were necessary to obtain a complete picture of osteoarthritic patients. J Clin Epidemiol 2006;59:160–7 [DOI] [PubMed] [Google Scholar]
- 23.Cunha IT, Simmonds MJ, Protas EJ, Jones S. Back pain, physical function, and estimates of aerobic capacity: what are the relationships among methods and measures? Am J Phys Med Rehabil 2002;81:913–20 [DOI] [PubMed] [Google Scholar]
- 24.Simmonds MJ, Rebelo V. Self-selected speed of movement during a repeated sit-to-stand task in individuals with and without LBP. Proceedings of the 4th Congress of European Federation of the International Association for the Study of Pain Chapters; 2003 Sep 2–6; Prague, Czech Republic. [Google Scholar]
- 25.Simmonds MJ. Measuring and managing pain and performance. Man Ther 2006;11:175–9 [DOI] [PubMed] [Google Scholar]
- 26.Olmstead LC, Carcia CR, Hertel J, Schultz SJ. Efficacy of the star excursion balance tests in detecting reach deficits in subjects with chronic ankle instability. J Athl Train 2002;37:501–6 [PMC free article] [PubMed] [Google Scholar]
- 27.Gribble PA, Hertel J. Considerations for normalization of measures of the Star Excursion Balance Test. Meas Phys Educ Sci 2003;7:89–100 [Google Scholar]
- 28.Hertel J, Braham RA, Hale SA, Olmstead-Kramer LC. Simplifying the star excursion balance test: analysis of subjects with and without chronic ankle instability. J Orthop Sports Phys Ther 2006;36:131–7 [DOI] [PubMed] [Google Scholar]
- 29.Colby SM, Hintermeister RA, Torry MR, Steadman RJ. Lower limb stability with ACL impairment. J Orthop Sports Phys Ther 1999;29:444–54 [DOI] [PubMed] [Google Scholar]
- 30.Bremander AB, Dahl LL, Roos EM. Validity and reliability of functional performance tests in meniscectomized patients with or without knee osteoarthritis. Scan J Med Sci Sports 2007;17:120–7 [DOI] [PubMed] [Google Scholar]
- 31.Alkjaer T, Simonsen EB, Magnusson SP, Aagaard H, Dyhre-Poulsen P. Differences in the movemtn pattern of a forward lung in two types of anterior cruciate ligament deficient patient: copers and non-copers. Clin Biomech 2002;17:586–93 [DOI] [PubMed] [Google Scholar]
- 32.Riseberg MA, Ekeland A. Assessment of functional tests after anterior cruciate ligament surgery. J Orthop Sports Phys Ther 1994;19:212–7 [DOI] [PubMed] [Google Scholar]
- 33.Wilk KE, Romaniello WT, Soscia SM, Arrigo CA, Andrews JR. The relationship between subjective knee scores, isokinetic testing, and functional testing in the ACL reconstructed knee. J Orthop Sports Phys Ther 1994;20:60–73 [DOI] [PubMed] [Google Scholar]
- 34.Reid A, Birmingham TB, Stratford PW, Alcock GK, Giffin JR. Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Phys Ther 2007;87:337–49 [DOI] [PubMed] [Google Scholar]
- 35.Petschnig R, Baron R, Albrecht M. The relationship between isokinetic quadriceps strength test and hop tests for distance and one-legged vertical jump test following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 1998;28:23–31 [DOI] [PubMed] [Google Scholar]
- 36.Ross MD, Langford B, Whelan PJ. Test-retest reliability of 4 single-leg hop tests. J Strength Cond Res 2002;16:617–22 [PubMed] [Google Scholar]
- 37.Augustsson J, Thome R, Karlsson J. Ability of a new hop test to determine functional deficits after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2004;12:350–6 [DOI] [PubMed] [Google Scholar]
- 38.Murphy MA, Olson SL, Protas EJ, Overby AR. Screening for falls in community-dwelling elderly. J Aging Phys Act 2003;11:66–80 [Google Scholar]
- 39.Dite W, Temple VA. A clinical test of stepping and change of direction to identify multiple falling older adults. Arch Phys Med Rehabil 2002;83:1566–71 [DOI] [PubMed] [Google Scholar]
- 40.Tinetti ME. Performance oriented assessment of mobility problems in elderly patients. JAGS 1986;34:119–26 [DOI] [PubMed] [Google Scholar]
- 41.Thorbahn LB, Newton RA. Use of the Berg balance test to predict falls in the elderly persons. Phys Ther 1996;76:576–83 [DOI] [PubMed] [Google Scholar]
- 42.Plisky PJ, Rauh MJ, Kaminski TW, Underwood FB. Star excursion balance test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther 2006;36:911–9 [DOI] [PubMed] [Google Scholar]
- 43.Kiesel K, Plisky PJ, Voight ML. Can serious injury in professional football be predicted by a preseason functional movement screen? North Am J Sports Phys Ther 2007;2:147–58 [PMC free article] [PubMed] [Google Scholar]
- 44.Chorba RS, Chorba DJ, Bouillon LE, Overmyer CA, Landis JA. Use of a functional movement screening tool to determine injury risk in female collegiate athletes. North Am J Sports Phys Ther 2010;5:47–54 [PMC free article] [PubMed] [Google Scholar]
- 45.Reiman MP, Manske RC. Functional testing in human performance. Champaign, IL: Human Kinetics; 2009 [Google Scholar]
- 46.Alaranta H, Luoto S, Heliovaara M, Hurri H. Static back endurance and the risk of low back pain. Clin Biomech 1995;10:323–4 [DOI] [PubMed] [Google Scholar]
- 47.Biering-Sørensen F. Physical measurements as risk indicators for low-back trouble over a one-year period. Spine (Phila Pa 1976) 1984;9:106–19 [DOI] [PubMed] [Google Scholar]
- 48.McGill SM, Childs A, Liebenson C. Endurance times for stabilization exercises: clinical targets for testing and training from a normal database. Arch Phys Med Rehabil 1999;80:941–4 [DOI] [PubMed] [Google Scholar]
- 49.Reiman MP, Krier AD, Nelson JA, Rogers MA, Stuke ZO, Smith BS. Reliability of trunk endurance testing modifications. J Strength Cond Res 2010;24:730–6 [DOI] [PubMed] [Google Scholar]
- 50.Udermann BE, Mayer JM, Graves JE, Murray SR. Quantitative assessment of lumbar paraspinal muscle endurance. J Athl Train 2003;38:259–62 [PMC free article] [PubMed] [Google Scholar]
- 51.Flanagan SP, Kulig K. Assessing musculoskeletal performance of the back extensors following a single-level microdiscectomy. J Orthop Sports Phys Ther 2007;37:356–63 [DOI] [PubMed] [Google Scholar]
- 52.Michaelides MA, Parpa KM, Thompson J, Brown B. Predicting performance on a firefighter’s ability test from fitness parameters. Res Q Exerc Sport 2008;79:468–75 [DOI] [PubMed] [Google Scholar]
- 53.Gibson L, Strong J. A review of functional capacity evaluation practice. Work 1997;9:3–11 [DOI] [PubMed] [Google Scholar]
- 54.Isernhagen SJ, Hart DL, Matheson LM. Reliability of independent observer judgments of level of lift in kinesiophysical functional capacity evaluation. Work 1999;12:145–50 [PubMed] [Google Scholar]
- 55.Cady LD, Bischoff DP, O’Connell ER, Thomas PC, Allan JH. Strength and fitness and subsequent back injuries in firefighters. J Occup Med 1979;21:269. [PubMed] [Google Scholar]
- 56.Jorgensen K. Human trunk extensor muscles: physiology and ergonomics. Acta Physiol Scand Suppl 1997;637:l–58 [PubMed] [Google Scholar]
- 57.Burton AK, Tillotson KM, Troup JDG. Variation in lumbar sagittal mobility with low back trouble. Spine (Phila Pa 1976) 1989;14:584–90 [DOI] [PubMed] [Google Scholar]
- 58.Smeets R, Hijdra H, Kester A, Hitters M, Knottnerus J. The usability of six physical performance tasks in a rehabilitation population with chronic low back pain. Clin Rehabil 2006;20:989–98 [DOI] [PubMed] [Google Scholar]
- 59.Novy DM, Simmonds MJ, Lee CE. Physical performance tasks: what are the underlying constructs? Arch Phys Med Rehabil 2002;83:44–7 [DOI] [PubMed] [Google Scholar]
- 60.Mizner RL, Petterson SC, Clements KE, Zeni JA, Irrgang JJ, Snyder-Mackler L. Measuring functional improvement after total knee arthroplasty requires both performance-based and patient-report assessments. J Arthroplasty 2010;to be published. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med 2001;29:213–8 [DOI] [PubMed] [Google Scholar]