Abstract
It has been suggested that tight hamstring muscle, due to its anatomical connections, could be a compensatory mechanism for providing sacroiliac (SI) joint stability in patients with gluteal muscle weakness and SIJ dysfunction. The purpose of this study was to determine the relationship between hamstring muscle length and gluteal muscle strength in subjects with sacroiliac joint dysfunction. A total of 159 subjects with and without low back pain (LBP) between the ages of 20 and 65 years participate in the study. Subjects were categorized into three groups: LBP without SIJ involvement (n = 53); back pain with SIJ dysfunction (n = 53); and no low back pain (n = 53). Hamstring muscle length and gluteal muscle strength were measured in all subjects. The number of individuals with gluteal weakness was significantly (P = 0.02) higher in subjects with SI joint dysfunction (66%) compared to those with LBP without SI joint dysfunctions (34%). In pooled data, there was no significant difference (P = 0.31) in hamstring muscle length between subjects with SI joint dysfunction and those with back pain without SI involvement. In subjects with SI joint dysfunction, however, those with gluteal muscle weakness had significantly (P = 0.02) shorter hamstring muscle length (mean = 158±11°) compared to individuals without gluteal weakness (mean = 165±10°). There was no statistically significant difference (P>0.05) in hamstring muscle length between individuals with and without gluteal muscle weakness in other groups. In conclusion, hamstring tightness in subjects with SI joint dysfunction could be related to gluteal muscle weakness. The slight difference in hamstring muscle length found in this study, although statistically significant, was not sufficient for making any definite conclusions. Further studies are needed to establish the role of hamstring muscle in SI joint stability.
Keywords: Low back pain, Sacroiliac joint, Hamstring muscle length, Gluteal muscle weakness, Pelvic dysfunction, Muscle imbalance
Introduction
Short hamstring muscles are often reported in patients with low back pain (LBP).1–4 The cause of such muscular tightness, however, has not been fully understood. Some have attributed hamstring tightness in patients with LBP as a compensatory mechanism for controlling the excess lumbar lordosis induced by specific patterns of muscle impairments known as ‘pelvic cross syndrome’.5–7 A previous study examined the proposed hypothesis.8 The authors, however, found no relationship between hamstring muscle length and the degree of lumbar lordosis in subjects with different patterns of muscle impairment. Several other studies have also shown no relationship between hamstring muscle length and lumbar lordosis,4,9,10 and between lumbar lordosis and LBP.4,11–14
Most of the studies reporting hamstring muscle tightness in individuals with LBP did not differentiate between lumbar versus sacral source of subjects' back pain.1–4
van Wingerden et al.15,16 proposed that hamstring tightness in individuals with LBP could be a compensatory mechanism for weak gluteal muscles and decreased sacroiliac (SI) joint stability in patients with sacroiliac disorders. They indicated that gluteus maximus muscle, due to its attachments to sacrum, iliac bones, and sacrotuberous ligament, plays a significant role in stability of the SI joint. The stabilizing forces applied to the SI joint, therefore, could be compromised with gluteal muscle weakness. In patients with gluteal weakness, shortening of the hamstring muscles, through their common attachments to the ischial tuberosity and sacrotuberous ligament, could compensate for gluteal muscle weakness and contribute to the SI joint stability.15,16 This notion has been indirectly supported by investigators who showed a link between hamstring muscle strain and SI joint dysfunctions;17 increased hamstring length following SI joint manipulation18 and resolution of hamstring muscle injuries following lumbosacral manipulations.19,20 In contrast, other studies showed no significant change in hamstring muscle length following SI joint manipulation.21,22
The purpose of this study was to investigate the relationship between hamstring muscle length and gluteal muscle strength in subjects with and without SI joint dysfunction.
The hypotheses of this study are as follows:
the number of individuals with gluteal weakness is significantly higher in subjects with SI joint dysfunction compared to those without SI joint dysfunction;
in subjects with SI joint dysfunction, subjects with gluteal weakness have significantly shorter hamstring muscle length compared to those without gluteal weakness.
Methods
Subjects
A total of 159 subjects with and without LBP, between the ages of 20 and 65 years, participated in this study. Subjects were selected among patients in the orthopedic and physical therapy clinics in various hospitals. At first, 124 subjects with LBP were tested for having SI joint dysfunction. Among the subjects tested, 53 individuals were diagnosed with SI joint dysfunction. Then 53 subjects with LBP without SI joint involvement and 53 subjects without LBP, matched in age and gender to those with SI dysfunction, were selected from the same clinical settings as control groups. All the subjects signed an informed consent form approved by the human subjects committee at the University of Social Welfare and Rehabilitation Sciences before participating in the study.
Selection criteria for subjects without LBP and those with LBP without SI joint involvement
Subjects with LBP had a history of back pain for more than 6 weeks before the study or had at least three episodes of intermittent LBP, each one lasting more than 1 week, during the year before the time of the study. Subjects without LBP had no history of back pain for at least 1 year before the study. Subjects with a history of spinal surgery, spinal, or pelvic fracture, hospitalization for severe trauma or car accident, fracture of the lower extremities, or any systemic diseases such as arthritis or tuberculosis were excluded.
Selection criteria for subjects with SI joint dysfunction
Subjects with LBP below the level of L5, or with pain over the posterior aspect of SI joint around posterior superior iliac spine and buttock with or without above knee leg pain were included in the study.
Subjects were excluded if they had midline or symmetrical pain above the L5 level, had radicular pain with neurological (sensory or motor) deficits,23,24 had a history of spinal surgery, spinal, pelvic, or lower extremity fracture; hospitalization for trauma or motor vehicle accident; hip or knee dysfunctions; pregnancy; any systemic disease such as arthritis, tuberculosis, liver, or kidney failure. Subjects with leg length discrepancies, because of its potential effect on hamstring muscle length,4 were also excluded.
Procedure for diagnosing SI joint dysfunction
At present, there are no widely accepted guidelines for diagnosing SI joint dysfunctions. Current evidence suggests that none of the SI joint provocation tests is valid enough to be solely used for diagnosing SI joint dysfunctions. Therefore, using a cluster of various tests has been suggested for diagnosing SI joint disorders.25–29
In this study, four SI joint special tests with good sensitivity, specificity, inter- and intra-rater reliability was used for screening subjects with SI joint dysfunction. Subjects who tested positive on three out of the four pain provocation tests were considered as having SI joint dysfunction. Laslett et al.23 reported highest sensitivity (93.8%) and specificity (78.1%) for SI joint pain provocation tests when a combination of at least three tests was used.
Testing procedures
Thigh thrust or posterior shear test
This test has excellent reported sensitivity (0.80), specificity (1.0), and inter-rater reliability (kappa = 0.88) for diagnosing SI joint dysfunction.30,31 As shown in Fig. 1, the subject lies supine on the table. The examiner brings the hip joint of the leg ipsilateral to the tested SI joint, to approximately 90° of flexion and slight adduction. At this position, the thigh is almost perpendicular to the table and the knee joint is flexed. The examiner with one hand cups the sacrum and wraps the other arm and hand around the flexed knee joint. Then an axial pressure is applied to the thigh, in the direction of the long axis of the femur, causing an anterior–posterior shear at the tested SI joint.23,25,31,32 The test was considered positive if pain in the SI joint was reported. This procedure was repeated for the other side.
Figure 1.

Thigh thrust or posterior shear test.
Compression test
This test has very good reported sensitivity (0.70), specificity (0.9), and inter-rater reliability (kappa = 0.75) for diagnosing SI joint dysfunction.30,31 The subject was placed in side lying position with hips and knees flexed to about a right angle. A downward manual pressure is applied vertically to the ilium, toward the opposite side.25,26,31 The test was considered positive if it induced pain in the SI joints.
Distraction test
This test has very good reported sensitivity (0.88), specificity (0.81), and inter-rater reliability (kappa = 0.69) for diagnosing SI joint dysfunction.30,31 The subject was supine on the table. The examiner, standing at the side of the table, applied a pressure to both anterior superior iliac spines directed posteriorly and laterally.25,26,31 The test was considered positive if it induced pain in the SI joints.
Sacral thrust test
This test has good reported sensitivity (0.69), specificity (1.0), and inter-rater reliability (kappa = 0.52) for diagnosing SI joint dysfunction.30,31 The subject was prone on the table (Fig. 2). The examiner, with the palm of his hand, applied a vertical force downward to the sacrum.23,32 The test was considered positive if it induced pain in the SI joints.
Figure 2.

Sacral thrust test.
Measuring hamstring muscle length
The straight leg-raising (SLR) method has previously been used for assessing hamstring muscles length.1,9,10,18,22 Owing to non-controlled pelvic rotation with SLR, the accuracy of this method, however, has been questioned. In this study, we used active knee extension method for assessing hamstring muscle length.4,22 An excellent reliability for this test (ICC = 0.91) has previously been reported.4
During this procedure, subjects, positioned in supine, were instructed to assume and maintain a 90° hip flexion in the testing leg. Using a goniometer, the degree of hip flexion was monitored by the therapist during the whole testing procedure. Subjects were then instructed to actively extend the knee joint. The degree of achieved active knee extension was then measured. The procedure was performed in both legs. The averaged active knee extension range was used as the measure of hamstring muscle length in this study.
Measuring gluteus maximus muscle strength
Gluteus maximus muscle strength was quantitatively measured by a pressure meter similar to the one described by Helewa et al.33,34 The reliability and validity of this procedure have previously been established.4,33 The unit used in this study was calibrated and had 99% measurement accuracy. To measure muscle strength, subjects assumed the standard positions for manual muscle testing of hip extensor muscle strength. The inflated bag of the pressure meter was placed between the examiner's hand and the specified contact point for the test on the subject's thigh.35 The pressure meter used in this study provided measurements in kPa units, which is defined as force per unit area. To assure reliability of measurements, all assessments were performed by one therapist. The reliability of this method (ICC = 0.96) has previously been demonstrated.4
Data analysis
Subjects who tested positive on three out of the four pain provocation tests were considered having SI joint dysfunction. Subjects with less than three positive provocation tests were classified as having LBP without SI joint involvement.
In all subjects, measured gluteus maximum muscle strength was normalized to the subject's calculated body mass index. Then using the receiver operating characteristic curve analysis36 through MedCalc® statistical software,37 a cut-off value for determining gluteal muscle weakness was obtained. We used the normalized values for gluteal muscle strength as determining variable, and having or not having SI dysfunction as the criterion variable for the ROC curve analysis. Using the obtained cut-off value, all subjects were categorized as with or without gluteal muscle weakness.
We used Fisher's exact test36 for comparing the number of individuals with gluteal muscle weakness among the three groups. Using multivariate analysis of variance, we compared gluteal muscle strength and hamstring muscle length among the three groups. Then, in subjects with SI joint dysfunction, using independent t-test, we compared the hamstring muscle length between those with and without gluteal muscle weakness.
Results
Descriptive data and average normalized values for gluteus maximus muscle strength and average hamstring muscle length (degree of knee extension) for the three groups are presented in Table 1. Analysis of variance showed no significant difference in subjects' age, height, and weight among the three groups.
Table 1. Descriptive data associated with subjects in each group.
| Variables | Without LBP | With SI dysfunction | Without SI dysfunction | P values (MNOVA) | |||
|
n = 53 |
n = 53 |
n = 53 |
|||||
| Mean | SD | Mean | SD | Mean | SD | ||
| Age | 45.74 | 14.45 | 42.75 | 12.6 | 39.15 | 14.43 | 0.053 |
| Weight (kg) | 66.58 | 7.16 | 70.45 | 10.12 | 69.49 | 12.78 | 0.66 |
| Height (m) | 1.66 | 0.09 | 1.65 | 0.09 | 1.67 | 0.08 | 0.26 |
| BMI | 24.9 | 3.6 | 26.2 | 4.95 | 24.6 | 3.96 | 0.14 |
| Knee extension (°) (hamstring length) | 153.96 | 8.6 | 160.7 | 11.2 | 156.04 | 13.8 | 0.008* |
| Gluteus maximus strength (kPa) | 29.70 | 7.2 | 22.11 | 7.5 | 25.47 | 7.0 | 0.000† |
Post hoc analysis: no LBP versus LBP without SI dysfunction: P = 0.61; no LBP versus LBP with SI dysfunction: P = 0.007; LBP with SI dysfunction versus LBP without SI dysfunction: P = 0.08.
Post hoc analysis no LBP versus LBP without SI dysfunction: P = 0.009; no LBP versus LBP with SI dysfunction: P = 0.000; LBP with SI dysfunction versus LBP without SI dysfunction: P = 0.04.
The results of the ROC curve analysis provided a cut-off value of 1.02 for normalized gluteal muscle strength (Fig. 3). The obtained cut-off value had sensitivity of 0.92 and specificity of 0.59 for differentiating subjects with and without gluteal weakness. This test had a diagnostic accuracy of 78%, as denoted by the area under the ROC curve35 with a 95% confidence interval of 75–85%.
Figure 3.
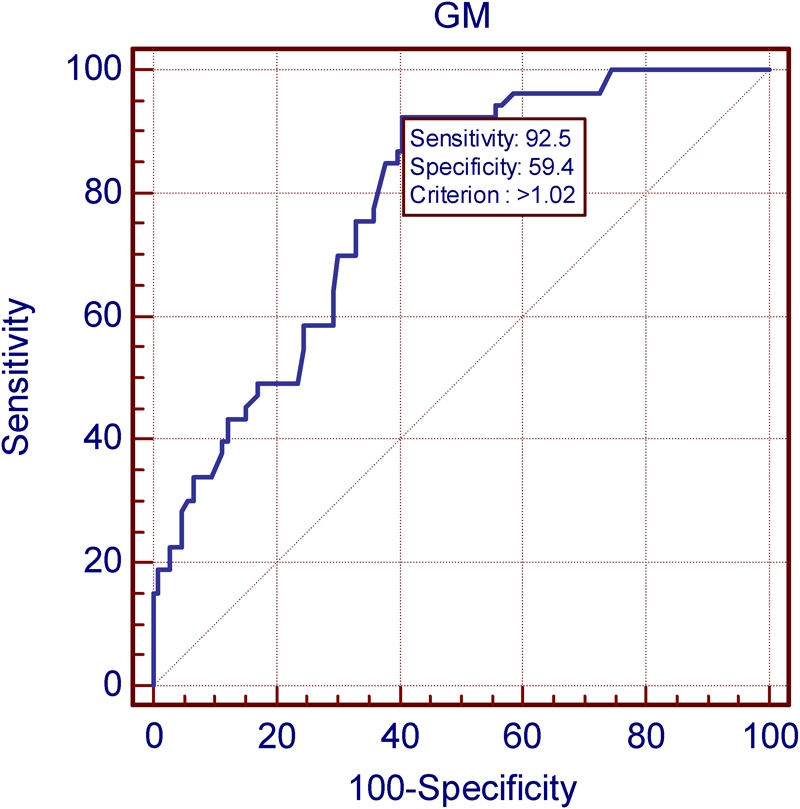
The result of ROC curve analysis used for differentiating subjects with and without gluteal muscle weakness.
Based on the ROC analysis, subjects were categorized as with (gluteal strength⩽1.02) or without (gluteal strength>1.02) gluteal muscle weakness.
Among all subjects with LBP (n = 106), 54% (n = 57) had gluteal muscle weakness. In subjects without LBP, only 8% (n = 4) of the subjects had gluteal muscle weakness (Table 2). In subjects with LBP, the results of the Fisher's exact test showed that the number of subjects with gluteal weakness was significantly (P = 0.02) higher in those with SI dysfunction (66%) compared to those without SI joint involvement (34%) (Table 2).
Table 2. Hamstring muscle length for subjects with and without gluteal muscle weakness in each group.
| Condition | With gluteal weakness |
Without gluteal weakness |
P value | ||
| Mean±SD | n | Mean±SD | n | ||
| LBP with SI joint dysfunction | 158±11.26 | 35 (66%) | 165±10.26 | 18 (34%) | 0.04 |
| LBP without SI joint dysfunction | 154±17.1 | 22 (42%) | 158±10.2 | 31 (58%) | 0.16 |
| Without LBP | 151.14±9.4 | 4 (8%) | 161±4.1 | 49 (92%) | 0.15 |
In all subjects with LBP (n = 106), there was no significant difference in hamstring muscle length (P = 0.05) between individuals with SI joint dysfunction (n = 53; mean = 160±11.2°) and those without (n = 53; mean = 156±13.7°).
In subjects with SI joint dysfunction, those with gluteal muscle weakness had slightly shorter but statistically significant (P = 0.04) hamstring muscle length (mean = 158±11°) compared to individuals without gluteal weakness (mean = 165±10°). Hamstring muscle length was not significantly different (P>0.05) between individuals with and without gluteal muscle weakness in subjects with no LBP and in those with LBP without SI involvement (Table 2).
Discussion
Our findings suggested a significantly higher proportion of individuals with gluteal muscle weakness among subjects with SI dysfunction compared to those without SI involvement (Table 2). Among subjects with LBP, those with SI joint dysfunction showed significantly (P = 0.04) weaker gluteal muscle strength compared with those without SI involvement (Table 1).
Our data did not show any significant difference in hamstring muscle length between subjects with and without SI joint dysfunction. However, we found that in subjects with SI joint dysfunction, those with gluteal weakness had slightly, but statistically significant, shorter hamstring muscle length compared to individuals without gluteal weakness.
These findings are in agreement with the notion proposed by van Wingerden et al.15,16 that hamstring tightness could be a compensatory mechanism for providing SI stability in subjects with SI joint dysfunction and gluteal muscle weakness. They indicated that gluteus maximus muscle crosses the SI joint and has attachments to the sacrum, and sacrotuberous and long dorsal sacral ligaments. Muscular tension applied by the gluteus maximus to the SI joint and to the sacrotuberous and long dorsal ligaments, contributes to the force closure stability of the SI joint. The hamstring muscle, particularly the long head of biceps femoris, also has common attachment to the sacrotuberous and long dorsal ligaments at the ischial tuberosity. They suggested that hamstring muscle shortening could increase tension on these ligaments and improve SI joint stability when force closure stability of the SI joint is decreased due to gluteal muscle weakness.15,16,38
Information from cadaver studies supports the notion proposed by van Wingerden et al.15,16 Using human cadavers, Vleeming et al.39,40 studied if loading hamstring and gluteus maximus muscle could increase the tension in the sacrotuberous and long dorsal sacral ligament. In all 12 cadavers tested, the gluteus maximus muscle was connected with sacrotuberous ligament and hamstring muscle had attachments to sacrotuberous ligament in six of the cadavers. They showed that increasing force through loading of the gluteus maximus muscle, as it would happen during active muscle contraction, led to increased tension in the sacrotuberous ligament. Force applied through loading of the biceps femoris caused increased tension in the sacrotuberous ligament and long dorsal ligaments in six of the cadavers. These studies support the speculation that compensatory shortening of the hamstring muscles, through their anatomical connections to the sacrotuberous and long dorsal ligaments, could compensate for ligamentous laxity, induced by gluteus maximus weakness, and improve SI joint stability.
Biomechanical studies also indicate that postural changes following hamstring muscle tightness could indirectly affect SI joint stability. Hamstring tightness could cause knee flexion, resulting in anterior displacement of center of mass and sacral nutation during upright standing.41,42 At the same time, short biceps femoris muscle, through its attachment to the ischial tuberosity could prevent innominate anterior rotation or even induce posterior rotation of the innominate bone. Posterior innominate rotation along with sacral nutation could increase SI joint stability.
Clinical studies provide conflicting evidence regarding the role of hamstring muscles in SI joint stability. Cibulka et al.17 showed a relationship between hamstring muscle strain and SI joint dysfunctions. Others have shown increased hamstring length18 and resolution of hamstring muscle injuries19,20 following lumbosacral joint manipulations. In contrast, other studies have shown no significant change in hamstring muscle length following SI joint manipulation.21
Our study showed that the proportion of subjects with gluteal weakness was significantly higher in those with SI joint dysfunction compared to those without SI joint involvement. We also found that in subjects with SI dysfunction, those with gluteal muscle weakness had slightly shorter hamstring muscle length compared to individuals without gluteal weakness. The small difference in hamstring muscle length between the two group, found in this study, although was statistically significant, might not be clinically meaningful to either support or disprove the hypothesis put forward by van Wingerden et al.15,16 More studies are needed to assess the therapeutic values of strengthening gluteal and hamstring muscles on treating patients with SI joint dysfunction.
Conclusion
Hamstring tightness in subjects with SI joint dysfunction could be related to gluteal muscle weakness. The slight difference in hamstring muscle length found in this study, although statistically significant, is not sufficient for making any definite conclusions. Further studies are needed to establish the role of hamstring muscle in SI joint stability.
Clinical implications
The results of this study could be beneficial to clinicians when prescribing therapeutic exercises for patients with low back pain, particularly those with SI joint involvement.
References
- 1.Halbertsma JP, Goeken LN, Hof AL, Groothoff JW, Eisma WH. Extensibility and stiffness of the hamstrings in patients with nonspecific low back pain. Arch Phys Med Rehabil 2001;82:232–8 [DOI] [PubMed] [Google Scholar]
- 2.Kendall FP, McCreary EK, Provance PG. Muscles: testing and function, with posture and pain. 5th ed.Baltimore, MD: Lippincott Williams & Wilkins; 2005 [Google Scholar]
- 3.McClure PW, Esola M, Schreier R, Siegler S. Kinematic analysis of lumbar and hip motion while rising from a forward, flexed position in patients with and without a history of low back pain. Spine 1997;22:552–8 [DOI] [PubMed] [Google Scholar]
- 4.Nourbakhsh MR, Arab AM. Relationship between mechanical factors and incidence of low back pain. J Orthop Sports Phys Ther 2002;32:447–60 [DOI] [PubMed] [Google Scholar]
- 5.Janda V. Muscle strength in relation to muscle length, pain and muscle imbalance. In: Harms-Ringdahl K, editor. Muscle strength (International perspectives in physical therapy). Edinburgh: Churchill Livingston; 1993;8:83–91 [Google Scholar]
- 6.Jull G, Janda V. Muscle and motor control in low back pain: assessment and management. Twomey LT, Taylor JR.editors.Physical therapy for the low back. 1987New York: Churchill Livingston; 253–278 [Google Scholar]
- 7.Schlink MB. Muscle imbalance patterns associated with low back syndromes. Watkins RG.editor.The spine in sports St Louis, MO: Mosby; 1996146–56 [Google Scholar]
- 8.Nourbakhsh MR, Arab AM, Salavati M. The relationship between pelvic cross syndrome and chronic low back pain. J Back Musculoskelet Rehabil 2006;19:119–28 [Google Scholar]
- 9.Toppenberg R, Bullock M. Normal lumbo-pelvic muscle lengths and their interrelationships in adolescent females. Aust J Physiother 1990;36:105–9 [DOI] [PubMed] [Google Scholar]
- 10.Gajdosik RL, Hatcher CK, Whitsell S. Influence of short hamstring muscles on the pelvis and lumbar spine in standing and during toe-touch test. Clin Biomech 1992;7:38–42 [DOI] [PubMed] [Google Scholar]
- 11.Murrie VL, Dixon AK, Hollingworth W, Wilson H, Doyle TA. Lumbar lordosis: study of patients with and without low back pain. Clin Anat 2003;16:144–7 [DOI] [PubMed] [Google Scholar]
- 12.Ng JK, Richardson CA, Kippers V, Parnianpour M. Comparison of lumbar range of movement and lumbar lordosis in back pain patients and matched controls. J Rehabil Med 2002;34:109–13 [DOI] [PubMed] [Google Scholar]
- 13.Norton BJ, Sahrmann SA, van Dillen FL. Differences in measurements of lumbar curvature related to gender and low back pain. J Orthop Sports Phys Ther 2004;34:524–34 [DOI] [PubMed] [Google Scholar]
- 14.Nourbakhsh MR, Mossavi SJ, Salavati M. The effect of lifestyle and work related physical activity on the size of lumbar lordosis and chronic low back pain in a Middle East population. J Spinal Disord 2001;14:283–92 [DOI] [PubMed] [Google Scholar]
- 15.van Wingerden JP, Vleeming A, Buyruk HM, Raissadat K. Stabilization of the sacroiliac joint in vivo: verification of muscular contribution to force closure of the pelvis. Eur Spine J 2004;13:199–205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van Wingerden JP, Vleeming A, Kleinrensink GJ, Stoeckart R. The role of the hamstrings in pelvic and spinal function. Vleeming A, Mooney V, Snijders CJ, Dorman TA, Stoeckart R.editors. Movement, stability and low back pain: the essential role of the pelvis 1997. New York: Churchill Livingstone; 207–10 [Google Scholar]
- 17.Cibulka MT, Rose SJ, Delitto A, Sinacore DR. Hamstring muscle strain treated by mobilizing the sacroiliac joint. Phys Ther 1986;66:1220–3 [DOI] [PubMed] [Google Scholar]
- 18.Hoehler FK, Tobis JS. Low back pain and its treatment by spinal manipulation: measures of flexibility and asymmetry. Rheumatol Rehabil 1982;21:21–6 [DOI] [PubMed] [Google Scholar]
- 19.Hoskins WT, Pollard HP. Hamstring injury management – Part 2: Treatment. Man Ther 2005;10:180–90 [DOI] [PubMed] [Google Scholar]
- 20.Hoskins WT, Pollard HP. Successful management of hamstring injuries in Australian Rules footballers: two case reports. Chiropr Osteopat 2005;13:1–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fox M. Effect on hamstring flexibility of hamstring stretching compared to hamstring stretching and sacroiliac joint manipulation. Clin Chiropr 2006;9:21–32 [Google Scholar]
- 22.Pollard H, Ward G. The effect of upper cervical or sacroiliac manipulation on hip flexion range of motion. J Manipulative Physiol Ther 1998;21:611–6 [PubMed] [Google Scholar]
- 23.Laslett M, Young S, Aprill C, McDonald B. Diagnosis of sacroiliac joint pain: validity of individual provocation tests and composites of tests. Man Ther 2005;10:207–18 [DOI] [PubMed] [Google Scholar]
- 24.Young S, Aprill C, Laslett M. Correlation of clinical examination characteristics with three sources of chronic low back pain. Spine J 2003;3:460–5 [DOI] [PubMed] [Google Scholar]
- 25.Kokmeyer DJ, van der Wurff P, Aufdemkampe G, Fickenscher TC. The reliability of multitest regimens with sacroiliac pain provocation tests. J Manipulative Physiol Ther 2002;25:42–8 [DOI] [PubMed] [Google Scholar]
- 26.Robinson HS, Brox JI, Robinson R, Bjelland E, Solem S, Telje T. The reliability of selected motion- and pain provocation tests for the sacroiliac joint. Man Ther 2007;12:72–9 [DOI] [PubMed] [Google Scholar]
- 27.Slipman CW, Sterenfeld EB, Chou LH, Herzog R, Vresilovic E. The predictive value of provocative sacroiliac joint stress maneuvers in the diagnosis of sacroiliac joint syndrome. Arch Phys Med Rehabil 1998;79:288–92 [DOI] [PubMed] [Google Scholar]
- 28.van der Wurff P, Hagmeijer RH, Meyne W. Clinical tests of the sacroiliac joint. A systemic methodological review. Part 1: Reliability. Man Ther 2000;5:30–6 [DOI] [PubMed] [Google Scholar]
- 29.van der Wurff P, Meyne W, Hagmeijer RH. Clinical tests of the sacroiliac joint. A systemic methodological review. Part 2: Validity. Man Ther 2000;5:89–96 [DOI] [PubMed] [Google Scholar]
- 30.Laslett M, Williams M. The reliability of selected pain provocation tests for sacroiliac joint pathology. Spine 1994;19:1243–9 [DOI] [PubMed] [Google Scholar]
- 31.Cleland J. Orthopaedic clinical examination: an evidence-based approach for physical therapists. Philadelphia, PA: Saunders; 2007. 215–28 [Google Scholar]
- 32.Laslett M, Young S, Aprill C, McDonald B. Diagnosing painful sacroiliac joints: a validity study of a McKenzie evaluation and sacroiliac provocation tests. Aust J Physiother 2003;49:89–97 [DOI] [PubMed] [Google Scholar]
- 33.Helewa A, Goldsmith C, Smythe H. Patient, observer and instrument variation in the measurement of strength of shoulder abductor muscles in patients with rheumatoid arthritis using a modified sphygmomanometer. J Rheumatol 1986;13:1044–9 [PubMed] [Google Scholar]
- 34.Helewa A, Goldsmith CH, Smythe HA. The modified sphygmomanometer. An instrument to measure muscle strength: a validation study. J Chronic Disord 1981;34:553–61 [DOI] [PubMed] [Google Scholar]
- 35.Nadler SF, Malanga GA, Feinberg FH, Prybicien M, Stitik TP, DePrinice M. Relationship between hip muscle imbalance and occurrence of low back pain in collegiate athletes. Am J Phys Med Rehabil 2001;80:572–7 [DOI] [PubMed] [Google Scholar]
- 36.Portney LG, Watkins MP. Foundations of clinical research: applications to practice. 3rd ed.Upper Saddle River, NJ: Prentice Hall; 2008. 635–9 [Google Scholar]
- 37.MedCalc Software bvba. MedCalc statistical software. Broekstraat 52, B-9030 Mariakerke, Belgium. [Google Scholar]
- 38.Lee D. The Pelvic Girdle – an approach to examination and treatment of the lumbo-pelvic-hip region. Philadelphia, PA: Churchill Livingston; 2004. 41–54 [Google Scholar]
- 39.Vleeming A, Pool-Goudzwaard AL, Hammudoghlu D, Stoeckart R, Snijders CJ, Mens JM. The function of the long dorsal sacroiliac ligament: its implication for understanding low back pain. Spine 1996;21:556–62 [DOI] [PubMed] [Google Scholar]
- 40.Vleeming A, Stoeckart R, Snijders CJ. The sacrotuberous ligament: A conceptual approach to its dynamic role in stabilizing the sacroiliac joint. Clin Biomech 1989;4:201–3 [Google Scholar]
- 41.Comstock CP, Carragee EJ, O'Saullivan GS. pondylolisthesis in the young athlete. S Phys Sports Med 1994;22:39–46 [DOI] [PubMed] [Google Scholar]
- 42.Motley G, Nyland J, Jacobs J, Caborn DN. The Pars interaticularis stress reaction, spondylolysis and spondylolisthesis progression. J Athl Train 1998;33:351–8 [PMC free article] [PubMed] [Google Scholar]


