Abstract
Background
International cohort studies have shown that antiretroviral treatment (ART) has improved survival of HIV-infected individuals. National population based studies of HIV mortality exist in industrialized settings but few have been presented from developing countries. Our objective was to investigate on a population basis, the regional situation regarding HIV mortality and trends in Latin America (LA) in the context of adoption of public ART policies and gender differences.
Methods
Cause of death data from vital statistics registries from 1996 to 2007 with "good" or "average" quality of mortality data were examined. Standardized mortality rates and Poisson regression models by country were developed and differences among countries assessed to identify patterns of HIV mortality over time occurring in Latin America.
Results
Standardized HIV mortality following the adoption of public ART policies was highest in Panama and El Salvador and lowest in Chile. During the study period, three overall patterns were identified in HIV mortality trends- following the adoption of the free ART public policies; a remarkable decrement, a remarkable increment and a slight increment. HIV mortality was consistently higher in males compared to females. Mean age of death attributable to HIV increased in the majority of countries over the study period.
Conclusions
Vital statistics registries provide valuable information on HIV mortality in LA. While the introduction of national policies for free ART provision has coincided with declines in population-level HIV mortality and increasing age of death in some countries, in others HIV mortality has increased. Barriers to effective ART implementation and uptake in the context of free ART public provision policies should be further investigated.
Background
The worldwide scale-up of antiretroviral therapy (ART) has substantially improved survival and quality of life of HIV-infected individuals. There is clear evidence that mortality associated with AIDS as well as incidence of AIDS-defining clinical conditions have fallen drastically in industrialized countries that provide good access to ART, such as the United States and Western European countries [1-9]. Improvement in survival among AIDS patients in developing countries has also been documented [10-12].
Despite increases in ART coverage to more than 4 million people in low- and middle-income countries by 2008 [13], HIV/AIDS has continued to be the fourth most frequent cause of death in low income countries [14]. Greater evidence is needed to better understand the impact of the HIV epidemic and AIDS mortality following the introduction of ART.
Models for the HIV epidemic for Latin America (LA) have shown a 21% increment in HIV annual mortality between 2001 and 2004 and a drop to 16% in the year 2008 [15]. The decline between 2004 and 2008 has been associated with increased availability and access to ART throughout the Latin American region [15]. Yet, differences both among and within countries exist and treatment coverage continues to be suboptimal in many areas [16-18].
Studies including cohorts from Latin American countries have shown improvements in survival among patients on ART [16,19]. In addition to HIV cohorts, the study of vital registration data and reported mortality due to HIV/AIDS can provide insight regarding the impact of HIV programs and policies at the population level. Several countries in LA have conducted trend analyses of reported HIV mortality [20-31]. Here, we provide a regional analysis of HIV/AIDS mortality between 1996 and 2007, in the context of adoption of public policies marking commencement of national provision of ART between 1997 and 2004 in Latin American countries with mortality records classified from average to good quality. The objective was to analyze patterns and trends in population-level mortality due to HIV/AIDS among Latin American countries and compare age-adjusted trends in mortality by sex.
Methods
This study draws on national vital registration mortality data from Latin American countries for the available years at the time of analysis using ICD10-coded data. Only countries with "good" or "average" quality mortality registration data, according to the Pan American Health Organization (PAHO) [32,33], were examined. The classification for quality of mortality data relies on a composite index based on the proportion of estimated mortality under-registration and on the proportion of deaths assigned to ill-defined and unknown causes. The index was calculated for each country for the years 2003 to 2005, using the formula:
Countries were classified according to the value of the index as having good quality (index ≤ 10%; Argentina, Chile, Cost Rica, Guatemala, Mexico, Uruguay, and Venezuela), average quality (11 to 20%; Brazil, Colombia, Ecuador, El Salvador, and Panama), poor or very poor quality (21 to 40%, and > 41%; Nicaragua, Peru, Bolivia, Paraguay) data. No data was available for Honduras and Guatemala was excluded because mortality data was only available for the years 2005 and 2006.
Data sources and analysis
HIV/AIDS mortality data were obtained from the PAHO database of reported mortality data [34] by cause of death, age and sex. This information is produced by national vital statistics departments, registries and ministries of health and is reported annually by ministries of health in LA to PAHO.
Crude mortality rates were calculated using the 2006 population estimates of the Division of Population of the United Nations as denominators. The numerators were the number of registered deaths for which the underlying cause of death was "Acquired Immunodeficiency Syndrome (AIDS)", corresponding to ICD-10 codes: B20 to B24. No correction for mortality under-registration or redistribution of causes was undertaken.
Poisson regression models were fitted by country to obtain adjusted rate ratios by year, age group and sex, using as baseline the year of commencement of public provision of antiretroviral therapy, as well as to test differences in time trends. When statistically significant differences in trends by sex were detected, using likelihood ratio tests, separate models for men and women were fit and tendencies by sex were presented separately. Processing and analysis of the data was carried out using STATA SE 11.0 for Windows (Stata Corporation, College Station TX, USA).
Age group categories used for standardization of death rates and for regression models were 0 to 4, 5 to 14, 15 to 24, 25 to 44, 45 to 64, and 65 years and over. Mean age at time of death was determined using mean mid-age-group data at time of death. These data were available in aggregated one-year age groups from 1 to 4 years in age and in five-year age groups thereafter. Comparisons of means were conducted using analysis of variance (ANOVA) when comparing by sex and year. Cases of unknown sex or age were included for the analysis of total mortality rates.
In 1996, Brazil became the first developing country to commit to and implement policies to provide free and universal access to highly active antiretroviral therapy (ART). Currently all countries in Latin America have established public policies that provide ART free of charge within designated publicly financed health service facilities. For purposes of the study, we defined the year when this occurred as the year when the national government first published a document delineating a national policy of provision of free of charge ART to all patients in need of treatment [35-39]. All countries included in the study had national ART guidelines that defined first-line regimens. The level of implementation of national guidelines is thought to be uneven within and among countries due to treatment costs, barriers to HIV testing and limitations in health services capacity in each country [40], yet is not known with precision. National estimates of ART coverage between 2004 and 2009 appear in Table 1.
Table 1.
Population, number and HIV prevalence, ART coverage, and establishment of national policy for public provision of ART (year), % of male deaths, HIV mortality rate ratios in men compared to women 1996-2007
| Country | Country population 2009 (in thousands) |
Number of persons living with HIV: Total/females 2001/2009 |
15-49 years old estimated HIV prevalence (%) 2001/2009 |
Estimated ART coverage (%) 2004** | Year of National ART Policy | % male deaths | Male-female HIV mortality rate ratio *** 95% confidence interval |
|---|---|---|---|---|---|---|---|
| Argentina | 40,666 | 110000/36000 | 0.4/0.5 | 88 | 19971 | 74.0% | 2.8 (2.7-2.9) |
| Brazil | 195424 | NA | [0.3-0.5]/[0.3-0.6]¥ | [70-95] ¥ | 19962 | 70.1% | 2.3 (2.3-2.4) |
| Chile | 17134 | 40000/12000 | 0.3/0.4 | 72 | 20013 | 87.45% | 6.9 (6.3-7.6) |
| Colombia | 46299 | 160000/50000 | 0.8/0.5 | 20 | 19994 | 81.1% | 4.3 (4.1-4.4) |
| Costa Rica | 4641 | 9800/2800 | 0.2/0.3 | 95 | 19975 | 84.8% | 5.6 (4.8-6.4) |
| Ecuador | 13772 | 37000/11000 | 0.5/0.4 | 10 | 20036 | 82.6% | 4.7 (4.4-5.1) |
| El Salvador | 6193 | 34000/11000 | 0.8/0.8 | 23 | 20047 | 72.3% | 2.6 (2.4-2.8) |
| Mexico | 110647 | 220000/59000 | 0.3/0.3 | 46 | 20038 | 83.8% | 5.2 (5.0-5.3) |
| Panama | 3507 | 20000/6300 | 1.4/0.9 | 25 | 20019 | 75.0% | 3.0 (2.8-3.2) |
| Uruguay | 3373 | 9900/3100 | 0.4/0.5 | 95 | 199710 | 76.4% | 3.2 (2.8-3.8) |
| Venezuela | 29044 | NA | NA | NA | 199911 | 81.7% | 4.5 (4.3-4.7) |
Source column #1: UN Population projections. Source columns #3, 4 and 5: UNAIDS. Report on the global AIDS epidemic 2010, Geneva, 2010
* Data unavailable for: Panama for 2005; Uruguay for 2002.
ART: antiretroviral therapy
IRR = Incidence rate ratio
** ART coverage using as numerator persons reported on treatment at end of reporting year and denominator the estimated treatment need criteria CD4 < 200.
1. National UNGASS report-Argentina, 2008
2. National UNGASS report -Brasil, 2008
3. National UNGASS report -Chile, 2008
4. OPS/ORAS/ONUSIDA Análisis de la situación de VIH en la subregión andina, 2003-2008, March 2007.
5. National UNGASS report -Costa Rica, 2008
6. National UNGASS report -Ecuador, 2008
7. National UNGASS report -El Salvador, 2008
8. National UNGASS report -México, 2008
9. National UNGASS report -Panamá, 2008
10. Ministerio de Salud Publica. Resolution Nª171/1997, that includes universal access to ARV drugs to all AIDS patients. Uruguay 1997
11. PAHO. Legislation and milestones on access to treatment in Latin America and the Caribbean. Pan American Health Organization. August 2003. Last accessed 30/1/2010. Available at http://www.paho.org/Spanish/AD/FCH/AI/acceso-arv-06.doc
*** Ratios adjusted for age groups and over time for the study period, p < 0.000 for all rate ratios.
NA: Not available
¥: point estimate unavailable for Brazil, modelled uncertainty interval provided
To compare HIV mortality trends among countries, age-standardized mortality rates were calculated for each year using the direct standardization method. The sum of the population estimates for the year 2000 from the Division of Population of the United Nations for the countries included in the study was used as the reference population. The ratio of standardized mortality rates for men relative to women adjusted for age was estimated for each country over the time period to summarize differences by sex.
Results
HIV/AIDS mortality rates were analyzed for the years 1996 to 2007. Most countries had available data for the years 1997 to 2006. The mean mortality follow up was 9.9 years, with a range of 7 years (for Uruguay) to 12 years (for Brazil) (Table 1). The mean crude HIV mortality rate over the study period was 5.3 per 100,000 population (95% CI 4.7-5.8) with a range of 3.0 to 13.1 per 100,000 across countries.a
Mortality patterns and trends
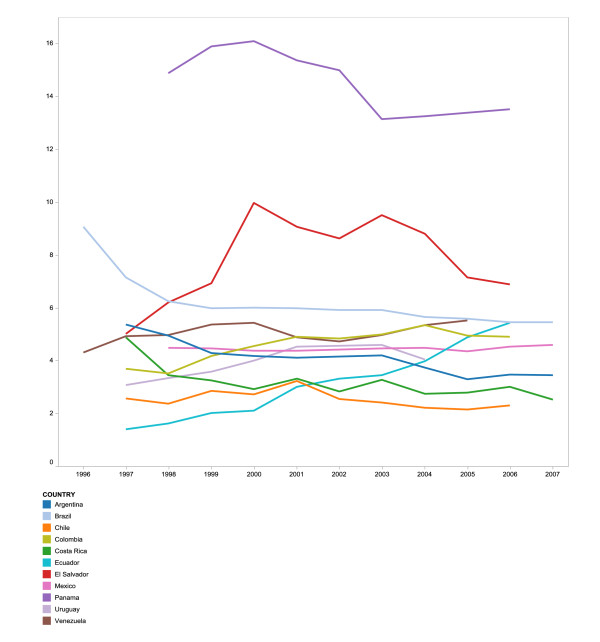
Age and sex-standardized mortality rates in the period prior to the adoption of public ART policies in the different countries ranged from 2.2 to 15.6 deaths per 100,000 (mean 5.7, CI 4.1-7.2). In comparison, after the ART public policy adoption the rates were 2.5 to 14.0 (mean 5.1, CI 4.5-5.7; p = 0.4). During the study periods of 1999 to 2004 and 2006, Panama, followed by El Salvador, presented the highest HIV mortality rates and Chile the lowest. Standardization did not alter the HIV mortality rates substantially. HIV mortality trends appear to follow three patterns. About half of the countries present a remarkable decrement in HIV mortality rates after the initiation of public provision of ART (Argentina, Brazil, Chile, Costa Rica and El Salvador). In Panama, the mortality rate decreased after the official start date of public ART provision, but this reduction did not achieve statistical significance. A second group of countries (Colombia and Ecuador) presented a remarkable increment in the HIV mortality trends. Finally, Mexico, Venezuela and Uruguay had varied trends in rate ratios with an overall increasing mortality pattern after adopting the public ART policies (Figure 1). Increase in male and female mortality rates, relative to the year of establishment of free ART public policies, varied from 12% to 39% among countries with an increasing trend, and declined by 15% to 54% for those with a decreasing trend.
Figure 1.
Sex and age-adjusted HIV mortality rate per 100,000 population.
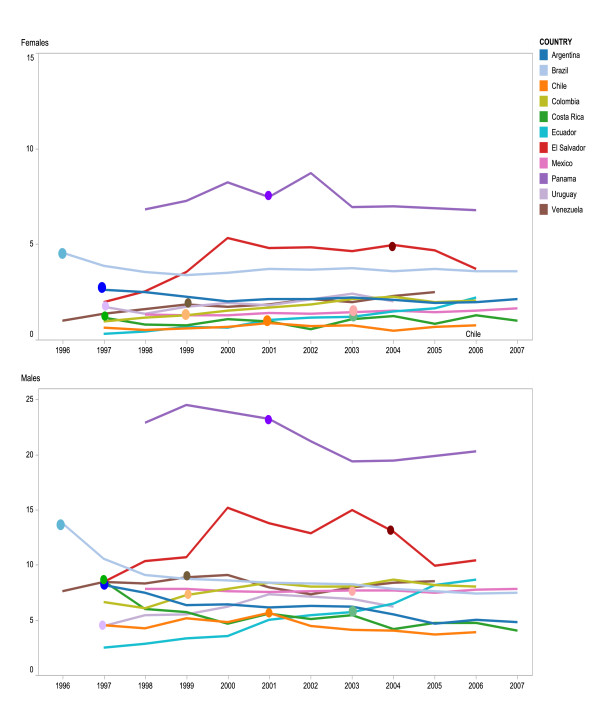
HIV mortality rates by country were much higher in males when compared to females over the study period, comprising 75% of total HIV/AIDS deaths and with rate ratios from 2.3 to 6.9 relative to females across countries (Table 1) (Figure 2). When evaluating the HIV mortality trends by sex groups significant differences were detected in Argentina, Brazil, Costa Rica, El Salvador, Colombia, Mexico and Venezuela (p < 0.001), not so in Chile, Ecuador, Panama and Uruguay.(Tables 2 and 3).
Figure 2.
Age-adjusted HIV mortality rate per 100,000 by sex in Latin American countries, 1996-2007. Note at bottom of figure: Dot on trends lines mark start year of national provision of antiretroviral treatment.
Table 2.
Age-Adjusted HIV mortality rate ratios 1996-2007 among countries with significant differences in time trend by sex
| Argentina | Brazil | Colombia | Costa Rica | El Salvador | Mexico | Venezuela | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F (95% CI) |
M (95% CI) |
F (95% CI) |
M (95% CI) |
F (95% CI) |
M (95% CI) |
F (95% CI) |
M (95% CI) |
F (95% CI) |
M (95% CI) |
F (95% CI) |
M (95% CI) |
F (95% CI) |
||
| 1996 | -- | -- | 1.00 | 1.00 | -- -- |
-- -- |
-- | -- | -- | -- -- |
-- -- |
-- | 0.80 (0.73-0.87) | 0.52 (0.41-0.65) |
| 1997 | 1.00 | 1.00 | 0.78 (0.76-0.80) |
0.87 (0.83-0.91) |
0.87 (0.81-0.94) |
0.73 (0.61-0.88) |
1.00 | 1.00 | 0.53 (0.45-0.63) |
0.34 (0.25-0.46) |
-- -- |
-- | 0.91 (0.83-0.99) | 0.72 (0.58-0.89) |
| 1998 | 0.93 (0.86-1.0) |
0.96 (0.84-1.1) |
0.69 (0.67-0.71) |
0.81 (0.77-0.85) |
0.81 (0.75-0.88) |
0.89 (0.75-1.07) |
0.73 (0.57-0.93) |
0.68 (0.35-1.39) |
0.66 (0.57-0.78) |
0.44 (0.34-0.59) |
0.91 (0.87-0.95) |
0.81 (0.73-0.90) |
0.91 (0.84-0.99) | 0.86 (0.70-1.05) |
| 1999 | 0.81 (0.75-0.87) |
0.87 (0.76-1.0) |
0.67 (0.65-0.69) |
0.79 (0.75-0.83) |
1.00 | 1.00 | 0.71 (0.55-0.90) |
0.67 (0.35-1.39) |
0.71 (0.61-0.83) |
0.63 (0.49-0.80) |
0.94 (0.90-0.98) |
0.80 (0.72-0.89) |
1.00 | 1.00 |
| 2000 | 0.83 (0.77-0.90) |
0.80 (0.70-0.92) |
0.68 (0.66-0.70) |
0.83 (0.80-0.87) |
1.10 (1.02-1.18) |
1.23 (1.05-1.45) |
0.60 (0.47-0.78) |
0.98 (0.57-1.94) |
1.03 (0.90-1.19) |
0.98 (0.79-1.22) |
0.93 (0.89-0.98) |
0.84 (0.76-0.94) |
1.05 (0.96-1.14) | 0.98 (0.81-1.18) |
| 2001 | 0.81 (0.75-0.87) |
0.87 (0.76-1.0) |
0.67 (0.65-0.69) |
0.90 (0.86-0.94) |
1.20 (1.12-1.29) |
1.39 (1.18-1.62) |
0.74 (0.58-0.94) |
0.86 (0.51-1.78) |
0.98 (0.85-1.13) |
0.91 (0.73-1.14) |
0.94 (0.90-1.0) |
0.92 (0.83-1.02) |
0.93 (0.85-1.02) | 1.06 (0.89-1.28) |
| 2002 | 0.84 (0.78-0.91) |
0.88 (0.77-1.01) |
0.68 (0.65-0.69) |
0.91 (0.87-0.95) |
1.18 (1.10-1.27) |
1.54 (1.32-1.79) |
0.69 (0.54-0.88) |
0.49 (0.26-1.15) |
0.93 (0.81-1.07) |
0.94 (0.76-1.18) |
0.98 (0.93-1.02) |
0.93 (0.84-1.03) |
0.88 (0.81-0.96) | 1.25 (1.04-1.49) |
| 2003 | 0.86 (0.79-0.93) |
0.95 (0.83-1.1) |
0.69 (0.67-0.71) |
0.95 (0.90-1.0) |
1.21 (1.13-1.30) |
1.8 (1.55-2.09) |
0.75 (0.59-0.95) |
1.01 (0.63-2.10) |
1.11 (0.97-1.28) |
0.93 (0.74-1.16) |
1.00 | 1.00 | 0.99 (0.91-1.10) | 1.18 (0.98-1.41) |
| 2004 | 0.78 (0.72-0.85) |
0.90 (0.79-1.04) |
0.67 (0.65-0.69) |
0.93 (0.89-0.98) |
1.33 (1.24-1.42) |
1.95 (1.68-2.26) |
0.60 (0.47-0.78) |
1.16 (0.76-2.40) |
1.00 | 1.00 | 1.02 (0.97-1.06) |
1.07 (0.97-1.18) |
1.06 (0.97-1.16) | 1.42 (1.19-1.69) |
| 2005 | 0.69 (0.63-0.75) |
0.87 (0.76-1.0) |
0.66 (0.64-0.68) |
0.98 (0.93-1.02) |
1.28 (1.19-1.37) |
1.75 (1.50-2.03) |
0.69 (0.54-0.88) |
0.76 (0.48-1.70) |
0.77 (0.67-0.90) |
0.98 (0.78-1.21) |
1.01 (0.96-1.05) |
1.05 (0.95-1.16) |
1.11 (1.02-1.21) | 1.58 (1.33-1.88) |
| 2006 | 0.75 (0.69-0.81) |
0.89 (0.77-1.01) |
0.66 (0.64-.68) | 0.97 (0.93-1.02) | 1.28 (1.20-1.37) |
1.86 (1.60-2.16) |
0.71 (0.56-0.91) |
1.20 (0.82-2.56) |
0.84 (0.72-0.97) |
0.79 (0.62-0.99) |
1.07 (1.02-1.11) |
1.12 (1.02-1.24) |
--- | -- |
| 2007 | 0.74 (0.68-.80) | 0.99 (0.87-1.13) | 0.68 (0.66-0.70) | 0.99 (0.95-1.04) | -- -- |
-- -- |
0.62 (0.48-0.80) |
0.98 (0.66-2.17) |
-- -- |
1.10 (1.04-1.14) | 1.22 (1.12-1.34) | --- | -- | |
HIV mortality rate ratios are calculated relative to the year of commencement of large-scale public provision of ART
* Countries present in this table have statistically significant interactions between sex and year for HIV mortality.
Models adjusted for age groups. Likelihood ratio test for interaction of age with time trend < 0,05 for all countries.
95% CI = 95% confidence interval
Table 3.
Age-Adjusted HIV mortality rate ratios 1996-2007 among countries with no significant difference in time trend by sex
| Year | Chile | Ecuador | Panama | Uruguay |
|---|---|---|---|---|
| 1996 | --- | --- | --- | --- |
| 1997 | 0.74 (0.65-0.84) | 0.36 (0.30-0.44) | --- | 1.00 |
| 1998 | 0.69 (0.61-0.79) | 0.43 (0.36-0.51) | 0.89 (0.78-1.02) | 1.13 (0.85-1.50) |
| 1999 | 0.86 (0.76-0.97) | 0.55 (0.47-0.64) | 0.98 (0.86-1.11) | 1.21 (0.92-1.6) |
| 2000 | 0.83 (0.73-0.94) | 0.58 (0.50-0.68) | 1.02 (0.90-1.16) | 1.39 (1.10-1.80) |
| 2001 | 1.00 | 0.85 (0.73-0.97) | 1.00 | 1.55 (1.20-2.00) |
| 2002 | 0.80 (0.70-0.90) | 0.95 (0.82-1.10) | 1.00 (0.88-1.13) | --- |
| 2003 | 0.77 (0.68-0.87) | 1.00 | 0.89 (0.78-1.02) | 1.63 (1.27-2.11) |
| 2004 | 0.72 (0.64-0.82) | 1.17 (1.03-1.34) | 0.92 (0.81-1.05) | 1.51 (1.17-1.95) |
| 2005 | 0.71 (0.62-0.80) | 1.46 (1.30-1.70) | --- | --- |
| 2006 | 0.76 (0.67-0.86) | 1.65 (1.46-1.86) | --- | --- |
HIV mortality rate ratios are calculated relative to the year of commencement of large-scale public provision of ART
Countries present in this table do not have statistically significant interactions among sex and year for HIV mortality rates.
In Argentina, Brazil, Costa Rica and El Salvador, HIV mortality rates among males decreased significantly after the public provision of ART (p < 0.000) (Tables 2 and 3). In contrast, HIV mortality trends among women in those countries either show no decrease, such as in the case of Costa Rica, or show smaller, inconsistent and not statistically significant declines like in the remaining countries. On the contrary, in Colombia, Venezuela and Mexico the HIV mortality rates increased for both men and women (p < 0.000), after ART public provision (Table 2).
In relation with the ART coverage, those countries with high percentage of coverage (more than 70%) had a better HIV mortality outcome. On the contrary, those counties with lower coverage present an increment in their mortality trend (Tables 1, 2 and 3). However Uruguay, with an increasing mortality trend had a high ART coverage (95% in 2004).
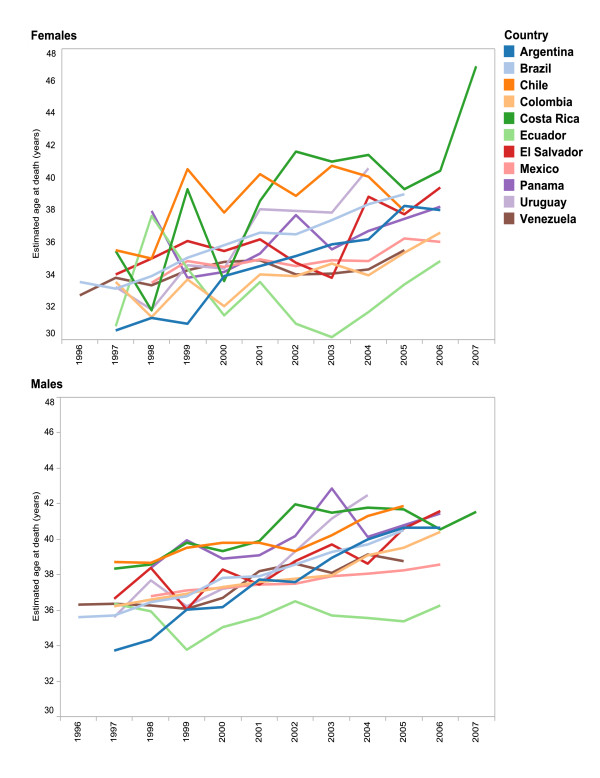
Mortality and age
For all countries, the highest mortality rate by age over the period was observed in the 25-44-years age group (p < 0.01)(data not shown). The estimated mean age at death increased over the study period around 2 to 8 years in all countries (p < 0.05), except in Ecuador where an increase in mean age at death occurred only among women. Statistical differences in mean age at death before and after public provision of ART appeared for all countries where mortality data was available (Chile, Colombia, El Salvador, Mexico, Panama, Venezuela) (p < 0.05), with the exception of Ecuador. Mean age at death was consistently lower for women over the period except in Chile and Costa Rica (p < 0.05) (Figure 3).
Figure 3.
Mean age at death, due to HIV, by sex, 1996-2007.
Discussion
This is the first article to present population trends in HIV mortality across selected Latin American countries. Results suggest that six out of the eleven countries examined show a decline in HIV mortality after the initiation of national policies providing free public-sector access to ART. The analysis also illustrates how men and women are affected and vulnerable with regards to HIV: adult men had consistently higher mortality due to HIV while women showed less improvement in rates over time and lower mean age at death.
The shift in mean age at HIV death, as measured in our data, ranged from 2 to 8 years. Many factors, including changes during the study period in HIV incidence overall and among specific age groups, an increase in HIV incidence among older adults [41-43], increase in life expectancy among HIV patients, access to and quality of ART, and patients' perceptions of ART availability and effectiveness, are likely to have influenced mortality rates during the period examined by this analysis. Our finding that introduction of national policies for public ART provision coincided with an increase in the mean age of death from 2 to 8 years requires further investigation to better understand the underlying factors. Among many possible explanations, an increase in survival of HIV-infected patients may be related to improved access and quality of ART and in the management and prophylaxis of opportunistic infections, as previously demonstrated in several cohort studies [44-46].
Mortality rates in this study were calculated relative to the census population so that observed changes may capture not only improvements in ART but also changes in epidemic dynamics. For example, decreasing HIV incidence with all other factors stable could, in theory, lead to mortality declines. However, estimated HIV cases and ART treatment caseloads increased, rather than decreased, in all countries included in this analysis during the period [13,47]. Similarly, an increase in the age distribution of incident cases could theoretically explain the increase in age of death observed in this study. Yet, this is unlikely to be the case as younger individuals continue to comprise the majority of reported HIV and AIDS cases [47].
The consistently elevated levels of mortality among men compared to women is most likely explained by the fact that men who have sex with men (MSM) continue to be one of the populations with the highest prevalence throughout Latin America [48]; and may also reflect prevalent gender norms, socioeconomic roles and structures that translate to gender inequities in access to timely diagnosis and treatment in Latin America, including homophobia and machismo [49,50].
Differentials in access to HIV services between men and women could contribute to differences in mortality, however the direction of this effect is unclear. Some studies in Latin America have found that women tend to start ART with higher CD4 counts than men, which could be attributed to the scale-up of HIV screening in pregnant women as an entry point to HIV care and treatment. This delay in the HIV detection in the male group could partially explain a higher HIV related mortality. On the other hand, socioeconomic disparities may affect women's ability to access adequate HIV treatments and services more than men both in the US and LA [51-53]. Our findings concurred with these previous publications.
The reduction in HIV mortality rates in the population appears remarkable. This begs the question of how, and how much, HIV mortality could be reduced further? In the United States, the age-adjusted HIV death rate fell by 28% from 1995 to 1996, by 46% from 1996 to 1997, and by 18% from 1997 to 1998. After 1998, the rate leveled off at around 5 per 100,000, which is similar to the level reported in Brazil, Argentina and Costa Rica for the same period [54,55]. Other factors also affect HIV mortality such as the unrelenting occurrence of new infections, lagging ART coverage in some areas, late presentation for HIV care with delayed ART uptake, suboptimal treatment and adherence and lack of treatment options [56]. Specific age, sex and gender identity subgroups may still be experiencing higher HIV mortality even within countries that have substantially lowered their rates. At the regional level this information is not available to conduct more in-depth analysis. National institutions, particularly those where mortality has remained stable or increased, should engage in operational research to identify lost opportunities in the response effort and address inequities in services' access that further reduce HIV mortality.
ART coverage and rate of scale-up, which were not captured in the models, differed among countries and were likely to influence HIV mortality trends. ART coverage may have been too low in some countries to reduce HIV mortality levels. This may be the case in Ecuador where ART scale-up was limited until 2006, when international funds became available [57,58].
Moreover, the rise in HIV mortality seen in some countries may have resulted from a gap in primary and secondary prevention and including late HIV testing and diagnosis, low adherence and issues in treatment quality despite relatively high ART coverage [13,16,46].
An effective universal ART coverage is one goal for controlling the HIV/AIDS epidemic. The introduction of policies that make the access of ART universal and free are key to fulfill this goal, but in reality their coverage varied greatly among the different countries. Furthermore, there are countries with low coverage and this issue could explain the mortality trends differences found in the study.
The principal limitations of the study are associated with the source and quality of the data. Errors in registered mortality could occur during data reporting collection and processing as well as by limitations in medical knowledge, diagnostic errors and deficiencies in the death certification. The validity of the distribution by cause is also affected by under reporting of deaths and cause of death certification, even when conducted by physicians. In many Latin American countries, registration of death is not performed by physicians, particularly in remote and rural areas, which can compromise the accuracy of cause of death classification. Physicians may also prefer certain kinds of diagnoses, introducing biases that may vary from country to country and over time [59]. In addition, legal and societal concerns may lead to the underreporting of causes of a sensitive nature, such as HIV, on the death certificate [59]. Another limitation of the study is the difference in the time of follow up after public ART introduction. Some like Brazil had 11 years of follow up while others, like El Salvador, had only 2 years of follow up post public ART provision.
We also expect some degree of bias due to variation in correct HIV diagnosis and cause of death registration over time. Tendencies to misclassify as well as intentionally replace the registered cause of death may change over time. For example, opportunistic infections and cancers may be more frequently recorded as cause of death in lieu of HIV [7,60-62]. The degree, to which such effects occur, however, is unclear and should be examined further.
Conclusions
Despite limitations, vital statistics are an important source of information to study the impact of the HIV epidemic at the population level in Latin America and to monitor the joint impact of response efforts. Given potential biases, this information should be analyzed in conjunction with other sources of data, such as HIV case-based reporting, biological and behavioural surveillance, HIV drug resistance surveillance, and coverage of prevention and treatment services in order to adequately monitor the epidemic and its response.
Given the differences by sex found in this study, future assessments of the response to HIV should include a gender perspective and explicitly examine sex and socioeconomic disparities with respect to services, norms and laws that may constitute barriers to service access. Similarly, intervention efforts should seek to involve both men and women as part of an equitable response [63,64]. These results provide useful information to support the monitoring of the epidemic, informing policy and programmatic action, and to motivate efforts to improve the effectiveness of ART implementation and uptake. Further improvement in vital registration data and analysis are needed to improve understanding of the behavior of the HIV epidemic, including sex and gender differences and resulting mortality.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
MAG: Had the original idea, compiled the data, conducted the bibliographical review, wrote the text, prepared the figures and coordinated the overall study. LM: Conducted part of the analysis, prepared the tables, and contributed in writing the text. SM: provided statistical advice and conducted the majority of the statistical analysis. He also contributed to reviewing the text. JOJ: reviewed the text, tables and figures, providing meaningful contributions to the text, analysis and tables and contributed to the bibliographical review. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
Monica Alonso Gonzalez, Email: alonsomon@paho.org.
Luise Martin, Email: luisemartin@web.de.
Sergio Munoz, Email: munozs@ufro.cl.
Jerry O Jacobson, Email: jacobjen@col.ops.oms.org.
Acknowledgements
We thank Dr. Txema Garcia Calleja and Dr. Fatima Marinho for their comments to the study and text. We also thank PAHO member states and their Statistical Registry Departments from which the data originate.
Endnotes
aCrude rates (not shown) can be requested from authors.
References
- Survival after introduction of HAART in people with known duration of HIV-1 infection. The CASCADE Collaboration. Concerted Action on SeroConversion to AIDS and Death in Europe. Lancet. 2000;355(9210):1158–9. [PubMed] [Google Scholar]
- Detels R, Munoz A, McFarlane G, Kingsley LA, Margolick JB, Giorgi J. et al. Effectiveness of potent antiretroviral therapy on time to AIDS and death in men with known HIV infection duration. Multicenter AIDS Cohort Study Investigators. JAMA. 1998;280(17):1497–503. doi: 10.1001/jama.280.17.1497. [DOI] [PubMed] [Google Scholar]
- Holtgrave DR. Causes of the decline in AIDS deaths, United States, 1995-2002: prevention, treatment or both? Int J STD AIDS. 2005;16(12):777–81. doi: 10.1258/095646205774988109. [DOI] [PubMed] [Google Scholar]
- Mocroft A, Ledergerber B, Katlama C, Kirk O, Reiss P, d'Arminio MA. et al. Decline in the AIDS and death rates in the EuroSIDA study: an observational study. Lancet. 2003;362(9377):22–9. doi: 10.1016/S0140-6736(03)13802-0. [DOI] [PubMed] [Google Scholar]
- Palella FJ Jr, Delaney KM, Moorman AC, Loveless MO, Fuhrer J, Satten GA. et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med. 1998;338(13):853–60. doi: 10.1056/NEJM199803263381301. [DOI] [PubMed] [Google Scholar]
- Perez-Hoyos S, Del AJ, Muga R, del RJ, Garcia de OP, Guerrero R. et al. Effectiveness of highly active antiretroviral therapy in Spanish cohorts of HIV seroconverters: differences by transmission category. AIDS. 2003;17(3):353–9. doi: 10.1097/00002030-200302140-00009. [DOI] [PubMed] [Google Scholar]
- Secretaría del Plan Nacional sobre SIDA. VIH y sida en España. Situación epidemiológica 2001. Madrid: Ministerio de Sanidad y Consumo; 2002. [Google Scholar]
- Serraino D, Zucchetto A, Suligoi B, Bruzzone S, Camoni L, Boros S. et al. Survival after AIDS diagnosis in Italy, 1999-2006: a population-based study. J Acquir Immune Defic Syndr. 2009;52(1):99–105. doi: 10.1097/QAI.0b013e3181a4f663. [DOI] [PubMed] [Google Scholar]
- Druyts E, Lepik KJ, Anema A, Zhang W, Muldoon KA, Hogg RS, Regional disparities in HIV-related deaths and access to HAART: evidence from a province-wide universal healthcare system. Cape Town, South Africa; 2009. [Google Scholar]
- Braitstein P, Brinkhof MW, Dabis F, Schechter M, Boulle A, Miotti P. et al. Mortality of HIV-1-infected patients in the first year of antiretroviral therapy: comparison between low-income and high-income countries. Lancet. 2006;367(9513):817–24. doi: 10.1016/S0140-6736(06)68337-2. [DOI] [PubMed] [Google Scholar]
- Herbst AJ, Cooke GS, Barnighausen T, KanyKany A, Tanser F, Newell ML. Adult mortality and antiretroviral treatment roll-out in rural KwaZulu-Natal, South Africa. Bull World Health Organ. 2009;87(10):754–62. doi: 10.2471/BLT.08.058982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahn A, Floyd S, Crampin AC, Mwaungulu F, Mvula H, Munthali F. et al. Population-level effect of HIV on adult mortality and early evidence of reversal after introduction of antiretroviral therapy in Malawi. Lancet. 2008;371(9624):1603–11. doi: 10.1016/S0140-6736(08)60693-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization, UNAIDS, UNICEF. Towards universal access: scaling up priority HIV/AIDS interventions in the health sector: progress report 2009. Geneva: WHO; 2009. [Google Scholar]
- World Health Organization. Global health risks. Mortality and burden of disease attributable to selected major risks. Geneva: World Health Organization; 2009. [Google Scholar]
- UNAIDS, WHO. AIDS Epidemic Update 2009. Geneva: Joint United Nations Programme on HIV/AIDS; 2009. [Google Scholar]
- Tuboi SH, Schechter M, McGowan CC, Cesar C, Krolewiecki A, Cahn P. et al. Mortality during the first year of potent antiretroviral therapy in HIV-1-infected patients in 7 sites throughout Latin America and the Caribbean. J Acquir Immune Defic Syndr. 2009;51(5):615–23. doi: 10.1097/QAI.0b013e3181a44f0a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawn Sd, Harries AD, Wood R. Strategies to reduce early morbidity and mortality in adults receiving antiretroviral therapy in resource-limited settings. Curr Opin HIV AIDS. 2010;5(1):18–26. doi: 10.1097/COH.0b013e328333850f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The ART-LINC Collaboration of the International Databases to Evaluate AIDS (IeDEA) Antiretroviral therapy in resource-limited settings 1996 to 2006: patient characteristics, treatment regimens and monitoring in sub-Saharan Africa, Asia and Latin America. Tropical Medicine & International Health. 2008;13(7):870–9. doi: 10.1111/j.1365-3156.2008.02078.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nash D, Katyal M, Brinkhof MW, Keiser O, May M, Hughes R. et al. Long-term immunologic response to antiretroviral therapy in low-income countries: a collaborative analysis of prospective studies. AIDS. 2008;22(17):2291–302. doi: 10.1097/QAD.0b013e3283121ca9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministerio de Salud de Argentina Boletín sobre el VIH-SIDA en la Argentina: Año XII - número 26 - noviembre de 2009. [Año XII - número 26]. 2009. Buenos Aires, Ministerio de Salud, presidencia de la Nacion Boletín sobre el VIH-SIDA en la Argentina21216839
- Carlos Hernández-Girón, Víctor Tovar-Guzmán, Carlos del Río. AIDS mortality trends in Mexico, 1988-1997. Salud pública Méx [serial on the Internet] 2002;44(3):207–12. doi: 10.1590/s0036-36342002000300003. [DOI] [PubMed] [Google Scholar]
- García M, Olea A. Evolución y situación epidemiológica de la infección por virus de inmunodeficiencia humana y síndrome de inmunodeficiencia adquirida en Chile. Rev Chil Infect. 2008;25(3):162–70. [PubMed] [Google Scholar]
- Magis-Rodríguez C, Bravo-García E, Rivera P. El sida en Mexico en el año 2000. La respuesta mexicana al sida: Mejores practicas. Mexico City: Instituto Nacional de Salud Publica de Mexico; 2000. [Google Scholar]
- Carmen Soler Claudín. Universal access, six years results in the Mexico City HIV/AIDS Program. Salud pública Méx [serial on the Internet] 2009;51(1):26–33. doi: 10.1590/s0036-36342009000100007. [DOI] [PubMed] [Google Scholar]
- Bautista-Arredondo S, Mane A, Bertozzi S. Economic impact of antiretroviral therapy prescription decisions in the context of rapid scaling-up of access to treatment: lessons from Mexico. AIDS. 2006;20:101–9. doi: 10.1097/01.aids.0000198096.08444.53. [DOI] [PubMed] [Google Scholar]
- Caceres C, Mendoza W, Konda K, Lescano A. Nuevas evidencias en VIH - Perú. Lima: Universidad Peruana Cayetano Heredia; Organización Panamericana de la Salud; 2007. [Google Scholar]
- Ministerio de Salud de Chile. Situación epidemiológica de VIH/SIDA, Chile 1984-2008. Santiao de Chile, Chile: Ministerio de Salud de Chile; 2009. [Google Scholar]
- Candiani TM, Pinto J, Cardoso CA, Carvalho IR, Dias AC, Carneiro M. et al. Impact of highly active antiretroviral therapy (HAART) on the incidence of opportunistic infections, hospitalizations and mortality among children and adolescents living with HIV/AIDS in Belo Horizonte, Minas Gerais State, Brazil. Cad Saude Publica. 2007;23(Suppl 3):S414–S423. doi: 10.1590/s0102-311x2007001500009. [DOI] [PubMed] [Google Scholar]
- Brito AM, Castilho EA, Szwarcwald CL. Regional patterns of the temporal evolution of the AIDS epidemic in Brazil following the introduction of antiretroviral therapy. Braz J Infect Dis. 2005;9(1):9–19. doi: 10.1590/s1413-86702005000100004. [DOI] [PubMed] [Google Scholar]
- Publicación del Programa Municipal de Sida y el Sistema Municipal de Epidemiología. Boletín Epidemiológico Municipal de VIH/SIDA. Año 10. 2008. Report No.: 10.
- Reyes MP Rivera, Sánchez K Sánchez. Mortality caused by AIDS in Mexico: an analysis of future trends and projections. 2008.
- Pan American Health Organization. Health Situation in the Americas: Basic Indicators 2008. 1-6-2008. Washington, D.C, Pan American Health Organization. Health Situation in the Americas: Basic Indicators. PAHO: Health Information and Analysis; 2010. [Google Scholar]
- Pan American Health Organization, editor. Pan American Health Organization. Health Situation in The Americas. Basic Indicators 2009. Washington DC, Pan American Health Organization. Health Situation in the Americas: Basic Indicators. Pan American Health Organization, Health Information and Analysis; 2009. 1-2-2010. [Google Scholar]
- Health Statistics from the Americas, 2006 Edition. http://www.paho.org/english/dd/ais/HSA2006_TOC.pdf [cited 2010 Apr 20]
- Direcciónde Sida y ETS del Ministerio de Salud de la Nación Argentina RECOMENDACIONES PARA EL TRATAMIENTO ANTIRRETROVIRAL Buenos Aires, Argentina; 7 A.D 2007. 21808980
- Roy Wong-McClure María-Paz León-Bratti Efecto de la terapia antirretroviral en la rehospitalización por enfermedad oportunista en Costa Rica Acta méd.costarric 2006484179–184.1-2-201121781056 [Google Scholar]
- Schumacher C Precoz tratamiento antirretroviral logra reducir la mortalidad por sida Nación.com/aldea global 4-23-000921800621
- Bortman M, Saenz L, Pimenta I, Isern C, Rodriguez AE, Miranda M, Situación del VIH/SIDA y respuesta a la epidemia. Washington, DC: Banco Internacional de Reconstrucción y Fomento/Banco Mundial; 2006. [Google Scholar]
- Frasca T. AIDS in Latin America. New York: Palgrave MacMillan; 2005. [Google Scholar]
- Pan American Health Organization. 3 by 5 Report for the Americas. Washington DC: Pan American Health Organization; Toward Universal Access to HIV Prevention, Care, and Treatment. 6 A.D. Jun 20. [Google Scholar]
- Simone MJ, Appelbaum J. HIV in older adults. Geriatrics. 2008;63(12):6–12. [PubMed] [Google Scholar]
- Nguyen N, Holodniy M. HIV infection in the elderly. Clin Interv Aging. 2008;3(3):453–72. doi: 10.2147/cia.s2086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manfredi R. HIV infection and advanced age emerging epidemiological, clinical, and management issues. Ageing Res Rev. 2004;3(1):31–54. doi: 10.1016/j.arr.2003.07.001. [DOI] [PubMed] [Google Scholar]
- Campos DP, Ribeiro SR, Grinsztejn B, Veloso VG, Bastos FI, Morgado MG. et al. Survival of AIDS patients using two case definitions, Rio de Janeiro, Brazil, 1986-2003. AIDS. 2005;19:S22–S26. doi: 10.1097/01.aids.0000191486.92285.1c. [DOI] [PubMed] [Google Scholar]
- Nash D, Katyal M, Brinkhof MW, Keiser O, May M, Hughes R. et al. Long-term immunologic response to antiretroviral therapy in low-income countries: a collaborative analysis of prospective studies. AIDS. 2008;22(17):2291–302. doi: 10.1097/QAD.0b013e3283121ca9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zala C, Rustad CA, Chan K, Khan NI, Beltran M, Warley E. et al. Determinants of Treatment Access in a Population-based Cohort of HIV-positive Men and Women Living in Argentina. J Int AIDS Soc. 2008;10(4):78. doi: 10.1186/1758-2652-10-4-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LAC reported HIV cases. 2010. http://new.paho.org/hq/index.php?option=com_content&task=view&id=1610&Itemid=1410 [cited 2010 Jan 6]
- Calleja JM, Walker N, Cuchi P, Lazzari S, Ghys PD, Zacarias F. Status of the HIV/AIDS epidemic and methods to monitor it in the Latin America and Caribbean region. AIDS. 2002;16(Suppl 3):S3–12. doi: 10.1097/00002030-200212003-00002. [DOI] [PubMed] [Google Scholar]
- Uribe-Zuñiga P, Magis-Rodriguez C, Bravo Garcia E, Gayet Serrano C, Villegas-Icazabalceta L, Hernandez-Tepechin G. El SIDA en las mujeres: logros y asignaturas pendientes. Perinatol Reprod Hum. 2003;17:255–70. [Google Scholar]
- Bozon M, Gayet C, Barrientos J. A life course approach to patterns and trends in modern Latin American sexual behavior. J Acquir Immune Defic Syndr. 2009;51(Suppl 1):S4–S12. doi: 10.1097/QAI.0b013e3181a2652f. [DOI] [PubMed] [Google Scholar]
- Arrivillaga M, Ross M, Useche B, Alzate ML, Correa D. Social position, gender role, and treatment adherence among Colombian women living with HIV/AIDS: social determinants of health approach. Rev Panam Salud Publica. 2009;26(6):502–10. doi: 10.1590/S1020-49892009001200005. [DOI] [PubMed] [Google Scholar]
- Smith KY. Paying the price for late starts and early stops: racial and sex disparities in HIV-related mortality. Clin Infect Dis. 2009;49(10):1579–81. doi: 10.1086/644773. [DOI] [PubMed] [Google Scholar]
- Gebo KA, Fleishman JA, Conviser R, Reilly ED, Korthuis PT, Moore RD. et al. Racial and gender disparities in receipt of highly active antiretroviral therapy persist in a multistate sample of HIV patients in 2001. J Acquir Immune Defic Syndr. 2005;38(1):96–103. doi: 10.1097/00126334-200501010-00017. [DOI] [PubMed] [Google Scholar]
- Department of Health and Human Services CfDCaP, editor. Centers for Disease Control and Prevention. HIV/AIDS Surveillance Report, 2007. Atlanta, U.S, Department of Health and Human Services, Centers for Disease Control and Prevention; 2010. [19]. 7-3-2010. [Google Scholar]
- Jaggy C, von OJ, Ledergerber B, Schwarz C, Egger M, Rickenbach M. et al. Mortality in the Swiss HIV Cohort Study (SHCS. and the Swiss general population. Lancet. 2003;362(9387):877–8. doi: 10.1016/S0140-6736(03)14307-3. [DOI] [PubMed] [Google Scholar]
- Battegay M, Fehr J, Fluckiger U, Elzi L. Antiretroviral therapy of late presenters with advanced HIV disease. J Antimicrob Chemother. 2008;62(1):41–4. doi: 10.1093/jac/dkn169. [DOI] [PubMed] [Google Scholar]
- World Health Organization, editor. World Health Organization, UNAIDS, UNICEF. Towards universal access: scaling up priority HIV/AIDS interventions in the health sector. Progress Report 2007. Geneva, World Health Organization; 2007. [Google Scholar]
- World Health Organization. Progress on global access to HIV antiretroviral therapy: a report on "3 by 5" and beyond, March 2006. Geneva: World Health Organization; 2006. [Google Scholar]
- Hessol NA, Buchbinder SP, Colbert D, Scheer S, Underwood R, Barnhart JL. et al. Impact of HIV infection on mortality and accuracy of AIDS reporting on death certificates. Am J Public Health. 1992;82(4):561–4. doi: 10.2105/AJPH.82.4.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacheco AG, Tuboi SH, May SB, Moreira LF, Ramadas L, Nunes EP. et al. Temporal changes in causes of death among HIV-infected patients in the HAART era in Rio de Janeiro, Brazil. J Acquir Immune Defic Syndr. 2009;51(5):624–30. doi: 10.1097/QAI.0b013e3181a4ecf5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krentz HB, Kliewer G, Gill MJ. Changing mortality rates and causes of death for HIV-infected individuals living in Southern Alberta, Canada from 1984 to 2003. HIV Med. 2005;6(2):99–106. doi: 10.1111/j.1468-1293.2005.00271.x. [DOI] [PubMed] [Google Scholar]
- Bhaskaran K, Hamouda O, Sannes M, Boufassa F, Johnson AM, Lambert PC. et al. Changes in the risk of death after HIV seroconversion compared with mortality in the general population. JAMA. 2008;300(1):51–9. doi: 10.1001/jama.300.1.51. [DOI] [PubMed] [Google Scholar]
- Hankins C. Gender, sex, and HIV: how well are we addressing the imbalance? Curr Opin HIV AIDS. 2008;3(4):514–20. doi: 10.1097/COH.0b013e32830136b4. [DOI] [PubMed] [Google Scholar]
- Carael M, Marais H, Polsky J, Mendoza A. Is there a gender gap in the HIV response? Evaluating national HIV responses from the United Nations General Assembly Special Session on HIV/AIDS country reports. J Acquir Immune Defic Syndr. 2009;52(Suppl 2):S111–S118. doi: 10.1097/QAI.0b013e3181baeec2. [DOI] [PubMed] [Google Scholar]