Abstract
The intraoperative knowledge of margin status on mandibulectomy specimens is important for primary reconstruction. The goal of this study was to evaluate whether intraoperative bone marrow (BM) curettings and inferior alveolar nerve (IAN) biopsies are representative of final decalcified cross-sectional (shave) mandibular bone margins. Forty-seven margins in 27 patients consecutively treated with segmental mandibulectomy for squamous cell carcinoma were reviewed. These patients had BM or IAN margins sampled by surgeons and assessed intraoperatively by routine frozen section. The full cross-section of mandibular bone margins were sampled by pathologists at the time of routine gross examination. Intraoperative evaluation of BM/IAN biopsies is characterized by a 50% sensitivity (3 of 6 cases were false negative) and a 100% specificity. IAN biopsies are representative of the final bone margin. Given the technical feasibility of intraoperative BM and IAN assessment, we favor routine intraoperative evaluation of mandibular bone margins. However, even when bone margins are sampled intraoperatively, obtaining a full cross-section of the bone margin at the time of gross examination should also be performed as it remains the most accurate modality of bone margin assessment.
Keywords: Margins, Mandibulectomy, Squamous cell carcinoma, Frozen section
Introduction
Of all head and neck squamous cell carcinomas (SCC), oral SCCs with mandibular invasion have the highest local recurrence rates [1, 2]. In a study of 194 carcinomas of the oral cavity, tumors involving the mandibular alveolus had one of the highest recurrence rates (61.9%) and one of the lowest 5-year overall survival (25.8%) [2].
Primary reconstruction following segmental mandibulectomy improves quality of life [3, 4] and knowledge of the status of bone margins is desirable at the time of surgery before proceeding with immediate reconstruction.
However, preoperative clinical and radiographic assessment of bone invasion and of the extent of mandibular involvement is suboptimal. For instance, one-third of oral SCC with mandibular bone involvement showed no clinical signs of invasion [5]. Moreover, although bone invasion is routinely assessed by panoramic films, computed tomography (CT), and magnetic resonance imaging (MRI), half of the patients with apparently normal CT studies ultimately showed histologic evidence of bone invasion [5].
Once SCC involves bone marrow of the mandible, with or without invasion of the inferior alveolar nerve (IAN), there is little barrier to carcinomatous spread. However, frozen section evaluation of un-decalcified cortical bone is not practical. Alternatively, bone marrow (BM) curettings and IAN biopsies are commonly sent for intraoperative evaluation by frozen section. This observation prompted our review of segmental mandibulectomies in which bone margins were assessed by two modalities: (1) first by intraoperative frozen section of BM curettings or IAN biopsies obtained by the surgeon, and (2) later, by examination of decalcified full cross-section of mandibular bone margins sampled by pathologists.
The goal of this study was to evaluate whether BM curettings and IAN biopsies are representative of the entire cross-sectional mandibular bone margins. Three other groups addressed this issue previously [6–9]. However, the current study characterizes IAN biopsies as a complementary method of mandibular bone margin assessment. In addition, the current analysis was controlled for the status of soft tissue margins. The proximity of the positive soft tissue margin may influence the extent of mandibulectomy. Therefore, our study is restricted to segmental mandibulectomies with benign soft tissue margins. Furthermore, this study summarizes the current practices by several head and neck surgeons without special instrumentation.
Materials and Methods
Pathology records were searched from 02/2005 to 02/2010 for patients with oral SCC treated by segmental mandibulectomy. Inclusion criteria were as follows:
Histologic diagnosis of SCC with mandibular bony invasion (i.e., sarcomas, carcinomas metastatic to the mandible, and odontogenic neoplasms were excluded).
Segmental mandibulectomy was performed (cases of marginal mandibulectomy were excluded).
A full cross-section of the mandibular bone margin was obtained by a pathologist at the time of grossing.
All soft tissue margins were reported as benign. In all cases, the status of soft tissue margins was reported intra-operatively.
Cases satisfying these criteria from 02/2010 to 12/2010 were included prospectively. The BM and IAN were evaluated by frozen section, performed in a routine fashion (Fig. 1a) (identical to frozen sections performed for the evaluation of soft tissue margins). All BM margins assessed by frozen sections were biopsied by surgeons and sent to pathology via a pneumatic tube system. The main specimen (i.e., segmental mandibulectomy) is customarily received in a routine fashion, hours later, precluding its intraoperative gross examination. Only in one case, the mandibulectomy specimen was available for intraoperative review and the bone margin was sampled by the pathologist (as prompted by the surgeon). The BM samples were obtained by surgeons from the residual mandibular stump using a curette. Frozen section remnants were resubmitted for permanent sections (Fig. 1b). The true final shave bone margins were obtained from the resected mandible and represented a full cross-section of the anterior and posterior mandibular resection margins (Fig. 1c).
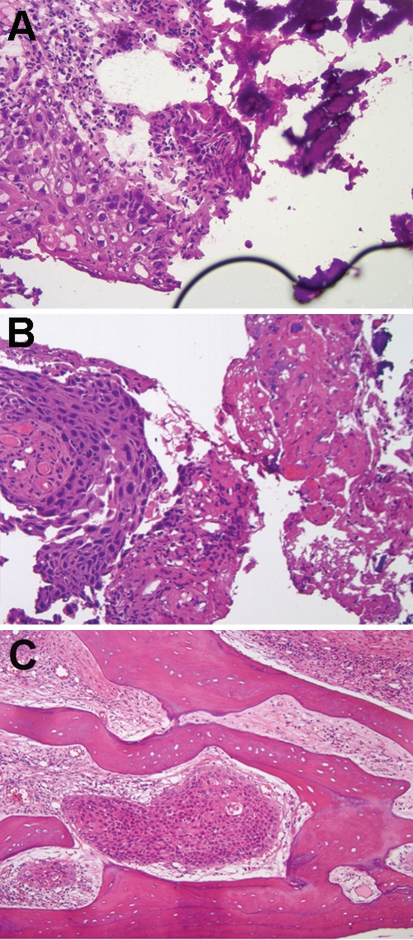
Fig. 1.
Representative case of segmental mandibulectomy with intraoperative evaluation of bone marrow. a Routine frozen section preparation of bone marrow. All intraoperative bone marrow biopsies contained bony spicules (right upper corner). Bony spicules may damage microtome blade, create uneven/“scratched” sections, and lift the coverslip creating pockets of air (right lower corner). However, fragments of squamous cell carcinomas can still be recognized (left half of the image), H&E, 200×. b Permanent H&E preparation of the frozen section remnant. Frozen section remnants can be processed without decalcification and serve as a control for intraoperative bone marrow evaluation, H&E, 200×. c Representative field of a final decalcified cross-sectional shave bone margin with squamous cell carcinoma, H&E, 100×
Technically adequate frozen sections were performed in all but one case—frozen section was impossible for one bony margin biopsy as it was entirely represented by the cortical bone.
One bone marrow biopsy was reported intraoperatively as “defer, atypical cells present”. In our practice, “deferred” interpretation of a margin usually prompts surgeons to obtain additional material. Accordingly, in this one case, an extended mandibulectomy was performed and for the purpose of this study, this report was counted as “positive”.
The study was approved by the Total Quality Council, University of Pittsburgh Medical Center.
Results
From February 2005 to December 2010, 94 patients with SCC invading mandibular bone were treated with segmental mandibulectomy. Of 67 segmental mandibulectomies without intraoperative bone margin assessment, seven showed SCC extending to the final bone margin.
Bone margins were assessed intraoperatively by routine frozen section analysis for the remaining 27 patients with 47 margins, including 35 BM and 12 IAN biopsies. Clinical features of these patients are summarized in Table 1. In 4 cases, segmental mandibulectomy was performed for recurrent disease.
Table 1.
Demographic and clinicopathologic features of studied patients
| Feature | |
|---|---|
| Male to female ratio | 17:10 |
| Average age, years | |
| Men | 55 |
| Females | 66 |
| Anatomic sites, n | |
| Floor of mouth, lateral | 11 |
| Floor of mouth, anterior | 7 |
| Alveolar ridge | 5 |
| Lip | 1 |
| Retromolar trigone | 3 |
| Lymph node involvement, N stage | |
| N0 | 10 |
| N1 | 5 |
| N2 | 12 |
| Average length of resected mandible, cm | 8.5 (ranging from 5.3 to 11) |
True Negative Intraoperative Reports
In 21 cases, all 40 bony margins (29 BM and 11 IAN) were free of carcinoma. There were no false positive reports.
False Negative Intraoperative Reports
There were three false negative intraoperative reports (Table 2). In the first case, the BM (frozen and permanent sections) and IAN biopsies were negative, but the final (decalcified, full-section) margin showed a <0.1 cm focus of SCC (Case 1). In the second case, a segment of IAN was assessed and the original frozen section showed no carcinoma (Case 2). However, permanent sections of the frozen section remnant revealed a 0.15 cm focus of SCC and the final decalcified full cross-section of the posterior bone margin also showed carcinoma. In the third case (Case 6), two BM biopsies (frozen and permanent sections of each) were negative. However, a 0.2 cm focus of carcinoma extended to the margin along the surface of the cortical bone on the final decalcified shave margin.
Table 2.
Summary of intraoperative findings for patients with positive final bone margin
| #. Age (years)/gender | Biopsy type | Intraoperative evaluation | Evaluation of permanent slides prepared from frozen section remnant | Decalcified shave bone margin, i.e. final margin | Additional procedures following intraoperative report? | Comment |
|---|---|---|---|---|---|---|
| 1. 52/M | 1 BM and 1 IAN | Both benign | Both benign | The margin represented by BM biopsy—malignant (<0.1 cm) | No | False negative1 |
| 2. 59/M | 1 IAN | Benign | Malignant (0.15 cm) | Malignant | No | False negative2 |
| 3. 59/F | 2 BM | Anterior—benign; Posterior—malignant (0.1 cm) | Similar to intraoperative evaluation | Similar to intraoperative evaluation | Completion hemi-mandibulectomy | True positive3 |
| 4. 75/F | 2 BM and 1 IAN | IAN and 1 BM—benign; 1 BM—deferred (atypical cells) | All benign | Deferred margin (atypical cells)—malignant (0.2 cm) | Yes, additional mandibular excision | True positive3 |
| 5. 88/M | 1 BM | Malignant (0.4 cm)4 | Malignant | Malignant | Yes, additional mandibular excision | True positive |
| 6. 82/F | 2 BM | Benign | Benign | One benign and one malignant (0.2 cm) | No | False negative1 |
1False negative, due to non-representative biopsy
2False negative. The biopsy was representative; however, apparently insufficient number of H&E levels was obtained at the time of intraoperative evaluation
3Additional mandibular bone segment showed carcinoma
4The only case where BM margin was sampled by the pathologist intraoperatively
M male, F female, BM bone marrow, IAN inferior alveolar nerve
True Positive Intraoperative Reports
Overall, of 6 full-section mandibular bone margins that were positive on final examination after decalcification, 3 were identified intraoperatively by frozen section of BM biopsies (true positive, Table 2, Cases 3–5).
Analysis of Inferior Alveolar Nerve Biopsies
Twelve biopsies of the IAN were sent for intraoperative evaluation. In 10 of 12 cases, large nerve was seen on the final decalcified section of the mandibular bone margin. In these 10 cases, both intraoperative evaluation and final decalcified full cross-section margins showed no carcinoma.
In one case, the posterior mandibular margin was represented intraoperatively by BM and IAN biopsies (Table 2, Case 4). The IAN biopsy and one of the two BM biopsies were negative. The other BM biopsy was deferred due to the presence of atypical cells. The final decalcified cross section of the posterior mandibular bone margin showed a 0.2 cm focus of SCC. Notably, this decalcified cross section of the posterior mandibular bone margin showed no IAN. Since the mandibulectomy resection line was superior to the mandibular foramen, this may be explained by sampling of a “mandibular”/extraosseous segment rather than the “inferior alveolar nerve”/intraosseous segment of the lower branch of the trigeminal nerve.
Discussion
Intraoperative evaluation of bone margins may contribute to the success of primary mandibular reconstruction. The feasibility of intraoperative analysis of bony margins was previously reported by three groups (Table 3). However, the present study offers the following additional information. First, the frequency of intraoperative bone margin assessment (29%, 27/94) was documented. Next, only cases with benign soft tissue margins were included in this study, to control for the possible effect of an adjacent positive soft tissue margin on the extent of mandibulectomy. Moreover, the design of the present study differs from that of previously published studies. For instance, we limited our study to SCCs while other groups included carcinomas metastatic to mandibular bone, sarcomas, and odontogenic neoplasms arising in mandibular bone. In addition, we included in our analysis segmental mandibulectomies only, while other groups included not only marginal mandibulectomies, but also bone biopsies. Finally, we analyzed routine practice by multiple surgeons and characterize IAN biopsies as a complementary method of mandibular bone margin assessment.
Table 3.
Oral squamous cell carcinoma and intraoperative evaluation of mandibular bone margins by routine frozen section, literature review
| Number of patients1, n | Sensitivity (%) | Specificity (%) | All soft tissue margins free of carcinoma? | Reference |
|---|---|---|---|---|
| 152 | NA | NA | NA | [7] |
| 153, 4 | 88.9 | 100 | NA | [9] |
| 255 | 88.9 | 100 | NA | [6] |
| NA4,5 | 805 | 955 | NA | [8] |
| 275 | 506 | 100 | Yes | Current study |
1Only patients with squamous cell carcinoma invading mandibular bone and treated with segmental mandibulectomy are included in this summary
2Frozen section analysis was able to correctly predict adequacy of resection in 32 (97%) of 33 margins. However, of 16 patients with proven mandibular invasion, one had metastatic breast carcinoma. Therefore, insufficient data are provided to calculate sensitivity of frozen section for SCC only
3Cortical bone, rather than bone marrow was analyzed. Type of mandibulectomy was not indicated. Exact number of SCC involving mandibular bone is not available
4Sensitivity and specificity are calculated for patients
5Sensitivity and specificity are calculated for bone margins
6Calculation of sensitivity is affected by the preferred way to categorize one intraoperative consultation that was “deferred” (“Materials and Methods”)
BM bone marrow, IAN intra-alveolar nerve, N.A. data not available
In agreement with previous studies by Forrest and Oxford [7, 9], there were no false positive reports. Accordingly, BM or IAN biopsies positive for carcinoma can be considered as representative of the entire mandibular bone margin and warrant further mandibular resection.
However, the sensitivity of BM and IAN biopsies in this study was 50%. Due to variations in study design (summarized above), it is difficult to compare our result to those from previous studies. Our results reflect an analysis of the routine practice of BM and IAN sampling by several surgeons without specialized instrumentation (i.e., no curved osteotomes or trephine drill). By design, we control for the potential bias introduced by positive soft tissue margins and limit our study to SCC with bone invasion only.
Of three false negative intraoperative reports, two resulted from BM biopsy and one from IAN biopsy. No previous work has methodically assessed the utility of evaluating IAN biopsies as an adjunct method for intraoperative analysis of bony margins. We showed that the mandibular bone margin status can also be assessed by the biopsy of the intraosseous segment of mandibular nerve, i.e. IAN proper. The only false negative report of IAN biopsy (Table 2, Case 2) is best explained by the limitations of frozen section due to sampling issues. Carcinoma was present in the frozen section remnant. However, 3 H&E levels examined intraoperatively showed no carcinoma. Based on 1 of 3 false negative cases, the sensitivity of frozen section analysis may be further increased by obtaining additional deeper (e.g 5–7) H&E levels.
A possible limitation of assuming that IAN biopsy is representative of the bone margin is related to the issue of terminology. The most inferior, third branch of the trigeminal nerve (cranial nerve V) is correctly referred to as the “mandibular nerve” (V3). Only after passing through the mandibular foramen should it be called the “inferior alveolar nerve”. On two occasions, mandibulectomy extended above the mandibular angle (and above the mandibular foramen) and no nerve was seen on the final decalcified section of the mandibular bone margin. However, in both cases, biopsied nerves were labeled as “inferior alveolar nerve”. As discussed, nerve biopsies are routinely submitted for frozen section analysis before the mandibulectomy specimen is available for review. Careful recognition of the precise anatomic site and use of proper terminology are critical to distinguish between extraosseous (non-IAN) and intraosseous (IAN proper) segments of the mandibular nerve and whether the specimen can be used as a true marker of the posterior mandibular bone margin. It is uncertain whether gross examination of the specimen by a pathologist or a standardized sampling technique would enhance the sensitivity of frozen section analysis of this margin.
In conclusion, given the technical feasibility of intraoperative BM and IAN assessment, we favor routine evaluation of BM and IAN as surrogate markers of mandibular bone margins. Additionally, however, considering the 50% sensitivity of intraoperative BM/IAN biopsies, examination of the entire cross-section of the bone margin should also be performed, as it remains the most accurate modality of bone margin assessment. In other words, even when BM or IAN biopsies are evaluated intraoperatively, final shave biopsies of the bony resection margins should still be sampled at the time of grossing.
References
- 1.Batsakis JG. Surgical excision margins: a pathologist’s perspective. Adv Anat Pathol. 1999;6:140–148. doi: 10.1097/00125480-199905000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Langdon JD, Harvey PW, Rapidis AD, et al. Oral cancer: the behaviour and response to treatment of 194 cases. J Maxillofac Surg. 1977;5:221–237. doi: 10.1016/S0301-0503(77)80115-X. [DOI] [PubMed] [Google Scholar]
- 3.Maciejewski A, Szymczyk C. Fibula free flap for mandible reconstruction: analysis of 30 consecutive cases and quality of life evaluation. J Reconstr Microsurg. 2007;23:1–10. doi: 10.1055/s-2006-958695. [DOI] [PubMed] [Google Scholar]
- 4.Holzle F, Kesting M, Holzle G, et al. Clinical outcome and patient satisfaction after mandibular reconstruction with free fibula flaps. Int J Oral Maxillofac Surg. 2007;36:802–806. doi: 10.1016/j.ijom.2007.04.013. [DOI] [PubMed] [Google Scholar]
- 5.Tsue T, McCulloch T, Girod D, et al. Predictors of carcinomatous invasion of the mandible. Head Neck. 1994;16:116–126. doi: 10.1002/hed.2880160204. [DOI] [PubMed] [Google Scholar]
- 6.Forrest LA, Schuller DE, Karanfilov B, et al. Update on intraoperative analysis of mandibular margins. Am J Otolaryngol. 1997;18:396–399. doi: 10.1016/S0196-0709(97)90060-0. [DOI] [PubMed] [Google Scholar]
- 7.Forrest LA, Schuller DE, Lucas JG, et al. Rapid analysis of mandibular margins. Laryngoscope. 1995;105:475–477. doi: 10.1288/00005537-199505000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Wysluch A, Stricker I, Holzle F, et al. Intraoperative evaluation of bony margins with frozen-section analysis and trephine drill extraction technique: a preliminary study. Head Neck. 2010;32:1473–1478. doi: 10.1002/hed.21350. [DOI] [PubMed] [Google Scholar]
- 9.Oxford LE, Ducic Y. Intraoperative evaluation of cortical bony margins with frozen-section analysis. Otolaryngol Head Neck Surg. 2006;134:138–141. doi: 10.1016/j.otohns.2005.09.007. [DOI] [PubMed] [Google Scholar]