Abstract
Background and Objectives
Statin therapy after percutaneous coronary intervention (PCI) has been associated with reduced major adverse cardiovascular events (MACE). However, it has been less clear as to whether statin therapy before acute coronary syndrome (ACS) is beneficial. We studied the effect of previous statin therapy, initiated ≥1 month before PCI, on the outcome of patients with ACS who had undergone early invasive strategies.
Subjects and Methods
We stratified 479 consecutive patients with ACS who had undergone PCI, according to preprocedural statin administration as follows: previous statin-treated patients (statin group, n=237) and statin-naive patients (control group, n=242). The incidence of periprocedural myocardial infarction (MI) and in-hospital MACE was assessed.
Results
The incidence of Braunwald class III angina and MI presentation were significantly lower in the statin group than in the control group. Angiographic and procedural characteristics were similar between the two groups; however, slow/no reflow phenomenon occurred more frequently in the control group. After PCI, the incidence of periprocedural MI was higher in the control group than in the statin group (6.6% vs. 2.1%, p=0.016). Multivariate analysis revealed that no prior use of statin {odds ratio (OR)=2.8; 95% confidence interval (CI)=1.1-7.2; p=0.038), procedural complication (OR=4.0; 95% CI=1.5-10.5; p=0.004), stent overlap (OR=4.7; 95% CI=1.3-16.4; p=0.015), and old age (OR=3.2; 95% CI=1.2-8.0; p=0.016) were independent predictors for in-hospital MACE.
Conclusion
Previous statin therapy before ACS was associated with milder clinical presentation and lower incidence of in-hospital MACE after early invasive strategies. The beneficial outcome is attributable to a significant reduction in periprocedural MI after PCI.
Keywords: Angioplasty, Myocardial infarction, Stents, Hydroxymethylglutaryl-coenzyme A reductase inhibitors, Treatment outcome
Introduction
Statins have been known to significantly reduce cardiovascular clinical events in a variety of patients, ranging from those with established cardiovascular disease to those who are at risk for cardiovascular disease.1-6) The role of statins in patients with acute coronary syndrome (ACS) also has been clarified. Large scaled randomized trials have shown that early and high doses of statin therapy significantly improve the prognosis in patients with ACS.7),8)
Since an early invasive strategy has been the standard therapy for ACS, several studies have been conducted to determine whether periprocedural use of statins is beneficial in these cases. Some reports have suggested that statin loading prior to percutaneous coronary intervention (PCI) is associated with reduced mortality and decreased periprocedural myocardial injury after PCI in patients with ACS.9),10) Another study demonstrated that pretreatment with statin for three to seven days in patients with ACS was associated with a reduction of myocardial necrosis and late cardiac events after PCI.11),12) However, it has been less clear as to whether statin therapy before a coronary event is beneficial.
Therefore, we designed a retrospective study involving consecutive ACS patients who underwent PCI. We compared the hospital course and mortality between those patients who had undergone previous statin treatment for more than one month, which was set to avoid statin therapy after the occurrence of ACS and to enroll patients showing the lipid lowering effect of statin, as well as patients without statin pretreatment.
Subjects and Methods
Study population
We analyzed a single center ACS and PCI cohort from December 2008 to December 2009. During the study period, 479 consecutive patients were recruited and followed-up during their clinical course to document patient characteristics, acute therapy, PCI data, and hospital outcome. According to the patient's past medication history, we divided the patients into two groups, and compared their hospital course. Two hundred thirty-seven patients had previously undergone statin treatment for more than one month prior to PCI (statin group) and 242 patients were statin-naive patients (control group). All patients gave informed consent for processing their anonymous data according to a protocol approved by the Institutional Review Board of Wonkwang University Hospital.
Percutaneous coronary intervention
PCI was performed according to the current clinical practice at the physician's discretion and within 48 hours after admission. In all patients, aspirin (300 mg/day) and clopidogrel (300 mg/day) were loaded before the procedure. An intravenous bolus of 5,000 U of unfractionated heparin was given, and then additional heparin was given to maintain an activated clotting time greater than 300 s during the procedure. Platelet glycoprotein IIb/IIIa inhibitors (GPI) were administered according to operator preference.
Post-procedural management
Aspirin (100 mg/day), clopidogrel (75 mg/day) and statins were prescribed to all patients following the procedure. Creatine kinase MB fraction (CK-MB) and troponin T were measured before (at admission, mean 18±4 hours before PCI), and at 8, 16, and 24 hours after PCI. High-sensitivity C-reactive protein (hsCRP) and fibrinogen were also assessed before PCI and at 24 hours after PCI.
Definitions
Periprocedural myocardial infarction (MI) was defined as a postprocedural increase of CK-MB more than three times higher than the normal upper limit in patients with a normal baseline level of enzyme. In patients with elevated baseline levels of CK-MB, MI was defined as a subsequent increase of more than 3-fold in CK-MB from baseline values.13) Non-periprocedural MI was defined as spontaneous MI occurring for more than 24 hours after PCI. Further, MACE included a composite of death, periprocedural, and non-periprocedural non-fatal MI, ischemic stroke, and target vessel revascularization.
Statistical analysis
All measurements were represented as means±standard deviation or absolute numbers (percentage). The inter-group analysis was done by independent t-test and χ2 test, using Statistical Package for the Social Sciences (SPSS) 12.0 for Windows (SPSS Inc., Chicago, IL, USA). To compare changes in cardiac and inflammatory biomarkers before and after PCI, we used a paired t-test. A multivariable logistic regression model was constructed to predict in-hospital MACE. The following variables, selected according to significance in a univariate analysis, were inserted into the logistic regression analysis: no prior use of statin, procedural complication, age more than 65 years, thrombus lesion, stent overlap, MI presentation on admission, and use of glycoprotein IIb/IIIa receptor antagonist. Statistical significance was set at p<0.05.
Results
Baseline characteristics
The baseline clinical characteristics of patients in the control and statin groups have been provided in Table 1. In the statin group, 63.5% of patients received atorvastatin, 12.9% rosuvastatin, 11.4% ezetimibe/simvastatin, 5.2% simvastatin, 3.0% pravastatin, 2.5% pitavastatin, and 1.5% fluvastatin. The duration of statin therapy was as follows; 22.1% of the patients, more than 1 year; 53.5%, 6 months to 1 year; and 24.4%, 1 to 6 months. Further, the statin group had lower baseline low density lipoprotein (LDL) cholesterol levels (124±40 mg/dL vs. 113±42 mg/dL, p=0.002) and incidences of Braunwald class III angina and MI presentation were also significantly lower in the statin group than in the control group.
Table 1.
Baseline clinical characteristics
PCI: percutaneous coronary intervention, NSTEMI: non-ST-segment elevation myocardial infarction, HDL-C: high density lipoprotein-cholesterol, LDL-C: low density lipoprotein-cholesterol
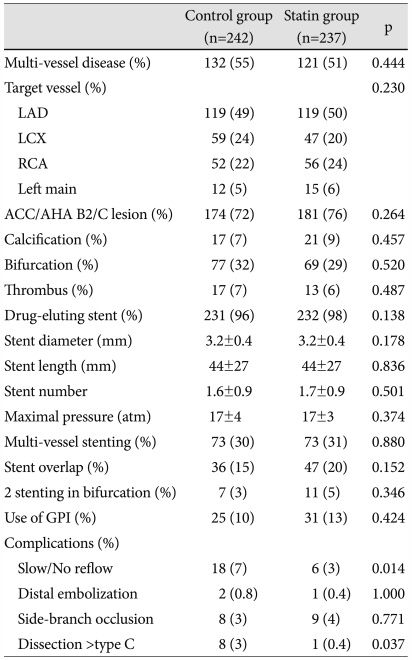
Coronary angiography and revascularization
Most patients (97%) received drug-eluting stents, and over 30% of the patients received multi-vessel stenting (Table 2). Angiographic and procedural characteristics were similar between the two groups; however, slow/no reflow phenomenon was more frequent in the control group (7% vs. 3%, p=0.014).
Table 2.
Coronary angiographic and procedural characteristics
LAD: left anterior descending artery, LCX: left circumflex artery, RCA: right coronary artery, ACC/AHA: American College of Cardiology/American Heart Association lesion classification, GPI: glycoprotein IIb/IIIa inhibitor
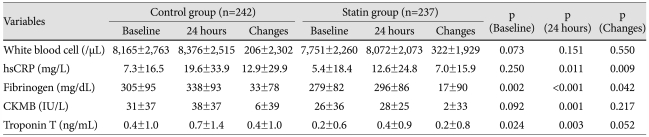
Changes of cardiac biomarker and inflammatory marker
The statin group revealed lower baseline serum troponin T and fibrinogen levels (Table 3) and less elevation of both markers after PCI. Mean baseline hsCRP levels were similar between the two groups; however, after PCI, the peak value of hsCRP were elevated significantly higher in the control group. That is, hsCRP increased from 7.3±16.5 to 19.6±33.9 mg/L in the control group, and from 5.4±18.4 to 12.6±24.8 mg/L in the statin group (p=0.009).
Table 3.
Changes of inflammatory and myocardial biomarker after percutaneous coronary intervention
hsCRP: high sensitivity C-reactive protein, CK-MB: creatine kinase MB
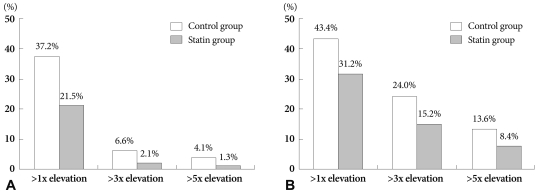
Periprocedural myocardial injury
Myocardial infarction, defined as a postprocedural elevation of CK-MB >3 times the upper normal limit or baseline level, was detected in 16 (6.6%) of patients in the control group and in 5 (2.1%) patients in the statin group (p=0.016). Moreover, the incidences of a >5 fold elevation in postprocedural CK-MB levels (4.1% vs. 1.3%, p=0.048), and a >1 fold elevation (37.2% vs. 21.5%, p<0.001), was higher in the control group than in the statin group (Fig. 1).
Fig. 1.
Incidence of cardiac biomarker elevation after percutaneous coronary intervention. A: incidences of any CK-MB elevation (37.2% vs. 21.5%, p<0.001), >3 times elevation (6.6% vs. 2.1%, p=0.016), and >5 times elevation (4.1% vs. 1.3%, p=0.054) were higher in the control group than in the statin group. B: incidences of any troponin elevation (43.4% vs. 31.2%, p=0.006), >3 times elevation (24.0% vs. 15.2%, p=0.016), and >5 times elevation (13.6% vs. 8.4%, p=0.070) were higher in the control group than in the statin group.
Troponin T elevation after PCI was also higher in the control group than in the statin group. The instances of overall elevation in troponin T levels (43.4% vs. 31.2%, p=0.006), >3 times elevation in troponin T levels (24.0% vs. 15.2%, p=0.016), and >5 times elevation in troponin T levels (13.6% vs. 8.4%, p=0.070) after PCI occurred more frequently in the control group than in the statin group.
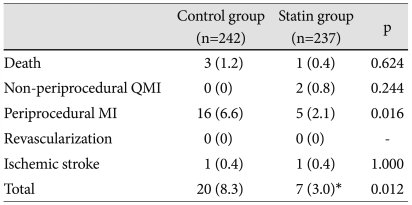
In-hospital major adverse cardiovascular events
The patients in the statin group had a lower incidence of in-hospital MACE compared to the patients in the control group (8.3% vs. 3.0%, p=0.012). The different outcomes mainly resulted from a higher incidence of periprocedural MI in the control group (Table 4).
Table 4.
In-hospital major adverse cardiovascular events in control and statin-treated groups
*Two patients with periprocedural myocardial infarction experienced re-infarction on a subsequent hospital day. QMI: Q wave myocardial infarction, MI: myocardial infarction
A multivariate analysis revealed that no prior use of statin {odds ratio (OR)=2.8; 95% confidence interval (CI)=1.1-7.2; p=0.038), procedural complication (OR=4.0; 95% CI=1.5-10.5; p=0.004), stent overlap (OR=4.7; 95% CI=1.3-16.4; p=0.015), and old age (OR=3.2; 95% CI=1.2-8.0; p=0.016) were independent predictors for in-hospital MACE (Table 5).
Table 5.
Multivariate analysis for the prediction of in-hospital major adverse cardiovascular events
OR: odds ratio, CI: confidence interval, NSTEMI: non-ST-segment elevation myocardial infarction, GPI: glycoprotein IIb/IIIa inhibitor
Discussion
In this study, we showed that previous statin therapy before ACS was associated with milder clinical presentation and lower incidence of MACE after an early invasive strategy. The beneficial outcomes observed in the statin group can be attributed to a reduction in the inflammatory response and periprocedural MI after PCI.
Statin therapy before PCI has been shown to reduce the incidence of periprocedural MI and improve outcomes in patients with stable angina. Briguori et al.14) reported that the incidence of CK-MB elevation greater than five times the upper normal limit after PCI was approximately 50% lower in statin-treated angina patients as compared to the statin-naïve patients. In addition, the CK-MB peak after stenting was shown to be significantly lower in the statin group than in the control group. Another study demonstrated that chronic statin therapy before PCI reduced CK-MB by greater than three times the elevation after PCI and decreased the incidence of 6-12 months MACE.12),15) Further, a meta-analysis showed that statin pretreatment in patients with stable angina resulted in a 59.3% reduction of relative risk of procedural MI and a 20.5% overall reduction in MACE.16) However, there was a limitation on data regarding the clinical benefits of chronic pretreatment with statins in patients with ACS undergoing PCI.
Previous studies have also shown that statin therapy improves the prognosis of patients with ACS. The Pravastatin or Atorvastatin Evaluation and Infection Therapy study reported that intensive statin therapy within 10 days after ACS results in 28% and 6% risk reduction at 30 days and two years, respectively.8) Further, the Myocardial Ischemia Reduction with Aggressive Cholesterol Lowering study reported that 80 mg atorvastatin within 24-96 hours after hospital admission reduced the risk of the composite primary end point of death, MI, cardiac arrest, and recurrent ischemia by 16% compared to placebo.7) In addition, we previously reported that high dose statin loading approximately 16 hours before PCI resulted in a 53% reduction in the risk of periprocedural MI and a 63% reduction in the risk of 30-day MACE, compared to no statin pretreatment.10) These studies indicate that early statin therapy significantly improves the prognosis of patients with ACS. In the current study, we demonstrated that previous statin therapy prior to the onset of ACS also has beneficial effects on the reduction of periprocedural MI and improvement of the in-hospital clinical course after PCI.
Previous statin therapy seems to attenuate the severity and extent of MI. In an analysis of the Global Registry of Acute Coronary Events registry, patients receiving statins had a lower incidence of MI and cardiogenic shock. Size of infarcted myocardium was significantly smaller because ST-segment elevation MI occurred less often, and CK levels were lower among patients with chronic statin therapy.17) Previous statin therapy also has been demonstrated to favorably affect the hospital outcome in patients with MI. Bauer et al.18) reported that pretreatment with statins was associated with smaller MI size and a 35% reduction of hospital mortality in patients with non-ST-segment elevation MI. The results of the current study were similar to those of the aforementioned studies, despite differences in the study population. Overall, patients with previous statin therapy revealed lower levels of baseline and peak troponin and a lower incidence of in-hospital MACE.
The benefits of statins in cardiovascular diseases can be explained not only by their lipid-lowering potential but also by mechanisms unrelated to lipids, or the so called pleiotropic effects.19) Such pleiotropic effects encompass non-lipid mechanisms that modify endothelial function, inflammatory responses, plaque stability, and thrombus formation.20) Thus, they may potentially improve outcomes after PCI. Our study showed a lower elevation of hsCRP levels after PCI in patients undergoing previous statin therapy. Previous studies have shown that elevation of hsCRP levels after PCI to be associated with troponin elevation, and periprocedural myocardial injury has been shown to be correlated with vascular inflammation.21),22) Moreover, the CRP elevation after PCI has been associated with a higher incidence of MACE in patients with ACS.23) In the current study, the hsCRP peak after stenting was significantly lower in the statin group than in the control group, supporting the notion that prevention of myocardial injury via lipid lowering and pleiotrophic effects of statins is important in improving the clinical outcomes in patients with ACS.
Our study has several limitations. The study was not randomized, and the sample size was small. It was difficult to randomize because the study group was classified by long-term treatment status. Furthermore, the clinical outcomes according to the type and dose of statins and the exact duration of the therapy were not identified due to the small sample size. A large registry study is needed to generalize our results.
In conclusion, previous statin therapy before PCI attenuated the clinical presentation of ACS and was associated with a lower incidence of MACE after an early invasive strategy. Inflammatory responses after PCI were also inhibited by a reduction of myocardial injury during the intervention in patients who had previously received statin therapy.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Sacandinavian Simvastatin Survival Study (4S) Randomized trial of cholesterol lowering in 4444 patients with coronary heart disease. Lancet. 1994;344:1383–1389. [PubMed] [Google Scholar]
- 2.Shepherd J, Cobbe SM, Ford I, et al. West of Scotland Coronary Prevention Study Group. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. N Engl J Med. 1995;333:1301–1307. doi: 10.1056/NEJM199511163332001. [DOI] [PubMed] [Google Scholar]
- 3.Sacks FM, Pfeffer MA, Moye LA, et al. Cholesterol and Recurrent Events Trial investigators. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. N Engl J Med. 1996;335:1001–1009. doi: 10.1056/NEJM199610033351401. [DOI] [PubMed] [Google Scholar]
- 4.Long-Term Intervention with Pravastatin in Ischemic Disease (LIPID) Study Group. Prevention of cardiovascular events and death with pravastatin in patients of coronary heart disease and a board range of initial cholesterol levels. N Engl J Med. 1998;339:1349–1357. doi: 10.1056/NEJM199811053391902. [DOI] [PubMed] [Google Scholar]
- 5.Hong YJ, Jeong MH, Lim JH, et al. The prognostic significance of statin therapy according to the level of C-reactive protein in acute myocardial infarction patients who underwent percutaneous coronary intervention. Korean Circ J. 2003;33:891–900. [Google Scholar]
- 6.Ridker PM, Danielson E, Fonseca FA, et al. Reduction in C-reactive protein and LDL cholesterol and cardiovascular event rates after initiation of rosuvastatin: a prospective study of the JUPITER trial. Lancet. 2009;373:1175–1182. doi: 10.1016/S0140-6736(09)60447-5. [DOI] [PubMed] [Google Scholar]
- 7.Schwartz GG, Olsson AG, Ezekowitz MD, et al. Effects of atorvastatin on early recurrent ischemic events in acute coronary syndromes: the MIRACL study: a randomized controlled trial. JAMA. 2001;285:1711–1718. doi: 10.1001/jama.285.13.1711. [DOI] [PubMed] [Google Scholar]
- 8.Ray KK, Cannon CP, McCabe CH, et al. Early and late benefits of high-dose atorvastatin in patients with acute coronary syndromes: results from the PROVE IT-TIMI 22 trial. J Am Coll Cardiol. 2005;46:1405–1410. doi: 10.1016/j.jacc.2005.03.077. [DOI] [PubMed] [Google Scholar]
- 9.Patti G, Pasceri V, Colonna G, et al. Atorvastatin pretreatment improves outcomes in patients with acute coronary syndromes undergoing early percutaneous coronary intervention: results of the ARMYDA-ACS randomized trial. J Am Coll Cardiol. 2007;49:1272–1278. doi: 10.1016/j.jacc.2007.02.025. [DOI] [PubMed] [Google Scholar]
- 10.Yun KH, Jeong MH, Oh SK, et al. The beneficial effect of high loading dose of rosuvastatin before percutaneous coronary intervention in patients with acute coronary syndrome. Int J Cardiol. 2009;137:246–251. doi: 10.1016/j.ijcard.2008.06.055. [DOI] [PubMed] [Google Scholar]
- 11.Ishii H, Ichimiya S, Kanashiro M, et al. Effects of receipt of chronic statin therapy before the onset of acute myocardial infarction: a retrospective study in patients undergoing primary percutaneous coronary intervention. Clin Ther. 2006;28:1812–1819. doi: 10.1016/j.clinthera.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 12.Chang SM, Yazbek N, Lakkis NM. Use of statins prior to percutaneous coronary intervention reduces myonecrosis and improves clinical outcome. Catheter Cardiovasc Interv. 2004;62:193–197. doi: 10.1002/ccd.20078. [DOI] [PubMed] [Google Scholar]
- 13.Di Sciascio G, Patti G, Pasceri V, Gaspardone A, Colonna G, Montinaro A. Efficacy of atorvastatin reload in patients on chronic statin therapy undergoing percutaneous coronary intervention: results of the ARMYDA-RECAPTURE (Atorvastatin for Reduction of Myocardial Damage During Angioplasty) Randomized Trial. J Am Coll Cardiol. 2009;54:558–565. doi: 10.1016/j.jacc.2009.05.028. [DOI] [PubMed] [Google Scholar]
- 14.Briguori C, Colombo A, Airoldi F, et al. Statin administration before percutaneous coronary intervention: impact on periprocedural myocardial infarction. Eur Heart J. 2004;25:1822–1828. doi: 10.1016/j.ehj.2004.07.017. [DOI] [PubMed] [Google Scholar]
- 15.Chan AW, Bhatt DL, Chew DP, et al. Relation of inflammation and benefit of statins after percutaneous coronary interventions. Circulation. 2003;107:1750–1756. doi: 10.1161/01.CIR.0000060541.18923.E9. [DOI] [PubMed] [Google Scholar]
- 16.Ebrahimi R, Saleh J, Toggart E, et al. Effect of preprocedural statin use on procedural myocardial infarction and major cardiac adverse events in percutaneous coronary intervention: a meta-analysis. J Invasive Cardiol. 2008;20:292–295. [PubMed] [Google Scholar]
- 17.Spencer FA, Allegrone J, Goldberg RJ, et al. Association of statin therapy with outcomes of acute coronary syndromes: the GRACE study. Ann Intern Med. 2004;140:857–866. doi: 10.7326/0003-4819-140-11-200406010-00006. [DOI] [PubMed] [Google Scholar]
- 18.Bauer T, Bohm M, Zahn R, et al. Effect of chronic statin pretreatment on hospital outcome in patients with acute non-ST-elevation myocardial infarction. J Cardiovasc Pharmacol. 2009;53:132–136. doi: 10.1097/FJC.0b013e3181976a3c. [DOI] [PubMed] [Google Scholar]
- 19.Takemoto M, Liao JK. Pleiotropic effects of 3-hydroxy-3-methylglutaryl coenzyme a reductase inhibitors. Arterioscler Thromb Vasc Biol. 2001;21:1712–1719. doi: 10.1161/hq1101.098486. [DOI] [PubMed] [Google Scholar]
- 20.Sposito AC, Chapman MJ. Statin therapy in acute coronary syndromes: mechanistic insight into clinical benefit. Arterioscler Thromb Vasc Biol. 2002;22:1524–1534. doi: 10.1161/01.atv.0000032033.39301.6a. [DOI] [PubMed] [Google Scholar]
- 21.Rhee SJ, Yun KH, Oh SK, et al. Changes of C-reactive protein are associated with myocardial injury after successful percutaneous coronary intervention. Korean Circ J. 2008;38:135–139. [Google Scholar]
- 22.Choi SY, Yang HM, Tahk SJ, et al. Preprocedural hs-CRP level serves as a marker for procedure-related myocardial injury during coronary stenting. Korean Circ J. 2005;35:140–148. [Google Scholar]
- 23.Yun KH, Jeong MH, Oh SK, et al. Response of high-sensitivity C-reactive protein to percutaneous coronary intervention in patients with acute coronary syndrome. Heart Vessels. 2009;24:175–180. doi: 10.1007/s00380-008-1110-5. [DOI] [PubMed] [Google Scholar]