Abstract
Objectives
Falls are a major problem in the elderly. Age-related degeneration of the human balance system increases the risk of falls. Kyphosis is a common condition of curvature of the upper spine in the elderly and its development occurs through degenerative change. However, relatively little is known about the effect of kyphotic changes on balance in the elderly. The aim of this study is to investigate the influence of kyphosis on the balance strategy through use of the motor control test (MCT) in computerized dynamic posturography.
Methods
Fifty healthy subjects who were not affected by other medical disorders that could affect gait or balance were enrolled in the study. By simulation of kyphotic condition through change of the angles of the line connecting the shoulder to the hip and the ankle axis by approximately 30°, the latency and amplitude of the MCT were measured in upright and kyphotic condition.
Results
In the kyphotic condition, latency was shortened in backward movement. In forward movement, latency was shortened only in large stimulation. The amplitude in forward movement was decreased in kyphotic condition. However, the change of amplitude was not significant in large intensity backward movement in the same condition.
Conclusion
Kyphotic condition decreases the latency of MCT, especially in backward movement. These findings imply that kyphotic condition may serve as a protective factor against falls.
Keywords: Kyphosis, Accidental falls, Dynamic posturography
INTRODUCTION
As the elderly population is increasing worldwide, concern over health problems of the elderly is growing, and has resulted in increased medical and social costs more by token. Kyphotic condition is known as the sagittal convexity of the normal thoracic spine with aging (1). The prevalence of kyphotic condition in the elderly population is considered to be between 20% and 40% (2).
Falls due to the decline of posture and balance control in the elderly are associated with fatal complications, including hip fracture, cervical fracture, and even death (3, 4). The frequency of falls among the elderly is significantly high; 30% of women and 20% of men older than 50 years suffer from falls each year (5). Prediction of those with high risk factors for falls through appropriate tests and preventive measures in the elderly population is important.
Computerized dynamic posturography (CDP) is a useful test for evaluation of the comprehensive balance ability and risk of falls (6-10). CDP consists of two tests for balance function, which are motor control test (MCT) and sensory organizing test. MCT is used for evaluation of cooperative motion between body and low extremity through automatic postural response evoked by sudden support surface movement when in standing stance.
Some studies have suggested that kyphotic condition alters balance and increases falls. However, the influence of the kyphotic condition on balance is controversial (2, 5, 11). The aim of this study is to investigate the influence of kyphotic condition on the balance strategy through MCT, which has not been used before, and to estimate the risk of falls in kyphotic patients.
MATERIALS AND METHODS
Subject recruitment and selection
From January 2009 to March 2009, fifty subjects were recruited from community groups and volunteers at this medical center. Excluded were subjects who had a history of dizziness, orthopedic problems, trauma, visual impairment, sensory or motor function impairment of the low extremity, neurological, cognitive or proprioceptive disorder, or any other medical problems that could affect gait or balance. The mean age of the subjects was 27.5 years with a range from 23 to 33 years. The average height was 170.7, with a range from 160 to 182 cm. This study was approved by the Institutional Review Board at the Korea University Medical Center (IRB number: GR09186-001).
Motor control test
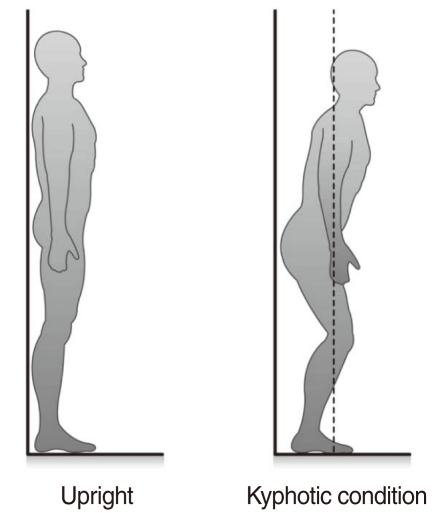
MCT was conducted using EQUITEST®(NeuroCom International Inc., Portland, OR, USA) in accordance with the NeuroCom® instruction manual. Subjects underwent MCT simulation in upright condition and kyphotic condition, which involved change of the angles between the lines connecting the shoulder to the hip and the hip to the ankle by approximately 30°, keeping their condition to the marked point of the machine and being checked for the right condition by the goniometer in clothes and the observer (1st author) (Fig. 1).
Fig. 1.
Upright and kyphotic conditions in motor control test. Kyphotic condition was simulated by changing the angles between the lines connecting the shoulder to the hip and the hip to the ankle by approximately 30°. Amplitude and latency were evaluated during upright standing and kyphotic condition. Center of gravity (dotted line) was not changed according to degree of kyphotic condition.
Two parameters, the latency and amplitude of the MCT, were acquired in two different conditions (upright, kyphotic condition) when the footplate swayed forward and backward. Latency and amplitude were defined as the time in milliseconds and angular momentum between the onset of footplate movement and initiation of the reactive response at the intensities of large (8.0 degree/second) and medium (6.0 degree/second) movement, respectively. The average and standard deviation of these tests were compared with the kyphotic condition and upright condition, considering forward and backward movement separately. During the test, center of gravity (COG) was not changed by angle of kyphotic condition.
Data analysis
All data are expressed as mean±SD. The Student's t-test was conducted for cross-correlation with the change of latency and amplitude by two different postures, intensity of response, and conditions between each group using SPSS ver. 9.0 (SPSS Inc., Chicago, IL, USA). A P-value of 0.05 was set as the significance level throughout this study. All values are represented as mean±SD.
RESULTS
Change of latencies in the MCT according to the kyphotic condition and upright condition
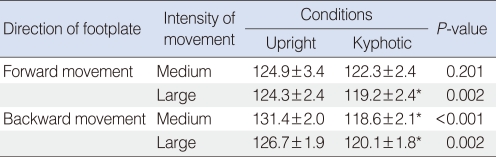
In the kyphotic condition, participants had significantly faster reactive responses to movement of the footplate than in upright condition. The duration of latency was shorter in backward movement than in forward movement of the footplate (Table 1).
Table 1.
Latency changes of the motor control test in upright and kyphotic condition
Values are presented as means±SD (millisecond).
Medium: 6.0 degree/second; Large: 8.0 degree/second.
*P-value<0.05.
In forward movement, latency decreased only at large intensity. Reduction of latency was 4.0% in kyphotic condition, compared with latency in upright condition (P=0.002). In backward movement, latency showed a decrease in all degrees of stimulation. In backward movement with medium intensity, reduction of latency was 9.9% in kyphotic condition, compared with latency in upright condition (P<0.001). And, with large intensity, reduction of latency was 4.8% in kyphotic condition, compared with latency in upright condition (P=0.002).
Change of amplitude in the MCT according to the kyphotic condition and upright condition
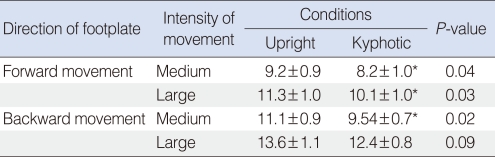
In the kyphotic condition, participants showed a significantly smaller degree of amplitude than in upright (Table 2).
Table 2.
Amplitude changes of the motor control test in upright and kyphotic condition
Values are presented as mean±SD (degree/second).
Medium: 6.0 degree/second; Large: 8.0 degree/second.
*P-value<0.05.
In forward movement, reduction of amplitude was 10.9% in medium and 10.7% in large intensity in kyphotic condition, compared with the amplitude in upright (P=0.04, P=0.03). In backward movement, reduction of amplitude was 14.1% in medium and 8.9% in large intensities in kyphotic condition, compared with the amplitude in upright. However, it showed statistical significance only in medium degree of stimulation (P=0.02).
In forward and backward movement, as intensity of stimulation was increased, amplitudes increased. No differences in changes of amplitude were observed according to sex, weight, and height.
DISCUSSION
Postural correction after sudden movement is important for maintenance of dynamic stability of the human system and for avoidance of falls. The ability to avoid a fall involves three processes: 1) detection of a stimulus from the environment, 2) processing of the information contained in the stimulus, and 3) correct execution of the appropriate reactive response within a critical time frame (12).
Body organs related to balance, vestibular system, visual system, and somatosensory system show degeneration with the aging process. Age-related degeneration of the human balance system usually reduces the ability of the elderly to respond in time to sudden stimuli.
MCT is used for measurement of the ability of balance control in patients with vestibular or neurologic deficit. Two important parameters, amplitude and latency, were evaluated on MCT. Amplitude is the degree of movement of the center of gravity. Latency is defined as the duration between the onset of movement and initiation of reactive response. As the footplate moves forward or backward, the COG moves in the opposite direction of the movement of the footplate; rapid movement in time is then needed for reconditioning of the center of gravity for maintenance of balance (5, 12-14). The delay of latency on MCT indicates prolongation of automatic postural response, resulting in a fall.
The influence of kyphosis, common in elderly, on balance has not yet been determined. Some reports have shown that kyphosis increases the incidence of the self reported injurious fall (11). Other studies have found no association of kyphosis with impaired balance (15).
In our study, we found that latency, the most important factor in maintenance of balance control, is significantly decreased in the kyphotic condition, when compared with normal posture, especially in backward movement. These results indicate that the kyphotic condition can cause a faster response to sudden movement, especially for compensation of late response to stimulation in the elderly. Reduction of latency in kyphotic condition might originate from the lowered center of gravity, which can respond rapidly to change in surface movement. There were no significant changes in latency between 45° kyphotic condition and 30° kyphotic condition (data not shown). It is thought that severe kyphotic change of 45° inevitably requires excessive muscle tone in order to maintain posture, compared with the 30° kyphotic condition. This excessive muscle tone in severe kyphotic condition could interfere with the prompt response to surface movement, compared with mild kyphotic condition (30°). Latency was more significantly reduced in backward movement than in forward movement of the footplate in kyphotic condition, compared with upright condition. These results suggest that a mild degree (30°) of kyphosis can serve more effectively as a protective factor against falls in the elderly in forward body movement than in backward body movement.
An earlier study showed that loss of balance in the posterior sway is more common in the elderly than in younger members of the population (16). Younger people were found to use the toe's muscle activity for maintenance of balance. However the elderly were not able to sufficiently utilize the toe's muscle activity and only used the heel area in the posterior sway. Therefore, automatic postural response latency was reduced in the elderly for the compensation of limited utilization of the forefoot. Results of this study show that there was a significant latency reduction in backward movement. The elderly are more prone to falls in backward movement; therefore, preventive training concentrated on backward movement, rather than forward movement, is needed.
The amplitude of perturbation was reduced in the kyphotic condition. In small intensity, both upright and kyphotic condition could move within the cone of stability. As a large intensity of stimulation over the cone of stability was applied to both conditions, the amplitude difference between two conditions was increased. In that case, the risk of fall is increased in the kyphosis group, especially in backward movement.
To determine the difference between the kyphotic and upright condition effect on MCT, this study was conducted by normal healthy adults simulating the kyphotic condition for control of these confounding factors that could affect individual variation of posture changes.
Our study has some limitations, including relatively small study numbers, and the possibility of change of kyphotic angle. Moreover, from time to time, kyphotic patients may not show consistent results in MCT due to other balance related problems. However, the result of our study is still important because it reveals the influence of kyphotic condition on the balance strategy.
In conclusion, latency of reactive response is important to maintenance of the balance of the body. In the kyphotic condition, the latency of reactive response showed a decrease, especially in backward movement. The amplitude on MCT also showed a decrease in forward and backward movement. These findings suggest that 30° degree of kyphotic condition can lower the risk of falls, especially in backward movement.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Milne JS, Lauder IJ. Age effects in kyphosis and lordosis in adults. Ann Hum Biol. 1974 Jul;1(3):327–337. doi: 10.1080/03014467400000351. [DOI] [PubMed] [Google Scholar]
- 2.Kado DM, Prenovost K, Crandall C. Narrative review: hyperkyphosis in older persons. Ann Intern Med. 2007 Sep 04;147(5):330–338. doi: 10.7326/0003-4819-147-5-200709040-00008. [DOI] [PubMed] [Google Scholar]
- 3.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988 Dec 29;319(26):1701–1707. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- 4.Overstall PW, Exton-Smith AN, Imms FJ, Johnson AL. Falls in the elderly related to postural imbalance. Br Med J. 1977 Jan 29;1(6056):261–264. doi: 10.1136/bmj.1.6056.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hindmarsh JJ, Estes EH., Jr Falls in older persons: causes and interventions. Arch Intern Med. 1989 Oct;149(10):2217–2222. [PubMed] [Google Scholar]
- 6.Lynn SG, Sinaki M, Westerlind KC. Balance characteristics of persons with osteoporosis. Arch Phys Med Rehabil. 1997 Mar;78(3):273–277. doi: 10.1016/s0003-9993(97)90033-2. [DOI] [PubMed] [Google Scholar]
- 7.Fernie GR, Gryfe CI, Holliday PJ, Llewellyn A. The relationship of postural sway in standing to the incidence of falls in geriatric subjects. Age Ageing. 1982 Feb;11(1):11–16. doi: 10.1093/ageing/11.1.11. [DOI] [PubMed] [Google Scholar]
- 8.Maki BE, Holliday PJ, Topper AK. A prospective study of postural balance and risk of falling in an ambulatory and independent elderly population. J Gerontol. 1994 Mar;49(2):M72–M84. doi: 10.1093/geronj/49.2.m72. [DOI] [PubMed] [Google Scholar]
- 9.Lord SR, Ward JA, Williams P, Anstey KJ. Physiological factors associated with falls in older community-dwelling women. J Am Geriatr Soc. 1994 Oct;42(10):1110–1117. doi: 10.1111/j.1532-5415.1994.tb06218.x. [DOI] [PubMed] [Google Scholar]
- 10.Whitney SL, Marchetti GF, Schade AI. The relationship between falls history and computerized dynamic posturography in persons with balance and vestibular disorders. Arch Phys Med Rehabil. 2006 Mar;87(3):402–407. doi: 10.1016/j.apmr.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 11.Kado DM, Huang MH, Nguyen CB, Barrett-Connor E, Greendale GA. Hyperkyphotic posture and risk of injurious falls in older persons: the Rancho Bernardo Study. J Gerontol A Biol Sci Med Sci. 2007 Jun;62(6):652–657. doi: 10.1093/gerona/62.6.652. [DOI] [PubMed] [Google Scholar]
- 12.Voorhees RL. The role of dynamic posturography in neurotologic diagnosis. Laryngoscope. 1989 Oct;99(10 Pt 1):995–1001. doi: 10.1288/00005537-198210000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Voorhees RL. Dynamic posturography findings in central nervous system disorders. Otolaryngol Head Neck Surg. 1990 Jul;103(1):96–101. doi: 10.1177/019459989010300114. [DOI] [PubMed] [Google Scholar]
- 14.Shepard NT, Schultz A, Alexander NB, Gu MJ, Boismier T. Postural control in young and elderly adults when stance is challenged: clinical versus laboratory measurements. Ann Otol Rhinol Laryngol. 1993 Jul;102(7):508–517. doi: 10.1177/000348949310200704. [DOI] [PubMed] [Google Scholar]
- 15.Greig AM, Bennell KL, Briggs AM, Wark JD, Hodges PW. Balance impairment is related to vertebral fracture rather than thoracic kyphosis in individuals with osteoporosis. Osteoporos Int. 2007 Apr;18(4):543–551. doi: 10.1007/s00198-006-0277-9. [DOI] [PubMed] [Google Scholar]
- 16.Tanaka T, Takeda H, Izumi T, Ino S, Ifukube T. Effects on the location of the centre of gravity and the foot pressure contribution to standing balance associated with ageing. Ergonomics. 1999 Jul;42(7):997–1010. doi: 10.1080/001401399185261. [DOI] [PubMed] [Google Scholar]