Abstract
Objective To examine the association of critical parenting behaviors with preadolescent reported depressive symptoms, self-efficacy, and self-care behaviors in youth with type 1 diabetes (T1D). Method A total of 84 youth with T1D, ages 9–11 years, completed the Diabetes Family Behavior Checklist, Child Depression Inventory, Self-Efficacy for Diabetes scale, and Self-Care Inventory during a baseline assessment for a randomized controlled trial of an intervention to promote adherence. Results Preadolescents who reported more critical parenting behaviors reported more depressive symptoms and lower self-efficacy. The relationship between critical parenting and self-efficacy was partially mediated by depressive symptoms. In a second model, depressive symptoms were associated with lower self-efficacy and fewer self-care behaviors. The relationship between depressive symptoms and self-care was fully mediated by self-efficacy. Conclusions Critical parenting behaviors are associated with preadolescents’ psychological well-being, which has implications for self-care. Clinical implications include decreasing critical parenting behaviors and monitoring preadolescents with T1D for depressive symptoms.
Keywords: adherence, critical parenting, depression, self-efficacy, type 1 diabetes
Introduction
Type 1 diabetes (T1D) is a chronic illness requiring complex daily management, including adherence to an insulin regimen (via injections or an insulin pump), blood glucose monitoring, and careful attention to nutrient intake and physical activity (Wysocki, Buckloh, & Greco, 2009). As one of the most common chronic diseases of school-age children (ADA, 2007), it affects many children, and thereby their parents. Many studies have demonstrated that consistent adherence to a T1D regimen is challenging, with particularly high rates of nonadherence among adolescents (Anderson, Ho, Brackett, Finkelstein, & Laffel, 1997). The potential short- and long-term negative consequences of poor adherence have been well documented (Silverstein et al., 2005), yet further examination of the factors which influence adherence is still needed.
There is strong evidence that interpersonal (e.g., parental) and intrapersonal (e.g., mood, self-efficacy) factors contribute to youths’ self-care and adherence to T1D regimens (Greening, Stoppelbein, & Reeves, 2006). The social ecological model posits that these interpersonal and intrapersonal systems interact with one another to influence behavior and adjustment (Bronfenbrenner, 1977). Examining these interrelationships is important for understanding illness management in youth with T1D. For example, Naar-King and colleagues (2006) examined the joint effect of intrapersonal and interpersonal factors and found that child externalizing behaviors, poor family relationships, and less satisfaction with healthcare providers interact to contribute to poor illness management. These results suggest that it is important to examine factors from multiple (e.g., child and parental) systems and their interrelationships when studying youths’ self-care behaviors and overall adherence.
Parental Involvement
Parental involvement in the management of T1D care in youth has been associated with increased adherence to youths’ medical regimens as well as better glycemic control (Anderson et al., 1997; La Greca et al., 1995; Wysocki, Nansel et al., 2009). However, it appears that the quality of the parental interaction is paramount. In fact, negative family interactions have been shown to be associated with worse adherence and metabolic control (Hood, Butler, Anderson, & Laffel, 2007; Jaser & Grey, 2010; Lewin et al., 2006; Schafer, McCaul, & Glasgow, 1986). Specifically, critical parenting (i.e., criticism, nagging, and negativity) appears to be a salient predictor of poor adherence and metabolic control, especially for older adolescents (Duke et al., 2008; Lewin et al., 2006).
Not only are critical parenting behaviors related to adherence and metabolic control, they also appear to influence child psychological well-being. For example, in adolescents with T1D, Butler, Skinner, Gelfand, Berg, & Wiebe (2007) demonstrated that a parenting style characterized by attempts to regulate an adolescent’s thoughts and opinions through guilt and criticism was associated with higher adolescent reported depression as well as lower self-efficacy for managing diabetes, but was not related to reports of adherence. Further, Jaser and Grey (2010) found that observed maternal hostility was correlated with more depressive symptoms in adolescents with T1D.
These findings suggest that examining the quality of parental involvement is very important, as critical parenting has been related to poor adherence and metabolic control (Duke et al., 2008; Jaser & Grey, 2010), adolescent reported depression (Jaser & Grey, 2010), and adolescent reported self-efficacy for diabetes management (Butler et al., 2007). However, the majority of these findings on the effects of parenting behaviors on youth psychological functioning and adherence have focused on older adolescents with relatively little emphasis on younger children or preadolescents. This represents a significant gap in the literature, especially considering that parental involvement is higher in younger children than older adolescents (Anderson, Auslander, Jung, Miller, & Santiago, 1990) and preadolescence is an age when responsibility for diabetes care begins to shift from parent to child (La Greca, Follansbee, & Skyler, 1990) Additionally, research has shown that adolescence is typically marked by a decline in adherence behaviors (Anderson et al., 1997); therefore, studying the preadolescent period before the onset of these difficulties could provide valuable information on both preventative measures as well as the possible mechanisms of decreased adherence.
Child Psychological Characteristics and T1D
Recent research suggests that depression is an influential factor to consider with regard to children’s management of T1D. For example, Butler et al. (2007) have found that critical parenting behaviors are associated with depression in adolescents. Additionally, the presence of depressive symptoms has been linked to poor adherence in adolescents (Korbel, Wiebe, Berg, & Palmer, 2007) and adults (DiMatteo, Lepper, & Croghan, 2000). It has been suggested that increased depressive symptoms may interfere with a child’s ability to cope with diabetes-related stressors and decrease motivation to engage in self-care behaviors (Dantzer, Swendsen, Maurice-Tison, & Salamon, 2003; Korbel et al., 2007). Further, depression appears to be more common in youth with T1D than in the general population (Dantzer et al., 2003), highlighting the importance of studying the relationship of depressive symptoms to self-care and adherence. However, there is currently little research conducted in preadolescent children with regard to depression and self-care and little understanding in this age group of how depression is interrelated with other systems, such as parenting, to affect care.
Self-efficacy is another significant intrapersonal characteristic to consider in the understanding of the contributors to self-care in youth with T1D. Self-efficacy has been found to be negatively related to critical parenting (Butler et al., 2007) and positively related to adherence and glycemic control in older adolescents (Iannotti et al., 2006; Ott, Greening, Palardy, Holderby, & DeBell, 2000). One speculation is that positive parental involvement promotes adolescents’ adherence though increased self-efficacy (Greening et al., 2006). Supporting this hypothesis, Ott et al. (2000) found that self-efficacy served as a mediator between critical parenting behaviors and adherence in adolescents with T1D. Despite the importance of self-efficacy in diabetes management, relatively little attention has been paid to its predictors and correlates and these relationships have not been examined among preadolescents.
Current Study
As the social ecological model suggests, examining the interrelationship of multiple systems is important to gain a better understanding of the complex factors that are related to self-care and adherence in youth with T1D. Critical parenting behaviors have been found to be related to adolescent depression and low self-efficacy for diabetes care, all of which are additionally associated with poorer self-care and adherence to diabetes regimens (Butler et al., 2007; Iannotti et al., 2006; Lewin et al., 2006). Given that these relationships have not been explored during the period of preadolescence, it is therefore important to examine these factors together in a model predicting self-care in preadolescents. The current study aims to elucidate the relationship of critical parenting behaviors, child depressive symptoms, child self-efficacy for diabetes care, and self-care behaviors in preadolescents. Specifically, it was hypothesized that child depressive symptoms would mediate the relationship between critical parenting and self-efficacy and that self-efficacy would mediate the relationship between child depressive symptoms and self-care behaviors in preadolescent youth with T1D.
Method
Participants and Procedure
Participants were 84 preadolescent youth with T1D from outpatient endocrinology clinics at a large, mid-Atlantic urban children’s hospital and its satellite clinics. The sample was mostly Caucasian (73%) with 58% of families earning >$75,000 per year. The sample was 54% female, ages 9–11 years (M = 10.8 years, SD = 0.75). Fifty-five percent of the children were using scheduled insulin injections (2 or 3 shots/day of mixed NPH/regular or analog), while the other 43% were on a more flexible basal/bolus regimen (insulin pump or multiple daily injections). Youth in the sample had an average hemoglobin A1c of 8.1% (SD = 1.22). Participants were enrolled in a larger randomized controlled trial (RCT) study. All data for the current study were obtained at the baseline assessment of the larger intervention trial aimed at assessing the efficacy of an adherence promotion program. This program was delivered in conjunction with standard diabetes education and compared to a standard care condition.
Eligibility requirements included the ability to speak and write in English and being free of developmental disabilities, psychotic disorders, or other serious medical conditions. As the focus of the larger study was on preadolescents, females who had reached menarche were also excluded.
Approval for the study was obtained from the Institutional Review Board. Introductory letters were sent to all parents of preadolescents within the ages of 9–11 years at participating clinics. Phone contact was made to verify enrollment criteria and determine desire to participate. Of the 260 informational letters mailed, 209 families were successfully contacted, 155 of whom met all eligibility criteria. Verbal consent was obtained by 108 families (70%). Of these, 84 (78%) completed baseline data prior to their participation in the RCT. Following study consent and preadolescent assent, the majority of baseline questionnaires were completed through the mail, with ~5% conducted by a trained research assistant either over the telephone or at the child’s diabetes clinic visit.
Measures
Demographic and Medical Data
Medical record reviews provided demographic information as well as insulin regimen and hemoglobin A1c (A1c). A participating parent provided information on income and ethnicity.
Parenting Behaviors
To assess critical parenting behaviors, children completed the Diabetes Family Behavior Checklist (DFBC; Schafer et al., 1986), a measure of perceived family support of diabetes related behaviors. Children rated their parents on items such as “How often does your parent criticize you for not recognizing the results of a blood sugar check?” and “How often does your parent nag you about following your nutrition plan?” The measure is rated on a 5-point Likert scale from “Never” to “At least once a day.” The seven item Negative Parenting subscale was utilized for the current study. Previous studies have found the internal consistency using adolescent reports ranged from .60 to .82 for the Negative Parenting subscale (Lewin et al., 2005). Internal consistency in the current study was marginal (α = .66).
Self-Efficacy
Preadolescents completed a modified version of the Self-Efficacy for Diabetes questionnaire (SED; Grossman, Brink, & Hauser, 1987), which consisted of 24 items assessing how much a child believes that he/she can or cannot handle situation-specific challenges of his/her current diabetes regimens. Responses are rated on a 5-point Likert scale from 1 (very sure I cannot) to 5 (very sure I can), and total scores are represented by the mean item score. Previous studies have shown good reliability and construct validity for the SED (Schilling et al., 2009). Internal consistency in the current study was good (α = .90).
Depressive Symptoms
The Child Depression Inventory (CDI; Kovacs, 1985) consists of 27 items to indicate the degree of depressive symptoms experienced in the past 2 weeks on a 3-point Likert scale ranging from 0 to 2 (total scores range from 0 to 54). This widely used scale has been validated on a large population of 7- to 17-year olds (Kovacs et al., 1996), has good internal consistency (α = .87; Korbel et al., 2007), and correlates with structured diagnostic interviews (Garber, 1984). Internal consistency in the current study was adequate (α = .86). Participants who endorsed suicidal ideation were briefly evaluated by a psychologist and referred for care as needed.
Self-Care Behaviors
The child version of the Self-care Inventory (SCI; La Greca, Swales, Klemp, & Madigan, 1988) was used to measure self-care behaviors. The youth reported on how well they followed prescribed recommendations for 14 specific diabetes-related activities over the past 2-week period. The questionnaire uses a 5-point Likert scale ranging from “Never do it” to “Always do this as recommended without fail,” as well as an option for each question to be marked “not applicable” (N/A). Items on the questionnaire are summed and divided by the total number of questions (subtracting those marked N/A). Scores are then multiplied by 10 in order to provide a more conventional metric. Previous studies have reported good internal consistency for the adolescent report (α = .79; Korbel et al., 2007). Internal consistency in the current study was also adequate (α = .83). Additionally, parents also completed the SCI, reporting on their child’s self-care behaviors. Internal consistency was adequate (α = .78).
Results
Overview of Data Analytic Procedures
First, bivariate correlations were conducted to examine relationships among the variables of interest and demographic variables to determine the need for inclusion as covariates in the mediation model. Hierarchical linear regressions were conducted in PASW (SPSS, Version 18) to assess the hypotheses that the relationship of critical parenting behaviors to self-efficacy for diabetes management is mediated by child depressive symptoms, and the relationship of child depressive symptoms to self-care behaviors is mediated by self-efficacy for diabetes management. Mediation analyses were conducted according to the guidelines of Baron and Kenny (1986): (1) there must be a significant association between the predictor and the outcome, (2) the predictor must be significantly associated with the mediator, (3) that there should be a significant association between the mediator and the outcome, and finally (4) that the addition of the mediator to the regression model should decrease the significance of the relationship between the predictor and the outcome, utilizing Sobel’s test. The effect sizes of the standardized path loadings were assessed according to Cohen (1988) 0.1 = small, 0.3 = medium, and 0.5 = large.
Current Sample
Means and standard deviations of the key variables were examined in order to evaluate the characteristics of the current sample (Table I). Among the participants, the mean CDI score was consistent with research on similarly aged youth with T1D (de Wit & Snoek, 2010) and indicates, on average, low levels of depressive symptoms. Thirteen youths (15%) reported scores above the clinical cutoff (≥13), which is comparable to what other studies have found in youth with T1D (Hood et al., 2006). Youth also reported a rate of critical parenting behaviors consistent with previous studies (Schafer et al., 1986). Similarly, in concert with prior research (Iannotti et al., 2006; Ott et al., 2000), youth reported fairly high levels of self-efficacy for diabetes, reporting on average that they were sure they could complete most diabetes-related tasks. Additionally, reported self-care behaviors were comparable to other samples (Lewin et al., 2009).
Table I.
Correlations Between Study Variables
| Variable | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | Mean (SD) | Range |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Child’s gender | 1 | |||||||||||
| 2. Age | .01 | 1 | ||||||||||
| 3. Ethnicitya | .20 | .09 | 1 | |||||||||
| 4. Insulin regimenb | .07 | −.05 | .22* | 1 | ||||||||
| 5. Critical parenting behaviors | .13 | .04 | −.17 | −.28** | 1 | 17.16 (5.47) | 8–35 | |||||
| 6. Child depression inventory total | .21 | −.23* | .03 | .01 | .31** | 1 | 6.45 (6.09) | 0–27 | ||||
| 7. Self-efficacy | −.11 | .11 | −.05 | .08 | −.27** | −.40** | 1 | 3.85 (5.7) | 2.04–4.96 | |||
| 8. Self-care inventory (child) | −.05 | −.15 | .01 | .09 | −.11 | −.25* | .34** | 1 | 40.15 (6.12) | 25.71–50 | ||
| 9. Self-care inventory (parent) | −.24* | .00 | .19 | .16 | −.18 | −.33** | .19 | .31** | 1 | 38.26 (5.92) | 19.7–50 | |
| 10. Hemoglobin A1c | −.03 | .12 | −.15 | −.02 | .16 | −.01 | .10 | −.01 | −.06 | 1 | 8.1 (1.2) | 5.1–11.9 |
aEthnicity dummy coded in reference to Caucasian.
bInsulin regimen dummy coded in reference to basal/bolus regimen.
*p < .05; **p < .01.
Bivariate correlations were conducted among the psychosocial variables and demographic variables (Table I). Age was significantly negatively correlated with CDI score. As age was the only demographic variable correlated with any of the hypothesized mediators or outcomes, it was included as the first step in both subsequent analyses. Critical parenting behaviors were not significantly associated with child- or parent-reported self-care behaviors. A1c was not significantly correlated with any of the predictor or outcome variables. Both child and parent report of self-care behavior was negatively correlated with child depression. However, only child report of self-care was associated with self-efficacy. Therefore, the mediation model hypothesized between critical parenting, depressive symptoms, and self-efficacy was examined first, followed by the mediation model hypothesized between depressive symptoms, self-efficacy, and child report of self-care behaviors.
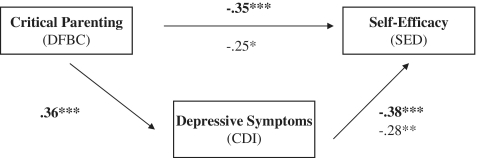
Study Aim 1: Depressive Symptoms Mediating Critical Parenting and Self-Efficacy
Using the criteria for a mediation effect set forth by Baron and Kenny (1986), critical parenting behaviors were significantly associated with depressive symptoms F (2, 83) = 8.93, p < .001, 95% confidence interval (95% CI: 0.18 to 0.65) and self-efficacy F (2, 83) = 6.36, p = .003, 95% CI (−0.05 to −0.02). With all variables in the model, including age in the first step as a covariate, depressive symptoms were significantly associated with self-efficacy F (2, 83) = 7.05, p = .002, 95% CI (−0.05 to −0.01), and the effect of critical parenting behaviors on self-efficacy was significantly decreased when depressive symptoms were included in the final model F (3, 83) = 6.74, p < .001, 95% CI (−0.05 to −0.004), Cohen’s f2 = .24 (Figure 1) indicating a small effect size and a partial mediation (Sobel’s equation z = 2.10, p = .04). Twenty-nine percent of the relationship between critical parenting behaviors and self-efficacy was due to depressive symptoms.
Figure 1.
Depressive symptoms (CDI) partially mediating the relationship between critical parenting behaviors (DFBC) and self-efficacy (SED). Figure illustrates how depressive symptoms partially mediate the relationship between critical parenting and self-efficacy. Bold numbers are beta weights of the relationship between the individual constructs. The non-bolded numbers are beta weights for the entire model after depressive symptoms have been included. *p ≤ .05; **p ≤ .01; ***p ≤ .001.
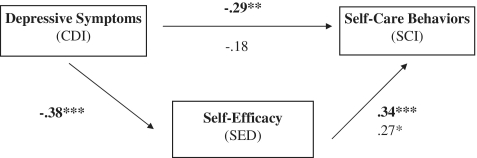
Study Aim 2: Self-Efficacy Mediating Depressive Symptoms and Self-Care Behaviors
Mediation analyses were then conducted to evaluate the relationship among child depressive symptoms, self-efficacy for diabetes management, and self-care behaviors. Depressive symptoms were significantly associated with both self-efficacy F (2, 83) = 7.05, p = .002, 95% CI (−0.05 to −0.02) and self-care behaviors F (2, 83) = 4.46, p = .02, 95% CI (−0.5 to −0.07). With all variables in the final model, including age as a covariate, self-efficacy was significantly associated with self-care behaviors F (2, 83) = 6.33, p = .003, 95% CI (0.56−5.32), and the effect of depressive symptoms on self-care behaviors was no longer a significant predictor of self-care behaviors when self-efficacy was included in the model F (3, 83) = 5.17, p = .003, 95% CI (−0.41 to −0.04), Cohen’s f2 = .17 (Figure 2) indicating a small effect size and a mediation (Sobel’s z = 2.01, p < .04). Thirty-six percent of the relationship between depressive symptoms and self-care was due to self-efficacy.
Figure 2.
Self-efficacy (SED) fully mediating the relationship between depressive symptoms (CDI) and self-care behaviors (SCI). Figure illustrates how self-efficacy mediates the relationship between depressive symptoms and self-care behaviors. Bold numbers are beta weights of the relationship between the individual constructs. The non-bolded numbers are beta weights for the entire model after self-efficacy has been included. *p ≤ .05; **p ≤ .01; ***p ≤ .001.
Discussion
In the important developmental period of preadolescence, critical parenting behaviors appear to be related to youth’s self-efficacy for diabetes management, with depressive symptoms also playing a significant role. These findings are consistent with previous literature concerning older youth or adolescents, which has demonstrated that parenting characterized by regulating a child’s behavior though criticism is associated with lower levels of self-efficacy and greater levels of depression (Butler et al., 2007). The current study corroborates these findings in a younger preadolescent population and elucidates the mechanisms by which critical parenting behaviors are associated with self-efficacy and self-care behaviors.
The relationship identified between critical parenting behaviors and child psychological well-being is of concern because youth with T1D have already been shown to be at greater risk than their non-T1D peers for psychiatric disorders (Blanz, Rensch-Riemann, Fritz-Sigmund, & Schmidt, 1993), including depression (Kovacs, Mukerji, Iyengar, & Drash, 1996). Therefore, the findings from the current study illustrate the importance of helping parents to be involved with their children’s diabetes care in a noncritical way, so as to lower risk for depressive symptoms and poor self-efficacy. Clinically, parental involvement in diabetes care is a primary focus of treatment of adolescents with T1D. However, the quality of that involvement, and the importance of promoting positive parental involvement in care with preadolescents, is highlighted by these findings. Indeed, previous research has found that youth who view their parents as being collaboratively involved in diabetes management report better self-care, fewer depressive symptoms, and more positive mood (Berg et al., 2007; Wiebe et al., 2005).
In the second mediation model, controlling for age, self-efficacy fully explained the relationship between depressive symptoms and self-care behaviors, such that more depressive symptoms were associated with lower self-efficacy, which was associated with fewer self-care behaviors. These findings are consistent with the current literature in adults, which has identified self-efficacy as a mediator of depression and glycemic control in males with T2D (Cherrington, Wallston, & Rothman, 2010). Notably, the current study helps to fill a gap in the literature identified by DiMatteo et al. (2000) by illuminating a mechanism of how depression may affect self-care behaviors, specifically by contributing to the relationship between self-efficacy and self-care behaviors. These findings also highlight the importance of continued assessment of, and potential intervention to improve, self-efficacy for diabetes self-care.
It is interesting to note that, contrary to prior works indicating higher depressive symptoms in older teens (Whittemore et al., 2002), in the current sample, the younger preadolescents, even within our small age range, showed more depressive symptoms than the older preadolescents, although most scores remained in the subclinical range. It is possible that the younger preadolescents in this sample are on the cusp of beginning to take responsibility for their own diabetes management (Anderson et al., 1990) and therefore are subject to an increase of stress, while at the same time, due to their young age, are less able to effectively cope with these new stressors (Landolt, Vollrath, & Ribi, 2002). This increase in responsibility for diabetes care stress coupled with ineffective coping strategies may lead to an increase in depressive symptoms (Berg et al., 2009) that declines with age as children develop more flexible and sophisticated coping styles (Hema et al., 2009). Future research should examine other variables associated with depressive symptoms (e.g., coping styles) and the developmental trajectory of these symptoms into early adolescence.
The fact that there was no significant correlation between critical parenting behaviors and self-care behaviors is consistent with other literature which has failed to find a relationship in younger youth (Schafer, McCaul, Glasgow, 1986; Lewin et al., 2006), although critical parenting has been shown to affect adherence and metabolic control in older adolescents (Duke et al., 2008; Lewin et al., 2006). The explanation for the absence of a correlation may be that, for younger preadolescent children, parents are still responsible for a majority of diabetes-related tasks; therefore, critical parenting behaviors may not have a direct influence on self-care behaviors. However, the negative interactions between youth and their parents may have a deleterious effect on the child’s psychological well-being, including depressive symptoms and poor self-efficacy, which are risk factors for poorer adherence in these preadolescents, as well as in the future as these youth take on more self-care responsibilities.
The lack of a significant relationship between current study variables and A1c is consistent with previous findings that have failed to find a direct relationship between psychosocial variables and glycemic control (Berg et al., 2007; Dantzer et al., 2003). Further, Helgeson (2009) found that depressive symptoms were not predictive of metabolic control concurrently, but rather were related to difficulties in metabolic control over time. Therefore, the relationship of depressive symptoms with glycemic control may not be seen in cross-sectional research (Helgeson, Siminerio, Escobar, & Becker, 2009). Future research should examine the effects of depressive symptoms on A1c over time.
Although our findings that self-care was not related to glycemic control are not consistent with the overall literature (Hood, Peterson, Rohan, & Drotar, 2009), it appears that the relationship between adherence and A1c in preadolescents may not be as clear as this relationship in adolescents. It has been speculated that hormonal changes associated with puberty account for the majority of differences in metabolic control during early adolescence, and self-care accounts for more variability in metabolic control as teens move to later adolescence (Helgeson et al., 2009). Indeed, research has found that poor self-care was more highly associated with poor glycemic control among older adolescents than younger adolescents (Helgeson et al., 2009; Iannotti et al., 2006; La Greca, Follansbee, & Skyler, 1990). Therefore it could be that the effects of poor self-care behaviors in preadolescence on glycemic control may not be detectable until later adolescence.
Of note is that parent report of self-care behavior, in contrast to child report, was not correlated with youth self-efficacy for diabetes, although it was related to youth depressive symptoms and youth report of self-care behaviors. Because preadolescence is a time period when some responsibilities are transferred to the child, and neither parent nor child report is a perfect measure of actual behaviors, future research should continue to examine both parent and child report.
Clinical Implications
The results from the current study suggest paying careful attention to, and potentially working toward minimizing, critical parenting behaviors in diabetes-specific interactions with preadolescents. There has been significant recent attention on encouraging parental involvement with diabetes management and continuing that involvement through adolescence (Wysocki et al., 2009). The quality of the involvement is clearly essential. If healthcare providers simply encourage parents to be involved with their preadolescent’s diabetes management without guidelines for promoting the type of supportive involvement necessary, parents may end up not only decreasing child self-care behaviors, but increasing risk for their child’s depressive symptoms and lowering their self-efficacy for diabetes management. Instead, providers could be specific that parental involvement should include encouragement and praise for self-care and avoid criticism or “nagging.” Indeed, research has shown that supportive parenting in conjunction with parental monitoring of diabetes tasks contributes to adherence (Ellis et al., 2007). Examples of clinical applications include the design of brief prevention programs aimed at providing parents with ideas of how to stay involved using authoritative, supportive parenting, and reducing critical parenting behaviors.
The current study also suggests that depressive symptoms are relevant to self-care in preadolescent children with diabetes. It is important not to ignore the importance of mood until youth reach adolescence, but rather to recognize the cascading impact that depressive symptoms, even those that are subclinical, may play on diabetes management. Therefore, it is important to assess for depressive symptoms in order to refer and treat these symptoms as a way to improve self-efficacy and self-care in youth (Monaghan, Singh, Streisand, & Cogen, 2010; Silverstein et al., 2005).
Because of the importance and interconnectedness of both parenting behaviors and youth internalizing concerns, it is crucial to involve both parents and youth in prevention and intervention efforts aimed at improving diabetes management in preadolescent children. Further, the importance of quality of parental involvement and child depressive symptoms cannot be ignored until adolescence, but needs to be addressed earlier in childhood.
Limitations and Future Research
Although findings are clinically relevant and add to the existing literature based largely on adolescents, the current study has several limitations that should be addressed. First, the study is cross-sectional which limits the ability to determine causality and the elucidation of the transactional relationship between child and parent factors. Future research should be longitudinal, particularly focused on expanding the understanding of how these relationships change across childhood and through adolescence. Second, only preadolescent report of parenting behaviors, internalizing concerns, and diabetes self-care were utilized. This adds to the possibility that the results may be inflated because of single-rater bias. Although the youth’s perception of these issues is important and relevant, future research should also examine parent reports of these concerns as well as other indicators of adherence and metabolic control, such as blood glucose variability. In addition, the internal consistency for the DFBC in the current study was marginal (α = .66) so results should be interpreted with caution. Additionally, data collection for this study began in 2003, and newer measures currently exist. Future research should utilize a more reliable measure of critical parenting to confirm the results of the current study, as well as utilizing the most up-to-date and well-validated measures.
Conclusion
It is important to examine factors associated with self-care of T1D in preadolescence, a time period which immediately precedes an age group with increased likelihood of a decline in disease management and glycemic control. The current study found that critical parenting behaviors, child depressive symptoms, and self-efficacy for diabetes care were interrelated and associated with self-care behaviors. Specifically, the association between critical parenting behaviors and self-efficacy was mediated by child depressive symptoms, and the association between depressive symptoms and self-care was mediated by self-efficacy. Clinical implications include the importance of providing support to parents to decrease critical behaviors and assessing and addressing child depressive symptoms and self-efficacy for diabetes care.
Funding
This research was supported by National Institutes of Health/the National Institute of Diabetes and Digestive and Kidney Diseases Grants (1K23DK62161 to R.S.).
Conflict of interest: None declared.
References
- American Diabetes Association (ADA) Diabetes care in the school and day care setting. Diabetes Care. 2007;30:S66–73. doi: 10.2337/dc07-S066. [DOI] [PubMed] [Google Scholar]
- Anderson B, Auslander W F, Jung K C, Miller J P, Santiago J V. Assessing family sharing of diabetes responsibilities. Journal of Pediatric Psychology. 1990;15:477–492. doi: 10.1093/jpepsy/15.4.477. [DOI] [PubMed] [Google Scholar]
- Anderson B, Ho J, Brackett J, Finkelstein D, Laffel L. Parental involvement in diabetes management tasks: Relationships to blood glucose monitoring adherence and metabolic control in young adolescents with insulin-dependent diabetes mellitus. Journal of Pediatrics. 1997;130:257–265. doi: 10.1016/s0022-3476(97)70352-4. [DOI] [PubMed] [Google Scholar]
- Baron R M, Kenny D A. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Berg C A, Skinner M, Ko K, Butler J M, Palmer D L, Butner J, Wiebe D J. The fit between stress appraisal and dyadic coping in understanding perceived coping effectiveness for adolescents with type 1 diabetes. Journal of Family Psychology. 2009;23:521–530. doi: 10.1037/a0015556. [DOI] [PubMed] [Google Scholar]
- Berg C A, Wiebe D J, Beveridge R M, Palmer D L, Korbel C D, Upchurch R, Swinyard MT, Lindsay R, Donaldson DL. Mother child appraised involvement in coping with diabetes stressors and emotional adjustment. Journal of Pediatric Psychology. 2007;32:995–1005. doi: 10.1093/jpepsy/jsm043. [DOI] [PubMed] [Google Scholar]
- Blanz B J, Rensch-Riemann B S, Fritz-Sigmund D I, Schmidt M H. IDDM is a risk factor for adolescent psychiatric disorders. Diabetes Care. 1993;16:1579–1587. doi: 10.2337/diacare.16.12.1579. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. Toward an experimental ecology of human development. American Psychologist. 1977;32:513–531. [Google Scholar]
- Butler J M, Skinner M, Gelfand D, Berg C A, Wiebe D J. Maternal parenting style and adjustment in adolescents with type I diabetes. Journal of Pediatric Psychology. 2007;32:1227–1237. doi: 10.1093/jpepsy/jsm065. [DOI] [PubMed] [Google Scholar]
- Cherrington A, Wallston K A, Rothman R L. Exploring the relationship between diabetes self-efficacy, depressive symptoms, and glycemic control among men and women with type 2 diabetes. Journal of Behavioral Medicine. 2010;33:81–89. doi: 10.1007/s10865-009-9233-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Earlbaum, NJ: Hillsdale; 1988. [Google Scholar]
- Dantzer C, Swendsen J, Maurice-Tison S, Salamon R. Anxiety and depression in juvenile diabetes: A critical review. Clinical Psychology Review. 2003;23:787–800. doi: 10.1016/s0272-7358(03)00069-2. [DOI] [PubMed] [Google Scholar]
- de Wit M, Snoek F J. Depressive symptoms and unmet psychological needs of Dutch youth with type 1 diabetes: results of a web-survey. Pediatric Diabetes. 2010;12:172–176. doi: 10.1111/j.1399-5448.2010.00673.x. [DOI] [PubMed] [Google Scholar]
- DiMatteo M R, Lepper H S, Croghan T W. Depression is a risk factor for noncompliance with medical treatment: Meta-analysis of the effects of anxiety and depression on patient adherence. Archives of Internal Medicine. 2000;160:2101–2107. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- Duke D C, Geffken G R, Lewin A B, Williams L B, Storch E A, Silverstein J H. Glycemic control in youth with type 1 diabetes: Family predictors and mediators. Journal of Pediatric Psychology. 2008;33:719–727. doi: 10.1093/jpepsy/jsn012. [DOI] [PubMed] [Google Scholar]
- Ellis D A, Podolski C L, Frey M, Naar-King S, Wang B, Moltz K. The role of parental monitoring in adolescent health outcomes: Impact on regimen adherence in youth with type 1 diabetes. Journal of Pediatric Psychology. 2007;32:907–917. doi: 10.1093/jpepsy/jsm009. [DOI] [PubMed] [Google Scholar]
- Garber J. Classification of childhood psychopathology: A developmental perspective. Child Development. 1984;55:30–48. [PubMed] [Google Scholar]
- Greening L, Stoppelbein L, Reeves C B. A Model for promoting adolescents’ adherence to treatment for Type 1 diabetes mellitus. Children's Heath Care. 2006;35:247–267. [Google Scholar]
- Grossman H Y, Brink S, Hauser S T. Self-efficacy in adolescent girls and boys with insulin-dependent diabetes mellitus. Diabetes Care. 1987;10:324–329. doi: 10.2337/diacare.10.3.324. [DOI] [PubMed] [Google Scholar]
- Helgeson V S, Siminerio L, Escobar O, Becker D. Predictors of metabolic control among adolescents with diabetes: A 4-year longitudinal study. Journal of Pediatric Psychology. 2009;34:254–270. doi: 10.1093/jpepsy/jsn079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hema D A, Roper S O, Nehring J W, Call A, Mandleco B L, Dyches T T. Daily stressors and coping responses of children and adolescents with type 1 diabetes. Child: Care, Health and Development. 2009;35:330–339. doi: 10.1111/j.1365-2214.2009.00937.x. [DOI] [PubMed] [Google Scholar]
- Hood K K, Butler D A, Anderson B J, Laffel L M. Updated and revised Diabetes Family Conflict Scale. Diabetes Care. 2007;30:1764–1769. doi: 10.2337/dc06-2358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hood K K, Huestis S, Maher A, Butler D, Volkening L, Laffel L M. Depressive symptoms in children and adolescents with type 1 diabetes: Association with diabetes-specific characteristics. Diabetes Care. 2006;29:1389–1391. doi: 10.2337/dc06-0087. [DOI] [PubMed] [Google Scholar]
- Hood K K, Peterson C M, Rohan J M, Drotar D. Association between adherence and glycemic control in pediatric type 1 diabetes: A meta-analysis. Pediatrics. 2009;124:e1171–e1179. doi: 10.1542/peds.2009-0207. [DOI] [PubMed] [Google Scholar]
- Iannotti R J, Schneider S, Nansel T R, Haynie D L, Plotnick L P, Clark L M, Sobel DO, Imons-Morton B. Self-efficacy, outcome expectations, and diabetes self-management in adolescents with type 1 diabetes. Journal of Developmental and Behavioral Pediatrics. 2006;27:98–105. doi: 10.1097/00004703-200604000-00003. [DOI] [PubMed] [Google Scholar]
- Jaser S S, Grey M. A pilot study of observed parenting and adjustment in adolescents with type 1 diabetes and their mothers. Journal of Pediatric Psychology. 2010;35:738–747. doi: 10.1093/jpepsy/jsp098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korbel C D, Wiebe D J, Berg C A, Palmer D L. Gender differences in adherence to type 1 diabetes management across adolescence: The mediating role of depression. Children's Heath Care. 2007;36:83–98. [Google Scholar]
- Kovacs M. The Children's Depression Inventory (CDI) Psychopharmacology Bulletin. 1985;21:995–998. [PubMed] [Google Scholar]
- Kovacs M, Mukerji P, Iyengar S, Drash A. Psychiatric disorder and metabolic control among youths with IDDM. A longitudinal study. Diabetes Care. 1996;19:318–323. doi: 10.2337/diacare.19.4.318. [DOI] [PubMed] [Google Scholar]
- La Greca A M, Swales T, Klemp S, Madigan S, Fisher E B, Jr, Santiago J V. I get by with a little help from my family and friends: Adolescents' support for diabetes care. Journal of Pediatric Psychology. 1995;20:449–476. doi: 10.1093/jpepsy/20.4.449. [DOI] [PubMed] [Google Scholar]
- La Greca A M, Follansbee D, Skyler J S. Developmental and behavioral aspects of diabetes management in youngsters. Children's Health Care. 1990;19:132–139. [Google Scholar]
- La Greca A M, Swales T, Klemp S, Madigan S. In Ninth Annual Sessions of the Society of Behavioral Medicine (p. A42) Baltimore, MD: Society of Behavioral Medicine; 1988. Self care behaviors among adolescents with diabetes. [Google Scholar]
- Landolt M A, Vollrath M, Ribi K. Predictors of coping strategy selection in paediatric patients. Acta Paediatrica. 2002;91:954–960. doi: 10.1080/080352502760272650. [DOI] [PubMed] [Google Scholar]
- Lewin A B, Geffken G, Heidgerken A, Duke D, Novoa W, Williams L, Storch E. The Diabetes Family Behavior Checklist: A psychometric evaluation. Journal of Clinical Psychology in Medical Settings. 2005;12:315–322. [Google Scholar]
- Lewin A B, Heidgerken A D, Geffken G R, Williams L B, Storch E A, Gelfand K M, Silverstein J H. The relation between family factors and metabolic control: The role of diabetes adherence. Journal of Pediatric Psychology. 2006;31:174–183. doi: 10.1093/jpepsy/jsj004. [DOI] [PubMed] [Google Scholar]
- Lewin A B, LaGreca A M, Geffken G R, Williams L B, Duke D C, Storch E A, Silverstein JH. Validity and reliability of an adolescent and parent rating scale of type 1 diabetes adherence behaviors: The Self-Care Inventory (SCI) Journal of Pediatric Psychology. 2009;34:999–1007. doi: 10.1093/jpepsy/jsp032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monaghan M, Singh C, Streisand R, Cogen F R. Screening and identification of children and adolescents at risk for depression during a diabetes clinic visit. Diabetes Spectrum. 2010;23:25–31. [Google Scholar]
- Naar-King S, Podolski C L, Ellis D A, Frey M A, Templin T. Social ecological model of illness management in high-risk youths with type 1 diabetes. Journal of Consulting and Clinical Psychology. 2006;74:785–789. doi: 10.1037/0022-006X.74.4.785. [DOI] [PubMed] [Google Scholar]
- Ott J, Greening L, Palardy N, Holderby A, DeBell W K. Self-efficacy as a mediator variable for adolescents' adherence to treatment for insulin-dependent diabetes mellitus. Children's Heath Care. 2000;29:47–63. [Google Scholar]
- Schafer L C, McCaul K D, Glasgow R E. Supportive and nonsupportive family behaviors: Relationships to adherence and metabolic control in persons with type I diabetes. Diabetes Care. 1986;9:179–185. doi: 10.2337/diacare.9.2.179. [DOI] [PubMed] [Google Scholar]
- Schilling L S, Dixon J K, Knafl K A, Lynn M R, Murphy K, Dumser S, Dixon J K. A new self-report measure of self-management of type 1 diabetes for adolescents. Nursing Research. 2009;58:228–236. doi: 10.1097/NNR.0b013e3181ac142a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverstein J, Klingensmith G, Copeland K, Plotnick L, Kaufman F, Laffel L, Deeb L, Grey M, Anderson B, Holzmeister LA, Clark N. Care of children and adolescents with type 1 diabetes: A statement of the American Diabetes Association. Diabetes Care. 2005;28:186–212. doi: 10.2337/diacare.28.1.186. PSAW (Version 18) [Computer software]. Chicago, IL: SPSS, Inc. [DOI] [PubMed] [Google Scholar]
- Whittemore R, Kanner S, Singleton S, Hamrin V, Chiu J, Grey M. Correlates of depressive symptoms in adolescents with type 1 diabetes. Pediatric Diabetes. 2002;3:135–143. doi: 10.1034/j.1399-5448.2002.30303.x. [DOI] [PubMed] [Google Scholar]
- Wiebe D J, Berg C A, Korbel C, Palmer D L, Beveridge R M, Upchurch R, Lindsay R, Swinyard MT, Donaldson DL. Children's appraisals of maternal involvement in coping with diabetes: Enhancing our understanding of adherence, metabolic control, and quality of life across adolescence. Journal of Pediatric Psychology. 2005;30:167–178. doi: 10.1093/jpepsy/jsi004. [DOI] [PubMed] [Google Scholar]
- Wysocki T, Buckloh L M, Greco P. The psychological context of diabetes mellitus in youths. In: Roberts M C, Steele R G, editors. Handbook of Pediatric Psychology Fourth Edition. New York: The Guilford Press; 2009. pp. 278–302. [Google Scholar]
- Wysocki T, Nansel T R, Holmbeck G N, Chen R, Laffel L, Anderson B J, Weissberg-Benchell J, Steering Committee of the Family Management of Childhood Diabetes Study Collaborative involvement of primary and secondary caregivers: Associations with youths' diabetes outcomes. Journal of Pediatric Psychology. 2009;34:869–881. doi: 10.1093/jpepsy/jsn136. [DOI] [PMC free article] [PubMed] [Google Scholar]