Schizophrenia, depression, epilepsy, dementia, alcohol dependence and other mental, neurological and substance-use (MNS) disorders constitute 13% of the global burden of disease (Table 1), surpassing both cardiovascular disease and cancer1. Depression is the third leading contributor to the global disease burden, and alcohol and illicit drug use account for more than 5% (ref. 2). Every seven seconds, someone develops dementia3, costing the world up to US$609 billion in 2009 (ref. 4). By 2020, an estimated 1.5 million people will die each year by suicide, and between 15 and 30 million will make the attempt5.
TABLE 1.
GLOBAL BURDEN OF MENTAL, NEUROLOGICAL AND SUBSTANCE-USE (MNS) DISORDERS*
| Rank | Worldwide | High-income countries† | Low- and middle-income countries | |||
|---|---|---|---|---|---|---|
| Cause | DALYs‡ (millions) | Cause | DALYs (millions) | Cause | DALYs (millions) | |
| 1 | Unipolar depressive disorders | 65.5 | Unipolar depressive disorders | 10.0 | Unipolar depressive disorders | 55.5 |
|
| ||||||
| 2 | Alcohol-use disorders | 23.7 | Alzheimer’s and other dementias | 4.4 | Alcohol-use disorders | 19.5 |
|
| ||||||
| 3 | Schizophrenia | 16.8 | Alcohol-use disorders | 4.2 | Schizophrenia | 15.2 |
|
| ||||||
| 4 | Bipolar affective disorder | 14.4 | Drug-use disorders | 1.9 | Bipolar affective disorder | 12.9 |
|
| ||||||
| 5 | Alzheimer’s and other dementias | 11.2 | Schizophrenia | 1.6 | Epilepsy | 7.3 |
|
| ||||||
| 6 | Drug-use disorders | 8.4 | Bipolar affective disorder | 1.5 | Alzheimer’s and other dementias | 6.8 |
|
| ||||||
| 7 | Epilepsy | 7.9 | Migraine | 1.4 | Drug-use disorders | 6.5 |
|
| ||||||
| 8 | Migraine | 7.8 | Panic disorder | 0.8 | Migraine | 6.3 |
|
| ||||||
| 9 | Panic disorder | 7.0 | Insomnia (primary) | 0.8 | Panic disorder | 6.2 |
|
| ||||||
| 10 | Obsessive–compulsive disorder | 5.1 | Parkinson’s disease | 0.7 | Obsessive–compulsive disorder | 4.5 |
|
| ||||||
| 11 | Insomnia (primary) | 3.6 | Obsessive–compulsive disorder | 0.6 | Post-traumatic stress disorder | 3.0 |
|
| ||||||
| 12 | Post-traumatic stress disorder | 3.5 | Epilepsy | 0.5 | Insomnia (primary) | 2.9 |
|
| ||||||
| 13 | Parkinson’s disease | 1.7 | Post-traumatic stress disorder | 0.5 | Multiple sclerosis | 1.2 |
|
| ||||||
| 14 | Multiple sclerosis | 1.5 | Multiple sclerosis | 0.3 | Parkinson’s disease | 1.0 |
Data from ref. 1. Examples of MNS disorders under the purview of the Grand Challenges in Global Mental Health initiative.
World Bank criteria for income (2009 gross national income (GNI) per capita): low income is US$995 equivalent or less; middle income is $996–12,195; high income is $12,196 or more.
A disability-adjusted life year (DALY) is a unit for measuring the amount of health lost because of a disease or injury. It is calculated as the present value of the future years of disability-free life that are lost as a result of the premature deaths or disability occurring in a particular year.
The absence of cures, and the dearth of preventive interventions for MNS disorders, in part reflects a limited understanding of the brain and its molecular and cellular mechanisms. Where there are effective treatments, they are frequently not available to those in greatest need. In 83% of low-income countries, there are no anti-Parkinsonian treatments in primary care; in 25% there are no anti-epileptic drugs6. Unequal distribution of human resources — between and within countries — further weakens access: the World Health Organization’s European region has 200 times as many psychiatrists as in Africa7. Across all countries, investment in fundamental research into preventing and treating MNS disorders is disproportionately low relative to the disease burden8.
To address this state of affairs, the Grand Challenges in Global Mental Health initiative has identified priorities for research in the next 10 years that will make an impact on the lives of people living with MNS disorders. The study was funded by the US National Institute of Mental Health (NIMH) in Bethesda, Maryland, supported by the Global Alliance for Chronic Diseases (GACD), headquartered in London. Answers to the questions posed will require a surge in discovery and delivery science. We use the term ‘mental health’ as a convenient label for MNS disorders. We exclude conditions with a vascular or infectious aetiology (such as stroke or cerebral malaria), because these fell within the scope of the two previous grand challenges initiatives — in global health and in chronic non-communicable diseases9.
This initiative differs from previous priority-setting exercises for mental health10–12 in four ways. First, its scope is global. Second, it is the first to employ the Delphi method13, a structured technique using controlled feedback to arrive at consensus within a dispersed panel of many participants. Third, it covers the full range of MNS disorders. Finally, the effort hopes to build a wide-ranging community of research funders — much as the challenge for non-communicable diseases led to the creation of the GACD.
SETTING PRIORITIES
The prioritization exercise assembled the largest international Delphi panel so far on the subject. An executive committee of leaders of key funding agencies provided broad oversight. A scientific advisory board comprising leaders in the relevant scientific disciplines guided the process. And an administrative team from the NIMH worked with the chairs of the committee and advisory board to coordinate communication and data analysis.
The advisory board nominated 594 researchers, advocates, programme implementers and clinicians; 422, working in more than 60 countries, agreed to participate. Researchers in genetics and genomics, neuroscience, basic behavioural science and neurodevelopment made up just over one-third of the panel. Mental-health services researchers constituted another quarter, and a further third were clinical researchers and epidemiologists (see Supplementary Figs 1–3).
In Round 1, panel members were asked to respond to the question “What are the grand challenges in global mental health?” by listing up to five areas they considered to be top priorities. As in previous initiatives14,15, a ‘grand challenge’ was defined as “a specific barrier that, if removed, would help to solve an important health problem. If successfully implemented, the intervention(s) it could lead to would have a high likelihood of feasibility for scaling up and impact.” Round 1 yielded 1,565 challenges.
These were distilled by the administrative team and chairs of the executive committee and advisory board into a shorter list of 154 unique challenges from which panellists selected their top 40 in Round 2 (Supplementary Table 1). The top 25 challenges from this list are shown in Table 2. Round 3 asked panellists to rank each challenge on a four-point scale for: ability to reduce disease burden; impact on equity; immediacy of impact; and feasibility (see Supplementary Methods). To arrive at the final ranked master list of grand challenges, individual rankings for each challenge were weighted, summed across all four criteria, and divided by the total number of responses (Supplementary Table 3).
TABLE 2.
GRAND CHALLENGES FOR MNS DISORDERS
| Top 25 challenges* | Illustrative research questions | |||
|---|---|---|---|---|
| Goal A Identify root causes, risk and protective factors |
|
|
||
| Goal B Advance prevention and implementation of early interventions |
|
|
||
| Goal C Improve treatments and expand access to care |
|
|
||
| Goal D Raise awareness of the global burden |
|
|
||
| Goal E Build human resource capacity |
|
|
||
| Goal F Transform health- system and policy responses |
|
|
||
| Summary principles |
|
|
|
|
The order in which the challenges are presented does not indicate frequency of endorsement or relative importance. Bold type denotes the top five challenges ranked by disease-burden reduction, impact on equity, immediacy of impact and feasibility.
THE LIST
The 25 grand challenges in Table 2 run the research gamut from preclinical questions into the aetiology and treatment of MNS disorders, to implementation and policy needs to scale up effective interventions. All the challenges emphasize the need for global cooperation in the conduct of research to create shared access to data, expertise and capacity-building opportunities. Children emerge as requiring particular attention for prevention and care. Most mental disorders involve developmental processes, so reducing the duration of untreated illness by focusing resources on the earliest definable clinical stage of illness could revolutionize treatment. Similarly, it is imperative that we explore the role of prenatal exposures and develop interventions to reduce the long-term negative impact of low childhood socioeconomic status on cognitive ability.
The challenges capture several broad themes. First, the results underscore the need for research that uses a life-course approach. This approach acknowledges that many MNS disorders either begin or manifest in early life, and is equally attentive to risk factors and disorders affecting children and the elderly. Efforts to build mental capital — the cognitive and emotional resources that influence how well an individual is able to contribute to society and experience a high quality of life — could also mitigate the risk of disorders such as depression, substance-use disorders, bipolar disorder and dementia16.
Second, the challenges recognize that the suffering caused by MNS disorders extends beyond the patient to family members and communities. Thus, health-system-wide changes are crucial, together with attention to social exclusion and discrimination. At the same time, research into systems interventions, such as integrating care for MNS disorders into chronic-disease care, could transform health services and reduce costs.
Third, the challenges underline the fact that all care and treatment interventions — psychosocial or pharmacological, simple or complex — should have an evidence base to provide programme planners, clinicians and policy-makers with effective care packages. Finally, the panel’s responses underscore important relationships between environmental exposures and MNS disorders. Extreme poverty, war and natural disasters affect large swathes of the world, and we still do not fully understand the mechanisms by which mental disorders might be averted or precipitated in those settings.
NEXT STEPS
There have been some major advances in our understanding of the aetiology and treatment of MNS disorders. Future breakthroughs are likely to depend on discoveries in genomics and neuroscience, in tandem with exploration of the role of sociocultural and environmental contexts. The top five challenges ranked by disease-burden reduction, impact on equity, immediacy of impact, and feasibility should serve as a starting point for immediate research and prioritization of policies (see bold lines in Table 2).
Action on all the challenges will require long-term investment. Substantial research progress can be achieved in the next ten years if funding begins immediately. Already, the NIMH’s initiative, Collaborative Hubs for International Research in Mental Health, has committed to support research on the use of non-specialist mental health-care providers and research training in low- and middle-income countries. But a wider set of stakeholders must also be engaged, particularly in problems that require integrated research and policy interventions.
The WHO should disseminate information on these challenges to its member countries’ health ministries and research councils to shape research and action priorities. Given the intimate relationship between economic and social development and the needs of people with MNS disorders, the World Bank, regional development banks, national development agencies, foundations, nongovernmental organizations and the global business community should all participate in addressing the challenges.
Researchers and funders have tremendous responsibility in this context. Consortia and networks, advocacy organizations, universities and their partners should organize their activities around one or more of the goals and the attendant grand challenges. The leaderships of the Grand Challenges in Global Mental Health, the GACD and their partners will meet in October to develop a strategy for regular monitoring of progress.
Even incremental progress in addressing the grand challenges in global mental health could lead to significant economic and quality-of-life benefits — including reductions in inappropriate use of health care and increased productivity for years to come17 — that would far outweigh investment costs. Although the greatest challenge — the elimination of MNS disorders — may not be attainable within the next 10 years, the research suggested above must be conducted forthwith.
Supplementary Material
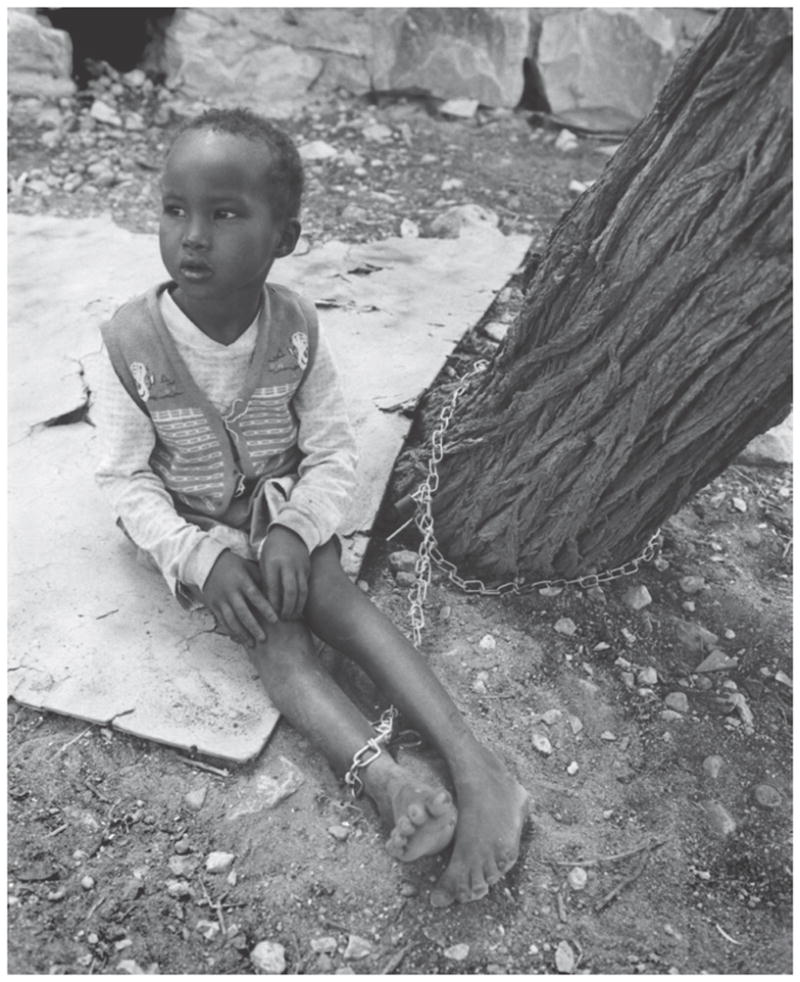
Improving treatment for children with mental illness, like this girl in Somalia, is an urgent priority.

Women in Priluki psychiatric hospital, Ukraine.
Footnotes
Supplementary Information and a full list of authors accompany this article online at www.nature.com/nature and can also be viewed at http://grandchallengesgmh.nimh.nih.gov.
Contributor Information
Pamela Y. Collins, Email: pamela.collins@nih.gov, Office for Research on Disparities and Global Mental Health, National Institute of Mental Health, Maryland, USA
Vikram Patel, Centre for Global Mental Health, London School of Hygiene & Tropical Medicine UK, Sangath, Goa, India.
Sarah S. Joestl, Office for Research on Disparities and Global Mental Health, National Institute of Mental Health, USA
Dana March, Office for Research on Disparities and Global Mental Health, National Institute of Mental Health, USA.
Thomas R. Insel, National Institute of Mental Health, USA
Abdallah S. Daar, Email: a.daar@utoronto.ca, University of Toronto and McLaughlin-Rotman Centre for Global Health, Toronto, Canada, and Chair, Global Alliance for Chronic Diseases
References
- 1.World Health Organization. The Global Burden of Disease: 2004 Update. WHO; 2008. [Google Scholar]
- 2.WHO. Atlas on Substance Use. WHO; 2010. [Google Scholar]
- 3.Ferri CP, et al. Lancet. 2005;366:2112–2117. doi: 10.1016/S0140-6736(05)67889-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wimo A, Winblad B, Jönsson L. Alzheimer’s & Dementia. 2010;6:98–103. doi: 10.1016/j.jalz.2010.01.010. [DOI] [PubMed] [Google Scholar]
- 5.Bertolote J, Flieschmann A. Suicidologi. 2002;7:6–8. [Google Scholar]
- 6.WHO. Country Resources for Neurological Disorders 2004. WHO; 2004. [Google Scholar]
- 7.WHO. Mental Health Atlas. WHO; 2005. [Google Scholar]
- 8.Saxena S, Thornicroft G, Knapp M, Whiteford H. Lancet. 2007;370:878–889. doi: 10.1016/S0140-6736(07)61239-2. [DOI] [PubMed] [Google Scholar]
- 9.Daar AS, et al. Nature. 2007;450:494–496. doi: 10.1038/450494a. [DOI] [PubMed] [Google Scholar]
- 10.Lancet Mental Health Group. Lancet. 2007;370:1241–1252. [Google Scholar]
- 11.Sharan P, et al. Br J Psychiatry. 2009;195:354–363. doi: 10.1192/bjp.bp.108.050187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tomlinson M, et al. Bull WHO. 2009;87:438–446. doi: 10.2471/BLT.08.054353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jones J, Hunter D. Br Med J. 1995;311:376–380. doi: 10.1136/bmj.311.7001.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Daar AS, et al. Nature. 2007;450:494–496. doi: 10.1038/450494a. [DOI] [PubMed] [Google Scholar]
- 15.Varmus H, et al. Science. 2003;302:398–399. doi: 10.1126/science.1091769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beddington J, et al. Nature. 2008;455:1057–1060. doi: 10.1038/4551057a. [DOI] [PubMed] [Google Scholar]
- 17.Rupp A. Br J Psychiatry. 1995;166:26–33. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


