Abstract
Background:
Aconitum napellus (Acn) is used topically to relieve pain, itching and inflammation, and internally to reduce febrile states, among others. Any circadian time-related consequences of Acn administration are unknown. The objective of this study was to explore the effects of two doses of Acn on body temperature (BT) of mice treated at six different times over 24 hours.
Materials and Methods:
BALB/c female mice were housed in six chambers (six mice each) with air temperature 24 ± 3°C, humidity 60 ± 4%, and a 12-hours light (L)/12-hours dark cycle, but with L-onset staggered by 4 hours between chambers so that study at one external test time resulted in six test times (02, 06, 10, 14, 18 and 22 hours [h] after light onset). Rectal temperature (RT; in °C) was measured at baseline (B) and 1 hour after oral treatment with placebo (P) or two doses of Acn (6C and 30C, two studies each) in six studies over an 8 day span. The difference in RT for each mouse from the respective B + P timepoint mean RT was computed following each Acn treatment, and data from each of the six studies (original RT and difference from B + P) were analyzed for time-effect by analysis of variance (ANOVA) and for circadian rhythm by 24-hour cosine fitting.
Results:
A circadian rhythm in RT was found at B and after P (mean: 35.58°C vs. 35.69°C; peak: 15:31 h vs. 15:40 h) and after each Acn dose (30C or 6C). Acn induced hyperthermia and the overall change in BT was rhythmically significant for each dose (mean = +1.95°C vs. +1.70°C), with greatest hyperthermia observed during the L-span for each dose (peak = 08:56 h vs. 05:17 h).
Conclusion:
Acn administered around the clock induced hyperthermia overall and in a time-dependent manner, with greatest effects during the resting (L) span. Thus, time of day may significantly impact the outcome of Acn and other homeopathic treatments and should be considered in determining optimal dosing and treatment time(s) in order to increase the desired outcome and decrease undesired effects.
Keywords: Aconite, Aconitum napellus, chronotherapy, circadian, homeopathy, hyperthermia, pharmacognosy
INTRODUCTION
Aconitum napellus, commonly called Aconite (Acn), is a perennial species of the Ranunculaceae plant family that is found in wet, shady places in hilly districts at high altitudes throughout the Northern Hemisphere mountainous regions in Europe, Asia and in northwestern North America. Its name is derived from Aconis, a Black Sea port in the ancient region of Bithynia (in Asia Minor corresponding roughly to modern central-northern Turkey), and napus, a turnip, due to the shape of its roots, which have occasionally been mistaken for horseradish. It has many English common names, such as: aconite, bear's foot, blue rocket, devil's helmet, friar's cap, helmet flower, monkshood, monksblood, queen's fettle, soldier's cap, Turk's cap and wolfsbane. Acn has been introduced as an ornamental garden plant and is used in herbal medicine, but it is considered a vertebrate poison (from cardio and respiratory actions) and is one of the most, if not the most, poisonous known alkaloids. Handling the plant can cause allergic reactions and rashes (even slight contact with the flowers can cause fingers to become numb) and is dangerous if exposed to open cuts, scratches or sores or ingested.[1,2] Its use dates to remote times when Asian warriors applied Aconitum tincture to arrow tips to turn them into lethal weapons of war.[3] Acn's poisonous properties have also been used in hunting and fishing, as well as for criminal purposes.[4]
Acn is safe only in extremely minute topical or oral doses. In ancient times, the dried tuberous root of A. napellus was used as a sedative medicine and painkiller. In the 2nd century BC, the Greek physician and poet Nicander of Colophon described in his “Alexipharmaca” the symptoms and uses of the herbal drug aconite.[5] Aconitum species have been used in China as an essential drug in traditional Chinese medicine for more than 2000 years,[6] and in the 2nd century AD, a famous Chinese surgeon, Hwa Tuo, employed aconite as part of a special powder in surgeries.[7] It was known to be used in the treatment of rheumatism, sciatica, and tumors, as well as a sudorific substance, but it was not until Samuel Hahnemann's studies early in the 19th century that its properties were really understood. Aconite is more closely associated with the rise and progress of homeopathy as a safe alternative to bleeding and purging than any other member of the Materia Medica, but it fell into disrepute until about the middle of the 20th century, when it was employed by Stoerck and given a place in the Pharmacopoeia.[8] In 1805, Hahnemann (1755–1843) published his studies about 27 medicines, including aconite, in a two-volume work entitled: “Fragmenta de Viribus Medicamentorum Positivus”.[9–11] Table 1 in Hahnemann's treatise illustrates the main compounds of Acn, including aconitine. Acn's most active and toxic principle chemical (C34H47N011), in addition to less toxic mesaconitine and hypaconitine, are characterized as steroidal (diterpenoid) alkaloid compounds. Hahnemann and his therapeutic approach transformed this toxic substance into a useful anesthetic and antipyretic compound, used mainly to treat fevers, cardiac conditions and neuralgia.[9]
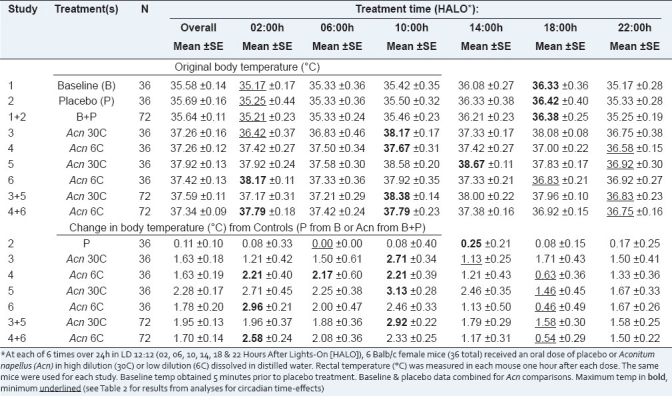
Table 1.
Body temperature timepoint means of mice at baseline and 1h after treatment with placebo or Acn at 6 circadian stages*
Acn is widely used in China, Korea, Japan, India and is gaining acceptance in Europe[4,12] as a quick and short-acting remedy in homeopathic medicine as a topical anesthetic agent to relieve pain, itching and inflammation, and as an internal agent to relieve neuralgic pain and, most commonly, to reduce febrile states associated with colds, pneumonia, laryngitis, croup, and asthma. In conjunction with conventional medicine, it has been reported that 1 day after treatment with Acn 200C, there was a significant reduction in postoperative pain and agitation.[13] In homeopathic therapeutics, Acn is often employed to treat early stages of fever in patients, including children, where it has been employed for control of fever in upper tract infections (URTIs).[14] It has also been demonstrated that there was no difference between response rates for homeopathic remedies (including Acn) versus conventional treatments for acute respiratory and ear complaints in an international multicenter study (57 primary care practices in 8 countries) after 14 days of therapy.[15] Other observational studies on the comparability of homeopathic treatment and conventional treatment of URTIs have also shown positive outcomes for homeopathy.[16,17] A double-blind crossover study in 27 healthy volunteers found a difference in reported responses (short-term signs and symptoms) when treated for 3 days with Acn 30 C versus placebo, indicating that Acn at that dose had a recognizable effect.[18]
Systemic effects of Acn follow within half an hour after its administration and seldom last over 3 hours due to a short duration of action brought about by rapid oxidization. The mode of action of Acn (and related alkaloids) is thought to be due to a depression of the vasomotor center and the cardiotoxicity and neurotoxicity that results from actions on the voltage-sensitive Na+ channels of the cell membranes of excitable tissues, including the myocardium, nerves, and muscles.[1] Symptoms of Acn poisoning can include systemic paralysis, nausea, vomiting, dizziness, palpitations, hypotension, arrhythmia, shock, coma and death.[12] Body temperature (BT) is also lowered, probably by an initial increase in heat dissipation from gastric warmth and a general flush on the body's surface following non-lethal doses.[19] Any time of day related (i.e., circadian) consequences of Acn administration on these effects due to the phenomenon of “chronopharmacology” are unknown.
For centuries, traditional Chinese medicine has incorporated the concept of timing into treatment for a wide variety of ailments,[20] whereby the time and site of a treatment by acupuncture or moxibustion (heat) or a dose of herbs and other medications will differ depending on the natural cycles of the patient, which may involve the time of day, day of the week, day within the menstrual cycle, phase of the moon, and/or season. In the field of biological rhythms (chronobiology), it is now clear that administration of most therapies will result in varying positive or negative effects, depending upon differences in pharmacokinetics of drug disposition resulting from the time of day (i.e., stage of rhythm) of treatment. Therefore, information about biological rhythms can be used to maximize positive and cost-effective outcomes of various interventions. This has far-reaching implications for selecting the best timing of procedures and medications for a wide range of conditions and diseases.[21]
Attempts to time treatment according to biological rhythms in order to achieve the goal of maximizing the desired effect and minimizing undesired effects is known as “chronotherapy”. Chronotherapy includes the best timing of drug treatments, medical and surgical procedures, as well as performance and exercise scheduling. The concept of “chronopharmacology” encompasses the time of drug administration and the body's response according to the underlying temporal structure of the organism receiving it. The concept of “chronopharmacokinetics” adds “time of day” as a variable that influences the pharmacokinetics of a drug. This includes rhythmic changes in drug disposition (absorption, distribution, metabolism, elimination) that result from an interaction in processes at the molecular and membrane levels (pharmacokinetics) and rhythms in the desired and undesired effects (susceptibility).[22–24] Drugs with rhythm-dependent effects include analgesics, anticoagulants, corticosteroids, melatonin, psychobiotics, and anti-hypertensive, anti-ulcer and anti-cancer medications.[22,24,25] Many drugs have been shown to produce less toxicity, better disease control and more cures at some times of the day than others.[26–34] All of these timing concepts most certainly apply to phytomedicine and homeopathy as well.
In order to study the effects of Acn on BT at different times of the day, we studied the rectal temperature of female mice before and after treatment with low and high doses of Acn every 4 hours for 24 hours.
MATERIALS AND METHODS
Animals
In order to study the circadian time-dependent effects of Acn, 36 female BALB/c mice, 10 weeks of age, were obtained from the animal facilities of CINVESTAV–IPN. Six mice were housed in each of six different chambers (three/cage in two plastic cages/chamber) with environmental conditions of 24 ± 3°C and 60 ± 4% humidity with alternating changes of 12-hour light (L) and 12-hour darkness (D). Onset of L was staggered by 4 hours between the six chambers so that after synchronization to the respective LD schedules, study at only one external test time during convenient working hours allowed six different circadian stages (times) to be tested concomitantly (02, 06, 10, 14, 18 and 22 hours after light onset: HALO).[35] This was possible since the local LD schedule synchronizes the body's endogenous biological clock to a 24-hour schedule, thereby setting the peak and trough of the endogenous circadian rhythms to specific times of the environmental day (L) and night (D) spans. Animals were fed with Purina Chow 5010 and sterilized tap water that were renewed every other day when bedding was changed (if a chamber was dark, a red dim room light was used in order to avoid any exposure of white light). These studies were approved by the local Institutional Animal Welfare Committee and were designed to meet the ethical standards of biological rhythm research.[36]
Acn decimal dilutions of Hahnemann
Highly diluted natural complexes of Acn are used as forms of therapy and follow Hahnemann's ancient homeopathic techniques for dilution using a centesimal or C scale that dilutes a substance by a factor of 100 at each stage.[37,38] For example, for a 2C solution, the C scale requires that a substance be diluted to 1 part in 100, and then 10% of that diluted solution diluted by a further factor of 100. This works out to one part of the original substance in 10,000 parts of the solution (10−6). In our case, a “mother” tincture of Acn was purchased from authorized agencies (At Mexico City, Mexico) sanctioned by the Mexican Health Ministry, which assures the quality (endotoxin free) and physicochemical composition of the product. Following Mexican homeopathic regulations and starting from the original mother tincture – an ethanolic extract in this case – several dynamizations/succussion (shaking by forceful striking) and serial dilutions in distilled water were performed to obtain 6th (6C) and 30th (30C) dilutions. (Note: Acn 30C is a common dosage used in homeopathy[18] and there have been no reported adverse effects from homeopathic remedies above 12C.)[39] The final solutions contained A. napellus, all in decimal dilutions of Hahnemann (dH) in distilled water, were colorless and odorless, and had a 1% alcohol concentration. This complex was maintained at room temperature and vigorously shaken (succussed) immediately before each treatment. Placebo (P) consisted of only distilled water and 1% alcohol at room temperature.
Temperature measurement
Rectal temperature (RT) was obtained using an electrical tele-thermometer instrument (Yellow Spring Instrument Co., OH, USA, Model 43TA, SN93D05034) and recorded to the nearest 0.5°C. RT was measured manually for 20 seconds using a plastic probe inserted 3 mm into the rectum of each of the 36 female mice in each of the six studies, resulting in 216 total values (6/mouse).
Study design and treatments
Sampling was staggered across the six chambers over the approximate 1 hour it took to complete all procedures and results were assigned to the midpoint of the total sampling span. Thus, in each study and beginning 30 min before the targeted midpoint, mouse #1 was used from chambers 1 through 6, then the second mouse from each chamber and so on until the sixth mouse per chamber, resulting in six mice from each chamber being studied, which corresponded to one circadian sampling time (target times = 02, 06, 10, 14, 18 and 22 HALO).
After 3 weeks of synchronization to the staggered LD schedules, RT of all mice was measured at baseline or 1 hour after oral treatment with P or a dose of Acn (6C or 30C diluted from original tincture) in six studies: 1) baseline (B), 2) placebo (P), 3) Acn 30C, 4) Acn 6C, 5) Acn 30C, and 6) Acn 6C. Following RT measurement at baseline, each mouse immediately received an oral dose of P and then RT was re-measured after 1 hour. RT was subsequently measured only 1 hour after the oral Acn treatments in the ensuing four experiments. Studies were carried out over a single 8-day span from a Monday to the next Monday in 2005 with a 24-hour span between studies 1 and 2 (Oct 24) and 3 (Oct 25), 3 and 4 (Oct 26), a 48-hour span from 4 to 5 (Oct 28), and a 72-hour span from 5 to 6 (Oct 31). Even though the systemic effects of Acn are short-acting, studies 5 and 6 were designed to monitor the retest effects of Acn after intervals longer than 24 hours between dosing.
Statistical analyses
Following placebo or Acn treatment, the difference in RT for each mouse from the respective timepoint baseline RT was computed. Data from each of the six studies (original RT and change/difference from baseline) were analyzed for time-effect across the six timepoints by one-way analysis of variance (ANOVA) and for circadian rhythm characteristics by the single cosinor procedure[40] by approximation of each time series data by the least-squares linear regression fit of a single component (24-hour) cosine using the Chronolab statistical package.[41] A P-value for the rejection of the zero-amplitude assumption was determined by an F-test of the variance accounted for by the fit of the 24-hour cosine versus the variance accounted for by a straight line approximation of the arithmetic mean. Rhythm detection and/or a time-effect by ANOVA was considered statistically significant if P ≤ 0.05. Rhythm characteristics determined from the best-fitting cosine model include: the “mesor” (M, the middle of the cosine representing an adjusted 24-hour average, which equals the arithmetic mean if sampling is equidistant and there are no missing data or timepoints, as in our study); “amplitude” (A, half the distance from the peak and trough of the best-fitting curve, with 2A indicating the predictable range of change); and the “phase” of the cosine model (Ø, in hh:mm from an external point, such as local midnight or L-onset, as in our case), with the peak of a single component cosine called the “acrophase” (aØ, acro = peak). Rhythm parameters (mesor, amplitude, acrophase) between studies were compared by parameter test.[42]
RESULTS
Timepoint means ± SE for each treatment and study are listed in Table 1 and displayed in Figures 1 and 2. During baseline conditions (B), mice displayed the anticipated circadian variation in their BT, with the highest values found in the middle of the dark/activity span and the lowest values found during the light/resting span [Figure 1]. A significant rhythm in RT was found at B and after P, with no significant differences in rhythm parameters (M = 35.58° vs. 35.69°, Ø = 15:31 hours vs. 15:40 hours) [top rows in Table 2]. Overall timepoint means for B and P values were thus computed to serve as the baseline values for comparison with each Acn series.
Figure 1.
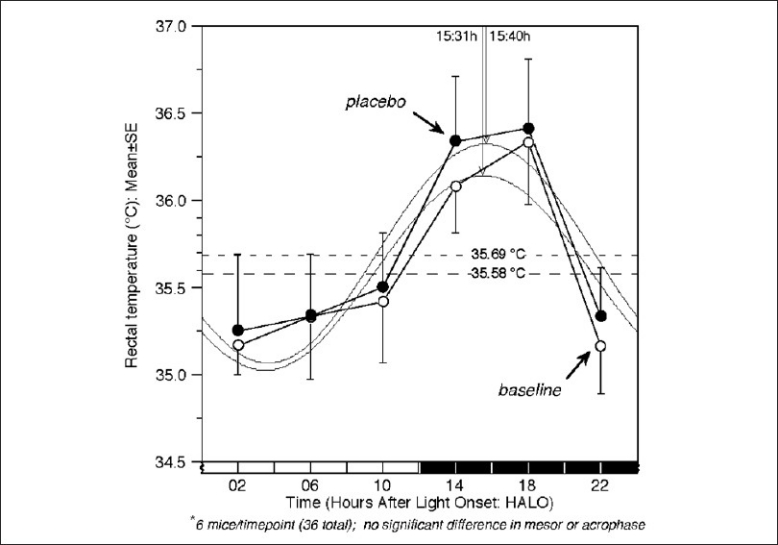
Chronograms showing circadian patterns for mouse body temperature at baseline (B) and 1 hour later after oral placebo (P) at six treatment times [in hours after lights on (HALO, h)]. 4-hour means ± SE from mice studied in LD 12:12 (6 mice/timepoint, 36 total) are shown with best-fitting 24-hour cosine. For time-effect, P-values from fit of a 24-hour cosine were 0.013 for B and 0.017 for P. No significant differences between B versus P were found for 24-hour mean (mesor) (35.58 vs. 35.69°C), amplitude (0.56 vs. 0.63°C), or acrophase (15:31 h vs. 15:40 h), allowing averaging for further comparison following Acn treatments. Dark bar = 12-hour dark/activity span
Figure 2.
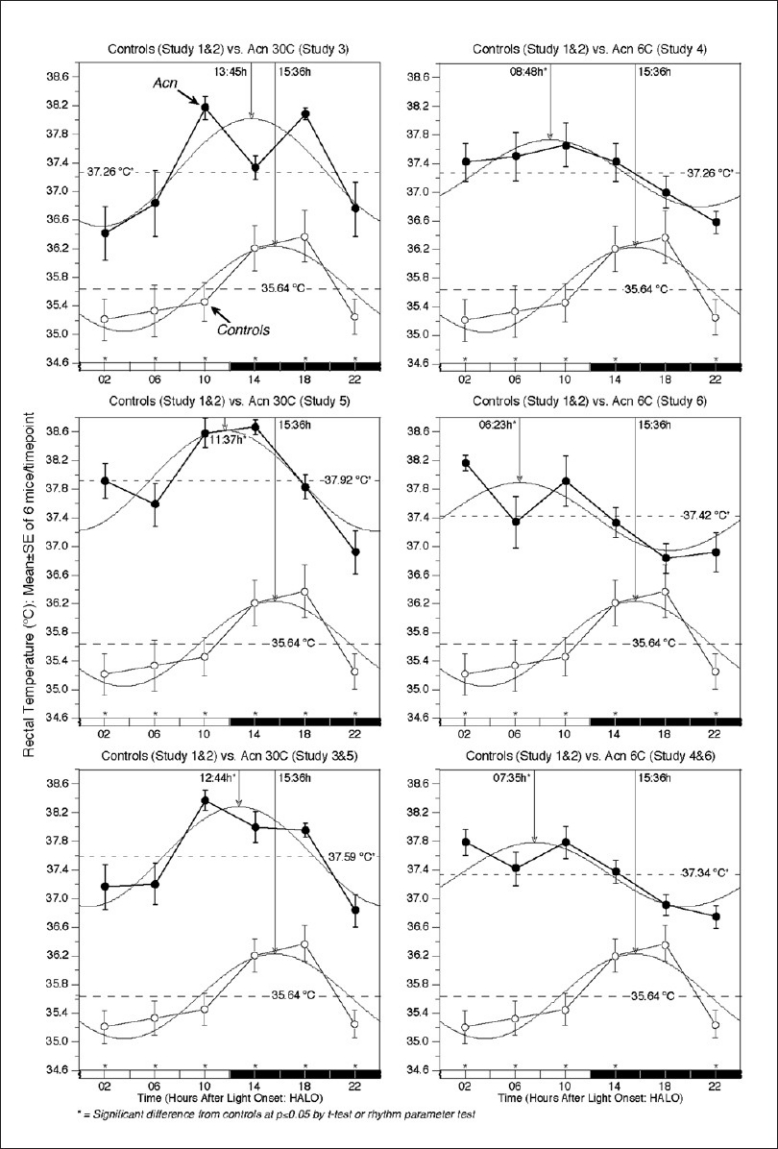
Chronograms showing circadian patterns for mouse body temperature at baseline (B + P) and 1 hour after oral Acn (30C or 6C) at six treatment times [in hours after lights on (HALO)]. 4-hour means ± SE from mice studied in LD 12:12 (6 mice/timepoint, 36 total) are shown with best-fitting 24-hour cosine. For time-effect, the fit of 24-hour cosine was significant at P < 0.05 for each series [see Table 2 for specifics]. An overall hyperthermia was significant following each Acn treatment in studies 3–6 separately or when the two studies of each dose were combined when compared with controls, while calculated acrophases (peaks) were significantly advanced, except for Study 3 (Acn 30C). Dark bar = 12-hour dark/activity span
Table 2.
Statistical evaluation of circadian stage-dependent variations in body temperature of mice treated with Acn*
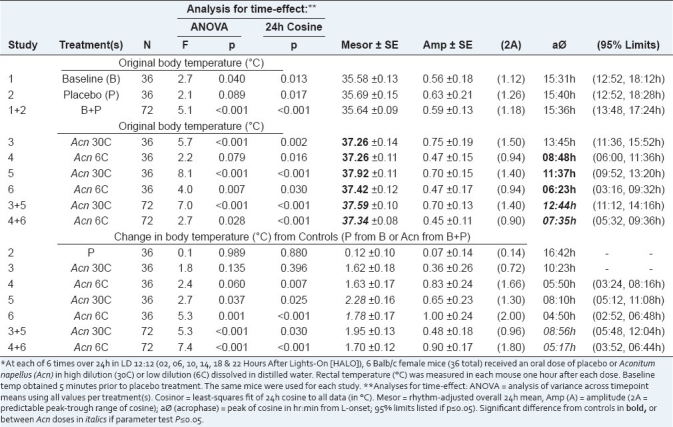
A significant rhythm was found in original RT after all Acn doses in studies 3–6 and overall for 30C in studies 3 and 5 and for 6C in studies 4 and 6, but with highest values shifted to late-L and early-D for 30C and during the L-span for 6C [middle rows in Tables 1 and 2; Figure 2]. Acn induced significant hyperthermia overall compared with B + P after both doses (M = 37.59° for 30C vs. 37.34° for 6C), and at each timepoint, except for 6C at 18 HALO, which increased but not significantly [Figure 2]. The RT Øs following Acn treatment (12:44 hours for 30C vs. 07:35 hours for 6C) were significantly advanced from baseline (15:36 hours) by ~3 hours and 8 hours, respectively, and different from each other by ~5 hours [Table 2; Figure 2].
Timepoint means ± SE for change in RT from baseline following P or Acn treatment in studies 3–6 and combined for 30C from studies 3 and 5 and for 6C from studies 4 and 6 are listed in Table 1 (bottom rows) and changes after Acn are displayed in Figure 3. There were only minor, but nonsignificant changes in baseline RT following P that ranged from 0.0 to +0.25°C [Table 1] and were not rhythmic [Table 2]. The change in BT from baseline was rhythmically significant in studies 4–6 and for each Acn dose overall when the comparable two studies were combined. There was a significant difference between overall means in study 5 carried out after a 48-hour break (Acn 30C, +2.28°) and study 6 carried out after a 72-hour break (Acn 6C, +1.78°) in treatments, but these levels were not significantly different between studies 3 and 4 (+1.62° for 30C vs. +1.63° for 6C) or when both studies for each dose were combined (M = +1.95° for 30C vs. +1.70° for 6C). Overall, the least hyperthermia was observed at 18 HALO following 6C treatment (+1.17°), which was significantly different from 30C (+1.79°) at the same time. Greatest hyperthermia was observed during the L-span for each dose (Ø = 08:56 hours for 30C vs. 05:17 hours for 6C) [bottom rows in Table 2; Figure 3]; these Øs were also significantly different from each other by about 3.75 hours by parameter test.
Figure 3.
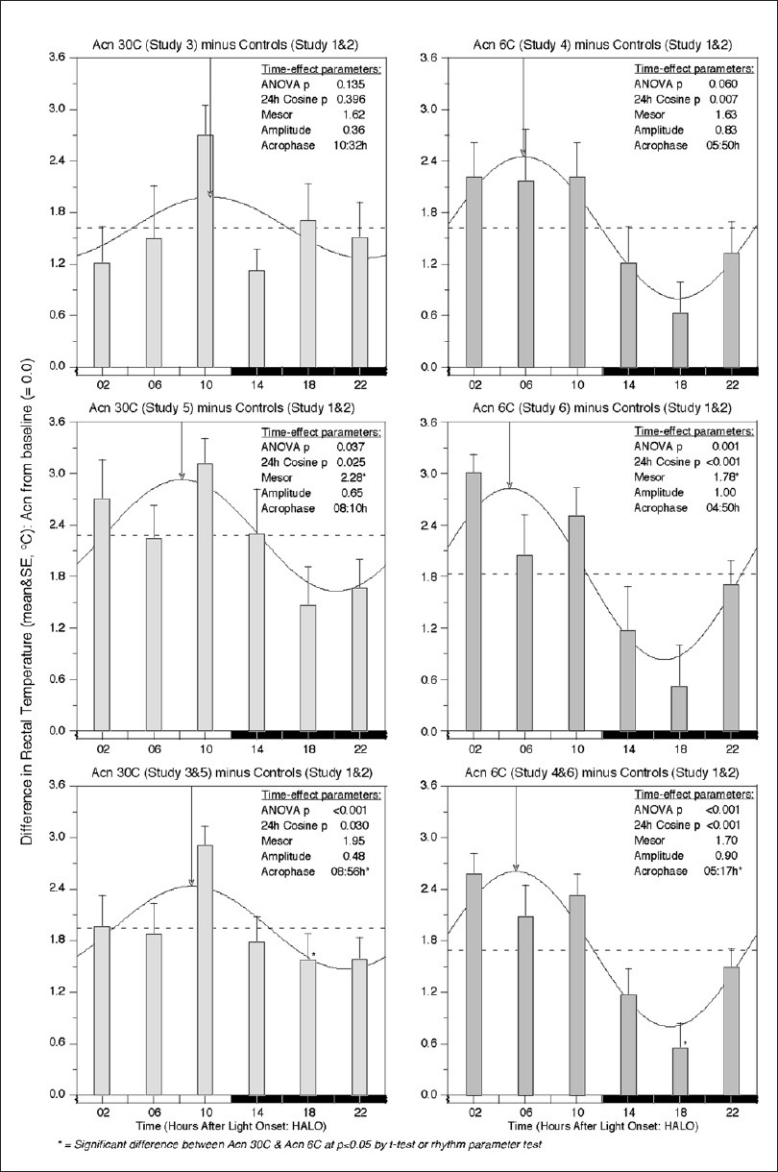
Bar graphs indicating a hyperthermic change from baseline following Acn treatments (30C and 6C) at six different times in four studies and when the two studies of each dose were combined. At each timepoint, body temperature was significantly increased over control values except at 18 HALO for Acn 6C [see Figure 2]. While hyperthermia was noted at each timepoint and after each dose level, maximum hyperthermia was noted during the L-span (resting) for each Acn dose level, while the smallest hyperthermic effects were noted during the D-span (activity) in these nocturnally active mice
DISCUSSION
For centuries, Acn has been used as a poison capable of inducing death – the ancient Greeks called it the Queen of Poisons, the deadliest of all. Single oral doses as low as 1–2 mg have been reported to be lethal in humans.[43–45] Eventually, it was identified as a neurotoxic compound that acts upon nerve hypothalamic centers, as well as on sympathetic peripheral nerves.[12] The cardiotoxicity and neurotoxicity of Acn and related alkaloids result in a combination of neurological, cardiovascular and gastrointestinal symptoms, and in high doses can induce paralysis and death.[1] The precise neurophysiologic mechanism of Acn action is not completely known, but its main and most toxic component, aconitine, which is characterized by a steroidal alkaloid chemical structure, has been studied in the central nervous system of rats at the level of the hippocampus neuronal activity.[46] Specialized neurophysiological research, based on patch-clamp techniques mainly related to the neuron excitability process, has demonstrated that a low physiological Acn dose (10−6 M) affects individual pre-synaptic rat neuron excitability by opening Na+ channels.[47]
Used as a homeopathic agent at very low doses (e.g., 6C and 30C), Acn has shown analgesic and anti-inflammatory properties. According to homeopathic theory, it was expected that low doses of Acn would induce hypothermia in the BT of female mice. However, when we administered two different oral doses of Acn to mice at six times around the clock on four occasions (each dose studied twice), the opposite effect was observed 60 min after treatment: each dose induced hyperthermia overall, but in a rhythmic, time-dependent manner, with the greatest effects during the resting (L) span after 30C and late-L to early-D (dark/activity) span after 6C [Figure 2]. This is not inconsistent, however, with the Eclectic Materia Medica description of an ultimate lowering of body temperature following an increase in heat dissipation from gastric warmth and a flush on the body's surface shortly after Acn treatment.[19] Also, from an allopathic point of view, one would expect that the extremely low dose of Acn 30C would not have any effect on mouse BT, but the hyperthermia that was observed was more or less comparable to that noted when mice were treated with the higher dose of Acn 6C (overall RT changes: 30C, +1.95 ± 0.13° vs. 6C, +1.70 ± 0.14°, n.s.) [Table 2].
The oral gavage procedure itself could not be responsible for the hyperthermia observed since the delivery of placebo (i.e., water and 1% ethanol) by the same method induced modest, but nonsignificant increases in RT from baseline overall (means: B, 35.58 ± 0.14° vs. P, 35.69 ± 0.16°, n.s.) [Table 1] and at some timepoints and not others (e.g., +0.0° at 06 HALO vs. +0.25° at 14 HALO) [Table 2]. No significant time-effects or 24-hour rhythm was found in the B to P changes, which were all substantially smaller than those induced by either of the Acn doses at the same circadian timepoints. Moreover, there were no significant differences between the rhythmic temperature parameters (M, A, Ø) in baseline versus placebo-treated mice [Table 2]. Therefore, we chose to incorporate the minor P-effects (possibly due to handling and/or the fact that RT after P was measured 1 hour after B measurements and minor changes could be due to the time course of the underlying circadian rhythm in BT) by averaging the B + P data for use as baseline RT data when computing changes from RT following Acn dosings.
Any influence on overall BT changes due to the 4–5 day estrus cycle of female mice were thought to be minimal in affecting the BT response to Acn dosing since the mice were dispersed over six separate boxes and would not be socially synchronized as a group by smell or sound. Nevertheless, it would be of interest in any future study to test male mice, as well as measure RT before as well as after 1 hour following each Acn treatment on each study day in order to obtain separate study baseline values (that may reflect effects of repeated handling and/or daily changes in BT due to estrus cycle changes), rather than rely on only the temperature values obtained at the beginning of the entire study prior to any treatment.
In order to study the chronic physiologic effects of administration on body weight (BW) and RT changes in mice, a recent investigation treated male mice intragastrically daily with Acn (1 mg/kg/day) for 22 days and measured BW and RT on days 0, 1, 3, and every 4 days thereafter to day 22.[48] Acn-treated mice showed virtually no BW gain over the 22-day study when compared with placebo-treated controls and day 0. However, when RT was measured at 10-min intervals for 90 min following each Acn treatment, a transient hypothermia was noted to occur within the first 30 min of dosing, followed by a gradual increase to the end of the 90 min observation span. The extent and duration of hypothermia lessened throughout the study such that on study day 11 and thereafter, RT had always returned to its pretreatment level or higher by 60–90 min. The authors concluded that long-term administration of Acn suppresses hypothermia and ultimately warms the body.
Another recent study of male mice exposed to room temperature of 4°C for 10 days to induce chronic cold stress reached the same conclusion when BW and RT were measured every 2 days.[49] Core BT in untreated mice was significantly decreased by about 1°C by day 5 of the cold exposure when compared with mice maintained at normal room temperature (24°C). However, in mice receiving Acn added to a standard murine powdered chow available ad libitum, the BT reduction was significantly counteracted in a dose-dependent manner (0.063, 0.25 and 1.0 g/kg/day were tested) such that there was no significant difference for any dose on any treatment day from the normal mice (the Acn 1.0 g dose actually showed significantly higher BT than normal controls on days 5, 7 and 9 after cold initiation). BW gain tended to be lower in the Acn-treated mice compared with room temperature controls, but there was no difference between cold-stressed controls and Acn-treated mice. Since the Acn treatment did not increase core BT in mice under normal room temperature conditions, the authors concluded that Acn did not directly stimulate thermogenesis, but rather facilitated a non-shivering physiological thermoregulation that occurs in brown adipose tissue, wherein the heat is produced through the metabolism of free fatty acids in the mitochondria.
Of note, the procedures in the two studies mentioned above appear to have been undertaken only once daily at a time(s) which may have been convenient to the researchers. In the study by Wada et al.,[48] there is no mention of the LD schedule for the mice or the time of day of Acn dosing and RT measurements. Assuming that the mice were kept in dark at night and with lights on during the day, the study was most likely carried out in the morning (e.g., between 08:00 and 12:00 hours or 02–06 HALO). In the study by Makino et al.,[49] they reported that the mice were housed under a 12-hour L–12 hour D schedule with L-on from 07:00 to 19:00 hours and BT was measured between 13:00 and 15:00 hours, which would be in the middle of the daily resting span (06–09 HALO). Both of these studies were thus carried out at only one of the six different circadian times that we used in our study in order to consider the well-known circadian variation in mouse body temperature (i.e., BT reaches its minima during mid-L and maxima during mid-D). Thus, for proper comparison to the human sleep–wake schedule, an extrapolation of the 22-day study mouse protocol of Wada and the 10-day study protocol of Makino would require similar treatment(s) during rest/sleep (i.e., at night after sleep onset).
CONCLUSION
Acn administered in two different doses (6C and 30C) to healthy mice at six times 4 hours apart over 24 hours each induced hyperthermia overall and in a significant time-dependent (i.e., circadian) manner, with greater effects during the resting (L) span in nocturnally active mice. These results suggest that time of day may significantly impact the outcome of not only Acn, but also other homeopathic treatments used in the field of pharmacognosy. A chronobiologic approach that considers timing presents a new perspective for exploring the temporal mechanisms of action(s) by Acn and other homeopathic compounds in relation to mitochondrial and genetic involvement in thermal regulation at the level of hypothalamic centers, as well as their affect on neuroendocrine-immune network interactions.[50] With regard to homeopathic treatments, the concept of “chronotherapy” should be considered in determining optimal dosing and time of treatment(s) in order to increase the desired outcome and decrease the undesired effects of homeopathic procedures. At the very least, time(s) of treatment(s) should be recorded and reported for any future comparisons.
ACKNOWLEDGMENTS
Grant support of the ICyT-DF, No. PICD08-82 and IML and SIP-IPN No. 20101632 to the principal author (SSP) is acknowledged. SSP is also grateful to the fellowship programs of de Estímulos al Desarrollo de Investigación (EDI) of the Instituto Politécnico Nacional (IPN), Mexico. JWB and IML would like to acknowledge grants conferred by the Comisión de Operación y Fomento de Actividades Académicas (COFAA) and Programa de Estímulos al Desarrollo Docente del IPN, Mexico.
All plastic cages, bottles and taps were kindly supplied by Dr. Eduardo Tena, Director of Bioterio Central Facilities at the del CMN Siglo XXI. Purina Chow 5010 was kindly provided by Fundación de Investigación Crono Oncológica A.C.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Chan TY. Aconite poisoning. Clin Toxicol (Phila) 2009;47:279–85. doi: 10.1080/15563650902904407. [DOI] [PubMed] [Google Scholar]
- 2.Facts and Comparisons 4.0. St Louis, MO: Wolters Kluwer Health, Inc; 2009. Jul, [last accessed on 2010 Jul 3]. Aconite. Review of Natural Products. Available from: http://www.drugs.com/npc/aconite.html#ixzz118RjCfVi . [Google Scholar]
- 3.Bisset NG. Arrow poisons in China. Part II. Aconitum-botany, chemistry, and pharmacology. J Ethnopharmacol. 1981;4:247–336. doi: 10.1016/0378-8741(81)90001-5. [DOI] [PubMed] [Google Scholar]
- 4.Bisset NG. One man's poison, another man's medicine? J Ethnopharmacol. 1991;32:71–81. doi: 10.1016/0378-8741(91)90105-m. [DOI] [PubMed] [Google Scholar]
- 5.Skaltsa H, Philianos S, Papaphilippou G. The Aconitine described by Nicander and today. Rev Hist Pharm (Paris) 1997;45:405–10. [PubMed] [Google Scholar]
- 6.Singhuber J, Zhu M, Prinz S, Kopp B. Aconitum in traditional Chinese medicine: A valuable drug or an unpredictable risk? J Ethnopharmacol. 2009;126:18–30. doi: 10.1016/j.jep.2009.07.031. [DOI] [PubMed] [Google Scholar]
- 7.Chu NS. Legendary Hwa Tuo's surgery under general anesthesia in the second century China. Acta Neurol Taiwan. 2004;13:211–6. [PubMed] [Google Scholar]
- 8.The Pharmacopoeia of the United States. Falls Church, Virginia. USA: American Institute of Homoeopathy; 1979. American Institute of Homoeopathy. [Google Scholar]
- 9.Gotfredsen E. The incomplete reference-guide to Herbal medicine. Liber Herbarum II. [last accessed on 2010 Jul 3]. Available from: http://www.liberherbarum.com/kilde026.htm .
- 10.Clarke HJ. A Dictionary of Practical Materia Medica. [last accessed on 2010 Jul 3]. Available from: http://www.farmaciasantantonio.it/Homeoint/clarke/a/acon.htm .
- 11.Duke AJ. Dr. Duke's Phytochemical and Ethnobotanical Databases. [last accessed on 2010 Jul 3]. Available from: http://www.ars-grin.gov/cgi-bin/duke/farmacy2.pl .
- 12.Ameri A. The effects of Aconitum alkaloids on the central nervous system. Prog Neurobiol. 1998;56:211–35. doi: 10.1016/s0301-0082(98)00037-9. [DOI] [PubMed] [Google Scholar]
- 13.Oberbaum M, Scheiber R, Rosenthal C, Itzchaki M. Homeopathic treatment in emergency medicine: A case series. Homeopathy. 2003;92:44–7. doi: 10.1054/homp.2002.0071. [DOI] [PubMed] [Google Scholar]
- 14.Steinsbekk A, Lewith G, Fønnebø V, Bentzen N. An exploratory study of the contextual effect of homeopathic care. A randomised controlled trial of homeopathic care vs. self-prescribed homeopathic medicine in the prevention of upper respiratory tract infections in children. Prev Med. 2007;45:274–9. doi: 10.1016/j.ypmed.2007.02.004. discussion 280-1. [DOI] [PubMed] [Google Scholar]
- 15.Haidvogl M, Riley DS, Heder M, Brien S, Jong M, Fischer M, et al. Homeopathic and conventional treatment for acute respiratory and ear complaints: A comparative study on outcome in the primary care setting. BMC Complement Altern Med. 2007;7:7. doi: 10.1186/1472-6882-7-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Trichard M, Chaufferin G, Nicoloyannis N. Pharmacoeconomic comparison between homeopathic and antibiotic treatment strategies in recurrent rhinopharyngitis in children. Homeopathy. 2005;94:3–9. doi: 10.1016/j.homp.2004.11.021. [DOI] [PubMed] [Google Scholar]
- 17.Friese KH, Kruse F, Lüdtke R, Möller H. The homeopathic treatment of otitis media in children- comparisons with conventional therapy. Int J Clin Pharmacol Ther. 1997;35:296–301. [PubMed] [Google Scholar]
- 18.Piltan D, Rist L, Simões-Wüst P, Saller R. Test of a homeopathic dilution of Aconitum napellus.A clinical, randomized, double-blind, controlled crossover study in healthy volunteers. Forsch Komplementmed. 2009;16:168–73. doi: 10.1159/000219316. [DOI] [PubMed] [Google Scholar]
- 19.Felter HW. Cincinnati, OH: Eclectic Medical Publications; 1992. PART II - Individual Drugs. Aconitum Napellus. The Eclectic Materia Medica, Pharmacology and Therapeutics; pp. 4–13. [Google Scholar]
- 20.Wu J. Neijing chronobiologic medical theories. Chin Med J. 1982;95:569–78. [PubMed] [Google Scholar]
- 21.Sothern RB. Hours of changing resistance. In: Koukkari WL, Sothern RB, editors. Introducing Biological Rhythms. A primer on the temporal organization of life, with implications for health, society, reproduction and the natural environment. New York: Springer; 2006. pp. 470–80. [Google Scholar]
- 22.Reinberg A, Smolensky M. Circadian changes in drug disposition in man. Clin Pharmacokinet. 1982;7:401–20. doi: 10.2165/00003088-198207050-00002. [DOI] [PubMed] [Google Scholar]
- 23.Ritschel WA, Forusz H. Chronopharmacology: A review of drugs studied. Methods Find Exp Clin Pharmacol. 1994;16:57–75. [PubMed] [Google Scholar]
- 24.Bruguerolle B. Chronopharmacokinetics. Current status. Clin Pharmacokinet. 1998;35:83–94. doi: 10.2165/00003088-199835020-00001. [DOI] [PubMed] [Google Scholar]
- 25.Smolensky MH, Haus E. Circadian rhythms and clinical medicine with applications to hypertension. Am J Hypertens. 2001;14:280S–90. doi: 10.1016/s0895-7061(01)02175-6. [DOI] [PubMed] [Google Scholar]
- 26.Reinberg A, Smolensky M. New York: Springer-Verlag; 1983. Biological Rhythms and Medicine. Cellular, Metabolic, Physiopathologic, and Pharmacologic Aspects; p. 305. [Google Scholar]
- 27.Rivard GE, Infante-Rivard C, Hoyeux C, Champagne J. Maintenance chemotherapy for childhood acute lymphoblastic leukemia: Better in the evening. Lancet. 1985;2:1264–6. doi: 10.1016/s0140-6736(85)91551-x. [DOI] [PubMed] [Google Scholar]
- 28.Rivard GE, Infante-Rivard C, Dresse MF, Leclerc JM, Champagne J. Circadian time-dependent response of childhood lymphoblastic leukemia to chemotherapy: A long-term follow-up study of survival. Chronobiol Int. 1993;10:201–4. doi: 10.3109/07420529309073888. [DOI] [PubMed] [Google Scholar]
- 29.Lemmer B, editor. New York: Marcel Dekker; 1989. Chronopharmacology: Cellular and Biochemical Interactions; p. 720. [Google Scholar]
- 30.Labrecque G, Bélanger PM. Biological rhythms in the absorption, distribution, metabolism and excretion of drugs. Pharmacol Ther. 1991;52:95–107. doi: 10.1016/0163-7258(91)90088-4. [DOI] [PubMed] [Google Scholar]
- 31.Redfern PH, Lemmer B, editors. Berlin: Springer-Verlag; 1997. Physiology and Pharmacology of Biological Rhythms; p. 668. [Google Scholar]
- 32.Sothern RB. Examples of applied chronotherapy. In: Koukkari WL, Sothern RB, editors. Introducing Biological Rhythms. A primer on the temporal organization of life, with implications for health, society, reproduction and the natural environment. New York: Springer; 2006. pp. 480–6. [Google Scholar]
- 33.Smolensky MH, Hermida RC, Ayala DE, Tiseo R, Portaluppi F. Administration-time-dependent effects of blood pressure-lowering medications: Basis for the chronotherapy of hypertension. Blood Press Monit. 2010;15:173–80. doi: 10.1097/MBP.0b013e32833c7308. [DOI] [PubMed] [Google Scholar]
- 34.Hermida RC, Ayala DE, Mojón A, Fernández JR. Influence of circadian time of hypertension treatment on cardiovascular risk: Results of the MAPEC study. Chronobiol Int. 2010;27:1629–51. doi: 10.3109/07420528.2010.510230. [DOI] [PubMed] [Google Scholar]
- 35.Sothern RB. Time of day versus internal circadian timing references. J Infus Chemother. 1995;5:24–30. [PubMed] [Google Scholar]
- 36.Portaluppi F, Touitou Y, Smolensky MH. Ethical and methodological standards for laboratory and medical biological rhythm research. Chronobiol Int. 2008;25:999–1016. doi: 10.1080/07420520802544530. [DOI] [PubMed] [Google Scholar]
- 37.Hahnemann S. The Organon of Medicine. In: Kunzli J, Naude A, Pendleton P, translators. 6th ed. 1982. p. 277. 1921 modern English. [Google Scholar]
- 38.Cook T. UK: Thorsons; 1981. Samuel Hahnemann, the Founder of Homeopathy. [Google Scholar]
- 39.La Pine MP, Malcomson FN, Torrance JM, Marsh NV. Night shift: Can a homeopathic remedy alleviate shift lag? Dimens Crit Care Nurs. 2006;25:130–6. doi: 10.1097/00003465-200605000-00015. [DOI] [PubMed] [Google Scholar]
- 40.Nelson W, Tong YL, Lee JK, Halberg F. Methods for cosinor rhythmometry. Chronobiologia. 1979;6:305–23. [PubMed] [Google Scholar]
- 41.Mojón A, Fernández JR, Hermida R. Chronolab: An interactive software package for chronobiologic time series analysis written for the Macintosh computer. Chronobiol Int. 1992;9:403–12. doi: 10.3109/07420529209064552. [DOI] [PubMed] [Google Scholar]
- 42.Bingham C, Arbogast B, Cornélissen GC, Lee JK, Halberg F. Inferential statistical methods for estimating and comparing cosinor parameters. Chronobiologia. 1982;9:397–439. [PubMed] [Google Scholar]
- 43.Camps FE. 2nd ed. Bristol: John Wright and Sons; 1968. Gradwohl's Legal Medicine; p. 674. [Google Scholar]
- 44.Rentoul E, Smith H. Edinburgh, Scotland: Churchill Livingstone; 1973. Glatier's Medical Jurisprudence and Toxicology; pp. 520–1. [Google Scholar]
- 45.Singh S, Fadnis PP, Sharma BK. Aconite poisoning. J Assoc Physicians India. 1986;34:825–6. [PubMed] [Google Scholar]
- 46.Ameri A. Structure-dependent inhibitory action of the Aconitum alkaloids 14-benzoyltalitasamine and talitasamine in rat hippocampal slices. Naunyn Schmiedebergs Arch Pharmacol. 1998;357:585–92. doi: 10.1007/pl00005212. [DOI] [PubMed] [Google Scholar]
- 47.Yamanaka H, Doi A, Ishibashi H, Akaike N. Aconitine facilitates spontaneous transmitter release at rat ventromedial hypothalamic neurons. Br J Pharmacol. 2002;135:816–22. doi: 10.1038/sj.bjp.0704517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wada K, Nuhira M, Ohno Y. Effects of chronic administrations of aconitine on body weight and rectal temperature in mice. J Ethnopharmacol. 2006;105:89–94. doi: 10.1016/j.jep.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 49.Makino T, Kato K, Mizukami H. Processed aconite root prevents cold-stress-induced hypothermia and immuno-suppression in mice. Biol Pharm Bull. 2009;32:1741–8. doi: 10.1248/bpb.32.1741. [DOI] [PubMed] [Google Scholar]
- 50.Sánchez de la Peña S. The feedsideward of cephalo-adrenal immune interactions. Chronobiologia. 1993;20:1–52. [PubMed] [Google Scholar]


