Abstract
Aim:
The long term outcomes of congenital hydrocephalus are still not clearly known despite it being a common clinical condition. Several clinical, radiological factors were correlated to predict the functional outcomes. This study aimed to correlate the clinical, radiological parameters with the regional functional outcomes of the brain.
Materials and Methods:
Children with congenital hydrocephalus were divided into Group A with hydrocephalus alone and Group B hydrocephalus with spina bifida. Ventriculoperitoneal shunt surgery was performed by the same surgeon. CT scans and neuropsychological assessments were performed before and serially after the shunt. The clinical and the radiological findings were correlated with the developmental levels during the follow-up.
Results:
There were 25 children in Group A and 15 children in Group B; 72% in Group A and 93% in Group B were less than 6 months of age at the time of treatment. Forty percent in Group A and 92% in Group B had the signs of hydrocephalus at admission. Cerebrospinal fluid (CSF) diversion results in the reduction in ventricular dilatation and corresponding increase in the cortical mantle thickness. The ventricular size and the cortical mantle thickness were measured serially and correlated with the development in the neuropsychological function. In this study, 80% in Group B reached near normal development in comparison to 33% in Group A. We have noticed a significant correlation in the increase in the regional cortical mantle thickness with corresponding improvement in the functional development. This clearly ratifies the improvement in the frontal and parietal areas having their distinctive effect on the functional development of the child.
Conclusion:
Early CSF diversion and timely intervention seems to benefit functional recovery. It is interesting to note that reconstitution of cortical mantle in different areas of the brain showing corresponding improvement in their respective areas. Large ventricles (head circumference more than 50 cm) recurrent subdural collections and repeated shunt obstructions have a bad influence on the long-term outcome. Unlike the previous belief the children with myelomeningocele can have equal benefit in terms of neuropsychological development after the shunt surgery.
Keywords: Congenital hydrocephalus, functional outcome, myelomeningocele, neuropsychological development
Introduction
Congenital hydrocephalus is one of the common conditions in paediatric neurosurgical practice characterized by abnormal dilatation of cerebral ventricular system. The incidence of congenital hydrocephalus varies from 0.92.9/1000 births. Increased ventricular volume due to accumulation of cerebrospinal fluid (CSF) results in increased intraventricular pressure. This causes corresponding compression on the surrounding cerebral parenchyma, leading to structural changes in white matter, cortex, and seepage of CSF into the periventricular spaces through ependymal tears.
Congenital hydrocephalus can occur in association with a number of developmental anomalies of brain and spinal cord. Hydrocephalus with an elevated intracranial pressure can lead to deterioration in motor, intellectual, cognitive, and other neuropsychological functions.
Therapy for hydrocephalus includes diversion of CSF or endoscopic ventriculostomy. Although shunts have greater propensity to reduce ventricular volumes on imaging, its efficacy in reversing the pathophysiological changes and its effect on functional and intellectual outcomes are variable. Similarly the precise role of anatomical reconstitution of cortical mantle following therapy in restoring normal functions needs to be studied.
Materials and Methods
Many studies have been published concerning the intelligence of hydrocephalic children.[1–15] They include both treated and untreated groups. Most studies have been purely descriptive and only a few have compared the treated and untreated groups. The determinants of intelligence level in hydrocephalic children are not fully established and the pattern of intelligence is also imperfectly understood.
It is very difficult to evaluate the literature regarding intellectual function in children with treated group of congenital hydrocephalus. The diagnostic criteria used were different in different studies. It is also difficult to compare different studies due to lack of adequate information, use of different methods of intelligence quotient assessment, different methods of data presentation, lack of proper definition of “Normal,” or the basis of sample selection.
This study includes children with congenital hydrocephalus who were surgically treated by ventriculoperitoneal shunt. Children with possible infections and multiloculated ventricles were excluded. Age, sex, economic status, intrapartum events, and associated congenital anomalies were not considered in the selection of sample.
Forty such children were divided into Group A—congenital hydrocephalus (N = 25) alone and Group B—hydrocephalus with myelomeingocoele (N = 15).
All children underwent elective ventriculoperitoneal shunts (Indian) using medium pressure valve. In Group B, shunt was performed first in 14 children, which was followed-up by the repair of myelomeningocoele. Clinical, radiological, and neuropsychological assessment was done before surgery, at discharge, and during follow-up at 3–6 month intervals. Preoperative assessments were taken as baseline.
Computed tomography (CT) scans repeated at intervals, ranging from 3 to 6 months to ensure that the shunt was functioning. Additional scans were performed in case of shunt malfunction and they were revised appropriately. Totally 9 children required revision of shunts—5 in Group A and 4 in Group B.
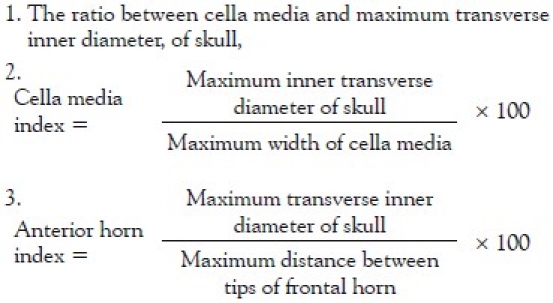
Linear measurements were used to assess the degree of ventricular dilatation and cortical mantle thickness. A scale in which 1 cm was divided into 20 equal parts was used to achieve an accuracy of 0.5 mm. The measurements include bifrontal diameter, absolute III ventricular diameter, the minimum width of the body of the lateral ventricle (cella media), and the maximum transverse inner diameter of the skull. From these measurements, the following indices (68) were calculated.
Cortical measurements were taken in frontal and parietal areas on both right and left sides. Frontal cortex was measured from tip of the corresponding frontal horn to the inner table in the sagittal plane and parietal cortex as the maximum diameter from ventricle to inner table in the coronal plane. Temporal and occipital cortices were not measured due to the variations of the size and shape of the temporal and occipital horns. The measured readings were multiplied by 3.5, the magnification factor for the design of the scanner used.
Postoperatively, corresponding cuts were used in the assessment of reduction in ventricular size and to measure the cortical thickness. In 10 patients ventricles were collapsed and postoperative measurements could not be done. These were labeled as “Slit ventricles.” Apart from this, postoperative subdural collections, and other complications were taken into cognizance in the final analysis.
Psychological assessment
Psychological development was assessed either by Gesell developmental schedules[16] or Bayley scales of infant development.[17,18] The Gesell developmental schedules were developed based on a series of longitudinal studies of the normal course of behavioral development in infants and preschool children. The schedules cover major areas of behavioral development, namely, motor, adaptive, language, personal, and social development. It involves a standardized procedure of observing and evaluating the various elements of behavior in the child. It includes tests, as well as observations of the child. These schedules are applicable for children from the age of 4 months to 6 years. Although the tests greatly depend on observational findings, a high examiner reliability of over 0.95 was reported.[7]
Bayley scales of infant development
This is a developmental schedule exceptionally suited for infants. The scale covers mental development up to 2 years and 6 months. As in the case of the Gesell developmental schedules, the Bayley scales are the outcome of continuous and longitudinal studies by Bayley and other co-workers. It has also incorporated the findings of Berkeley growth study. The Bayley scales provide three complimentary tools for assessing the developmental status of children between the ages of 2 months and 2½ years. The mental scale assesses functions, such as perceptions memory, learning, problem solving vocalization, and visual communication. It may be kept in mind that only the elementary aspects of these functions could be observed and assessed during the very early ages. Another component of the schedule is the motor scale, which measures the motor abilities, such as sitting, standing, walking, and so on. The scales provide the normal age range for the occurrence of each event during the developmental process. The third component of the test helps to measure essentially the emotional, personality development, and social behavior of the child. The Bayley scales are considered to be the most reliable and outstanding tool for assessing developmental processes in the infants. The normative data of these scales were established based on observation of 1262 children. During standardization procedure, the test has yielded reliability co-efficient of 0.81–0.93 in separate age groups.
The choice of the test depends on the age of the patient investigated initially. The child was observed for the period ranging from 1 to 2 h and later the parents were interviewed in detail. The developmental age of the child was derived from either of the two tests used, on eight of the tests the child was tested and observed to determine if the child would pass an individual item related to a specific age level. The maximum age level that could be reached on the developmental schedules in each child was considered his mental age.
The tests were administered both preoperatively and postoperatively. However, considerable caution was exercised in the preoperative assessment, in avoiding errors caused by the clinical condition of the child due to hydrocephalus.
Since the patients were infants or children in the very early ages, emphasis was laid on ascertaining their developmental levels rather than intelligent quotients. Although the mental age could be easily connected into an intellectual quotient (IQ) measure, it was considered more meaningful to use the criterion of mental age rather than that of IQ as the nature of the disease entity can produce a cluster of different functions. Although deriving an IQ will average out these discrepancies, the actual/developmental pattern of the child would be lost.
An attempt was made to find the association between the developmental age of the child and (different clinical findings such as) clinical and radiological parameters, both preoperatively and postoperatively. From these comparisons, an attempt was made to determine the developmental rate in the child after the shunt. Prognostic factors, the predictability of the future development and intellectual outcome based on the initial assessment were attempted for each child.
Results
Forty children who underwent ventriculoperitoneal shunts for congenital hydrocephalus were studied. They were divided into two groups. Group A with hydrocephalus alone and Group B with an associated myelomeningocele.
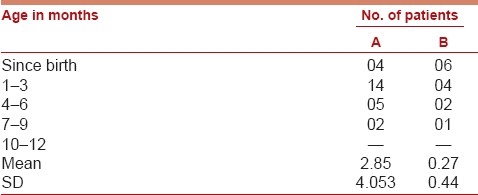
The results of both the groups with respect to each investigation were analyzed. The postoperative neurological improvement was correlated with radiological and psychological findings. Age and sex distribution is shown in Table 1a and 1b.
Table 1a.
Distribution of sample
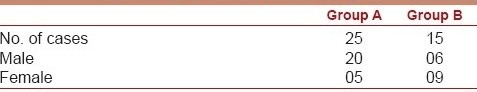
Table 1b.
Age distribution
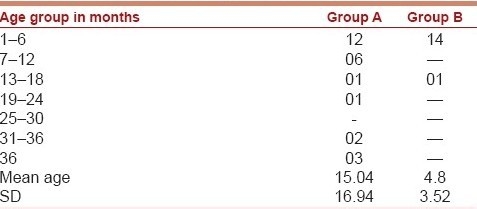
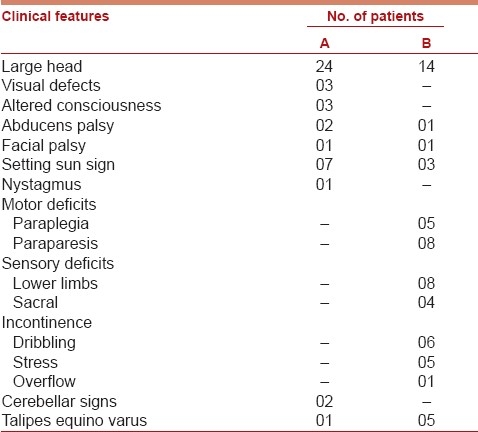
Progressive increase in head size was the most common symptom in both the groups. Four children (16%) of Group A had gross delay in milestones at the time of admission. In Group A, 6 patients (24%) had symptoms of increased intracranial tension and 3 (12%) had preoperative seizures. In two children, big head was noticed from birth [Table 2].
Table 2.
Clinical features
The onset of clinical symptoms of hydrocephalus was quite early in both the groups. Progressive increase in head circumference was noticed from birth in 16% of cases in Group A and 40% of cases in Group B. They were presented to our service with established disease in 92% of Group A and 93.2% of Group B. The mean ages of onset of symptoms were 2.85 months for Group A and 0.27 months for Group B [Table 3].
Table 3.
Age of onset of symptoms
Three children in Group A were drowsy at the time of admission and another 3 patients had impaired visual development. Most common cranial nerve deficit was sixth nerve palsy and lower motor neuron type of facial paresis, was noticed in 2 children, one in each group. Nystagmus and cerebellar signs were seen only in 2 children of Group A [Table 4].
Table 4.
Clinical features
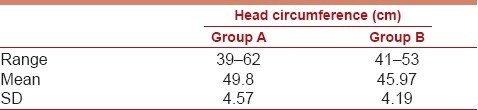
In Group B the location of myelomeningocele sac was lumbar in 6 (39.6), thoraco lumbar in 5 (33%), lumbosacral in 2, and thoracic and sacral in one each [Table 5]. They had corresponding neurological deficits below the level of the myelomeningocele. Thirteen children had complete weakness of lower limbs and paraparesis in 8. Twelve had urinary sphincter disturbance. Head circumference of these children varies from 39 to 62 cm in Group A and 41–53 cm in Group B with a mean value of 49.8 and 45.97, respectively [Table 6].
Table 5.
Group B
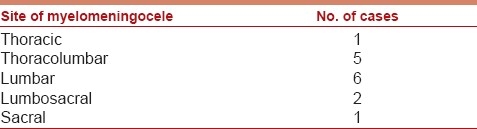
Table 6.
Head circumference
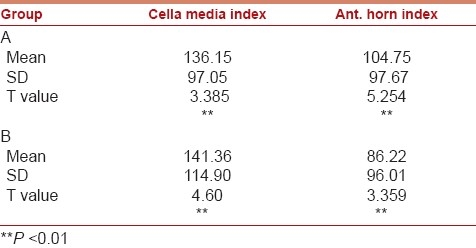
The cell media index and anterior horn index and absolute 3rd ventricular diameter were calculated in all these patients both preoperatively and postoperatively. There was a significant improvement of these indices toward normalcy in all the children (P < 0.01) after the shunt [Tables 7 and 8].
Table 7.
Ventricular measurement after shunt
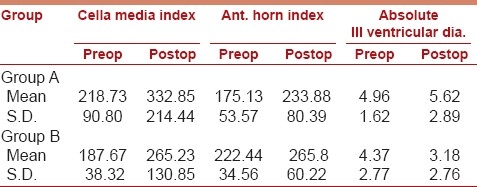
Table 8.
Postoperative ventricular indices on followup
In 10 patients (6 in Group A and 4 in Group B) the ventricles became SLIT and hence postoperative ventricular measurements could not be measured accurately.
The cortical mantle thickness varied with the degree of ventricular dilatation. In 8 patients the cortex was severely thinned out so that no measurement of cortical mantle is possible. The mean cortical mantle thickness in the frontal and parietal region is mentioned in Table 9.
Table 9.
Measurements of cortical mantle
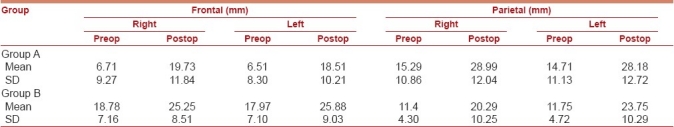
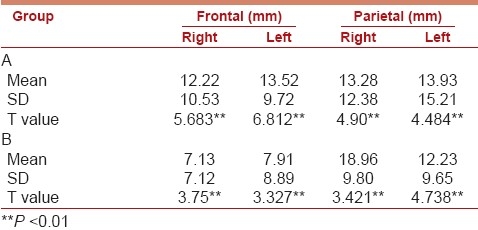
Mean duration of 5.25 months in Group A and 5.99 months in Group B. The increase in thickness of cortical mantle observed in the last scan was statistically significant, P < 0.01 [Table 10]. In 19 out of 40 cases the cortical mantle thickness was greater than 3 cm. There seems to be regional variation in cortical mantle reconstitution after surgery.
Table 10.
Improvement in the cortical mantle (postshunt)
Among those with almost invisible cortical mantle, preoperatively only one had shown improvement in cortical mantle and the rest did not show improvement in thickness.
Psychological assessment
Among the 40 children, Gesell developmental schedules could be successfully administered in 36 children. The following relationships were determined between demographic, clinical, neuroradiological, and psychological development in each group.
Association between pre- and postoperative interval and change in the functional levels of motor, language, social, and adaptive areas.
Correlation between the differences between pre- and postoperative cella media index, anterior horn index, and absolute 3rd ventricular diameter and the ratio of change in motor, language, social, and adaptive levels divided by respective chronological age [Table 10].
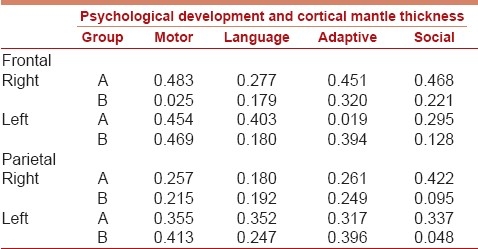
Correlation between changes in the thickness of the cortical mantle in the right, left, frontal, and parietal areas the ratio of changes in motor, language, social and adaptive levels divided by the respective chronological ages.
Preoperative assessment
Preoperatively only 4 children in Group B and 2 children in Group A had normal age-related psychological development. The rest were below the normal levels in their psychological development for their chronological age. The difference between mean chronological age and the mean mental age becomes very obvious in children presenting beyond 9 months of age to the hospital. It may be suggested, if the duration of hydrocephalus is longer preoperatively, the lower the mean mental age attained by the child.
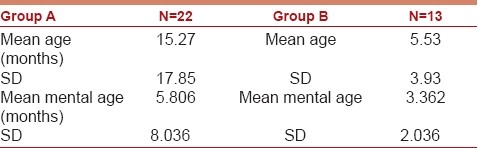
The mean mental age preoperatively was 5.81 months in Group A and 3.36 months in Group B. [Table 11]
Table 11.
Preoperative psychological assessment
Postoperatively there was a consistent improvement in psychological development. This improvement was assessed in terms of development in motor, language, adaptive, and social function in both groups, respectively.
In general near normal psychological development was seen in 8 cases (33.3%) of Group A and in a surprisingly large number of 12 (80%) in Group B [Table 12].
Table 12.
Postoperative psychological development
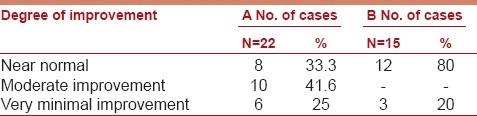
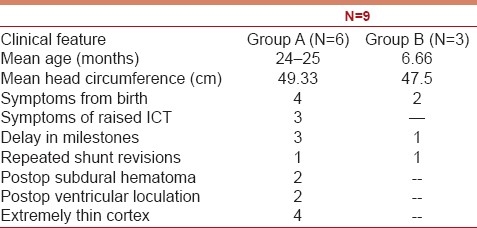
Minimal improvement subgroup analysis of 9 (6 in Group A and only 3 in Group B (22.5%) did not reveal any definite accountable factor. However, the common findings were the higher age group, symptoms of raised ICT, gross delay in milestones at presentation. Their mean head circumference was 48.72 cm with very thin cortical mantle [Table 13].
Table 13.
Analysis of minimal improvement subgroup
Correlative analysis between the psychological development and clinical and radiological parameters revealed that the percentage of improvement in each psychological function in relation to the chronological age was highly related to the age at which therapeutic intervention was made. The percentage of improvement of mental age was significantly greater when intervention was made at age level of less than 6 months. The improvement was also found to be rapid, when the surgical intervention was done at an earlier age.
Postoperative improvement in cella media index was seen with consistent improvement in motor development in both the groups. In Group B it could be correlated to improvement in language and adaptive functions [Table 14].
Table 14.
Correlative values of ventricular indices with psychological development
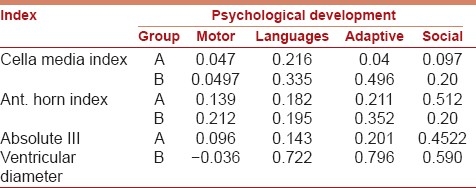
On the contrary, improvement in anterior horn index has significant correlation with improvement in adaptive function only in Group A.
Postoperative improvement in absolute 3rd ventricular diameter as suggested by Tromp et al,[11] has significant correlative value with improvement in language, adaptive and social development in Group B. Unlike in Group B, 3rd ventricular diameter correlated only with improvement in social functions in Group A.
Developmental pattern in group A
Improvement in social and adaptive function development was highly correlated with increase in right frontal cortical mantle. Similarly, language development was associated with increase in left frontal cortical mantle thickness. Both right and left frontal cortical mantle thickness were correlated with improvement in motor development.
Increase in right parietal cortical mantle has a high correlation value with social development, whereas left parietal cortex correlates with motor and language development, but in a lesser degree compared to frontal cortex.
Developmental pattern in group B
Increase in right frontal and right parietal cortical mantle thickness has no correlation with any of the developmental functions except a minimal correlation of increase in right frontal cortex and improvement in adaptive function. On the other hand, improvement in motor and adaptive development were correlated with increase in left frontal and left parietal cortical mantle thickness.
No correlation has been found between improvement in language function and increase in cortical mantle in Group B [Table 15].
Table 15.
Correlative values of cortical mantle thickness with psychological developments
Discussion
CSF diversion in hydrocephalic children reduces the ventricular dilatation. Though improvement in neurological and intellectual functioning is often seen, there is a wide variability in their outcome. A number of reports are available in the literature correlating the ultimate outcome of hydrocephalic children with various clinical and radiological parameters.
Thomson et al,[19] reported an inverse correlation of Ventricle Brain Ratio (VBR) with Bayley Mental scale showing a correlation between brain mass and IQ in older children with uncomplicated hydrocephalus in their series.
Prigatano et al,[9] reported average academic performance during follow-up in children with uncomplicated hydrocephalus despite normal-sized ventricles and functioning shunt.
The results of these reports are not comparable in view of the variability of parameters adopted.
In this study, we have attempted to correlate the clinical radiological findings with the outcome in surgically treated congenital hydrocephalus. Eighteen (72%) children in congenital hydrocephalus group and 93% of children in myelomeningocele group were of less than 6 months of age. More number of children in the second group were seen at a younger age initially. The early detection of hydrocephalus in this group could be due to the follow-up of these children for myelomeningocele. In contrast, the children in Group A were brought when the symptoms were obvious. In our study a large head was noticed at birth, along with a progressive increase in head size in 16% of cases in Group A and 40% in Group B; 92% of them had symptoms of hydrocephalus within 6 months after birth.
Asymmetrical dilatation of lateral ventricles was detected on radiology in 13 children. Similar observations were made by Dennis et al.[2] The asymmetry in ventricles in our study was noticed between the two lateral ventricles and between the various parts of the same lateral ventricle.
Predominant occipital horn dilatation was noticed in 60% with myelomeningocele. Dennis et al,[10] have hypothesized that the nuclear masses in the frontal region offer resistance to the dilating frontal horns and absence of such resistance allows occipital horns to dilate more. In two of our cases, there was only frontal horn dilatation in spite of the presence of normal occipital horns. The exact mechanisms by which this could happen are not clear.
The developmental anomalies of various areas of cerebral hemispheres could result in reduced quantum of cerebral parenchyma in a particular region of cerebral hemisphere. When the intraventricular pressure builds up these areas of decreased resistance, as compared to that offered by normal cerebral parenchyma, dilate more. This could explain the regional and hemispheric asymmetries in dilated ventricles. The exact significance of this asymmetric dilatation in the ultimate neuropsychological outcome is yet to be established.
CSF diversion leads to a reduction in ventricular dilatation and a corresponding increase in cortical mantle thickness. Rubin et al[14–16] reported that the reconstitution of cortical mantle results because of a diminution of white matter edema and due to reactive astrocytosis. He postulated that the clinical improvement results from functional improvement of the remaining neuronal elements rather than replacement of lost elements and the neurological recovery is reversible only up to a stage. In this study, the reconstitution of cortical mantle following shunt surgery occurred in both subgroups to a statistically significant extent (P value less than 0.01).
Many studies have been published concerning the intelligence of the hydrocephalic children. These studies have compared the results of treated and untreated hydrocephalus. Most of the reports have been poorly descriptive and not comparable because of:
the lack of information regarding the shunt and the child shunted;
the use of different instruments to measure intelligence quotient;
differing methods of data presentation; and
inclusion of varying causes.[10]
Preoperative neuropsychological assessment using Gesell development schedules revealed only 6 children among our patients having age appropriate psychological development. The gap between the mean chronological age and the mean mental age widens in patient population after the age of 9 months. Probably shunt surgery performed early in course of the disease before 9 months may minimize the damage due to hydrocephalus. Raimondi et al[10] have also highlighted the importance of early surgery in hydrocephalus. The recovery in these infants could be due to reversible stage of disease, recovery of partially damaged neurons, and neuronal plasticity.
In this series, all the patients had significant ventricular dilatation. However, ventricular sizes were significantly larger in Group A children as compared to infants in Group B. This difference in degree of ventricular dilatation could be explained by earlier detection of hydrocephalus in Group B. Nulsen and Rekate[21] have reported failure in the restitution of cortical mantle to 2 cm in thickness (or more), when infants were operated after 6 months of age.
The wide variation in cognitive outcome for treated hydrocephalus children has stimulated numerous studies. Only a few of these reports had included infants in their study group - presumably on the assumption that cognitive and neurological–psychological assessment techniques for infants do not have predictive validity. However, it has now been shown that there is adequate correlation between infant mental quotient and the IQ, recorded later in childhood.[19] This finding suggests that cognitive assessment of infants with hydrocephalus may be useful in monitoring the effects of treatment and predicting the outcome.
Preoperatively only 4 children in Group B, and 2 children in Group A had normal age-related psychological development. Postoperatively a near normal psychological development was seen in 33.3% cases in Group A and in 80% cases in Group B. Analysis of cases who did not reach normalcy in neuropsychological development did not reveal any clinical/radiological factors responsible. However, the mean age of patients who did not improve or minimally improved was significantly higher as compared to the recovery group. Correlative analysis between the psychological development and clinical and radiological parameters revealed that the percentage of improvement in each psychological function was related to age at which therapeutic intervention was made. The percentage of improvement in mental age was significantly greater when intervention was made before 6 months of age.
In the present study, 80% of children with myelomeningocele and hydrocephalus had reached near normal psychological development as compared to only 33% of children in the hydrocephalus group. This finding is encouraging since most believed that the psychological development in myelomeningocele children should be restrictive in view of physical disability and associated anomalies of brain. The present study proves that given the benefit of early detection and therapy, majority of these children can reach near normal mental development. Raimondi et al[10] also reported near normal cognitive functioning in infants with myelodysplasia and hydrocephalus. Although our results are in agreement with this observation, a follow-up study of these children, when they reach the school age, is necessary to detect specific neuropsychological deficits. Such deficits have been found in older myelodysplasia patients.
Although majority of our patients were in their infancy, some amount of functional lateralization was observed on neuropsychological assessment. On correlating the regional cortical mantle thickness with neuropsychological outcome, it was detected that improvement in social and adaptive function development was better correlated with increase in right frontal cortical mantle compared to the left, whereas language development was more effective with increase in left frontal cortical mantle compared to the right.
Conclusions
The aim of management of hydrocephalus is to achieve total clinical recovery and to obtain normal/near normal intellectual development. However, the outcome seems to depend on multiple factors. Among the 40 children prospectively studied in this series, 15 had associated myelomeningocele, only 6 children out of 40 had normal neuropsychological development preoperatively. Postoperative assessment revealed improvement in neuropsychological function in all cases, although normal age-related development was observed only in 33% of cases in hydrocephalic children. However, it was observed that the extent of improvement in relation to mental age was significantly higher when surgical intervention was done prior to 6 months of age.
Contrary to common belief, the children with myelomeningocele and hydrocephalus demonstrated excellent potential for improvement after CSF diversion. About 80% of children in this subgroup reached normal psychological development. This appears to be related to earlier institution of therapy in this subgroup since these infants were in close observation since birth, which would mean that earlier therapeutic intervention has a significant effect on functional brain development.
The study also revealed that the postoperative increase in cortical mantle was related to improvement in clinical and neuropsychological outcome in all, though to a variable extent. Recovery of neuropsychological function appeared to follow a particular pattern and supports the normal hemispheric functional lateralization established through several functional neuroimaging studies. It was observed that the social and adaptive functional development has higher levels of correlation with increase in right frontal cortical mantle and the language development was correlated to increase in left frontal and parietal cortical mantle.
The motor development was related to both the frontal cortices. It will be interesting to correlate the ultimate functional outcome to the asymmetries in the ventricular dilatation, both localized and generalized on long-term follow-up. Although the result of this study suggests that there is overall improvement in cognitive functioning, in the majority of children who were provided with early surgical intervention, follow-up for prolonged periods is necessary to delineate the ultimate outcome. Assessment of these children in school going age is necessary to detect minor and other specific neuropsychological deficits, which may prevent the total functional recovery in these children and for planning the therapeutic strategies to overcome these deficits.
Improvement in outcome of hydrocephalic children to normalcy or near normalcy appears to the possible with early detection and prompt institution of therapy along with serial and periodic follow-up program for diagnosing and treating complications and dysfunctions, which may be detected from time to time.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Brain TE, Laurence KM. The effect of Hydrocephalus on intelligence, visual perception and school attainment. Dev Med Child Neurol. 1975;17(Suppl 35):129–35. doi: 10.1111/j.1469-8749.1975.tb03592.x. [DOI] [PubMed] [Google Scholar]
- 2.Dennis M, Fitz CR, Netley CT, Sugar J, Harwood-Nash DC, Hendrick EB, et al. The intelligence of hydrocephalic children. Arch Neurol. 1981;38:607–15. doi: 10.1001/archneur.1981.00510100035004. [DOI] [PubMed] [Google Scholar]
- 3.Donofrio AF. Clinical value of Infant testing. Percept Mot Skills. 1965;21:571–4. doi: 10.2466/pms.1965.21.2.571. [DOI] [PubMed] [Google Scholar]
- 4.Howard EM, Thompson M, et al. Outcome in shunted hydrocephalic patients: Shunts and problem in shunts. Monogr Neural Sci. 1982;130:3. [Google Scholar]
- 5.Hunt GM, Holmes AE. Some factors relating to Intelligence in treated children with spina bifida cystica. Dev Med Child Neurol Suppl. 1975:65–70. doi: 10.1111/j.1469-8749.1975.tb03581.x. [DOI] [PubMed] [Google Scholar]
- 6.Hunt GM, Holmes AE. Factors relating to Intelligence in treated children with spina bifida cystica. Am J Dis Child. 1976;130:823–7. doi: 10.1001/archpedi.1976.02120090033006. [DOI] [PubMed] [Google Scholar]
- 7.Knobloch H, Pasamanick B. An evaluation of the consistency and predictive value of the 40 week Gesell developmental schedules. Psychiatr Res Rep Am Psychiatr Assoc. 1960;13:10–41. [PubMed] [Google Scholar]
- 8.Laurence KM. Neurological and intellectual sequelae of hydrocephalus. Arch Neurol. 1969;20:73–81. doi: 10.1001/archneur.1969.00480070083009. [DOI] [PubMed] [Google Scholar]
- 9.Prigatano GP, Zeiner HK, Pollay M, Kaplan RJ. Neuropsychological functions in children with shunted uncomplicated hydrocephalus. Childs Brain. 1983;10:112–20. doi: 10.1159/000120104. [DOI] [PubMed] [Google Scholar]
- 10.Raimondi AJ, Soare P. Intellectual development in shunted hydrocephalic children. Am J Dis Child. 1974;127:664–71. doi: 10.1001/archpedi.1974.02110240050005. [DOI] [PubMed] [Google Scholar]
- 11.Tromp CN, Vanden Burg W. Surgically treated infantile hydrocephalus and predictability of later intelligence. Adv Neurosurg. 1978;6:31. [Google Scholar]
- 12.Upadhyaya P, et al. The outcome of surgical management of hydrocephalus. NIMHANS J. 1985;3:63–8. [Google Scholar]
- 13.Upadhyaya P, Bhargava S, Dube S, Sundaram KR, Ochaney M. Results of Ventriculoatrial shunt surgery for hydrocephalus using Indian Shunt valve, evaluation of intellectual performance with particular reference to computerized axial tomography. Prog Pediatr Surg. 1982;15:209–32. [PubMed] [Google Scholar]
- 14.Rubin RC, Hochwald G, Tiell M, Liwnicz B, Epstein F. Reconstitution of the cerebral cortical mantle in shunt-corrected hydrocephalus. Dev Med Child Neurol Suppl. 1975:151–6. doi: 10.1111/j.1469-8749.1975.tb03595.x. [DOI] [PubMed] [Google Scholar]
- 15.Rubin RC, Hochwald GM, Tiell M, Epstein F, Ghatak N, Wisniewski H. Hydrocephalus: III. Reconstitution of the cerebral cortical mantle following ventricular shunting. Surg Neurol. 1976;5:179–83. [PubMed] [Google Scholar]
- 16.Rubin RC, Hochvald GM. Wood JH, editor. Reconstitution of cerebral cortical mantle following hydrocephalus. Neurobiology of Cerebrospinal fluid. 1983:821–2. [Google Scholar]
- 17.Gessell A, editor. The first five years of life -A Guide to the study of the Preschool Child. London: Methaen; 1971. [Google Scholar]
- 18.Black MM, Matula K. Essentials of Bayley Scales of Infant Development II Assessment. New York: John Wily; 1999. [Google Scholar]
- 19.Bayley N. Manual for the Bayley Scales of Infant Development. 2nd ed. San Antonio, TX: The Psychological Corporation; 1993. [Google Scholar]
- 20.Thompson MG, Eisenberg HM, Levin HS. Hydrocephalic infants: Developmental assessment and computed tomography. Childs Brain. 1982;9:400–10. doi: 10.1159/000120080. [DOI] [PubMed] [Google Scholar]
- 21.Nulsen FE, Rekate HL. Results of Treatment for Hydrocephalus as a guide to future management. In: Stratton GL, editor. Paediatric Neurosurgery, Surgery of Developing Nervous System. Pediatrics. 1. Vol. 52. New York, London: American Association of Neurological Surgeons; 1973. pp. 38–44. [Google Scholar]


