Summary
The Fogarty International Center (FIC) of the U.S. National Institutes of Health has supported long-term (>6 months) basic, clinical and applied research training and research for over 3,600 future leaders in science and public health from low- and middle-income countries (LMICs); tens of thousands more persons have received short-term training. FIC started these programs in 1988 with the flagship HIV/AIDS International Training and Research Program (AITRP) in response to the global pandemic. More than 23 extramural training and research programs plus an intramural program are now operating – all in collaboration with other Institutes and Centers at NIH, U.S. government agencies, foundations, and partner institutions in LMICs and the U.S. While infectious diseases still reign mightily in Sub-Saharan African and South East Asian countries, non-communicable diseases are emerging globally, including in LMICs. Newer FIC training programs are addressing chronic, non-communicable diseases and strengthening the quality of medical schools and health care provider training, in addition to expanding expertise in infectious diseases. The model for successful training is based on long-term commitments, institutional strengthening, “twinning” of research centers, focus on local problems, and active mentoring. Trainees from Africa, Asia, and Latin America have made notable scientific contributions to global health, attained leadership positions, and received special recognition nationally and internationally. As the FIC programs are institutional-strengthening partnerships and candidates are carefully selected and mentored, close to 90% of FIC trainees return to their countries of origin. After returning home the FIC-trained leaders have continued to mentor and train thousands of individuals in their home countries.
Keywords: Fogarty International Center, NIH, research training in poor countries, infectious and non-infectious diseases training
Introduction
The Fogarty International Center (FIC) is one of the 27 institutes and centers (ICs) of the United States National Institutes of Health (NIH), a component of the Department of Health and Human Services (DHHS). The FIC supports basic, clinical and applied research and research training for U.S. and foreign investigators working in low- and middle-income countries (LMICs). Since its establishment by Congress in 1968, over 3,600 scientists globally have received long-term (≥ 6 months) research training and research awards through FIC programs, mostly scientists and public health leaders from the poorest nations; tens of thousands more have received shorter-term training.
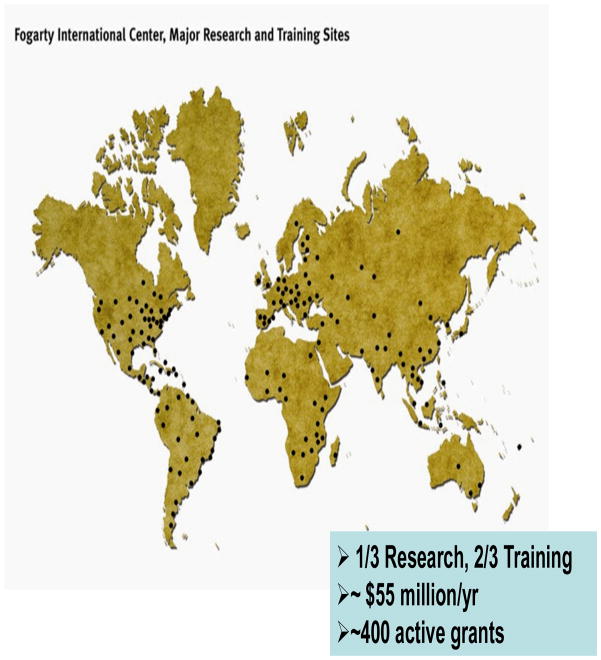
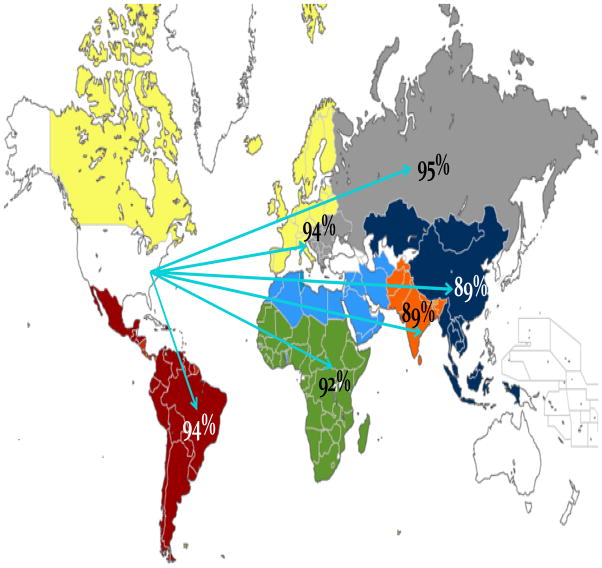
To implement its programs, FIC partners with more than 20 ICs at NIH, numerous U.S. Government agencies, the World Health Organization (WHO), the Bill & Melinda Gates Foundation and other foundations and, most importantly, LMICs, to develop, fund, and implement programs of common interest and mutual benefit. Over 400 extramural research training and research projects involving more than 100 U.S. universities are operating in over 100 LMICs (Figure 1). The FIC also convenes small and large conferences so that the most eminent authorities can address critical global health research problems such as polio eradication, the impact of climate on disease outbreaks, setting disease control priorities in developing countries, confronting the global epidemiological and demographic shift, defining the research agenda for stopping the spread of Plasmodium falciparum resistance to artemisinin compounds, and strengthening research capacity in LMICs. In addition to extramural activities, within FIC there is a research division focusing on quantification of epidemiological trends tied to influenza, diarrheal diseases, malaria, and other infectious diseases (IDs). Other divisions within the FIC define FIC global health research policies, strategies and programs; track and evaluate the success of FIC trainees and activities; promote international collaborations of all NIH institutes and centers; and, administer the global health programs.
Figure 1.
Fogarty-Supported Training and Research, 2011
Global health research is now one of the NIH director’s priorities; this commitment has increased enthusiasm and investment in global health research across the campus. The FIC director’s role as the NIH Associate Director for International Research enables Fogarty to encourage the mobilization of the NIH investment to focus strategically on priority global health issues. President Barack Obama and Secretary of State Hillary Clinton have identified global health as a top international priority within the administration’s new Global Health Initiative (1) which focuses on infectious diseases and maternal-newborn and child health.
Why this focus on young children and mothers? A recent review of under-five mortality has shown that worldwide mortality in children younger than 5 years of age has dropped from 11.9 million deaths in 1990 to 7.7 million deaths in 2010; yet, 3.1 million (40%), 2.3 million (30%), and 2.3 million (30%) of these deaths occur in the neonatal (<1 month), post-neonatal (1 month to 1 year), and 1 year to 5-year periods, respectively (2). Many if not most of these deaths are due to preventable infections. In addition, there are an estimated 150,000 maternal deaths yearly at the time of birth and these deaths are also avertable (2, 3).
The Disease Control Priorities Project and the Fogarty International Center Strategic Plan, 2008–2012
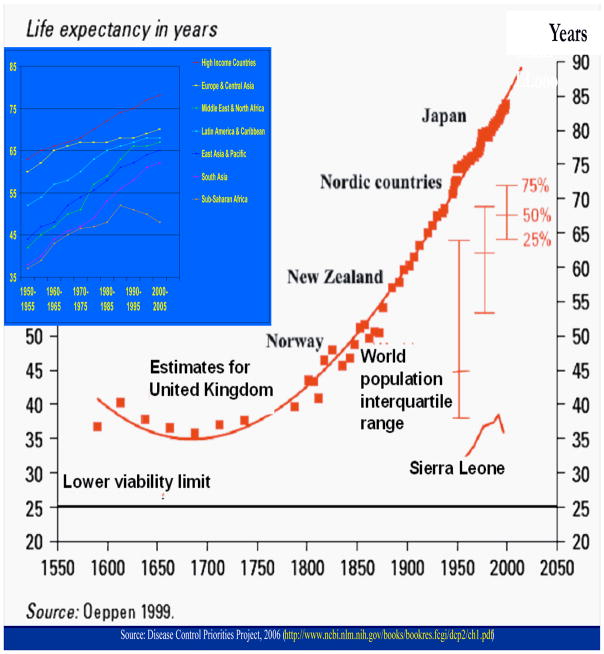
A landmark set of encyclopedic studies was published in 2006 by the Disease Control Priorities Project (DCPP) addressing global health and global health research priorities and the cost-effectiveness of interventions to address common health conditions in LMICs. The DCPP was an alliance of the FIC/NIH, World Bank, World Health Organization, Population Reference Bureau (for dissemination), and the Bill & Melinda Gates Foundation (as funder) with goals to quantify the global burden of diseases by geographic region, assess epidemiological and demographic trends and projections, and compute the cost-effectiveness of interventions to manage, control, and prevent those diseases (4–8). The FIC served as the Secretariat for the DCPP. The DCPP analyses showed that during the latter half of the 20th century, life expectancy increased dramatically throughout the world to greater than 60 years in all regions, except for Sub-Saharan Africa (SSA) where life expectancy at birth was 46 years in 2001 (Figure 2). Noteworthy is that chronic and non-communicable diseases have become more prominent in all regions, including the poorest as well as the richest where cardiovascular diseases, mental illness and cancers are also major problems (Table 1) (4, 5). Perinatal conditions (birth trauma, infections, respiratory distress) are among the top five causes of Disability Adjusted Life years (DALYs) in all but one LMIC region. Even with the demographic and epidemiological shift, IDs comprise close to 30% of the disease burden in LMICs (Table 2).
Figure 2.
Trends in Life Expectancy at Birth Globally and by Geographic (World Bank) Region, 1550–2050
Table 1.
Leading causes of Disability-Adjusted Life Years in Low/Middle-income and High-Income Countries, by World Bank Region, 2001
| Rank | South Asia (GNI: $450) LE:63 |
Sub-Saharan Africa (GNI: $460) LE:46 |
East Asia and the Pacific (GNI: $900) LE:69 |
Europe and Central Asia (GNI: $1,970) LE:69 |
Middle East and North Africa (GNI: $2,200) LE:68 |
Latin America and the Caribbean (GNI: $3,580) LE:71 |
High–income countries (GNI: $26,500) LE:78 |
|---|---|---|---|---|---|---|---|
| 1 | Perinatal conditions | HIV/AIDS | Cerebrovascular diseases | Ischemic heart disease | Ischemic heart disease | Perinatal conditions | Ischemic heart disease |
| 2 | Lower respiratory infections | Malaria | Perinatal conditions | Cerebrovascular diseases | Perinatal conditions | Unipolar depressive | Cerebrovascular diseases |
| 3 | Ischemic heart disease | Lower respiratory infections | Chronic obstructive pulmonary disease | Unipolar depressive disorders | Traffic accidents | Homicide and violence | Unipolar depressive disorders |
| 4 | Diarrheal diseases | Diarrheal diseases | Ischemic heart disease | Self-inflicted injuries | Lower respiratory infections | Ischemic heart disease | Alzheimer’s and other dementias |
| 5 | Unipolar depressive disorders | Perinatal conditions | Unipolar depressive disorders | Chronic obstructive pulmonary disease | Diarrheal diseases | Cerebrovascular diseases | Tracheal and lung cancer |
GNI = gross national income per capita (US$); LE = life expectancy at birth (average male and female).
Sources: Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL, edsin Global Burden of Disease and Risk Factors, 2006
World Development Indicators, 2003
Table 2.
Disease Burden, Low and Middle Income Countries, by World Bank Region, 2001
| Region | Population in millions (%) | Disability-Adjusted Life Years (DALYs)
|
||
|---|---|---|---|---|
| For all diseases, no. in millions (%) | For infectious and parasitic diseases, no. in millions (%) | Infectious diseases burden in region, %* | ||
| Sub-Saharan Africa | 668 (13) | 345 (25) | 173 (54) | 59 |
| South Asia | 1,388 (27) | 409 (29) | 88 (27) | 31 |
| Middle East/North Africa | 310 (6) | 66 (5) | 7 (2) | 16 |
| East Asia/Pacific | 1,850 (35) | 346 (25) | 37 (12) | 14 |
| Latin America/Caribbean | 526 (10) | 104 (8) | 10 (3) | 13 |
| Europe/Central Asia | 477 (9) | 117 (8) | 5 (2) | 6 |
|
| ||||
| Total | 5,219 (100) | 1,387 (100) | 320 (100) | 29 |
includes respiratory infections
Mathers et al, 2006, in Lopez et al, Global Burden of Disease and Risk Factors
Although SSA countries have only 13% of the population of LMICs, they have 25% of the DALYs, and 54% of all the IDs; SEA countries comprise 27% of the LMIC population, 29% of all DALYs, and 27% of the IDs. Within SSA and SEA regions, IDs contribute 59% and 31% of the entire disease burden, respectively (Table 2) (4–9). The top six IDs comprise almost 25% of all DALYs in LMICs (Table 3); SSA has the highest HIV/AIDS, malaria, measles, and sexually transmitted disease burdens and SEA leads in respiratory infections and diarrheal diseases (9).
Table 3.
Infectious Burden, Low-and Middle-Income Countries, by World Bank Region, 2001
| Disease | Disease Burden In LMICs DALYs, % | Disease burden by region, %
|
|||||
|---|---|---|---|---|---|---|---|
| SSA | SA | ME/NA | EA/P | LA/C | E/CA | ||
| Respiratory inf. | 6.3 | 36 | 40 | 4 | 14 | 4 | 3 |
| HIV/AIDS | 5.1 | 79 | 10 | 1 | 4 | 3 | 1 |
| Diarrheal disease | 4.2 | 37 | 38 | 4 | 15 | 4 | 1 |
| Malaria | 2.9 | 89 | 6 | 2 | 3 | 1 | .1 |
| TB | 2.6 | 22 | 38 | 2 | 30 | 3 | 4 |
| Measles | 1.7 | 59 | 28 | 2 | 10 | 0 | 1 |
| STD | 0.7
|
40 | 39 | 4 | 9 | 5 | 2 |
| 23.5 | |||||||
SSA = Sub Saharan Africa; SA = South Asia; ME/NA = Middle East/North Africa; EA/P = East Asia/Pacific; LA/C = Latin America/Caribbean; E/CA = Europe/Central Asia
Mathers et al, 2006, in Lopez et al, Global Burden of Disease and Risk Factors
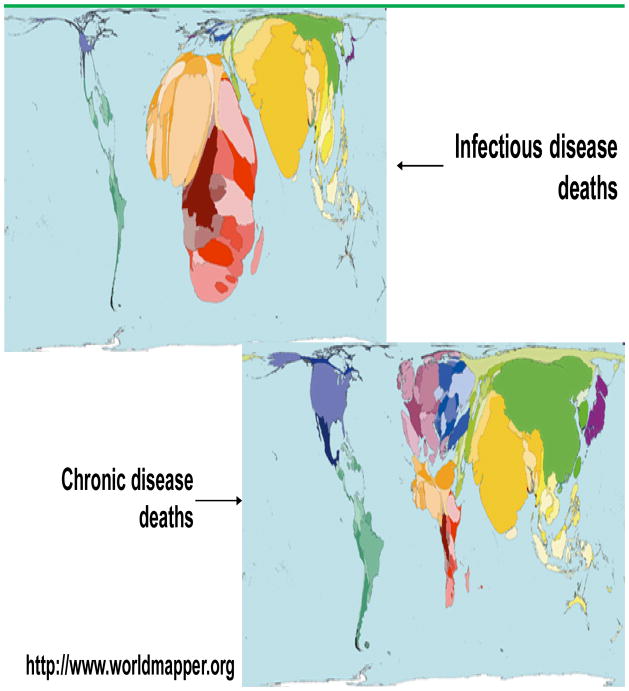
A map of the world with size of the country and regions reflecting infectious and chronic disease deaths is shown in Figure 3 (http://www.worldmapper.org); SSA and SEA are most prominent in this projection for deaths due to IDs. By virtue of their large populations, countries in SEA have a “dual burden” of disease and deaths.
Figure 3.
Deaths due to Infectious and Chronic (Non-Infectious) Diseases by Geographic Region and Country, 2002–2005
Best buys in health were calculated in the DCPP by a comprehensive set of cost-effectiveness analyses addressing over 300 conditions for which proven personal and community-based interventions are available; the “best buys” expressed as DALYs averted per dollar invested include both chronic and communicable diseases (Table 4) (7). These conditions are addressed by several of the FIC programs. Assisting LMICs in setting their own priorities based on local analytic exercises, including best buys, was a major goal. Several countries are using DCPP materials and methods. India and South Africa have begun extensive national priority-setting and health-sector planning exercises; these have been based on field research, health information, analysis, consensus meetings, and policy development actions which are leading to disease reduction programs (10, 11). Both countries have a large “dual burden” of disease.
Table 4.
Top Ten Best Buys in Health Using Disease Burden and Cost-Effectiveness Analysis
|
Adapted from Jamison, D.T., Breman, J.G., Measham, et al., Eds. Disease Control Priorities in Developing Countries, 2nd edition. New York: Oxford University Press; 2006.; Lopez, A. D., Ezzati, M., Mathers, et al., Eds. Global Burden of Disease and Risk Factors. New York: Oxford University Press; 2006.; Jamison, D.T., Breman, J.G., Measham, et al., Eds. Priorities in Health. New York: Oxford University Press; 2006.
The goals and priorities of the FIC Strategic Plan, 2008–2012, were informed by and derive in great part from the extensive reviews and analyses in the DCPP and from U.S. and LMIC stakeholders. As a research and training institution, the FIC vision is “a world in which the frontiers of health research extend across the globe and advances in science are implemented to reduce the burden of disease, promote health, and extend longevity for all people.” The FIC achieves this vision through: facilitating and conducting global health research; building partnerships between and strengthening research institutions in the U.S. and abroad; and, training the next generation of scientists to understand, control, and prevent diseases, especially those in LMICs. FIC specific goals and priorities in the Plan are shown in Table 5 (12); new goals address the shifting global burden of disease and disability while continuing to address the “unfinished agenda” of infectious diseases, research and research training, and implementation research to better deliver and scale-up efficacious locally feasible interventions.
Table 5.
The Fogarty International Center, NIH, Strategic Plan: Goals and Priorities, 2008 – 2012
|
FIC Programs
FIC programs address infectious diseases, non-infectious diseases, and a variety of cross-cutting themes. The FIC Extramural research training and research programs are listed in Table 6; the research training programs (usually D43s in NIH award classification) most often run for 5 years and are renewable through re-competitions. They have leadership development in science and public health as a primary goal. The FIC and NIH research programs (usually R01s, R03s, and 21s) do not have training as a primary goal per se but substantial numbers of LMIC scientists have emerged as leaders, benefitting directly from these collaborations. The FIC research training programs alone have trained over 3,600 scientists for periods from ≥6 months to 4 years; 50% of the trainees have been associated with the HIV/AIDS programs; the Global Infectious Diseases Program, and the International Bioethics Education and Career Development Program have trained over 400 persons each. All research training programs by beginning and ending dates, number of grants given, and persons trained since the first major grant program began in 1988, including numbers of foreign and U.S. trainees are in Table 7. The number of trainees by country is shown in Table 8. China, Brazil, South Africa, and India have had over 200 trainees each. In addition, tens of thousands of others have benefitted from shorter training experiences supported by the FIC and partners, including those tied to laboratory skills and technology transfer. Most importantly, thousands more scientists and public health workers have been mentored and trained by the FIC-trainees upon their return home – and these in turn are training others. Thus, the FIC programs are “a gift that keeps on giving.”
Table 6.
Fogarty International Center, NIH: Research and Research Training Grants, 1988–2011
Research Training Grants
|
Research Grants
|
Not active in 2011.
Table 7.
Fogarty International Center, NIH, Research Training Programs: Number of Grants and Trainees, 1988–2010
| Program | Years of the Program | Year of 1st Training (as reported in CareerTrac) | Number | ||
|---|---|---|---|---|---|
| Grants | Training Experiences for Long Term Foreign Trainees | Training Experiences for Long Term US Trainees | |||
| AIDS International Training and Research Program (AITRP) | 1988-Present | 1989 | 29 | 1559 | 22 |
| International Training and Research In Environmental and Occupational Health (ITREOH) | 1995-Present | 1995 | 14 | 187 | 1 |
| Global Research Training in Population Health (POP) | 1995–2010 | 1996 | 12 | 232 | 0 |
| Global Infectious Disease (GID) | 1997 -Present | 1996 | 41 | 405 | 1 |
| Actions for Building Capacity (ABC) * | 1998–2003 | 1997 | 7 | 48 | 0 |
| Maternal & Child Health (MCH) | 1999–2004 | 1998 | 10 | 64 | 0 |
| Informatics Training Programs (International Training in Medical Informatics & Informatics Training in Global Health) ** | 1999-Present | 1999 | 11 | 87 | 0 |
| International Malaria Research Training (MALAR) * | 1999–2003 | 2000 | 4 | 15 | 0 |
| International Bioethics Education and Career Development (BIOETHICS) | 2000-Present | 2001 | 18 | 415 | 1 |
| International Clinical, Operational and Health Services Research and Training Award (ICHORTA) | 2001–2010 | 2001 | 15 | 169 | 1 |
| International Implementation, Clinical, Operational, and Health Services Research Training Award for AIDS and Tuberculosis (IICHORTA - AIDS/TB) | 2002-Present | 2002 | 10 | 174 | 0 |
| International Collaborative Genetics Research Training (GENE) | 2002–2009 | 1999 | 6 | 31 | 4 |
| Scholars and Fellows Programs (Fogarty International Clinical Research Scholars Program & FIC/ELLISON Fellowships) *** | 2003-Present | 2004 | 1 | 215 | 212 |
| Trauma and Injury Research Training Program (TRAUMA) | 2004-Present | 2004 | 9 | 71 | 0 |
| TOTAL | 187 | 3672 | 242 | ||
Folded into the Global infectious Diseases Program in 2004
Medical Informatics folded into ITGH in 2003
FIC/ELLISON folded into FICRS in 2003
Table 8.
Countries and Number of Long-Term Trainees in Research Training Programs Supported by the FIC, 1988-Present Day
| 1 CHINA | 290 | 28 BOTSWANA | 29 |
|
54 ETHIOPIA | 8 |
|
|
| 2 BRAZIL | 273 | 28 TURKEY | 29 | 54 HUNGARY | 8 | |||
| 3 UNITED STATES* | 241 | 30 POLAND | 28 | 54 NICARAGUA | 8 | |||
| 4 SOUTH AFRICA | 228 | 31 ROMANIA | 26 | 57 BELARUS | 7 |
|
||
| 5 INDIA | 217 | 32 MOZAMBIQUE | 25 | 57 CONGO (DRC) | 7 | |||
| 6 UGANDA | 186 | 33 GHANA | 22 |
|
57 EL SALVADOR | 7 | ||
| 7 PERU | 170 | 33 MALI | 22 | 57 MONGOLIA | 7 | |||
| 8 ARGENTINA | 169 | 35 CAMEROON | 20 |
|
57 TAIWAN | 7 | ||
| 9 KENYA | 138 | 35 INDONESIA | 20 | 62 BOLIVIA | 5 |
|
||
| 10 HAITI | 122 | 37 PHILIPPINES | 18 | 62 CROATIA | 5 | |||
| 11 ZAMBIA | 108 | 38 UKRAINE | 17 | 62 ESTONIA | 5 | |||
| 12 MEXICO | 105 | 39 CZECH REPUBLIC | 15 |
|
62 LESOTHO | 5 | ||
| 13 NIGERIA | 100 | 39 HONDURAS | 15 | 62 NEPAL | 5 | |||
| 14 RUSSIA | 81 | 39 VENEZUELA | 15 | 67 ECUADOR | 4 |
|
||
| 15 THAILAND | 79 | 42 CAMBODIA | 14 |
|
67 LATVIA | 4 | ||
| 16 TANZANIA U REP | 67 | 42 COTE D’IVOIRE | 14 | 67 NAMIBIA | 4 | |||
| 17 MALAWI | 54 | 44 LAOS | 13 |
|
67 SUDAN | 4 | ||
| 18 VIETNAM | 52 | 44 SENEGAL | 13 | 67 UNITED KINGDOM | 4 | |||
| 19 BANGLADESH | 47 | 46 ARMENIA | 12 |
|
72 BURKINA FASO | 3 |
|
|
| 20 COLOMBIA | 45 |
|
46 ZAIRE/DROC | 12 | 72 GUATEMALA | 3 | ||
| 20 ZIMBABWE | 45 | 46 NOT STATED** | 12 | 72 KAZAKHSTAN | 3 | |||
| 22 GEORGIA | 44 |
|
49 DOMINICAN REP | 11 | 72 SRI LANKA | 3 | ||
| 22 PAKISTAN | 44 | 50 JAMAICA | 10 | 76 BARBADOS | 2 |
|
||
| 24 URUGUAY | 40 | 51 EGYPT | 9 |
|
76 GERMANY | 2 | ||
| 25 COSTA RICA | 34 | 51 LITHUANIA | 9 | 76 MOLDOVA | 2 | |||
| 28 CHILE | 32 |
|
51 SLOVAKIA | 9 | 76 SERBIA & MONTENEGO | 2 | ||
| 28 RWANDA | 32 | 76 SIERRA LEONE | 2 | |||||
| TOTAL | 3639 | |||||||
Reflects Clinical Scholars Program
12 Trainees provided no “Country of Origin”
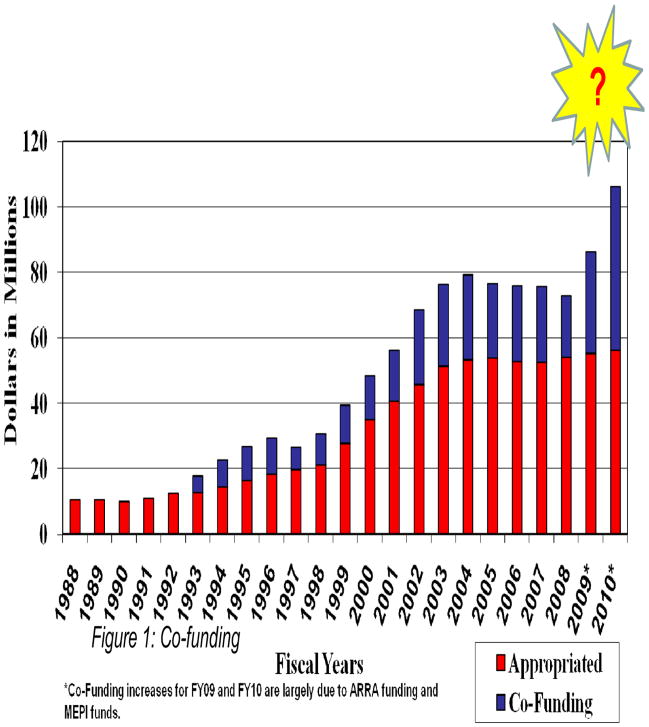
The FIC proposed budget for FY (fiscal year) 2011 is about $73 million of which $58 million is targeted toward the extramural research training programs. The FIC extramural budget grew substantially from 1988 to 2003 ($10 million to $50 million) but has flattened over the past 7 years; co-funding from partners has provided over 20 percent of FIC support over the past decade with a notable increase in FY 2009 and FY 2010 due largely to the American Recovery and Reinvestment Act (ARRA) and the Medical Education Partnership Initiative (MEPI) (discussed below) (Figure 4). From 1988 to 2010, FIC programs have invested over one billion dollars, including co-funding, on global health research training, research, and capacity building in LMICs through partnerships with U.S. institutions. A few examples of FIC programs follow.
Figure 4.
Fogarty International Center, NIH, Extramural Programs (Appropriated and Co-Funding), 1988–2010
Infectious Diseases Programs
The AIDS International Research and Training Program (AITRP), launched in 1988 in response to the HIV/AIDS epidemic, was the first FIC research training program to focus on LMICs and has remained the focus of FIC Extramural Programs; the AITRP has been the template for other Fogarty research training programs. Specific FIC programs have addressed the ecology of infectious diseases (a research program), malaria, tuberculosis, and global infectious diseases (non-HIV/AIDS), and biodiversity conservation/drug discovery from natural products (a research program).
–The AITRP
Since 1988, over 1,500 long-term trainees from more than 90 LMICs at greatest risk have benefited from over $200 million FIC dollars invested in the AITRP; close to 90% of these trainees have returned to their home country and assumed important positions combating HIV/AIDS and related conditions (Figure 5). Almost two-thirds of the trainees have been involved in Ph.D. or post-doctoral advanced training in patient diagnosis, management, and prevention and doing basic virology, pathogenesis, and immunological studies (13–24). What follows are a few examples of research and training conducted as part of the AITRP program.
Figure 5.
Return Rate of Fogarty International Center, NIH, Trainees, 1988–2010
The Botswana-Harvard AIDS Institute Partnership (BHP), established in 1996, addresses prevention of mother-child transmission, the genomic analysis of the HIV virus, vaccine development, and virus resistance and patient adherence to anti-retroviral drugs; the BHP Reference Laboratory is in a training facility building in Gaborone supported by the AITRP and other donors.
A Brazilian trainee linked to the University of California, Berkeley, AITRP has become Director of the National STI/HIV/AIDS Program and President of the National AIDS Commission.
Decreasing HIV/AIDS transmission by circumcision of HIV-infected men was shown by FIC-supported scientists from Uganda and John Hopkins University (22).
The recently published and highly-publicized study demonstrating the effectiveness of a vaginal gel in preventing HIV/AIDS transmission in South Africa was the result of several collaborations between the AITRP supported Center for the AIDS Program of Research in South Africa (CAPRISA), Cape Town, and Columbia University (17, 18).
Because HIV predisposes patients to opportunistic infections, tuberculosis (and drug-resistant TB) is a closely related area of training and investigation in the AITRP and other FIC cooperative initiatives (15, 16, 23).
–The Global Infectious Diseases Training Program (GID)
This program builds sustainable research-capacity in LMICs in Asia, Africa and Latin America that suffer from malaria and other infectious conditions including neglected tropical diseases (25, 26); special focus is given to conditions that affect young children and pregnant women. As of 2004, the program had helped train over 200 students at the undergraduate, graduate, and post-doctoral levels. Some examples of the science and training conducted under the GID program follow.
Grantees from the University of Maryland working with colleagues in Mali and Malawi have discovered genetic markers useful for detecting resistance of Plasmodium falciparum to antimalarial drugs (27).
Scientists from the University of California, San Francisco, has studied effective drug combinations, including artemisinin combination therapies, for managing malaria in working with Uganda colleagues (28).
PIs from Cornell University and the University of California, Berkeley, have been working with PIs from Foundation Oswaldo Cruz (FIOCRUZ) in Salvador and Rio de Janeiro, Brazil, studying leishmaniasis, schistosomiasis, HTLV-1, meningitis and other emerging pathogens of the urban and rural poor (29).
–Ecology of Infectious Diseases (EID)
This research program, partnered with the National Science Foundation, funds interdisciplinary research that elucidates ecological and biological mechanisms that govern the complex relationships tied to environmental changes and transmission dynamics of infectious diseases. Activities focus on the development of predictive models for the emergence and spread of diseases in humans and other animals, and to create and enhance strategies to prevent or control them.
One project focusing on a parasitic disease of coral reefs, is among the first to demonstrate conclusively that climate is a driver for infectious disease in marine ecosystems. The same project has adapted an RNA-based biosensor for field diagnosis of Aspergillus.
The FIC Intramural Program - International Epidemiology and Population Studies (DIEPS) focuses on the study of the determinants, spread, and burden of IDs using descriptive and analytic approaches, with a focus on mathematical modeling. The Multinational Influenza Seasonal Mortality Study (MISMS), Research and Policy for Infectious Disease Dynamics (RAPIDD), and Malnutrition and Enteric Diseases (Mal-ED) Network programs are collaborating globally to understand, describe, predict and prevent epidemics.
–MISMS investigators analyze national and global mortality patterns associated with global influenza virus circulation using modern molecular and modeling approaches (30–35). Collaborations have been established with more than 30 countries, many in the southern hemisphere where influenza patterns had been described sparsely. Information is disseminated via yearly meetings, interactive workshops, and a website (http://www.origem.info/misms/index.php). Recent seasonal influenza trends, epidemics, and basic reproduction numbers in Brazil have been reported by MISMS investigators (30). The MISMS network is funded in great part by the Office of Global Affairs, DHHS.
–RAPIDD researchers make mathematical modeling relevant to policy makers responding to infectious disease outbreaks through analysis and forecasting. Of particular interest are animal-human relationships manifesting in zoonoses. Selected infectious diseases addressed include emerging infections (hantavirus, nipah virus), monkeypox, and rotavirus (36–40). This program is supported by the Department of Homeland Security.
–The new MAL-ED Network is describing the complex inter-relationships between enteric infections and malnutrition in young children in eight LMICs in Asia, Africa, and Latin America. Countries have initiated longitudinal cohort studies using standardized protocols to describe the global pattern of nutritional and enteric factors influencing early childhood development. This large project is co-managed by FIC and the Foundation for the NIH and is funded by the Bill & Melinda Gates Foundation.
Continuing a long history of convening authorities to discuss critical issues in public health policy, the FIC has sponsored several consensus symposia in recent years dealing with infectious diseases.
In 2007, a meeting titled “Polio Immunization: Moving Forward” was co-organized with the National Institute of Allergy and Infectious Diseases (NIAID). This meeting advised research on inactivated and live polio vaccines and other topics in support of the polio eradication initiative (41).
In 2010, in Rio de Janeiro, FIC co-organized a historic symposium “Smallpox Eradication after 30 Years: Lessons, Legacies, and Innovations” with the Sabin Vaccine Institute and the Foundation Oswaldo Cruz, Rio de Janeiro. Emphasis at the symposium was placed on the relevance of smallpox eradication for other programs (42). A special issue of Vaccine will be devoted to the papers presented at this meeting which will focus on the newer disease control and eradication programs inspired by the triumph of smallpox eradication.
Also in 2010, the FIC and NIAID co-organized a meeting “Artemisinin Resistant Malaria: Addressing Research Challenges, Opportunities, and Public Health Challenges.” The research and control agendas and types of collaborations needed to stop the spread of artemisinin resistance are being disseminated widely.
Non-Infectious Disease and Cross-Cutting Programs
Several analyses of the trends in global disease burdens have indicated that cardiovascular diseases (heart attacks, stroke, hypertension), brain disorders and mental illness (depression, schizophrenia), cancer (lung, cervical, gastrointestinal, breast), trauma/injuries (motor vehicle, war), tobacco use, and lifestyle choices (nutrition-obesity-diabetes, hypertension), and others comprise the vast majority of health problems in rich and poor countries alike (Table 1) (4–7, 43). Acute and chronic environmental and occupational health problems are emerging as major challenges globally, especially in eastern European countries; the FIC has trained close to 200 scientists to deal with these growing air, water, and land pollution hazards (Table 7) (44). FIC has added recently several research and research training programs (Tables 6, 7) in response to the changes in demographics and epidemiological burdens. FIC programs are beginning to stress dissemination and implementation research. Evaluation, social science, and management research will be emphasized (45). The ultimate goal of implementation research is to deliver effectively and scale-up proven interventions.
–Chronic, Non-communicable Diseases and Disorders Across the Lifespan (NCD-LIFESPAN)
This new program is training scientists in the diagnosis, management and understanding of non-infectious, chronic diseases. Cardiovascular, nutritional, neuropsychiatric, metabolic and tobacco-related diseases are in this category (46–52).
–Trauma and Injury Research Training Program (TRAUMA)
This program supports research training on the diagnosis, prevention, and/or treatment related to injury and trauma in LMICs. The importance of this new program was shown recently in Cairo where those trained at the Ain Shams hospital in emergency care in collaboration with the University of Maryland saved lives during the recent turbulent political events in Egypt.
–Framework Program for Global Health (FRAME)
The FIC has supported the burgeoning development of multidisciplinary global health coalitions and curricula at U.S. universities. Schools of medicine, public health, nursing, veterinary medicine, and dentistry have joined with faculties of journalism, communications, law, arts and sciences, and others to respond to the growing interest of undergraduates and graduates in global health issues. Major foci of these new programs are to define “global health”, develop curricula, expand faculty interest and competence, and promote interdisciplinary global health research opportunities for students and faculty.
–Clinical Research Scholars and Fellows (FICRS-F)
This resoundingly successful co-funded program offers a one-year, carefully mentored, clinical research training experience for doctoral students and post-doctoral candidates from the U.S.; the scholars (mainly medical students; residents and fellows are newly added) are paired during their training with colleagues from LMICs where they will work. The research training sites are established at NIH-funded and vetted sites in 26 LMICs in Africa, Asia and South America. Vanderbilt University now manages this program which has trained more than 400 young scientists (>200 from the U.S. and >200 from abroad) who aspire to a career in clinical research and global health (Tables 7, 8).
–The Fogarty International Research Collaboration Award (FIRCA)
The FIRCA program fosters international research partnerships between NIH-supported scientists and their collaborators in LMICs; the program benefits the research interests of both collaborators while increasing and enhancing research capacity at the LMIC site. Only scientists who have an eligible NIH grant may apply. Special consideration is given to proposed research that addresses significant global health problems, particularly those problems of high relevance to the foreign country or region; social and behavioral science and chronic diseases are special focus topics.
–The Global Research Initiative Program for New Investigators (GRIP) was established by FIC in 2002 to promote productive re-entry of NIH-trained foreign investigators into their home countries. The specific goal of the initiative was to provide funding opportunities upon returning home for the increasing pool of foreign investigators and health professionals with state-of-the-art knowledge of research approaches to address local problems. GRIP uses the research (R01) funding mechanism. Since 2002, GRIP awards have been made to 77 investigators at 60 institutions in 22 countries.
–Medical Education Partnership Initiative (MEPI)
It is estimated that SSA has only 600,000 health care workers for a population of 682 million; relatively few of these are physicians (51–53). The new Medical Education Partnership Initiative (MEPI) is supporting 13 institutions in 12 SSA countries that, in partnership with the Health Resources and Services Administration (HRSA), receive support from the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR). The U.S. and African academic partners will develop, expand, and enhance models of medical education focusing on front-line health care providers. These models are intended to support PEPFAR’s goal of increasing the number of new health care workers by 140,000, strengthen existing medical education systems, and build clinical and research capacity in Africa as part of a retention strategy for faculty of medical schools, especially clinical professors. MEPI intends to provide up to $130 million in grants over five years to African institutions in a dozen countries, forming a network of about 30 regional partners, country health and education ministries, and more than 20 U.S. collaborators.
Eleven programmatic awards, largely funded by PEPFAR, will expand and enhance HIV/AIDS medical education and research training. Eight smaller non-HIV/AIDS awards, funded by the NIH Director’s Common Fund, with additional support from several NIH institutes, will encourage the development of expertise in maternal and child health, cardiovascular diseases, cancer, mental health, surgery, and emergency medicine. Over a five-year period, MEPI intends to provide up to $10 million for each programmatic award, up to $2.5 million for each linked project and up to $1.25 million for each pilot grant.
Fogarty Success Stories
In addition to successes mentioned above, FIC trainees have made numerous scientific advances, attained leadership positions, and received honors during and since their training. A few examples of these achievements are described briefly in Table 9.
Table 9.
Selected Fogarty Success Stories
|
Successful Training for Research in LMICs – The Fogarty Model
There is a great need to develop a much larger health workforce in LMICs. Over the past 23 years the FIC has developed a successful model for training scientists and public health workers in research and leadership and their application to local problems. Close to 90% of long-term trainees have returned to their home countries and many have become national and international leaders.
Over the years, FIC has developed strategies that assure the programs succeed in building capacity in LMICs. Experience with the development of these research training programs have led to a series of principles FIC uses to develop successful research collaboration training programs (Table 10). In general, Fogarty investments are long-term, made for 5 years, renewable by re-competition to 10 or more years; focus on institutional strengthening, including addressing managerial and administrative skills; require that U.S. institutions “twin” with foreign research centers emphasizing local priorities and involvement; require that the U.S. and other northern country grantee or the LMIC, have an underlying research grant (R01 or equivalent) supported by NIH or another funder; this gives the collaboration a solid research base and intellectual and financial support from other NIH research organizations, including institutes and centers. Further, Fogarty launched a program to expand opportunities for NIH trained foreign scientists to obtain competitive “re-entry” (GRIP) awards of about $50,000 per year to begin an independent research program in their home country.
Table 10.
Principles of Successful FIC Research Training and Research Programs
|
Principles for encouraging LMIC scientists to return to their countries and decreasing the “brain drain” are also addressed by the PIs during the training programs (56). One principle is to include an agreement between the trainees, their institutions and the co-principal investigator, in the U.S. and home country, for the trainee to return to the home country. Mentors often secure positions for successful trainees when they return, increasing their likelihood of success.
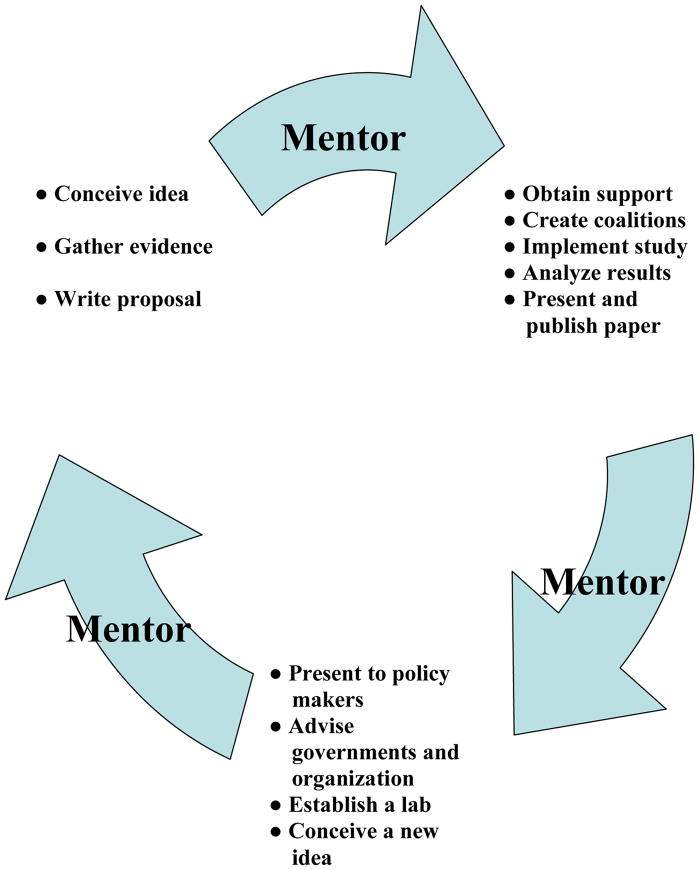
While institutions have rich research environments, networks, and cachet, highly motivated individuals create ideas, inventions and innovations that advance science and public health. We have developed a “12-Step Program” to develop leaders in science (Figure 6). In distinction from richer countries, many scientists from LMICs very frequently have the opportunity to present their analyses and views to decision-makers, are actively involved in developing disease management and prevention guidelines, and have a strong influence on priority setting, decision-making and allotment of funds for research, and public health and development programs. It is not uncommon for a leader in science in a LMIC to head a control or elimination program. Leaders in science and public health from rich and poor countries are increasingly faced with ethical issues tied to their research and its application. The FIC ethics research program is addressing this cross-cutting area (57).
Figure 6.
What a Superior Trainee-Scientist Must Do: The “12-Step Program” for Developing Successful Trainees
The importance of good mentoring in FIC programs must be stressed. Good mentoring is a long-term relationship between trainees and senior investigators, between trainees and persons with special experience and skills, and between trainees themselves. As research institutions in LMICs have become stronger in staff and other resources, collaborations between LMICs have blossomed; many trainees from northern, rich countries are now being mentored by scientist-grantees from and in LMICs. Most encouraging is that many young scientists trained by the FIC programs have gone on to publish in internationally renowned journals, win research awards (including R01s) and establish their own independent laboratories where they can mentor the next generation of research scientists in their own and other countries.
Conclusion
Since 1988, over one billion dollars have been invested, including co-funding, on global health research training, research, and capacity building in FIC programs targeting large LMICs through partnerships with US institutions. Through these efforts, FIC has supported a large cadre of scientists in becoming global health leaders. We have defined several characteristics of successful capacity building initiatives, including institutional strengthening, “twinning” of research centers, focus on local problems, active mentorship, mutual benefit to all partners, and, innovation in research. FIC’s ID programs, such as AITRP, GID and EID, have made breakthroughs in drug development and testing, genetic marker research and understanding and managing patients with neglected tropical diseases. Intramural epidemiology and population studies programs have made important contributions by defining global mortality patterns associated with influenza, and investigating animal-human relationships manifesting in zoonoses and the complex relationships between enteric infections and malnutrition in children. FIC-funded non-infectious disease programs have expanded global health teaching and training in the United States. Several new programs, such as TRAUMA and NCD-LIFESPAN, promote research on the heavy toll caused by non-communicable diseases and injuries. The FIRCA, GRIP, and MEPI foster capacity building and institutional strengthening in LMICs. The wide variety of programs, projects and initiatives supported by FIC reflects FIC’s goals of providing comprehensive training and tools to investigators to ultimately – and sustainably – build capacity in global health research and lessen the burden of global disease and illness worldwide.
Acknowledgments
We thank FIC scientist-program managers and support staff for their very capable stewardship of the research training and research programs: these are Josh Rosenthal, Flora Katz, Xingzhu Liu, Jeanne McDermott, Kathleen Michels, Myat Htoo Razak, Barbara Sina, and Yvonne Njage; Mark Miller, Ellis McKenzie, Cecile Viboud, and Stacey Knobler for research and leadership contributions in infectious diseases; and James Herrington, Karen Hofman, Letitia Robinson, Nalini Anand and Rachel Sturke for coordinating global science strategy, policy, and planning at NIH; we are very grateful for assistance on preparation of the manuscript from Mantra Singh, Celia Wolfman, Erica Schonman, Natalie Engmann, Danielle Bielenstein, Ann Puderbaugh, Farah Bader, and Vikash Parekh. Our special gratitude goes to the many FIC principal investigators in the U.S. and abroad and their trainees who are responsible for the achievements resulting from FIC support, and for training the next generation of leaders in science and public health.
Footnotes
The authors have nothing to disclose.
References
- 1.Secretary of State Hillary Rodham Clinton. The Global Health Initiative: The Next Phase of American Partnership in Health. Speech. http://www.state.gov/secretary/rm/2010/08/146002.htm; August 16, 2010.
- 2.Rajaratnam JK, Marcus JR, Flaxman, et al. Neonatal, postneonatal, childhood, and under-5 mortality for 187 countries, 1970–2010: a systematic analysis of progress towards Millennium Development Goal 4. The Lancet. 2010;375(9730):1988–2008. doi: 10.1016/S0140-6736(10)60703-9. [DOI] [PubMed] [Google Scholar]
- 3.Coovadia H, Rollins N. Tying up loose threads in delivery of a newborn care package. The Lancet. 2011;377(9763):361–3. doi: 10.1016/S0140-6736(11)60058-5. [DOI] [PubMed] [Google Scholar]
- 4.Jamison DT, Breman JG, Measham, et al., editors. Disease Control Priorities in Developing Countries. 2. New York: Oxford University Press; 2006. [PubMed] [Google Scholar]
- 5.Lopez AD, Ezzati M, Mathers, et al., editors. Global Burden of Disease and Risk Factors. New York: Oxford University Press; 2006. [Google Scholar]
- 6.Jamison DT, Breman JG, Measham, et al., editors. Priorities in Health. New York: Oxford University Press; 2006. [Google Scholar]
- 7.Laxminarayan R, Mills AR, Breman, et al. Advancement of global health: key messages from the Disease Control Priorities Project. The Lancet. 2006;367:1193–208. doi: 10.1016/S0140-6736(06)68440-7. [DOI] [PubMed] [Google Scholar]
- 8.Hotez PJ, Remme JH, Buss, et al. Combating tropical infectious diseases: report of the Disease Control Priorities Project in Developing Countries. Clin Infect Dis. 2004;38:871–878. doi: 10.1086/382077. [DOI] [PubMed] [Google Scholar]
- 9.Breman JG, Jamison D, Alleyne G, et al. Infectious Diseases and the Disease Control Project. In: Serageldin I, Masood E, El-Faham M, et al., editors. Changing Lives, BioVision, Alexandria. Biblioteca Alexandrina; Alexandria, Egypt: 2006. pp. 81–94. 2007. [Google Scholar]
- 10.Jha P, Laxminarayan R. Choosing Health: an entitlement for all Indians. Center for Global Health Research, University of Toronto; 2009. [Google Scholar]
- 11.Hofman K, Tollman SM. Health policies and practice: Setting priorities for health in 21st century South Africa. South African Med J. 2010;100(12):798–800. doi: 10.7196/samj.4438. [DOI] [PubMed] [Google Scholar]
- 12.FIC Strategic Plan reflects the collective wisdom of the Fogarty staff, the Fogarty Advisory Board, and the hundreds of stakeholders who provided advice and comments at national and international meetings or through the Fogarty Web site. A full copy of the Strategic Plan is available at: www.fic.nih.gov/about/plan/strategicplan_08-12.htm
- 13.Atashili J, Kalilani L, Seksaria V, et al. Potential impact of infant feeding recommendations on mortality and HIV-infection in children born to HIV- infected mothers in Africa: a simulation. BMC Infect Dis. 2008;8:66. doi: 10.1186/1471-2334-8-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dunkle KL, Stephenson R, Karita, et al. New heterosexually transmitted HIV infections in married or cohabiting couples in urban Zambia and Rwanda: an analysis of survey and clinical data. The Lancet. 2008;371(9631):2183–91. doi: 10.1016/S0140-6736(08)60953-8. [DOI] [PubMed] [Google Scholar]
- 15.Gupta A, Nayak U, Ram, et al. Postpartum Tuberculosis incidence and mortality among HIV-infected women and their infants in Pune, India, 2002–2005. Clinical Infectious Diseases. 2007;45(2):241–249. doi: 10.1086/518974. [DOI] [PubMed] [Google Scholar]
- 16.Harris JB, Hatwiinda SM, Randels KM, et al. Early lessons from the integration of tuberculosis and HIV services in primary care centers in Lusaka, Zambia. Int J Tuberc Lung Dis. 2008;12(7):773–9. [PubMed] [Google Scholar]
- 17.Karim QA, Kharsamy AB, Naidoo, et al. Co-enrollment in multiple HIV prevention trials – Experiences from the CAPRISA 004 Tenofavir gel trial. Contemp Clin Trials. 2011 January 26; doi: 10.1016/j.cct.2011.01.005. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Karim QA, Karim SSA, Frohlich, et al. on behalf of the CAPRISA 004 Trial Group. Effectiveness and Safety of Tenofovir Gel, an Antiretroviral Microbicide, for the Prevention of HIV Infection in Women. Sciencexpress. 2010;1193748:1–10. [Google Scholar]
- 19.Morris MB, Chapula BT, Chi BH, et al. Use of task-shifting to rapidly scale-up HIV treatment services: experiences from Lusaka, Zambia. BMC Health Serv Res. 2009;9:5. doi: 10.1186/1472-6963-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Potter D, Goldenberg RL, Chao A, et al. Do targeted HIV programs improve overall care for pregnant women?: Antenatal syphilis management in Zambia before and after implementation of prevention of mother-to-child HIV transmission programs. J Acquir Immune Defic Syndr. 2008;47(1):79–85. doi: 10.1097/QAI.0b013e31815d2f71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Turan JM, Miller S, Bukusi, et al. HIV/AIDS and maternity care in Kenya: how fears of stigma and discrimination affect uptake and provision of labor and delivery services. AIDS Care. 2008;20(8):938–45. doi: 10.1080/09540120701767224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wawer MJ, Makumbi F, Kigozi G, et al. Circumcision in HIV-infected men and its effect on HIV transmission to female partners in Rakai, Uganda: a randomized controlled trial. The Lancet. 2009;374(9685):229–37. doi: 10.1016/S0140-6736(09)60998-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhao M, Li X. Transmission of MDR and XDR tuberculosis in Shanghai, China. PLoS One. 2009;4(2):e4370. doi: 10.1371/journal.pone.0004370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mpontshane N, Van den Broeck J, Chhagan M, et al. HIV infection is associated with decreased dietary diversity in South African children. J Nutr. 2008;138(9):1705–11. doi: 10.1093/jn/138.9.1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jones KEP, Levy NG, Storeygard A, et al. Global trends in emerging infectious diseases. Nature. 2008;451:990–993. doi: 10.1038/nature06536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Berriman M, Haas BJ, LoVerde PT, et al. The genome of the blood fluke Schistosoma mansoni. Nature. 2009;460(7253):352–8. doi: 10.1038/nature08160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Laufer MK, Takala-Harrison S, Dzinjalamala, et al. Return of chloroquine-susceptible falciparum malaria in Malawi was a re-expansion of diverse susceptible parasites. J Infect Dis. 2010;202(5):801–8. doi: 10.1086/655659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nankabirwa J, Cundill B, Clarke S, et al. Efficacy, safety, and tolerability of three regimens for prevention of malaria: a randomized, placebo-controlled trial in Ugandan schoolchildren. PLoS One. 2010;5(10):e13438. doi: 10.1371/journal.pone.0013438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Riley LW, Ko AI, Unger A, et al. Slum health: diseases of neglected populations. BMC Intl Health Human Rights. 2007;7:2e. doi: 10.1186/1472-698X-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alonso WJ, Viboud C, Simonsen L, et al. Seasonality of influenza in Brazil: A traveling wave from the Amazon to the subtropics. American Journal of Epidemiology. 2007;165:1434–1442. doi: 10.1093/aje/kwm012. [DOI] [PubMed] [Google Scholar]
- 31.Chowell G, Bertozzi SM, Colchero MA, et al. Severe respiratory disease concurrent with the circulation of H1N1 Influenza. N Engl J Med. 2009;361(7):674–9. doi: 10.1056/NEJMoa0904023. [DOI] [PubMed] [Google Scholar]
- 32.Chowell G, Viboud C, Simonsen L, et al. The reproduction number of seasonal influenza epidemics in Brazil, 1996–2006. Proc Biol Sci. 2010;277(1689):1857–69. doi: 10.1098/rspb.2009.1897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ghedin E, Laplante J, DePasse J, et al. Deep sequencing reveals mixed infection with pandemic influenza A (H1N1) virus strains and the emergence of oseltamivir resistance. J Infect Dis. 2011;203(2):168–174. doi: 10.1093/infdis/jiq040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gordon A, Saborío S, Videa E, et al. Clinical attack rate and presentation of pandemic H1N1 influenza A and B in a pediatric cohort in Nicaragua. Clin Infect Dis. 2010;50(11):1462–7. doi: 10.1086/652647. [DOI] [PubMed] [Google Scholar]
- 35.Viboud C, Miller M, Olson D, et al. Preliminary estimates of mortality and years of life lost associated with the 2009 A/H1N1 pandemic in the US and comparison with past influenza seasons. PLoS Curr Influenza. 2010:RRN1153. doi: 10.1371/currents.RRN1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lloyd-Smith JO, George D, Pepin KM, et al. Epidemic dynamics at the human-animal interface. Science. 2009;326(5958):1362–67. doi: 10.1126/science.1177345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pepin KM, Lass S, Pulliam JRC, et al. Identifying genetic markers of adaptation for surveillance of viral host jumps. Nature Reviews Microbiology. 2010;8(11):802–13. doi: 10.1038/nrmicro2440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pitzer VE, Viboud C, Simonsen L, et al. Demographic variability, vaccination, and the spatiotemporal dynamics of rotavirus epidemics. Science. 2009;325(5938):290–4. doi: 10.1126/science.1172330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pulliam JR, Dushoff J. Ability to replicate in the cytoplasm predicts zoonotic transmission of livestock viruses. J Infect Dis. 2009;199(4):565–8. doi: 10.1086/596510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rimoin AW, Mulembakani PM, Johnston SC, et al. Major increase in human monkeypox incidence 30 years after smallpox vaccination campaigns cease in the Democratic Republic of Congo. Proc Natl Acad Sci. 2010;107(37):16262–7. doi: 10.1073/pnas.1005769107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ehrenfeld E, Glass RI, Agol VI, et al. Immunisation against poliomyelitis: moving forward. The Lancet. 2008;371:1385–87. doi: 10.1016/S0140-6736(08)60597-8. [DOI] [PubMed] [Google Scholar]
- 42.Breman JG, De Quadros C, Dowdle WR, et al. The role of research in disease eradication and elimination efforts other than malaria: lessons learned. PLoS Med. 2011;8(1):e1000012. doi: 10.1371/journal.pmed.1000405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Daar AS, Singer PA, Persad DL, et al. Grand Challenges in chronic non-communicable diseases. Nature. 2007;450(22):494–96. doi: 10.1038/450494a. [DOI] [PubMed] [Google Scholar]
- 44.Bridbord K, Breman JG, Primack K, et al. Building global environmental health capacity through international scientific cooperation and partnerships. Int J Occup Environ Health. 2006;12:295–299. doi: 10.1179/oeh.2006.12.4.295. [DOI] [PubMed] [Google Scholar]
- 45.Madon T, Hofman KJ, Kupfer L, et al. Implementation Science. Science. 2007;318:1728–29. doi: 10.1126/science.1150009. [DOI] [PubMed] [Google Scholar]
- 46.Gaziano TA, Young CR, Fitzmaurice G, et al. Laboratory-based versus non-laboratory-based method for assessment of cardiovascular disease risk: the NHANES I Follow-up Study cohort. The Lancet. 2008;371(9616):923–31. doi: 10.1016/S0140-6736(08)60418-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Boivin MJ, Bangirana P, Byarugaba J, et al. Cognitive impairment after cerebral malaria in children: A prospective study. Pediatrics. 2007;19(2):E360–E366. doi: 10.1542/peds.2006-2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fernald LC, Gertler PJ, Hou X. Cash component of conditional cash transfer is associated with higher body mass index and blood pressure in adults. J Nutr. 2008;138(11):2250–7. doi: 10.3945/jn.108.090506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Anjana RM, Lakshminarayanan S. Parental history of type 2 diabetes mellitus, metabolic syndrome, and cardiometabolic risk factors in Asian Indian adolescents. Metabolism. 2009;58(3):344–50. doi: 10.1016/j.metabol.2008.10.006. [DOI] [PubMed] [Google Scholar]
- 50.Hoddinott J, Maluccio JA, Behrman JA, et al. Effect of a nutrition intervention during early childhood on economic productivity in Guatemalan adults. The Lancet. 2008;371(9610):411–416. doi: 10.1016/S0140-6736(08)60205-6. [DOI] [PubMed] [Google Scholar]
- 51.Jha P, Jacob B, Gajalakshmi V, et al. A nationally representative case-control study of smoking and death in India. N Engl J Med. 2008;358(11):1137–47. doi: 10.1056/NEJMsa0707719. [DOI] [PubMed] [Google Scholar]
- 52.Pradeepa R, Anitha B, Mohan V, et al. Risk factors for diabetic retinopathy in a South Indian Type 2 diabetic population--the Chennai Urban Rural Epidemiology Study (CURES) Eye Study 4. Diabet Med. 2008;25(5):536–42. doi: 10.1111/j.1464-5491.2008.02423.x. [DOI] [PubMed] [Google Scholar]
- 53.Collins FS, Glass RI, Whitescarver J, et al. Developing Health Workforce Capacity in Africa. Science. 2010;330(6009):1324–5. doi: 10.1126/science.1199930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mullan F, Frehywot S, Omaswa F, et al. Medical schools in sub-Saharan Africa. The Lancet. 2010 doi: 10.1016/S0140-6736(10)61961-7. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 55.Mullan F, Frehywot S. Non-physician clinicians in 47 sub-Saharan African countries. The Lancet. 2007;370(9605):2158–63. doi: 10.1016/S0140-6736(07)60785-5. [DOI] [PubMed] [Google Scholar]
- 56.Kupfer L, Hofman K, Jarawan R, et al. Strategies to discourage brain drain. Bulletin of the World Health Organization. 2004;82(8):616–623. [PMC free article] [PubMed] [Google Scholar]
- 57.Ajuwon AJ, Kass N. Outcome of a research ethics training workshop among clinicians and scientists in a Nigerian university. BMC Med Ethics. 2008;9:1. doi: 10.1186/1472-6939-9-1. [DOI] [PMC free article] [PubMed] [Google Scholar]