Abstract
Aims
Determine whether 18 months of telephone continuing care improves 24 month outcomes for patients with alcohol dependence. Subgroup analyses were done to identify patients who would most benefit from continuing care.
Design
Comparative effectiveness trial of continuing care that consisted of monitoring and feedback only (TM) or monitoring and feedback plus counseling (TMC). Patients were randomized to treatment as usual (TAU), TAU plus TM, or TAU plus TMC, and followed quarterly for 24 months.
Setting
Publicly funded intensive outpatient programs (IOP)
Participants
252 alcohol dependent patients (49% with current cocaine dependence) who completed 3 weeks of IOP.
Measurements
Percent days drinking, any heavy drinking, and a composite good clinical outcome.
Findings
In the intent to treat sample, group differences in alcohol outcomes out to 18 months favoring TMC over TAU were no longer present in months 19–24. Approximately 50% of participants met criteria for Good Clinical Outcomes throughout treatment and follow-up with a non-significant trend for TMC to perform better than usual care. Overall significant effects favoring TMC and TM over TAU were seen for women; and TMC was also superior to TAU for participants with social support for drinking, low readiness to change, and prior alcohol treatments. Most of these effects were obtained on at least 2 of 3 outcomes. However, no effects remained significant at 24 months.
Conclusions
The benefits of an extended telephone-based continuing care programme to treat alcohol dependence did not persist after the end of the intervention. A post-hoc analysis suggested that women and individuals with social support for drinking, low readiness to change, or prior alcohol treatments may benefit from the intervention.
Keywords: comparative effectiveness study, alcohol dependence, continuing care, telephone counseling, monitoring and feedback
Introduction
Continuing care interventions can provide extended recovery support1–4 for patients with chronic substance use disorders.5–7 A recent review concluded that continuing care with longer planned durations and more active efforts to deliver the intervention tended to produce larger effects.3 The telephone holds promise for the delivery of continuing care, as it reaches individuals who cannot come to a clinic due to competing responsibilities, disabilities, distance, or other transportation issues.1 However, research on the effectiveness of telephone continuing care has generated mixed results, with some studies yielding positive findings8–9 and others mixed or negative findings.10–11
This comparative effectiveness study evaluated two 18 month telephone-based continuing care interventions for patients with alcohol dependence, many of whom also had co-occurring cocaine dependence. One intervention consisted of brief telephone calls that included an assessment of current status and feedback (Telephone Monitoring, or TM). The second intervention also provided counseling linked to the results of the assessment (Telephone Monitoring and Counseling, or TMC). All participants received treatment as usual (TAU) in Intensive Outpatient Programs (IOPs) and were randomized to receive TAU only, TAU plus TM, or TAU plus TMC.
TMC produced better outcomes than TAU on incidence and frequency of drinking and heavy drinking during the 18 month treatment phase. However, TM did not improve drinking outcomes over TAU.12 Analyses with 11 potential moderators indicated that none of the variables interacted significantly with the TMC vs. TAU contrast to predict drinking outcomes. Conversely, significant interactions were obtained in the comparison of TM and TAU, in which TM produced better drinking outcomes than TAU for women and for participants with lower readiness to change.13
The goal of the this article was to determine whether TM and TMC achieved better overall management of alcohol and drug dependence than TAU across the full 24 month follow-up. Two of the primary outcome measures from prior study publications12–13 were examined, percent days drinking and a dichotomous measure of any heavy drinking14, as well as a new composite “good clinical outcome” measure, which considered risky alcohol use, drug use, and inpatient treatment for substance use or psychiatric problems.
Although prior analyses13 had found few significant interactions between the continuing care conditions and potential moderators, these analyses had limited power due to the strong performance of TMC relative to TAU and the sample size. The possibility remained that the extended continuing care interventions were beneficial to some patients but not to others. Therefore, subgroup analyses were performed to determine whether significant treatment effects were limited to women and patients at heightened vulnerability to relapse because of social networks that supported or encouraged continued alcohol use, low readiness to change, or prior treatments for alcoholism.7,13,15–16
Methods
Participants
Participants were 252 patients in two IOPs who completed three weeks of treatment; had no psychiatric or medical conditions that precluded outpatient treatment; were 18 to 65 years old; had no IV heroin use within the past 12 months; were able to read at the 4th grade level; and had a minimum degree of stability in living situation.
The participants averaged 43.0 (sd= 7.4) years of age and 11.8 (sd= 1.8) years of education, and the majority were male (64.3%) and African American (88.9%) All participants had current alcohol dependence. They averaged 20.9 (sd= 9.3) years of regular alcohol use and 3.4 (sd= 3.7) prior treatments for alcohol problems. Rates of co-occurring cocaine dependence were high (79% lifetime; 49% current). A complete description of the sample is provided elsewhere.12
Continuing Care Treatment Conditions
Telephone monitoring (TM)
Participants received brief telephone calls for up to 18 months. These 5–10 minute calls were offered weekly for the first 8 weeks, every other week for the next 10 months, and once per month for the final 6 months. Each call consisted of a 10 item “progress assessment” that covered current substance use, other risk factors, and protective factors. A scoring algorithm produced a single summary score which was provided to the participant.12
Telephone monitoring and counseling (TMC)
The call schedule for TMC was the same as in TM, and participants also completed the progress assessment and were given their overall risk score at the beginning of each call. Current goals and the specific objectives to be accomplished to reach each goal were discussed and coping responses to existing or anticipated risky situations were identified and rehearsed. A complete description of TM and TMC is provided elsewhere.12
Therapists
Telephone continuing care was provided by seven therapists (four women, three men), who each delivered both interventions. Coding of audio-taped sessions indicated TMC and TM were provided in a manner consistent with the protocol and distinct from each other.12
Procedures
Recruitment
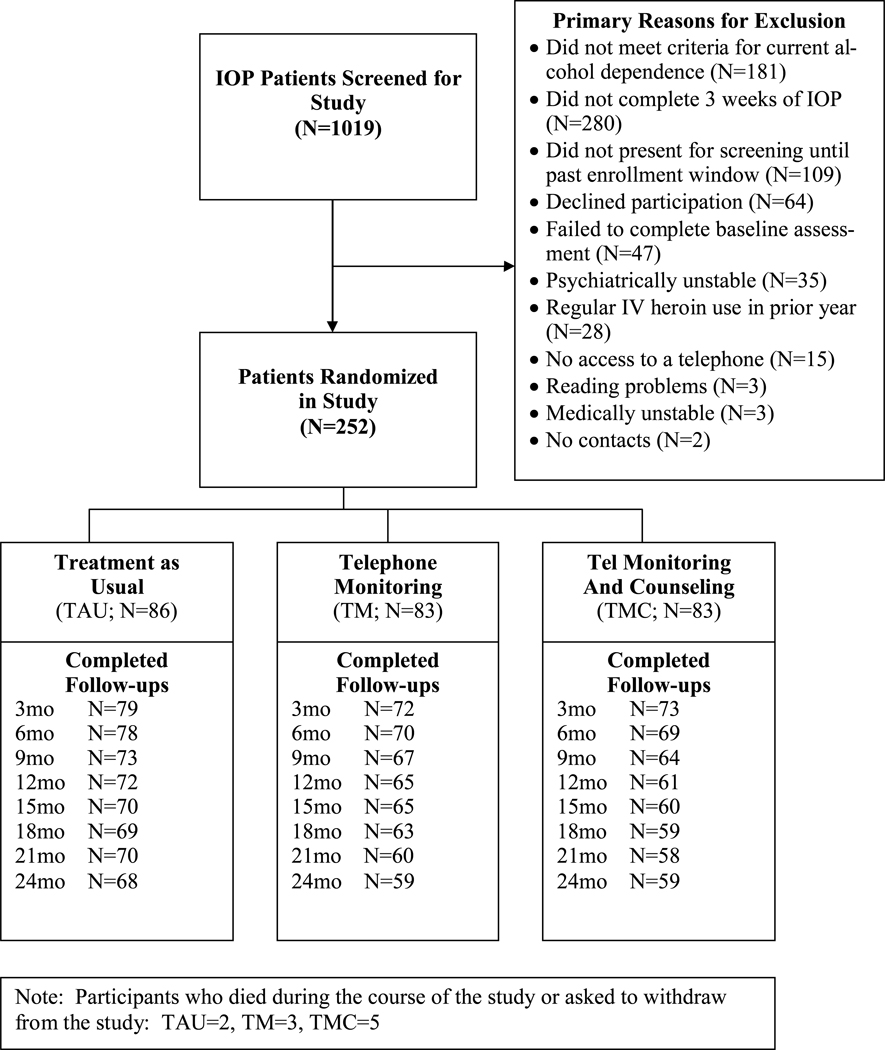
Potential participants were given a full screening if they completed three weeks of IOP. Informed consent procedures were completed prior to assessment. The size of the sample was selected to provide power to find a moderate size effect in the main effect analyses. The study was conducted in compliance with the policies of the Institutional Review Board of the University of Pennsylvania. Participants were recruited between May 17, 2004 and August 7, 2007. A total of 1019 patients were screened at the two IOPs, and of these, 252 were eligible and willing to participate and were enrolled in the study (see Figure 1).
Figure 1.
Consort Diagram
Randomization procedures
Blocked randomization was used to yield a balanced allocation of participants to the treatment conditions. The study statistician, KGL, generated the sequences. The assignments were concealed until randomization.
Baseline and follow-up assessments
Baseline assessments were administered in weeks 3 or 4 of IOP. The follow-up assessments were conducted every 3 months. Participants received $50 for the baseline assessment, and $35 for each follow-up assessment. All study interviews were conducted by research personnel who were blind to the study hypotheses but not to treatment condition. The follow-up rates ranged from 90% at 3 months to 77% at 24 months (TAU=81%, TM= 73.8%; TMC= 75.6%).
Measures
Diagnoses and problem severity
The Structured Clinical Interview for DSM-IV (SCID)17 was administered at baseline to assess Axis I disorders. Information on problem severity in seven domains was obtained with the Addiction Severity Index (ASI).18–19
Substance use
Self-reports of alcohol and cocaine use were obtained with the Time-line follow-back (TLFB).20 TLFB data have correlated .80 or better with collateral reports and show good agreement with urine test results.21–24 Self-reports of alcohol use in the context of a research study generally have been found to have high validity.25 In addition, urine samples were obtained at baseline and at each follow-up point and tested for cocaine, methamphetamine, barbiturates, and heroin.
Collateral reports of alcohol and drug use were available from 32% of the participants who provided data at the 12 month follow-up. Participants and collaterals agreed in 50.8% of these cases. In 32.8% of the cases, the participant reported alcohol or drug use and the collateral reported no use. In 16.4% of the reports, the participant reported abstinence but the collateral reported some alcohol or drug use. Participants without collaterals did not report less alcohol or cocaine use during the follow-up than those with collaterals.12
Outpatient alcohol treatment and self-help participation
Days of outpatient treatment within each quarter of the follow-up was obtained with the TLFB. Participation in self-help meetings was assessed by the Self-Help Behaviors Questionnaire.26
Subgroup measures
Social support for alcohol use was assessed with the Important People and Activities (IPA) interview.27 Participants nominate up to 10 people in their social network, and indicate how many support or encourage continued alcohol use. Participants were categorized into two groups: 0 (N=178) vs. 1 or more people (N=71). Readiness to change was assessed with the University of Rhode Island Change Assessment Questionnaire (URICA).28 A total score was calculated as the sum of the contemplation, action, and maintenance scores divided by the pre-contemplation score. A median split was used to dichotomize participants into low (N=130) and high (N=122) readiness groups. Prior treatment for alcoholism was assessed with the ASI.18 Participants were categorized into two groups: 0 (N=53) vs. 1 or more prior treatments (N=199). Utilization of inpatient substance use and psychiatric treatment within each quarter of the follow-up was assessed with the TLFB (any inpatient treatment: yes/no).
Outcome Measures
Two alcohol use measures were examined, percent days drinking and any heavy drinking (i.e., 5 or more drinks/day for men, 4 or more drinks/day for women)14 within a given 3-month follow-up period. In addition, participants were categorized as having a good clinical outcome within a given 3 month period if they had: (a) no heavy alcohol use; (b) no more than 15% days of any light drinking (i.e., one day of drinking/week); (c) no self-reported cocaine use; (d) no urine toxicology tests positive for cocaine, methamphetamine, barbiturates, or heroin; and (e) no days of inpatient treatment for psychiatric, alcohol, or drug problems. This new variable was included to provide an indicator of good disease management in a sample of alcohol dependent patients with high rates of co-occurring cocaine and other drug use disorders and multiple prior treatments.
Data Analyses
Differences between the three conditions at baseline and in treatment received were evaluated with kruskal-wallis tests (continuous measures) and chi-square tests (categorical measures). Generalized estimating equations (GEE; SAS PROC GENMOD) were used to compare the continuing care groups on the continuous percent days drinking and binary any heavy drinking and good clinical outcome measures within each 3 month segment of the follow-up. The primary analyses were conducted with the full sample (i.e., intent to treat), and used a compound symmetry/exchangeable covariance structure.
In the analyses to determine main effects, the independent variables in these models were treatment condition, time, treatment by time, and the baseline value of percent days heavy drinking. Hypothesized subgroup effects involving gender, social support, readiness, and prior treatment were each examined in separate analyses with the three outcome measures. The four subgroup variables examined were unrelated, with bi-serial correlations r≤ 0.10. Interactions involving these moderator variables, treatment condition, and time were examined, and differences of least square means were used to test for treatment group differences within specific subgroups. Finally, pattern mixture analyses were conducted to evaluate the potential effects of non-ignorably missing TLFB and urine toxicology data.29 No evidence of bias due to missing data was found in these analyses.
Results
Comparison of Treatment Conditions at Baseline
The continuing care conditions did not differ on 21 demographic, diagnostic, treatment, and problem severity level variables assessed at baseline.12
Participation in Treatment
Participants averaged 36 days of IOP or OP treatment in months 1–6 of the follow-up, with no differences between treatment conditions [F(2,223)= 0.17, p= .84]. Three-quarters of participants in the continuing care conditions initiated participation in the interventions (TM= 77%, TMC= 76%). Participants who initiated the protocols received 11.5 (SD= 9.7) sessions in TM and 9.1 (SD= 9.6) sessions in TMC. About 38% of participants who initiated TMC or TM had at least one session between months 12 and 18.
Main Effect Analysis
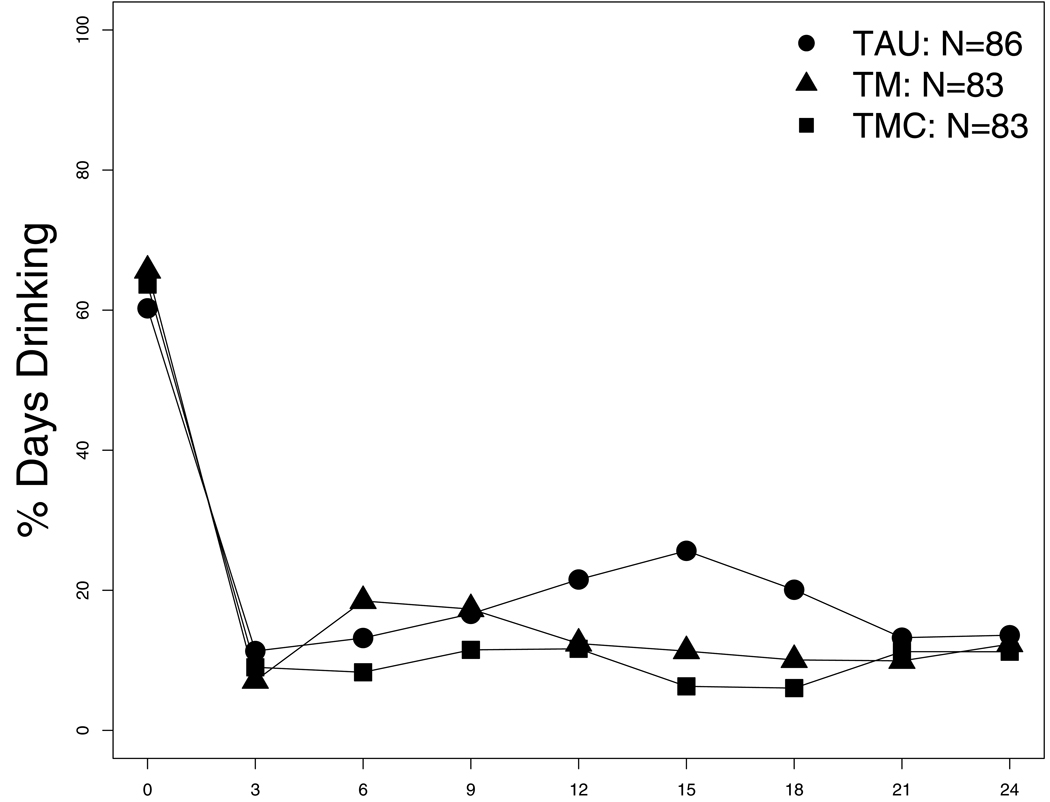
Table 1 indicates that the beneficial effects of TMC over TAU on percent days drinking (but not on heavy drinking or good clinical outcome) remained significant when 21- and 24-month data were included in the analysis. However, Figure 2 shows that effects of the interventions on drinking measures were generally confined to the active intervention period and were no longer apparent after the 18-month follow-up. The exception was on the new measure, good clinical outcome, where rates were consistently (though not significantly) higher in TMC than in TAU throughout the follow-up (Figure 2). For example, rates of good clinical outcome during months 19–24 were 60% in TMC versus 46% in TAU,
Table 1.
Treatment Condition Main Effects over a 24-month follow-up period
| Outcome Measure | Treatment (df=2) |
Month (df=7) |
Treatment × Month (df=14) |
TMC vs. TAU (df=1) |
TM vs. TAU (df=1) |
TMC vs. TM (df=1) |
|---|---|---|---|---|---|---|
| % Days Any Drinking | x2=5.22, p= .07 | x2=9.84, ns | x2=23.62, p= .05 | OR=0.62, x2=5.30, p= .02 | x2=0.80, ns | x2=1.53, ns |
| Any Heavy Drinking | x2=4.15, ns | x2=8.81, ns | x2=20.62, ns | OR=0.63, x2=2.92, p= .09 | x2=0.01, ns | OR=0.61, x2=3.14, p= .08 |
| Good Clinical Outcome | x2=3.47, ns | x2=12.03, ns | x2=8.76, ns | OR=1.57, x2=3.33, p= .07 | x2=0.16, ns | x2=1.85, ns |
Figure 2.
Main effect of percent days drinking (top panel), any heavy drinking (middle panel) and good clinical outcome (bottom panel) in groups receiving aftercare treatment as usual (TAU), Telephone Monitoring (TM) or Telephone Monitoring plus Counseling (TMC) during an 18 week intervention with follow-up to 24 months.
Subgroup Analyses
Treatment condition by moderator variable interactions on each of the three outcome measures, and focused subgroup contrasts that reached the p≤ .10 level of significance, are presented in Table 2. Selected significant subgroup effects on the good clinical outcome measure are depicted in figures 3 and 4.
Table 2.
Subgroup Analyses
| Moderator | Interaction (df=2) |
Group (df=1) |
TMC vs. TAU (df=1) |
TM vs. TAU (df=1) |
TMC vs. TM (df=1) |
|---|---|---|---|---|---|
| Gender | |||||
| % Days Drinking | X2=5.87, p= .053 | Men | -------------- | -------------- | OR=0.63, x2=3.39, p< .07 |
| Women | OR=0.47, x2=4.23, p= .04 | OR=0.44, x2=6.15, p= .01 | -------------- | ||
| Any Heavy Drinking | X2=7.45, p=.024 | Men | -------------- | OR=1.96, x2=4.30, p= .04 | OR=0.41, x2=7.58, p= .006 |
| Women | -------------- | OR=0.40, x2=4.62, p= .03 | -------------- | ||
| Good Clinical Outcome | X2=12.05, p= .003 | Men | -------------- | OR=0.51, x2=4.20, p= .04 | OR=2.03, x2=5.58, p= .02 |
| Women | OR=2.58, x2=3.96, p= .05 | OR=3.55, x2=7.99, p= .005 | -------------- | ||
| Social Support Alcohol | |||||
| % Days Drinking | X2=1.42, ns | No | -------------- | -------------- | -------------- |
| Yes | OR=0.44, x2=5.13, p= .02 | -------------- | -------------- | ||
| Any Heavy Drinking | X2=0.98, ns | No | -------------- | -------------- | -------------- |
| Yes | OR=0.40, x2=3.65, p< .06 | -------------- | -------------- | ||
| Good Clinical Outcome | X2=1.69, ns | No | -------------- | -------------- | -------------- |
| Yes | OR= 2.46, x2=5.25, p= .02 | -------------- | -------------- | ||
| Readiness for Change | |||||
| % Days Drinking | X2=3.81, ns | High | -------------- | -------------- | OR=0.64, x2=2.78, p= .10 |
| Low | OR=0.53, x2=4.59, p= .03 | OR=0.55, x2=3.95, p= .05 | -------------- | ||
| Any Heavy Drinking | X2=3.93, ns | High | -------------- | -------------- | OR=0.42, x2=4.99, p< .03 |
| Low | OR=0.56, x2=2.65, p= .10 | -------------- | -------------- | ||
| Good Clinical Outcome | X2=3.41, ns | High | -------------- | -------------- | -------------- |
| Low | OR=1.97, x2=4.01, p< .05 | -------------- | -------------- | ||
| Prior Alcohol TX | |||||
| % Days Drinking | X2=3.18, ns | No | -------------- | -------------- | -------------- |
| Yes | OR=0.59, x2=5.26, p= .02 | OR=0.67, x2=2.84, p= .09 | -------------- | ||
| Any Heavy Drinking | X2=3.81, ns | No | -------------- | -------------- | OR=0.32, x2=2.67, p= .10 |
| Yes | OR=0.56, x2=4.23, p= .04 | -------------- | -------------- | ||
| Good Clinical Outcome | X2=1.72, ns | No | -------------- | -------------- | -------------- |
| Yes | OR=1.63, x2=3.66, p< .06 | -------------- | -------------- |
Note: Table presents all contrasts that were p≤ .10.
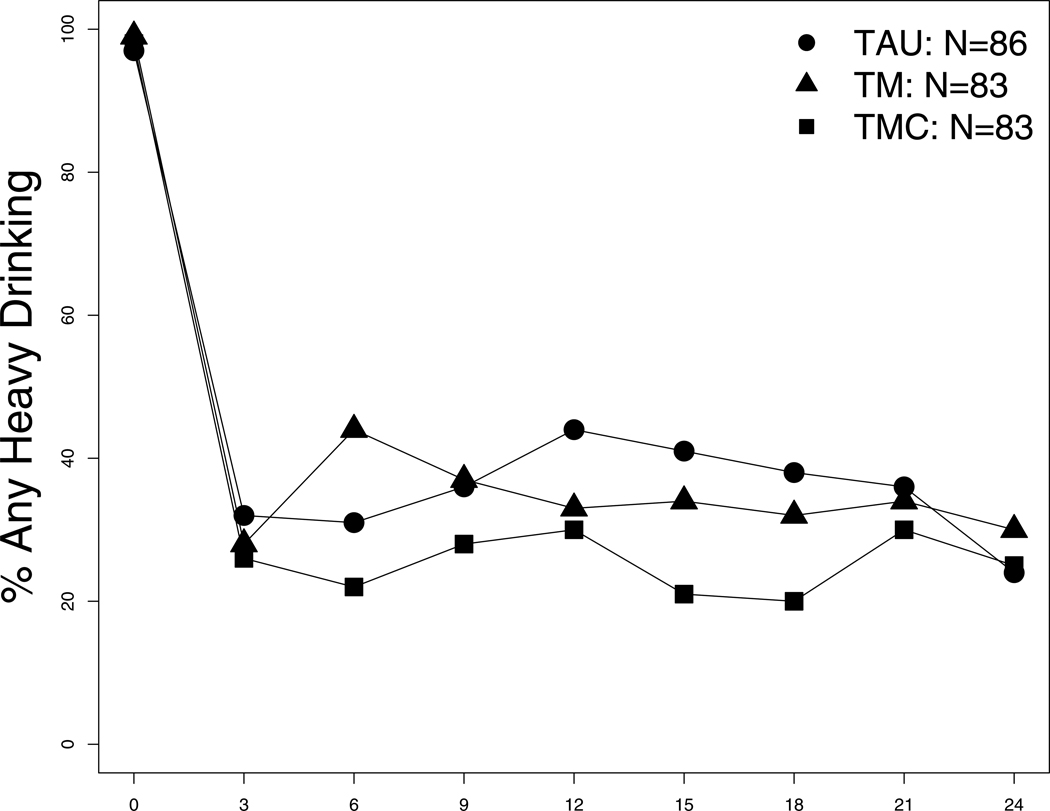
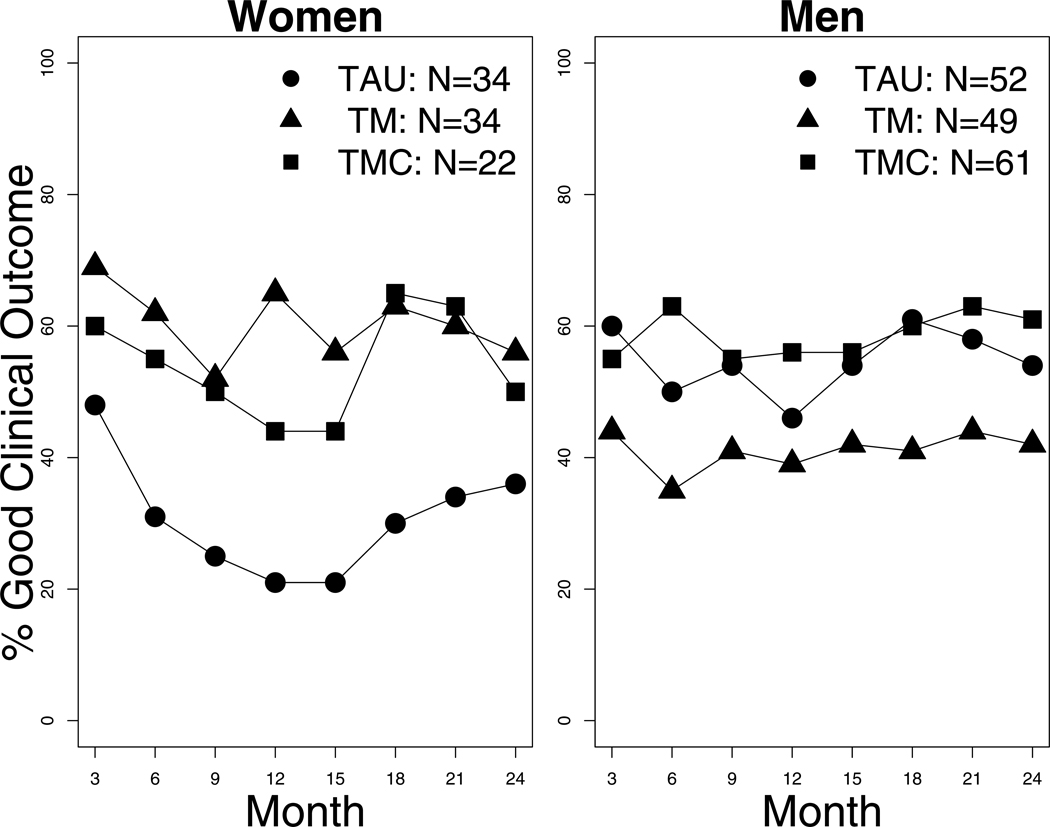
Figure 3.
Rates of good clinical outcomes among women (left panel) and men (right panel) receiving aftercare treatment with TAU, TM, and TMC
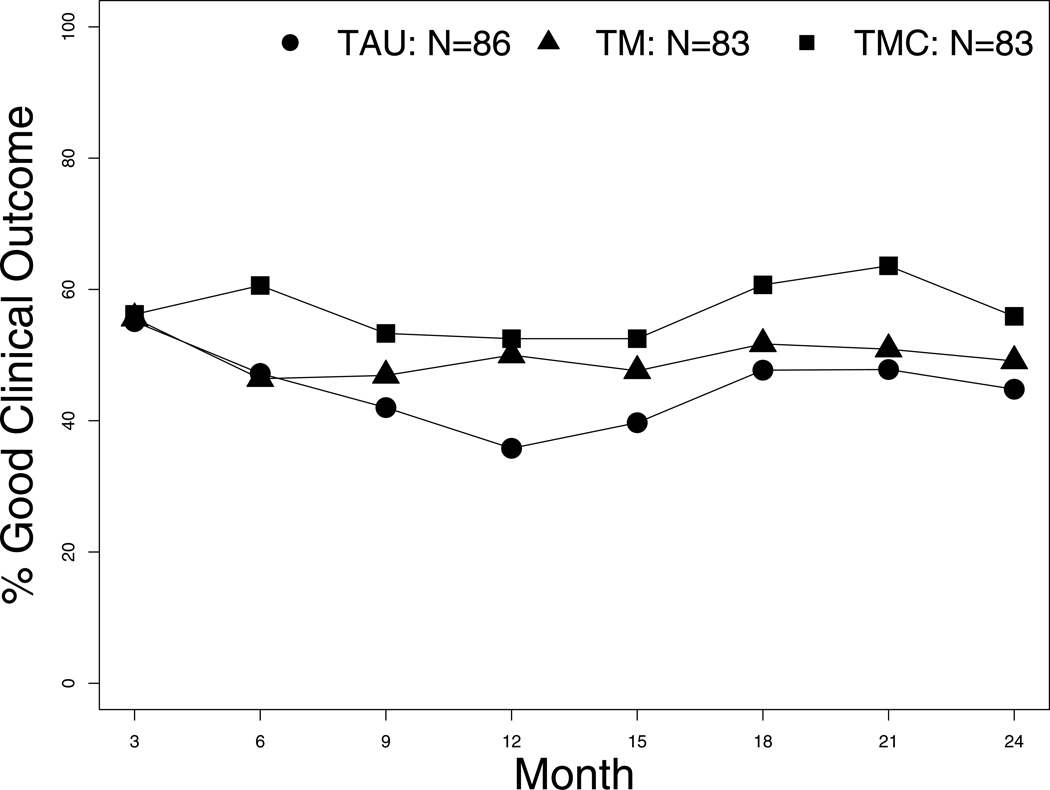
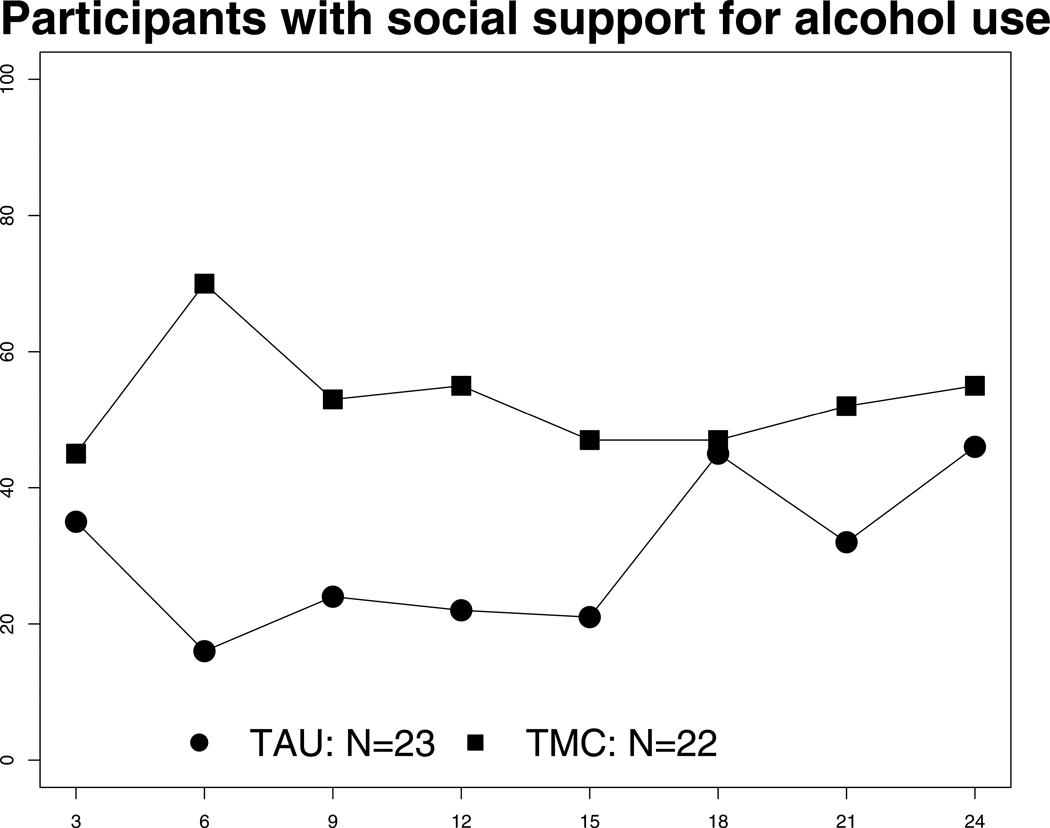
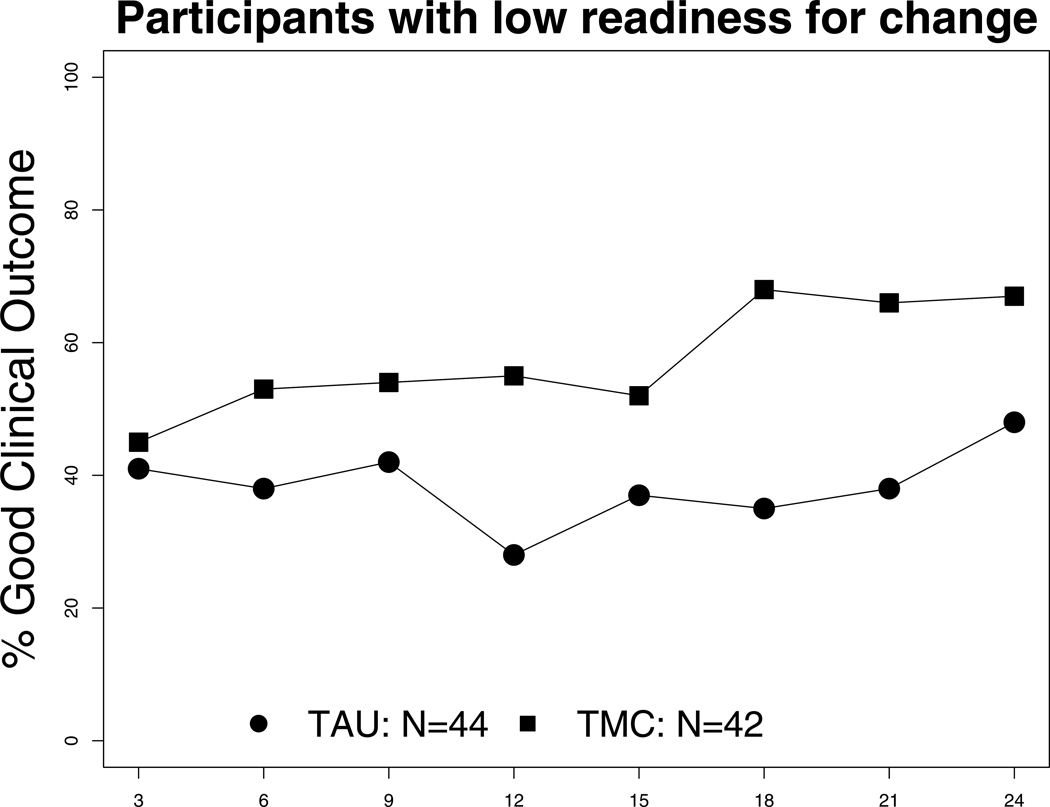
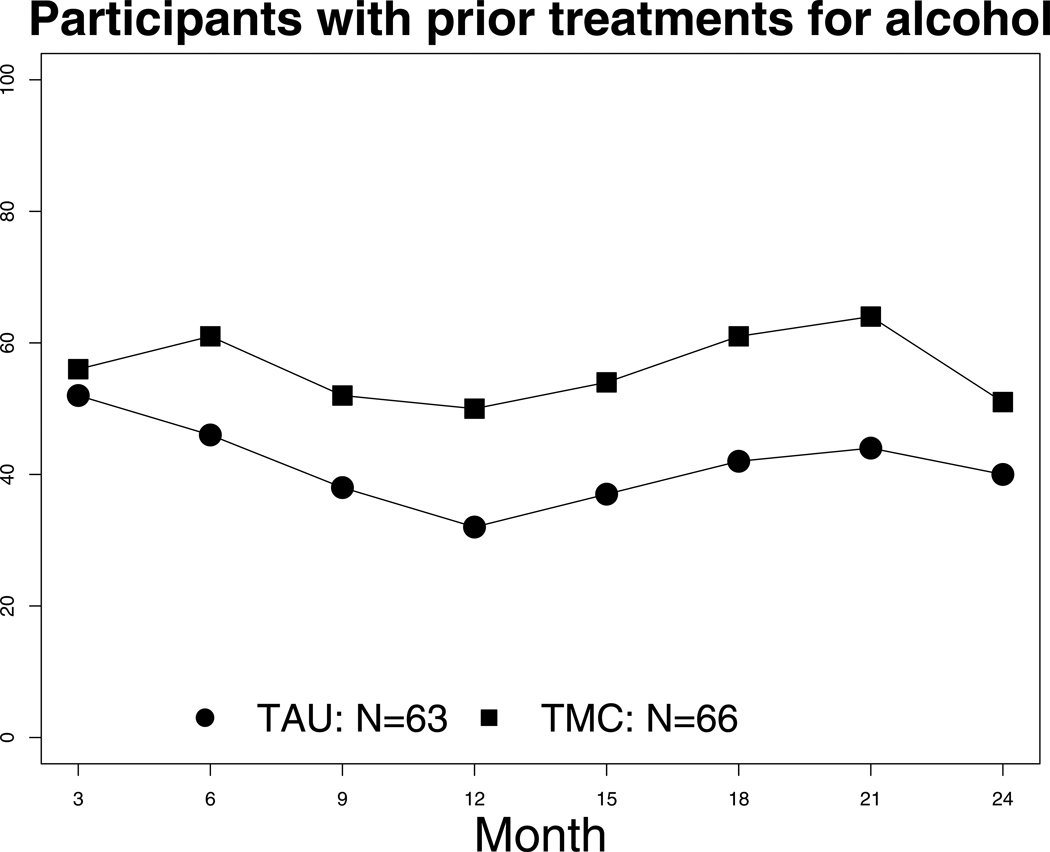
Figure 4.
Rates of good clinical outcome among participants with social support for continued alcohol use (top panel), low readiness for change (middle panel) and prior treatments for alcohol (bottom panel) who received TAU and TMC during the 18 week continuing care intervention.
Gender
Significant or near significant (p = 0.53) interactions between gender and treatment condition were obtained on all drinking outcomes (Table 2). Gender effects on good clinical outcome are presented in Figure 3. In women, both TMC and TM were more effective than TAU for percent days drinking and good clinical outcome measures, while TM was also more effective than TAU on any heavy drinking. The effects favoring TM and TMC over TAU in women were no longer significant by month 24. In men, the TM intervention did poorly, with both TMC and TAU being consistently superior to TM on most outcomes (Table 2, Figure 3). As in women, none of the effects seen in men was significant by month 24
Social network support for continued alcohol use
The interactions between social support for drinking and treatment condition were not significant (Table 2). However, subgroup contrasts presented in Table 2 indicate that for participants with social networks that supported continued alcohol use, TMC was superior to TAU on percent days drinking (p = .02), good clinical outcome (p = .02), and any heavy drinking (p= .056). However, as seen in Figure 4, these effects were no longer present after 15 months. No effects for continuing care were obtained among participants without social support for alcohol use (all p > .10).
Readiness to change
The interactions between readiness to change and treatment condition were not significant (Table 2). However, subgroup contrasts indicated that in participants with lower readiness to change, TMC was superior to TAU on percent days drinking (p = .03), good clinical outcome (p = < .05) and any heavy drinking (p < .06). As seen in Figure 4, the effect favoring TMC over TAU on good clinical outcome was no longer apparent by month 24. In high readiness participants, rates of heavy drinking were lower in TMC than TM, although the effect was no longer significant at the 21 and 24 month follow-ups.
Prior alcohol treatment
The interactions between prior alcohol treatment and treatment condition were not significant (Table 2). However, subgroup contrasts indicated that in participants with prior alcohol treatment, TMC was associated with lower percent days drinking (p = .02), any heavy drinking (p = .04) and good clinical outcome (p= .056) than TAU. However, as seen in Figure 4, which presents data on rates of good clinical outcome, these effects were relatively small in magnitude and no longer apparent by month 24. No effects for continuing care were obtained among participants without prior alcohol treatment (all p> .10).
Supplemental Analyses
Outpatient treatment and self-help participation
The treatment conditions did not differ on days of outpatient substance abuse treatment [x2 (2)= 0.41, p= .81] or on participation in selfhelp programs during the follow-up [x2 (2) = 0.49, p= .78].
Gender differences at baseline
To explore variables that might account for gender differences in treatment response, men and women were contrasted on the 21 variables used to compare treatment conditions at baseline,12 nine scales from the IPA, and additional ASI measures. Women had fewer years of education than men (11.5 vs. 12.0 years, p= .03), but did not differ significantly on rates of current major depression (23.4% vs. 11.5%, p= .08) or employment problem severity (0.87 vs. 0.82, p= .10). Women had lower legal (0.03 vs. 0.09, p< .0001), alcohol (0.25 vs. 0.31, p= .009), and drug (0.08 vs. 0.11, p= .01) ASI problem severity scores than men, and a higher percentage of important people who did not accept or support alcohol use (77.7% vs. 69.7%, p= .05). Moreover, women were less likely to be living with someone with an alcohol (11.1% vs. 21.1%, p= .05) or drug problem (4.4% vs. 13.7%, p= .02). Men and women did not differ on the other baseline measures examined, number of IOP sessions attended in months 1–6, or the other three subgroup variables.
Discussion
In this study, the beneficial effects of telephone-based continuing care provided to patients who had achieved initial engagement in intensive outpatient treatment dissipated after the end of the 18 month intervention. It is possible that extending the duration of the intervention might produce longer lasting results. One of the advantages of telephone continuing care is that it is relatively easy to deliver and could conceivably be kept in place for longer periods of time, especially for those who are likely to derive the most benefit from it.
Some of the larger effects for the two continuing care interventions were in women. Interestingly, one prior study found that telephone recovery support was more effective in women than in men.30 In the present study, these effects were due in part to the particularly poor outcomes of women who received standard care only. Prior research has concluded that men and women generally do not differ on outcomes from alcohol and drug treatment.31–32 However, women may have more severe problems than men at intake,33–34 which in some cases could contribute to worse outcomes.31 In this study, women had fewer years of education than men, but generally did not have greater problem severity at baseline, either in the full sample or in those who received TAU. Therefore, it is not clear why women in TAU had such bad outcomes. The reasons for the relatively poor performance of men in TM also remain to be determined.
The mechanisms by which TMC was helpful to higher risk patients have not yet been formally examined. The extended support and assistance with problem solving may have helped to shore up or otherwise counteract low motivation while also facilitating the development of strategies to deal with friends or relatives who encouraged continued drinking, thereby reducing relapse rates and the need for inpatient treatment. In addition, the extended relationship with the counselor provided further social support for recovery. Increasing social network support for abstinence by as few as one person can improve alcohol use outcomes.15
Study Limitations
Some of the analyses that missed statistical significance may have been significant with a larger sample. The results of the subgroup analyses should be interpreted with some caution, due to the small samples sizes in some of the groups examined. In addition, these analyses were retrospective, and need confirmation in prospective designs. Other limitations of the study have been described elsewhere.12
Final Conclusions
Findings from this comparative effectiveness study indicated that adding TMC to standard care improved drinking outcomes for 18 months12, but that effects on drinking did not persist beyond that point. Significant effects of a more substantial magnitude were found with women (TM and TMC over TAU) and individuals with lower readiness to change when they entered continuing care (TMC over TAU). TMC was also significantly more effective than TAU for individuals with social networks that supported continued drinking and those with prior alcohol treatments, although these subgroup effects were not generally sustained beyond 18 months. Therefore, although this study of telephone continuing care provides further support for the positive effects of extended treatment on alcohol use and on rates of overall good clinical outcome for high risk substance dependent patients,35–40 the results suggest that the benefits of the interventions may be limited to certain patients and effects may not persist beyond the end of treatment.
Acknowledgements
This research was supported by grants R01AA14850 and P01AA016821 from the National Institute on Alcohol Abuse and Alcoholism, and grants K02 DA000361 and K24 DA029062 from the National Institute on Drug Abuse. Additional support was provided by the Department of Veterans Affairs. These agencies were not involved in the design and conduct of the study; collection, management, analysis, or interpretation of the data; or the preparation, review, or approval of the manuscript. Dr. McKay had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. We thank the management and staffs of the two treatment programs that participated in this study, North-East Treatment (NET) Centers and Presbyterian Hospital.
Footnotes
Megan Ivey, Donna Coviello, Qin Yu, and Kevin G. Lynch report no conflicts of interest and no financial disclosures. Drs. McKay and Drapkin have provided consultation in telephonic continuing care to Altarum, which has provided technical assistance to SAMHSA state grantees. Drs. McKay and Van Horn are authors of a manual for delivering telephone based continuing care, which has been published by Hazelden. Dr. McKay has also provided consultation to investigators at Wright State University, Columbia University, and the University of Wisconsin who have received NIH grants to study other approaches to disease management in the addictions, and was a consultant to the National Quality Forum on the development of a White Paper on the measurement of continuing care management in the addictions. Dr. McKay also consults to Caron Treatment Centers on ways to improve continuing care. Dr. Van Horn has provided training in, or has received a fee or honorarium to speak about, treatment for substance use disorders at 23 organizations from the start of the present study up through publication. She is owner of Deborah H.A. Van Horn, PhD, LLC, which has provided continuing education courses to health care professionals treating substance use disorders. None of the training, speaking engagements, or courses focused on the intervention models are tested in the present study. Dr. Oslin’s research is supported by grants from Hazelden, the Commonwealth of Pennsylvania, the Department of Veterans Affairs, and the NIH.
References
- 1.McKay JR. Treating substance use disorders with adaptive continuing care. Washington DC: American Psychological Association; 2009. [Google Scholar]
- 2.Humphreys K, Tucker JA. Toward more responsive and effective intervention systems for alcohol-related problems. Addiction. 2002;97:126–132. doi: 10.1046/j.1360-0443.2002.00004.x. [DOI] [PubMed] [Google Scholar]
- 3.McKay JR. Continuing care research: What we've learned and where we're going. Journal of Substance Abuse Treatment. 2009;36:131–145. doi: 10.1016/j.jsat.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miller WR, Weisner C. Integrated care. In: Miller WR, Weisner CM, editors. Changing substance abuse through health and social systems. New York: Kluwer Academic/Plenum; 2002. pp. 243–253. [Google Scholar]
- 5.Hser YI, Longshore D, Anglin MD. The life course perspective on drug use: a conceptual framework for understanding drug use trajectories. Evaluation Review: A Journal of Applied Social Research. 2007;31:515–547. doi: 10.1177/0193841X07307316. [DOI] [PubMed] [Google Scholar]
- 6.McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: Implications for treatment, insurance, and outcomes evaluation. Journal of the American Medical Association. 2000;284:1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- 7.Dennis ML, Scott CK. Managing addiction as a chronic condition. Addiction Science and Clinical Practice. 2007 December;:45–55. doi: 10.1151/ascp074145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Horng F, Chueh K. Effectiveness of telephone follow-up and counseling in aftercare for alcoholism. Journal of Nursing Research. 2004;12:11–19. doi: 10.1097/01.jnr.0000387484.40568.bb. [DOI] [PubMed] [Google Scholar]
- 9.McKay JR, Lynch KG, Shepard DS, Pettinati M. The effectiveness of telephone based continuing care for alcohol and cocaine dependence: 24 month outcomes. Archives of General Psychiatry. 2005;62:199–207. doi: 10.1001/archpsyc.62.2.199. [DOI] [PubMed] [Google Scholar]
- 10.Connors GJ, Tarbox AR, Faillace LA. Achieving and maintaining gains among problem drinkers: Process and outcome results. Behavior Therapy. 1992;23:449–474. [Google Scholar]
- 11.Hubbard RL, Leimberger JD, Haynes L, Patkar AA, Holter J, Liepman MR, et al. Telephone enhancement of long-term engagement (TELE) in continuing care for substance abuse treatment: A NIDA Clinical Trials Network study. American Journal on Addictions. 2007;16:495–502. doi: 10.1080/10550490701641678. [DOI] [PubMed] [Google Scholar]
- 12.McKay JR, Van Horn D, Oslin D, Lynch KG, Ivey M, Ward K, Drapkin M, Becher J, Coviello D. A randomized trial of extended telephone-based continuing care for alcohol dependence: Within treatment substance use outcomes. Journal of Consulting and Clinical Psychology. 2010;78:111–120. doi: 10.1037/a0020700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lynch KG, Van Horn D, Drapkin M, Ivey M, Coviello D, McKay JR. Moderators of response to extended telephone continuing care for alcoholism. American Journal of Health Behavior. 2010;34:788–800. doi: 10.5993/ajhb.34.6.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Falk D, Wang XQ, Liu L, Fertig J, Mattson M, Ryan M, Johnson B, Stout R, Litten RZ. Percentage of subjects with no heavy drinking days: Evaluation as an efficacy endpoint for alcohol clinical trials. Alcohol Clin Exp Res. 2010;34:2022–2034. doi: 10.1111/j.1530-0277.2010.01290.x. [DOI] [PubMed] [Google Scholar]
- 15.Litt MD, Kadden RM, Kabela-Cormier E, Petry NM. Changing network support for drinking: Network support project 2-year follow-up. Journal of Consulting and Clinical Psychology. 2009;77:229–242. doi: 10.1037/a0015252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Project Match Research Group. Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. Journal of Studies of Studies on Alcoholism. 1997;58:7–29. [PubMed] [Google Scholar]
- 17.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders—patient edition (SCID-I/P, version 2.0) NY: Biometrics Research Department, New York State Psychiatric Institute; 2006. [Google Scholar]
- 18.McLellan AT, Luborsky L, Woody GE, O'Brien CP. An improved diagnostic evaluation instrument for substance abuse patients: The Addiction Severity Index. Journal of Nervous and Mental Disease. 1980;168:26–33. doi: 10.1097/00005053-198001000-00006. [DOI] [PubMed] [Google Scholar]
- 19.McLellan AT, Luborsky L, Cacciola J, Griffith J, Evans F, Barr H, O'Brien CP. New data from the Addiction Severity Index: Reliability and validity in three centers. Journal of Nervous and Mental Disease. 1985;173:412–423. doi: 10.1097/00005053-198507000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Sobell LC, Maisto SA, Sobell MB, Cooper AM. Reliability of alcohol abusers' self-reports of drinking behavior. Behavior Research and Therapy. 1987;17:157–160. doi: 10.1016/0005-7967(79)90025-1. [DOI] [PubMed] [Google Scholar]
- 21.Maisto SA, Sobell LC, Sobell MB. Comparison of alcoholics' self-reports of drinking behavior with reports of collateral informants. Journal of Consulting and Clinical Psychology. 1979;47:106–122. [PubMed] [Google Scholar]
- 22.Stout RL, Beattie MC, Longabaugh R, Noel N. Factors affecting correspondence between patient and significant other reports of drinking [abstract] Alcoholism: Clinical and Experimental Research. 1989;12:336. [Google Scholar]
- 23.Ehrman RN, Robbins SJ. Reliability and validity of six-month timeline reports of cocaine and heroin use in a methadone population. Journal of Consulting and Clinical Psychology. 1994;62:843–850. doi: 10.1037//0022-006x.62.4.843. [DOI] [PubMed] [Google Scholar]
- 24.Fals-Stewart W, O’Farrell TJ, Freitas TT, McFarlin SK, Rutigliano P. The timeline follow-back reports of psychoactive substance use by drug-abusing patients: Psychometric properties. Journal of Consulting and Clinical Psychology. 2000;68:134–144. doi: 10.1037//0022-006x.68.1.134. [DOI] [PubMed] [Google Scholar]
- 25.Babor TF, Steinberg K, Anton R, Del Boca F. Talk is cheap: Measuring drinking outcomes in clinical trials. Journal of Studies on Alcohol. 2000;61:55–63. doi: 10.15288/jsa.2000.61.55. [DOI] [PubMed] [Google Scholar]
- 26.McKay JR, Alterman AI, McLellan AT, Snider E. Treatment goals, continuity of care, and outcome in a day hospital substance abuse rehabilitation program. American Journal of Psychiatry. 1994;15:254–259. doi: 10.1176/ajp.151.2.254. [DOI] [PubMed] [Google Scholar]
- 27.Zywiak WH, Neighbors CJ, Martin RA, Johnson JE, Eaton CA, Rohsenow DJ. The important people drug and alcohol interview: Psychometric properties, predictive validity, and implications for treatment. Journal of Substance Abuse Treatment. 2009;36:321–330. doi: 10.1016/j.jsat.2008.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Prochaska JO, DiClemente CC. The transtheoretical approach: Crossing traditional boundaries of therapy. Homewood, IL: Dow Jones, Irwin; 1984. [Google Scholar]
- 29.Hedeker D, Gibbons R. Applications of random-effects pattern-mixture models for missing data in longitudinal studies. Psychological Methods. 1997;2:64–78. [Google Scholar]
- 30.Carter RE, Haynes LF, Back SE, Herrin AE, Brady KT, Leimberger JD, Sonne SC, Hubbard RL, Liepman MR. Improving the transition from residential to outpatient addiction treatment: Gender differences in response to supportive telephone calls. American Journal of Drug and Alcohol Abuse. 2008;34:47–59. doi: 10.1080/00952990701764599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Green CA. Gender and use of substance abuse treatment services. Alcohol Research and Health. 2006;29:55–62. [PMC free article] [PubMed] [Google Scholar]
- 32.Greenfield SF, Brooks AJ, Gordon SM, Green CA, Kropp F, McHugh RK, Lincoln M, Hien D, Miele GM. Substance abuse treatment entry, retention, and outcome in women: A review of the literature. Drug and Alcohol Dependence. 2007;86:1–21. doi: 10.1016/j.drugalcdep.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Arfken CL, Klein C, di Menza S, Schuster CR. Gender differences in problem severity at assessment and treatment retention. Journal of Substance Abuse Treatment. 2001;20:53–57. doi: 10.1016/s0740-5472(00)00155-0. [DOI] [PubMed] [Google Scholar]
- 34.Hernandez-Avila CA, Rounsaville BJ, Kranzler HR. Opiod-, cannabis- and alcohol-dependent women show more rapid progression to substance abuse treatment. Drug and Alcohol Dependence. 2004;74:265–272. doi: 10.1016/j.drugalcdep.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 35.McLellan AT, Skipper GS, Campbell M, DuPont RL. Five-year outcomes in a cohort study of physicians treated for substance use disorders in the United States. BMJ. 2008;337:a2038. doi: 10.1136/bmj.a2038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Morgenstern J, Blanchard KA, McCrady BS, McVeigh KH, Morgan TJ, Pandina RJ. Effectiveness of intensive case management for substance-dependent women receiving temporary assistance for needy families. American Journal of Public Health. 2006;96:2016–2023. doi: 10.2105/AJPH.2005.076380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Morgenstern J, Hogue A, Dauber S, Dasaro C, McKay JR. Does coordinated care management improve employment for substance using welfare recipients? Journal of Studies on Alcohol and Drugs. 2009;70:955–963. doi: 10.15288/jsad.2009.70.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Scott CK, Dennis ML. Results from two randomized clinical trials evaluating the impact of quarterly recovery management checkups with adult chronic substance users. Addiction. 2009;104:959–971. doi: 10.1111/j.1360-0443.2009.02525.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Silverman K, Svikis D, Wong CJ, Hampton J, Stitzer ML, Bigelow GE. A reinforcement-based therapeutic workplace for the treatment of drug abuse: Three-year abstinence outcomes. Experimental and Clinical Psychopharmacology. 2002;10:228–240. doi: 10.1037//1064-1297.10.3.228. [DOI] [PubMed] [Google Scholar]
- 40.Willenbring ML, Olson DH. A randomized trial of integrated outpatient treatment for medically ill alcoholic men. Archives of Internal Medicine. 1999;159:1946–1952. doi: 10.1001/archinte.159.16.1946. [DOI] [PubMed] [Google Scholar]