Abstract
Objective
To determine the proportion of emergency department (ED) patients who have been tested for human immunodeficiency virus (HIV) infection and assess if patient history of HIV testing varies according to patient demographic characteristics.
Design
From July 2005–July 2006, a random sample of 18–55-year-old English-speaking patients being treated for sub-critical injury or illness at a northeastern US ED were interviewed on their history of HIV testing. Logistic regression models were created to compare patients by their history of being tested for HIV according to their demography. Odds ratios (ORs) with 95% confidence intervals (CIs) were estimated.
Results
Of 2107 patients surveyed who were not known to be HIV-infected, the median age was 32 years; 54% were male, 71% were white, and 45% were single/never married; 49% had private health-care insurance and 45% had never been tested for HIV. Of the 946 never previously tested for HIV, 56.1% did not consider themselves at risk for HIV. In multivariable logistic regression analyses, those less likely to have been HIV tested were male (OR: 1.32 [1.37–2.73]), white (OR: 1.93 [1.37–2.73]), married (OR: 1.53 [1.12–2.08]), and had private health-care insurance (OR: 2.10 [1.69–2.61]). There was a U-shaped relationship between age and history of being tested for HIV; younger and older patients were less likely to have been tested. History of HIV testing and years of formal education were not related.
Conclusion
Almost half of ED patients surveyed had never been tested for HIV. Certain demographic groups are being missed though HIV diagnostic testing and screening programmes in other settings. These groups could potentially be reached through universal screening.
INTRODUCTION
In 2006, the US Centers for Disease Control and Prevention (CDC) recommended that universal, routine screening for human immunodeficiency virus (HIV) infection be performed in health-care settings, including emergency departments (EDs), for all 13–64-year-olds regardless of their apparent risks for an HIV infection.1 CDC considers HIV screening to be justifiable because it is a serious health disorder that can be diagnosed among asymptomatic persons; HIV can be accurately detected through testing; those identified through screening can receive treatment that can reduce mortality and morbidity; and the costs of screening are reasonable in comparison with the benefits of screening.1 According to the National Health Interview Survey, there are marked differences across demographic groups with regard to history of ever having been tested for HIV.2 Males, whites, older adults, those who had never been married, and with private health insurance are less likely to have been tested for HIV. CDC advocated enhanced HIV screening in EDs and other health-care settings because prior risk- and demographic characteristic-based HIV screening and HIV diagnostic testing efforts have failed to identify an estimated 250–300,000 people in the US who are unaware of their infection.1 These efforts have created untested pockets of people who could be sources of infection for the remainder of the population.
EDs might be ideal venues in which to conduct en masse HIV screening programmes. Many US EDs provide medical care to people without regular access to medical care who might not be screened for HIV elsewhere.3,4 Researchers have demonstrated that EDs in some communities provide medical care to patients at higher risk for HIV;5,6 that the prevalence of HIV among ED patients is frequently higher than other settings in the surrounding communities they serve;7–12 and that EDs can successfully conduct HIV screening programmes, identify HIV-infected persons, and link these persons to appropriate medical care.13–19 There are no current published estimates of what proportion of ED patients have ever been tested for HIV and when they were last tested.20 The reasons why some ED patients have never been tested is also not known. These reasons may impact the success of ED-based HIV screening efforts. It also is not yet known if HIV testing histories among ED patients vary according to demographic characteristics. Knowing which patients are more likely to never have been tested for HIV would be helpful in designing interventions to improve uptake of ED-based HIV screening. Demographic variations in HIV-testing history could also lend support to the call for universal HIV screening in EDs.
We surveyed a random sample of ED patients on their history of being tested for HIV, the time elapsed since their last HIV test, and the main reason for their last test or main reason for never having been tested for HIV. The primary objective was to learn what proportion of ED patients had ever been tested for HIV. The secondary objective was to determine if history of HIV testing, reasons for previous HIV testing, and reasons for never having been tested for HIV differ by ED patient demography.
METHODS
Study design and setting
From July 2005 to July 2006, we randomly selected 18–55-year-old patients at an adult ED in New England and surveyed them about their history of HIV testing. As reported previously, the study authors developed a questionnaire to assess patient history of HIV testing, performed cognitive-based assessments, and conducted pilot testing of the questionnaire.21,22 The questionnaire queried participants about their history of HIV testing, reasons for their last HIV test, reasons for never having been tested for HIV, the time elapsed since their last HIV test, and type of their last HIV test. The hospital institutional review board approved the study.
Participant selection and data collection
As outlined in a prior publication, the dates on which the study was conducted each month, the shifts during which the research assistants (RAs) enrolled patients for the study, and the patients assessed for possible inclusion in the study were randomly selected.21 RAs assessed the eligibility of ED patients randomly selected for possible inclusion in the study by reviewing their ED patient medical record and through an in-person assessment. The RAs administered the questionnaire to those who agreed to be assessed and were eligible for the study. Patients whose ED medical record noted that they were HIV-infected were not interviewed. Patients eligible for the study were aged 18–55 years, English-speaking, did not have a mental or physical disability that would preclude them from participating in the research study, were not prison inmates, not pregnant, not critically ill or injured, not presenting for an acute psychiatric illness, and not participating in an HIV vaccine trial. Only 18–55-year-old patients were included because data from the State Department of Health indicated that 95% of the new HIV infections were occurring in patients of this age group.23 The study was completed prior to the CDC’s recommendation for HIV screening until age 64.24
Data analysis
Summary statistics for the responses to the questions on patient demography and HIV-testing history were calculated. The percentage of participants who had never been tested for HIV was calculated by each demographic characteristic. The association between participant demographic characteristics and history of previous HIV testing was assessed through bivariate analyses using Pearson’s χ2 and Wilcoxon rank-sum tests. Differences were considered significant at the α = 0.05 level.
Logistic regression models were constructed to explore the relationship between participant demographic characteristics and the outcome of a history of never having been tested for HIV. Demographic characteristics identified through the bivariate analyses as being associated with a history of never having been tested for HIV were employed in the logistic regression analyses. Demographic groups with the highest percentage of people previously tested for HIV were the reference groups for these models. Multivariable logistic regression models were formed using demographic characteristic variables associated with the outcome in univariable analyses. Odds ratios (ORs) with corresponding 95% confidence intervals (CIs) were estimated. The predicted probabilities of never having been tested for HIV were calculated using the multivariable logistic model according to participant age, gender, and race/ethnicity.
The responses to questions asking for the reason for the participant’s last HIV test or for their reason for never having been tested for HIV were grouped into categories and summarized. Two multivariable, multinomial regression models were created. The first model included patients who had previously been tested for HIV and examined the association between their demographic characteristics and the main reason for their last test. A requirement to be tested was the base outcome selected for this model. The purpose of this multinomial model was to determine which participants were more or less likely to have been required to be tested for HIV, compared with some other reason for being tested. In the second model, participants who had never been tested for HIV were included. This model examined the association between their demographic characteristics and the main reason for not having been tested for HIV. Believing oneself not to be at risk was the base outcome for this model. The purpose of this multinomial model was to determine which participants were more or less likely not to have been tested for HIV out of a belief that they were not at risk for an HIV infection, compared with other reasons for not having been tested for HIV. Dichotomized versions of participant demographic characteristics were employed for the multinomial models. Demographic groups identified in the bivariate analyses as being less likely to have been tested for HIV were compared with those more likely to have been tested for HIV. Relative risks (RRs) with 95% CIs were estimated for each model.
RESULTS
HIV-testing history
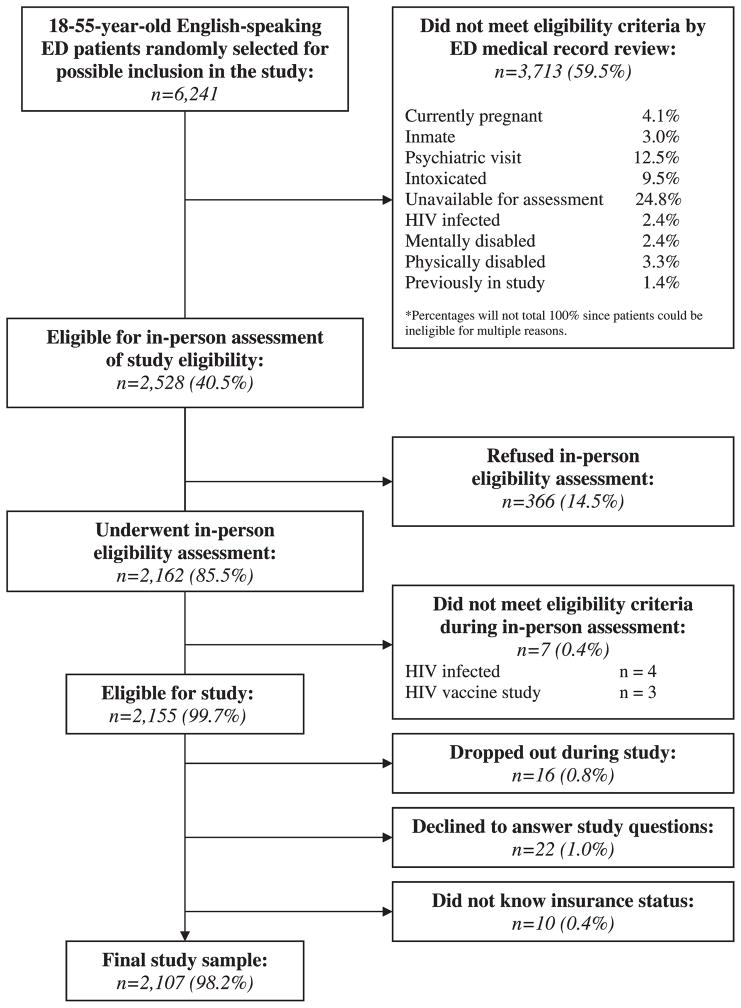
Figure 1 depicts the results of the study eligibility assessment and enrolment process. Of the 6241 18–55-year-old English-speaking patients whose ED medical records were reviewed, 2.4% were documented by the ED clinicians as being HIV-infected. During the in-person eligibility assessments, an additional four patients informed the RA that they were HIV-infected.
Figure 1.
Eligibility assessment and enrolment diagram
Of the 2107 study participants, 54.5% knew that they had previously been tested for HIV not as a part of a blood donation. An additional 22 people indicated that they had previously been tested for HIV as a part of a blood donation. Of those previously tested for HIV not as part of a blood donation, 42.5% had been tested within the previous year and 93.1% had undergone conventional/standard HIV blood testing.
HIV testing history and study participant demography
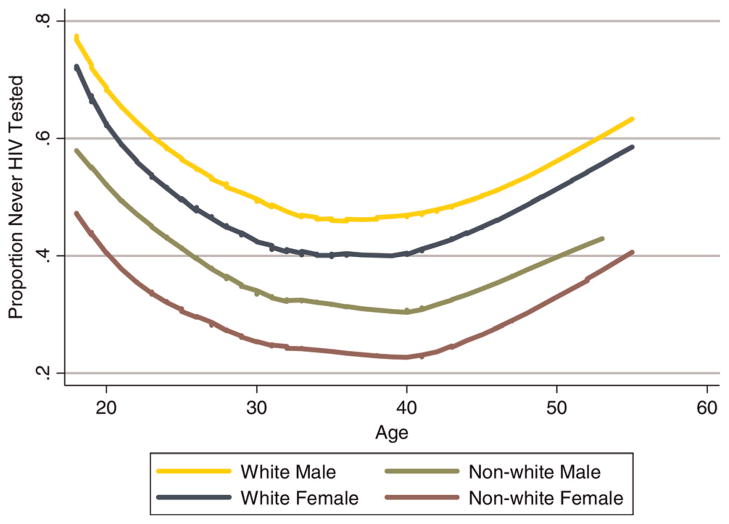
In the bivariate analyses, prior HIV testing was associated with age, gender, race, marital status, and health-care insurance status, but was not associated with years of formal education (Table 1). There was a U-shaped relationship between age and prior HIV testing; testing was highest for 32–36-year-old participants and lowest for those aged 18–21 and 52–55 years. As shown in Table 2, participants who were male, white, married, single/never married/not partnered and those who had private health-care insurance were more likely never to have been tested for HIV, compared with the reference groups. The multivariable logistic regression analyses also showed a curvilinear relationship between age and never having been tested: both younger and older adults were less likely to have been tested for HIV. As shown in Figure 2, the probability of having been tested was lowest among white males and younger adults and was highest among non-white females and for adults around 39 years old. White 18-year-old males had the highest probability of having never been tested for HIV, while non-white 39-year-old females had the highest probability of having been tested for HIV.
Table 1.
Demographic characteristics by HIV-testing history
| All study participants | Never HIV tested | Previously HIV tested | P-value | Participants never previously HIV tested by demographic factor | ||
|---|---|---|---|---|---|---|
| n = 2107 | n = 941 | n = 1166 | ||||
| Median age (range) | 32 (18–55) | 30 (18–55) | 33 (18–55) | <0.001 | ||
| (%) | (%) | (%) | n | (%) | ||
| Age (categorical) | ||||||
| 18–21 | 15.7 | 22.3 | 10.3 | 330 | 63.6 | |
| 22–26 | 19.0 | 18.1 | 19.7 | 400 | 42.5 | |
| 27–31 | 14.2 | 12.9 | 15.4 | 300 | 40.3 | |
| 32–36 | 12.1 | 9.1 | 14.4 | 254 | 33.9 | |
| 37–41 | 12.3 | 9.8 | 14.3 | 259 | 35.5 | |
| 42–46 | 12.9 | 11.8 | 13.8 | 272 | 40.8 | |
| 47–51 | 9.3 | 10.3 | 8.5 | 196 | 49.5 | |
| 52–55 | 4.5 | 5.7 | 3.6 | 96 | 56.3 | |
| Gender | <0.001 | |||||
| Female | 45.4 | 50.7 | 57.6 | 1149 | 41.5 | |
| Male | 54.5 | 49.3 | 42.3 | 957 | 48.5 | |
| Transgender | 0.1 | 0 | 0.1 | 1 | 0.0 | |
| Ethnicity/race | <0.001 | |||||
| White | 70.7 | 78.7 | 64.1 | 1489 | 49.7 | |
| Black | 17.6 | 13.0 | 21.3 | 370 | 33.0 | |
| Hispanic | 9.3 | 6.2 | 11.9 | 197 | 29.4 | |
| Other | 2.4 | 2.1 | 2.7 | 51 | 39.2 | |
| Partner status | <0.001 | |||||
| Married | 28.2 | 30.9 | 26.1 | 595 | 48.9 | |
| Divorced/Widowed/Separated | 14.4 | 10.9 | 17.2 | 304 | 33.9 | |
| Single/Never married | 44.6 | 48.5 | 41.5 | 940 | 48.5 | |
| Unmarried couple | 12.7 | 9.7 | 15.2 | 268 | 34.0 | |
| Health-care insurance status | <0.001 | |||||
| Private | 49.4 | 61.5 | 39.6 | 1041 | 55.6 | |
| Governmental* | 32.0 | 22.8 | 39.5 | 674 | 31.8 | |
| None | 18.6 | 15.7 | 20.9 | 392 | 37.8 | |
| Education | <0.079 | |||||
| College 4 or more years | 14.1 | 15.0 | 13.4 | 297 | 47.5 | |
| College 1–3 years | 29.3 | 29.9 | 28.9 | 618 | 45.5 | |
| High school graduate/GED† | 35.2 | 36.5 | 34.1 | 742 | 46.4 | |
| Grades 9–11 | 18.1 | 15.5 | 20.2 | 381 | 38.3 | |
| Grades 1–8 | 3.3 | 3.1 | 3.4 | 69 | 42.0 | |
Medicaid, Medicare, US military, hospital-sponsored medical care;
General Equivalence Degree
Table 2.
Logistic regression analysis of covariates of HIV-testing history
| n = 2106* | Univariable analysis | Multivariable analysis |
|---|---|---|
| OR (95% CI) | OR (95% CI) | |
| Age (categorical) | ||
| 18–21 | 1.00 | 1.00 |
| 22–26 | 0.42 (0.31–0.57) | 0.42 (0.31–0.58) |
| 27–31 | 0.39 (0.28–0.53) | 0.41 (0.29–0.59) |
| 32–36 | 0.29 (0.21–0.41) | 0.28 (0.19–0.41) |
| 37–41 | 0.32 (0.23–0.44) | 0.32 (0.22–0.47) |
| 42–46 | 0.39 (0.28–0.55) | 0.39 (0.27–0.57) |
| 47–51 | 0.56 (0.39–0.80) | 0.51 (0.34–0.78) |
| 52–55 | 0.73 (0.46–1.17) | 0.69 (0.41–1.15) |
| Gender | ||
| Female | 1.00 | 1.00 |
| Male | 1.33 (1.12–1.58) | 1.32 (1.10–1.60) |
| Ethnicity/race | ||
| Hispanic | 1.00 | 1.00 |
| White | 2.38 (1.72–3.28) | 1.93 (1.37–2.73) |
| Black | 1.18 (0.81–1.72) | 1.03 (0.69–1.53) |
| Other | 1.55 (0.82–2.93) | 1.45 (0.74–2.84) |
| Partner status | ||
| Divorced/widowed/separated | 1.00 | 1.00 |
| Married | 1.89 (1.40–2.49) | 1.53 (1.12–2.08) |
| Single/never married | 1.84 (1.41–2.41) | 1.46 (1.06–2.02) |
| Unmarried couple | 1.00 (0.71–1.42) | 0.95 (0.66–1.39) |
| Health-care insurance status | ||
| Governmental | 1.00 | 1.00 |
| Private | 2.69 (2.19–3.29) | 2.10 (1.69–2.61) |
| None | 1.30 (1.00–1.69) | 1.09 (0.83–1.44) |
Excludes the participant who was transgendered
Figure 2.
Predicted probabilities of never having been tested for HIV
Main reason for last HIV test or main reason for never having had an HIV test
Among the 1095 participants previously tested for HIV, 13.1% reported that their last test was required by the military, judicial system, or another group; 27.5% had wanted to know their HIV status; 37.4% were tested because of a medical examination, illness or because of pregnancy; 17.8% had been tested because of a possible exposure to HIV; and 4.2% for other reasons. As shown in Table 3, those aged 39 years and younger were more likely to be tested because they wanted to know their HIV status or because of a medical examination, illness or pregnancy than because of a requirement to be tested. Males were more likely than females to have been required to be tested for the last HIV test. Married participants were more likely to have been tested because they had been required to do so than out of a desire to know their HIV status.
Table 3.
Demographic and HIV Testing History factors associated with reasons for the last or never having had an HIV test multivariable multinomial regression
| Age ≥40 vs. Age <40 | Male vs. Female | White vs. Non-white | Married vs. Non-married | Private vs. Non-private | .12 vs. ≤12 yrs of education | |
|---|---|---|---|---|---|---|
| RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | |
| Reasons for last HIV test | ||||||
| n = 1165* | ||||||
| Required | Base outcome | Base outcome | Base outcome | Base outcome | Base outcome | Base outcome |
| Wanted to know | 0.56 (0.37–0.86) | 0.26 (0.17–0.41) | 0.89 (0.57–1.39) | 0.47 (0.28–0.80) | 1.22 (0.75–1.99) | 1.26 (0.79–2.02) |
| Medical Exam/Illness/Pregnancy | 0.53 (0.35–0.80) | 0.15 (0.10–0.24) | 0.76 (0.50–1.17) | 1.23 (0.76–1.99) | 1.10 (0.68–1.76) | 1.43 (0.91–2.27) |
| Possible HIV exposure | 0.81 (0.52–1.29) | 0.23 (0.14–0.37) | 1.06 (0.66–1.72) | 0.58 (0.33–1.01) | 1.16 (0.69–1.95) | 1.39 (0.84–2.29) |
| Other | 0.86 (0.43–1.71) | 0.28 (0.14–0.58) | 0.77 (0.38–1.56) | 0.80 (0.35–1.84) | 1.19 (0.54–2.62) | 1.35 (0.64–2.88) |
| Reasons for never having been tested for HIV | ||||||
| n = 941 | ||||||
| Not at risk | Base outcome | Base outcome | Base outcome | Base outcome | Base outcome | Base outcome |
| Hadn’t considered being tested | 0.53 (0.38–0.76) | 1.48 (1.09–2.00) | 1.05 (0.72–1.53) | 0.71 (0.50–1.00) | 0.71 (0.51–0.98) | 0.55 (0.40–0.77) |
| Inconvenience | 0.56 (0.26–1.18) | 2.14 (1.10–4.19) | 0.69 (0.33–1.43) | 1.05 (0.51–2.16) | 0.45 (0.22–0.90) | 0.38 (0.18–0.83) |
| Scared/Worried | 0.32 (0.14–0.70) | 1.67 (0.95–2.93) | 0.60 (0.33–1.11) | 0.28 (0.12–0.69) | 0.49 (0.27–0.89) | 0.46 (0.24–0.87) |
| Other | 0.96 (0.45–2.04) | 1.71 (0.85–3.42) | 0.98 (0.41–2.33) | 0.53 (0.23–1.24) | 0.73 (0.34–1.56) | 1.07 (0.52–2.24) |
Model excludes the participant who was transgendered
Among the 946 participants never previously tested for HIV, 56.1% had not been tested because they did not consider themselves to be at risk for HIV, 29.4% had never considered being tested, 6.5% were scared or worried about being tested because of the testing process and potential test outcomes, 4.3% found it to be too inconvenient to be tested, and 3.7% cited other reasons. As shown in Table 3, those who were aged 39 years and younger were more likely to indicate that they were scared/worried or hadn’t considered being tested. Male participants were much more likely to indicate that testing was an inconvenience or that they hadn’t considered being tested. Non-married participants were more likely to indicate that they were scared/worried about the test results. Participants without private health-care insurance and those with fewer than 12 years of education were more likely to indicate that they had never been tested because testing was an inconvenience, or because they were scared/worried or because they simply ‘hadn’t considered being tested’.
DISCUSSION
The results of this study illustrate that a large proportion of ED patients have not previously been tested for HIV, which suggests that EDs are a place where significant numbers of people could be screened for HIV. It also shows how years of risk- and demographic characteristic targeted HIV screening and diagnostic testing efforts have led to variations in HIV testing along demographic lines. Although targeted screening previously might have been a reasonable method of identifying those most likely to have an HIV infection, it clearly does not locate all cases. It also creates unexplored reservoirs of potential sources of HIV infection. Particular demographic groups are less likely to have been tested for HIV: younger and older adults, males, whites, married or single/never married/not partnered patients, and patients with private health-care insurance. It is ironic that demographic groups historically with the greatest access to health care in the US – white patients with private health-care insurance – were less likely to have been tested for HIV than those historically with reduced access to health care, which is in distinct contrast to many other preventive health tests and medical services. On the other hand, efforts to enhance HIV screening and testing among blacks and Hispanic/Latinos appear to be showing some success.
Personal motivation for HIV testing may play an important role in patient acceptance of ED-based HIV screening. Testing as part of a medical evaluation is still a common reason for being tested,25 which also indicates that access to HIV testing for this population is through the health-care setting. As reported in other studies, a belief of not being at risk remains a primary rationale for not being tested.25,26 There are demographic variations in the main reason for an ED patient’s last HIV test and for never having been tested for HIV. Males, patients over age 40, and married patients were more likely to have been required to be tested than out of a desire to know their HIV status. These groups appear to be less motivated to know their HIV status and therefore could be targeted with interventions to appreciate the importance to themselves and others of knowing whether or not they are HIV-infected. Females, patients over age 40, those with private health care insurance, and those with more than 12 years of formal education were also more likely not to have been tested because they did not believe themselves to be at risk of an HIV infection. Because we did not assess the HIV risk factors for these patients, we cannot determine if this belief was reasonable. Nevertheless, the results indicate groups who may benefit from interventions to make them aware of their personal risk for an HIV infection in an effort to improve uptake of HIV screening.
LIMITATIONS
Since the study was based at a single hospital, the findings might not be generalizable to some other EDs. However, we believe that our random sample of ED provided a representative sample of patients from different demographic groups. Our findings about differences in HIV testing along demographic characteristics might not be applicable to the groups excluded from our study. This study also examined HIV-testing history only and not HIV risk factors. As such, we cannot estimate the extent to which a history of HIV testing is related to real or perceived risk of having an infection. We can only identify demographic factors that were associated with lack of HIV testing.
CONCLUSIONS
A substantial proportion of ED patients have never been tested for HIV, which supports CDC’s recommendations that EDs perform HIV screening. Prior risk- and demographic characteristic-based HIV screening and diagnostic testing efforts have led to variations in HIV-testing history along demographic lines. Universal HIV screening might help to reduce gaps in HIV testing by demography in the US, thus reducing unexplored reservoirs of HIV infections. Efforts to improve uptake in HIV screening will need to address these differences in motivations for testing.
Acknowledgments
Dr Merchant and this study were supported by a career development grant from the National Institute for Allergy and Infectious Diseases (K23 A1060363). The study was also supported by a cooperative agreement grant from the Centers for Disease Control and Prevention (U65/CCU124504). Dr Mayer was supported by the Center for AIDS Research at Lifespan/Tufts/Brown (P30 AI42853). The authors gratefully acknowledge the helpful advice of Sheryl Lyss, Duncan MacKellar, and Maxia Dong from the Centers for Disease Control and Prevention to the design of the study. The authors are especially grateful to the able research assistants who collected the data for the study: Kelly Cockcroft, Erin Argueta, Bethany Catanzaro, Shereen Mohiuddin and Jeremy Katzen.
Footnotes
The results of this study were presented at the American College of Emergency Physicians Scientific Assembly on 9 October 2007 Accepted for publication 5 May 2009
Contributor Information
Roland C Merchant, Department of Emergency Medicine; Department of Community Health, Warren Alpert Medical School of Brown University, Providence, RI; Department of Epidemiology, Harvard School of Public Health, Boston, MA, USA.
Bethany M Catanzaro, Department of Emergency Medicine, Warren Alpert Medical School of Brown University, Providence, RI, USA.
George R Seage, III, Department of Epidemiology, Harvard School of Public Health, Boston, MA, USA.
Kenneth H Mayer, Department of Community Health, Warren Alpert Medical School of Brown University, Providence, RI; Department of Medicine, Division of Infectious Diseases, Warren Alpert Medical School of Brown University, Providence, RI, USA.
Melissa A Clark, Department of Community Health, Warren Alpert Medical School of Brown University, Providence, RI, USA.
Victor G DeGruttola, Department of Biostatistics, Harvard School of Public Health, Boston, MA, USA.
Bruce M Becker, Department of Emergency Medicine; Department of Community Health, Warren Alpert Medical School of Brown University, Providence, RI, USA.
References
- 1.Centers for Disease Control and Prevention. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006;55(RR-14):1–17. [PubMed] [Google Scholar]
- 2.Lethbridge-Çejku M, Rose D, Vickerie J. Summary Health Statistics for U.S. Adults: National Health Interview Survey, 2004. National Center for Health Statistics. Vital Health Statistics. 2006;10(228):1–151. [PubMed] [Google Scholar]
- 3.McCaig LF, Nawar EW. National Hospital Ambulatory Medical Care Survey: 2004 emergency department summary. Adv Data. 2006;23(372):1–29. [PubMed] [Google Scholar]
- 4.Ragin DF, Hwang U, Cydulka RK, et al. Reasons for using the emergency department: results of the EMPATH Study. Acad Emerg Med. 2005;12(12):1158–66. doi: 10.1197/j.aem.2005.06.030. [DOI] [PubMed] [Google Scholar]
- 5.Alpert PL, Shuter J, DeShaw MG, Webber MP, Klein RS. Factors associated with unrecognized HIV-1 infection in an inner-city emergency department. Ann Emerg Med. 1996;28(2):159–64. doi: 10.1016/s0196-0644(96)70056-2. [DOI] [PubMed] [Google Scholar]
- 6.Shuter J, Alpert PL, DeShaw MG, Greenberg B, Chang CJ, Klein RS. Gender differences in HIV risk behaviors in an adult emergency department in New York City. J Urban Health. 1999;76(2):237–46. doi: 10.1007/BF02344679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goggin MA, Davidson AJ, Cantril SV, O’Keefe LK, Douglas JM. The extent of undiagnosed HIV infection among emergency department patients: results of a blinded seroprevalence survey and a pilot HIV testing program. J Emerg Med. 2000;19(1):13–9. doi: 10.1016/s0736-4679(00)00175-x. [DOI] [PubMed] [Google Scholar]
- 8.Sturm JT. HIV prevalence in a midwestern emergency department. Ann Emerg Med. 1991;20(3):276–8. doi: 10.1016/s0196-0644(05)80939-4. [DOI] [PubMed] [Google Scholar]
- 9.Baraff LJ, Talan DA, Torres M. Prevalence of HIV antibody in a noninner-city university hospital emergency department. Ann Emerg Med. 1991;20(7):782–6. doi: 10.1016/s0196-0644(05)80842-x. [DOI] [PubMed] [Google Scholar]
- 10.Baker JL, Kelen GD, Sivertson KT, Quinn TC. Unsuspected human immunodeficiency virus in critically ill emergency patients. Jama. 1987;257(19):2609–11. [PubMed] [Google Scholar]
- 11.Kelen GD, Fritz S, Qaquish B, et al. Substantial increase in human immunodeficiency virus (HIV-1) infection in critically ill emergency patients: 1986 and 1987 compared. Ann Emerg Med. 1989;18(4):378–82. doi: 10.1016/s0196-0644(89)80574-8. [DOI] [PubMed] [Google Scholar]
- 12.Jui J, Modesitt S, Fleming D, et al. Multicenter HIV and hepatitis B seroprevalence study. J Emerg Med. 1990;8(3):243–51. doi: 10.1016/0736-4679(90)90001-c. [DOI] [PubMed] [Google Scholar]
- 13.Kelen GD, Hexter DA, Hansen KN, et al. Feasibility of an emergency department-based, risk-targeted voluntary HIV screening program. Ann Emerg Med. 1996;27(6):687–92. doi: 10.1016/s0196-0644(96)70184-1. [DOI] [PubMed] [Google Scholar]
- 14.Kelen GD, Shahan JB, Quinn TC. Emergency department-based HIV screening and counseling: experience with rapid and standard serologic testing. Ann Emerg Med. 1999;33(2):147–55. doi: 10.1016/s0196-0644(99)70387-2. [DOI] [PubMed] [Google Scholar]
- 15.Lyons MS, Lindsell CJ, Ledyard HK, Frame PT, Trott AT. Emergency department HIV testing and counseling: an ongoing experience in a low-prevalence area. Ann Emerg Med. 2005;46(1):22–8. doi: 10.1016/j.annemergmed.2004.12.022. [DOI] [PubMed] [Google Scholar]
- 16.Lyons MS, Lindsell CJ, Ledyard HK, Frame PT, Trott AT. Health department collaboration with emergency departments as a model for public health programs among at-risk populations. Public Health Rep. 2005;120(3):259–65. doi: 10.1177/003335490512000307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Silva A, Glick NR, Lyss SB, et al. Implementing an HIV and sexually transmitted disease screening program in an emergency department. Ann Emerg Med. 2007;49(5):564–72. doi: 10.1016/j.annemergmed.2006.09.028. [DOI] [PubMed] [Google Scholar]
- 18.Lyss SB, Branson BM, Kroc KA, Couture EF, Newman DR, Weinstein RA. Detecting unsuspected HIV infection with a rapid whole-blood HIV test in an urban emergency department. J Acquir Immune Defic Syndr. 2007;44(4):435–42. doi: 10.1097/QAI.0b013e31802f83d0. [DOI] [PubMed] [Google Scholar]
- 19.Brown J, Shesser R, Simon G, et al. Routine HIV screening in the emergency department using the new US Centers for Disease Control and Prevention Guidelines: results from a high-prevalence area. J Acquir Immune Defic Syndr. 2007;46(4):395–401. doi: 10.1097/qai.0b013e3181582d82. [DOI] [PubMed] [Google Scholar]
- 20.Shuter J, Alpert PL, DeShaw MG, Greenberg B, Klein RS. Rates of and factors associated with self-reported prior HIV Testing among adult medical patients in an inner city emergency department in the Bronx, New York City. J Acquir Immune Defic Syndr Human Retrovirol. 1997;14(1):61–6. doi: 10.1097/00042560-199701010-00010. [DOI] [PubMed] [Google Scholar]
- 21.Merchant RC, Seage GR, III, Mayer KH, Clark MA, DeGruttola VG, Becker BM. Emergency department patient acceptance of optin, universal, rapid HIV screening. Public Health Rep. 2008;123(Supplement 3):27–40. doi: 10.1177/00333549081230S305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Merchant R, Gee E, Clark M, Mayer K, Seage GI, DeGruttola V. Comparison of patient comprehension of rapid HIV pre-test fundamentals by information delivery format in an emergency department setting. BMC Public Health. 2007;7(7) doi: 10.1186/1471-2458-7-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Office of HIV/AIDS: Rhode Island Department of Health. Comprehensive Plan for HIV Prevention, Rhode Island 2003. Providence, RI: Rhode Island Department of Health; 2003. [Google Scholar]
- 24.Branson B, Handsfield HH, Lampe MA, et al. Revised recommendations for HIV Testing of adults, adolescents, and pergnant women in health-care settings. Morbidity and Mortality Weekly Report. 2006;55(RR14):1–17. [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention. National Health Interview Survey. Atlanta, GA: Centers for Disease Control and Prevention; 2006. [Google Scholar]
- 26.Kaiser Family Foundation. Survey of Americans on HIVAIDS. 2006. [Google Scholar]