Abstract
Objectives:
To assess the effects of Vipassana meditation on the physical and psychological health in a multi-ethnic population in the city of Muscat.
Method:
The subjects were participants of a Vipassana meditation course taught in a ten-day residential retreat. Self-assessments of health-related parameters and physical and psychological symptomatology were collected from them before and immediately after the course. A control group was tested for a similar time interval.
Results:
Immediately after their 10-day training, the Vipassana participants assessed themselves significantly higher compared to their levels prior to the course, suggesting that the 10 days’ practice had significantly improved their physical and psychological well-being. The control group did not exhibit such changes.
Conclusion:
The present preliminary findings, juxtaposed with the results of studies from other parts of the world, suggest that the practice of Vipassana meditation may help mitigate psychological and psychosomatic distress.
Keywords: Vipassana, meditation, stress, physiological, psychological, Oman
Vipassana, which means to see things as they really are, is an ancient technique to improve concentration and self-awareness through meditation. The theory and philosophy of Vipassana have been extensively reviewed elsewhere.1–3 Vipassana seeks self transformation through self observation, where the meditator pays disciplined attention to the physical sensations that continuously interact with and condition the mind.3,4 Being an ancient technique, many schools of Vipassana—both sectarian and non-sectarian—have evolved. Prominent among the non-sectarian approaches is the one adopted by S. N. Goenka and Assistant Teachers in their ten-day residential courses conducted in many countries including UAE and Oman.3–6 One of their courses conducted in Oman provided data for this study.
Vipassana’s observation-based journey to the common root of mind and body is expected to reduce the tendency of the mind to dwell on the past (thereby reducing regrets), or to delve into the future (thus lowering expectations and anxieties), helping the participant to remain in the ‘here and now’ and achieve relative mental tranquillity.1,3,4,7,8 Both traditional and clinical literature suggest that Vipassana practice increases awareness, promotes integration of subjective experience and facilitates acceptance and tolerance to sufficiently reduce physical and psychological distress.2,3 With the advent of invasive measurement tools, there is also evidence that changes reported from non-invasive assessment measures are accompanied by altered physiological parameters.9
If a technique has universal application, then it ought to transcend cultural barriers and show its efficacy in all populations. Studies in the West on meditative techniques akin to Vipassana have demonstrated enhancement in functional status, and physical and mental well-being in practitioners.10 Studies in Asia have also reported similarly.2,6,7 Among the most intriguing of these cross-cultural studies have been the ones conducted among prisoners where Vipassana meditation reportedly improved the inmates’ mood and behaviour.2, 6, 11
There is a need for the quantification of the relevance of these health-promoting techniques in other regions of the world, especially in the Middle East.12 Lack of reports from the Arab world prompted the need for testing the effect of Vipassana meditation on the health-related quality of life and physical and psychological symptomatology in the residents of this region. The present study was therefore designed to test the hypothesis that Vipassana training could improve the health-related quality and impact on physical and psychological symptomatology in a multiethnic population like that in Oman.
METHOD
DESIGN
The study constituted a naturalistic experiment with 14 Vipassana participants who were voluntarily attending a ten-day residential meditation course in Muscat, Oman, during July 2001. The participants were tested twice, once at the beginning of the 10-day course and thereafter upon completion of the course. The control group consisted of 31 students of Sultan Qaboos University. These students did not take part in the meditation sessions but were given the same assessment instruments both at the beginning and at the end of the 10-day period. Being a naturalistic experiment, the groups were not initially matched for specific factors that could arise by chance.
Vipassana meditation course requires the novice to maintain strict silence for 9 days except to clear doubts with the teacher or to solve material problems with volunteers. The meditators are permitted to break their silence on the morning of the 10th day, to facilitate their transition back to the outside world. The course ends the 11th day morning.
Prior to start of the course, a brief explanation of the study was given to the participants and they were assured that the data and results would be treated confidentially. Their oral consent was then taken. The control group students were also similarly assured and their oral consent obtained.
Both the groups were assessed twice. The first assessment (time1) was administered just before the start of the 10-day meditation training session. The second assessment (time2) was done immediately after the conclusion of the training. Even though the group of students did not take part in the training, their assessment was done at the same time as that of the training group. Both the groups were asked during the assessment not to discuss the questionnaire between themselves so as to avoid peer pressure.
ASSESSMENT MEASURES
All the participants were assessed with non-invasive measures, via self-report questionnaires. In this study, it was not viable to collect biochemical markers or conduct clinical interviews to verify self-report data. Since the participants could elect not to fill the questionnaire, there was no obvious reason for them to give inaccurate information. The subjective functioning data using Likert type self-report are described in the result.
Conventional assessment measures were also used and included GHQ-28, a 28-item scaled version of the original General Health Questionnaire (GHQ), with four subscales derived by factor analysis.13 These include somatic symptoms, anxiety and insomnia, social dysfunction, and severe depression.
The validity of the subscales is discussed in Goldberg & Williams.14 The four subscales in GHQ-28 represent dimensions of symptomatology; thus more symptoms result in a higher score but high scores do not necessarily correspond to any psychiatric diagnosis. The present analysis was derived from the composite score of GHQ-28. The other conventional assessment measure used, the Hospital Anxiety and Depression Scale (HADS),15 is a 14-item questionnaire with two 7-item sub-scales, one for depression and the other for anxiety. Symptoms are listed and subjects rate the frequency or severity of these during the preceding week on a 4-point scale (0–3), making a maximum possible score of 21 on each sub-scale. The original validation study for the HADS suggested that on either sub-scale, non-cases scored 7 or less, doubtful cases 8–10, and definite cases 11 or more. Separate indices of anxiety and depression were recorded for the present analysis.
STATISTICAL ANALYSIS
The statistical software SPSS Version 10 for Windows was used to analyse the data. The summary statistics were computed for some of the demographic variables by group. Independent-sample t-test and paired t-test were used to compare group means. Cross-tabulation was used on the categorical variables and the chi-square (χ2) statistic and corresponding p-values computed were applicable. For 2×2 tables, Fisher-exact p-values were computed.
RESULTS
(i). Demographic information
Fourteen subjects (7 male and 7 female; mean age 40.14±12.67 years) participated in the Vipassana training session. Thirty-one subjects (14 male and 17 female; mean age 19.77±0.84) formed the control group. The two groups differed significantly in age (p<0.001). Being a naturalistic experiment, it was logistically not possible to balance ages between the groups. In terms of marital status, in Vipassana group, 9 were married and 5 were single. Among the controls, only 2 were married and the rest were single.
(ii). time 1: Subjective functioning on Health-Related Quality of Life
The subjective functioning pertaining to health parameters are summarized below. Most participants believed in their own abilities to overcome difficult situations [Table 1], with no significant difference between the two groups (p=0.558).
Table 1.
Response to: ‘Do you have a high level of belief in your own ability to overcome difficult situations?’
| Yes | No | Total | p | ||
|---|---|---|---|---|---|
| TIME1 | Vipassana | 10 | 4 | 14 | |
| Control | 23 | 8 | 31 | 0.850 | |
| Total | 33 | 12 | 45 | ||
Over 90% (41/45) of the participants agreed that faith or spiritual values helped them cope with pressures of life [Table 2]. There was no significant differences between the two groups, p=0.366.
Table 2.
Response to: ‘Your faith or spiritual values help you cope with the pressure of life.’
| Yes | No | Total | p | ||
|---|---|---|---|---|---|
| TIME1 | Vipassana | 12 | 2 | 14 | |
| Control | 29 | 2 | 31 | 0.366 | |
| Total | 41 | 4 | 45 | ||
The control group perceived they had insufficient or poor financial resources [Table 3], as is typical of students.
Table 3.
Response to: ‘How would you describe your current level of income?’
| Sufficient | Insufficient | p | |||
|---|---|---|---|---|---|
| TIME1 | Vipassana | 9 | 4 | 13 | |
| Control | 2 | 29 | 32 | 0.366 | |
| Total | 11 | 33 | 45 | ||
The perceived fitness levels of the two groups were similar [Table 4]. Thirteen percent felt they were in excellent physical condition while 40% felt the opposite.
Table 4.
Response to: ‘How do you rate your current level of fitness?’
| Excellent | Good | Poor | Total | p | ||
|---|---|---|---|---|---|---|
| TIME1 | Vipassana | 2 | 6 | 6 | 14 | |
| Control | 4 | 15 | 12 | 31 | 0.942 | |
| Total | 6 | 21 | 18 | 45 | ||
(iii). Performance across time1 and time2
The subjective functioning of the participants is summarized in Table 5. In the first assessment, the majority (29/45) felt undecided whether they were happy or unhappy. However, the majority of the Vipassana group (9/14) felt happy about life in the first assessment itself. At the second assessment, four more participants from the Vipassana group indicated that they felt happy about life.
Table 5.
Response to: ‘How do you feel about your life as a whole at present?’
| Happy | Undecided | Unhappy | p | ||
|---|---|---|---|---|---|
| TIME1 | Vipassana | 9 | 4 | 1 | 0.0001 |
| Control | 1 | 25 | 5 | ||
| TIME2 | Vipassana | 13 | 1 | 0 | 0.0001 |
| Control | 1 | 25 | 5 | ||
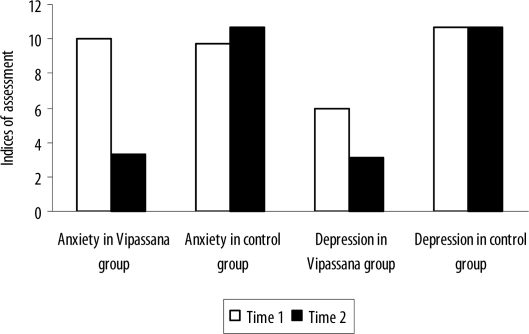
All Vipassana meditators showed a pronounced improvement in Hospital Anxiety and Depression Scale and Modified General Health Questionnaire. Scores for time1 and time2 are presented in Table 6.
Table 6.
Summary of Anxiety and Depression Scores
| TIME1 | TIME2 | p | ||||
|---|---|---|---|---|---|---|
| Mean | Std | Mean | Std | |||
| Anxiety | Vipassana | 10.00 | 1.24 | 3.29 | 0.73 | 0.001 |
| Control | 9.68 | 1.35 | 10.70 | 2.28 | ||
| Depression | Vipassana | 6.00 | 1.71 | 3.14 | 2.38 | 0.001 |
| Control | 10.71 | 2.28 | 10.91 | 2.28 | ||
Affective functioning
The summary statistics of the Hospital Anxiety and Depression Scale are provided in Table 6. All the participants of Vipassana showed a pronounced improvement in anxiety and depression. The drop in the anxiety level in this group was particularly significant: an average drop from 10 to 3.29 (p=0.001). On the other hand, the average anxiety level of the control group increased marginally. The Vipassana group also showed a marked drop on the Depression score (p=0.004). Before meditation, they scored 6, but after the course the score dropped significantly to 3.14.
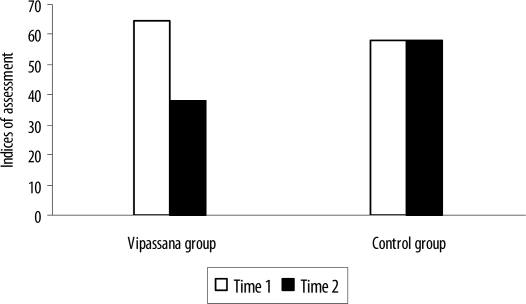
General health
There were significant changes (p<0.001) between the time1 and time2 assessment using the Modified General Health Questionnaire (GHQ-28). As can be seen from Table 7 and Figure 2, the control group’s total score remained relatively stable. In contrast, the Vipassana group showed steep reduction in the indices of psychiatric symptomatology, suggesting the retreat was effective in ameliorating their psychiatric symptomatology.
Table 7.
General Health Score
| TIME1 | TIME2 | p | |||
|---|---|---|---|---|---|
| Mean | Std | Mean | Std | ||
| Vipassana | 64.71 | 23.55 | 38.07 | 18.94 | 0.791 |
| Control | 57.81 | 18.59 | 57.94 | 18.17 | |
Figure 2.
General Health Score
DISCUSSION
In this age when many people seek alternative therapeutic methods, there is a dearth of research of the efficacy on such interventions in the population in the Middle East, and particularly in Oman. This pilot study has attempted to address this lack by examining the effects of Vipassana training on health-related quality of life and physical and psychological symptomatology in a heterogeneous group of subjects from among the resident population of Muscat. Studies from elsewhere provide evidence that such an undertaking can enhance one’s functional status and well-being as well as reduce physical symptoms and psychological distress.4,16,17
In the present study, prior to Vipassana training, the performance of those subjects who voluntarily elected to enrol in the 10-day course of Vipassana meditation had not differed from that of the control group. Specifically, on subjective functioning (apart from the issue pertaining to income and whether they were happy or not) the two groups did not differ. These results support the observation by Gillani18 and Smith19 that prospective meditators do not differ from the general population in their level of stress or distress. When tested immediately after the 10-day training, their performance on several parameters changed, suggesting alleviation of physical symptoms and decreased psychological distress. In contrast, such fluctuations were not seen in the control subjects who were tested at the same interval. This finding is compatible with emerging evidence suggesting that meditative techniques can have a great effect on physical and psychological functioning.2,19,20
The present study is, however, not conclusive and had several possible limitations. The scope of generalizing its findings could be limited due to various factors. First, the sample size was small. Second, the Vipassana subjects were a self-selective group of different ages and it was not clear how many participants had previous experience with meditation. Third, being naturalistic, the study relied entirely on subjective reports. To overcome these limitations, it would be necessary to replicate the study in different and larger populations and to use stronger experimental methodology with random allocation between conditions. Future studies could also employ objective physiological measures to confirm the subjects’ perceived improvement. In the emerging functional in-vivo neuro-imagining techniques, misreporting by subjects can be independently verified.21,22 Fourth, it was not clear how long the observed improvement would persist, since the post assessment was conducted right at the end of the retreat. On the other hand, some studies have reported that one-year follow-up revealed maintenance of initial improvements on several outcome parameters.2 Data collection by questionnaire is also not without problems.23 Although some structured questionnaires are easy to apply, studies have found that different cultures attach different meanings to life and thus conceive reality differently.24 Although all the items of the screening instrument have been validated in cross-cultural settings,14,25–26 its usefulness could still be hampered by subtle linguistic and conceptual misunderstandings. Therefore, specificity and sensitivity of these assessment tools need to be examined.
A factor that could have enhanced the positive subjective states of the Vipassana participants is the retreat environment itself rather than the exercise per se: the subjects were residing in a tension-free, cloistered environment for 10 days. They were completely sheltered from outside happenings, since TV, newspapers, telephones and visitors were forbidden. The simple food served could also have had a positive effect. Breakfast was served at 6:30 am, lunch at 11:30 am, and tea and fruit at 5 pm, after which no food was served. The meditators went to sleep at 9:30 pm to awake the next day at 4:00 am. No physical exertion apart from walking in a confined area was permitted. Ten days of such an uncomplicated routine could have contributed positively to the mood and behaviour of the novice. Again, since the meditators spent ten valuable days on this process, they might have liked to think that their efforts were successful.18 This might have caused them to rate themselves higher in the second assessment. Similarly, the researcher’s expectations could have influenced the results. However, the authors are of the view that these limitations do not obscure the fact that Vipassana meditation, with its simple technique and tightly controlled variables, offers a fertile field for future studies, which should comprise precise invasive and non-invasive methods.
The evidence from this study, however partial, combined with those from other studies around the world, suggests that Vipassana meditation may have the potential to enhance the health-related quality of life and physical and psychological symptomatology, irrespective of ethnic or cultural backgrounds. In Oman, the population has been growing since the late 1970s at an annual rate of 4.86%,27 one of the fastest in the world, which would increase competition for social and occupational roles, and leave many failed individuals behind.28 Such a demographic trend would place more and more individuals at risk for developing various adjustment problems.29 The trend so far has been to embrace ‘hi-tech’ therapeutic methods including psychotropic medications which are expensive and often have side effects.30–32 With the rising cost of running health care systems33 and in an age where many physical and psychological disorders arise because of what people do to themselves rather than solely from external sources,34 a non-sectarian technique such as Vipassana may help in prevention and therapy. The next challenge to the healthcare planners in developing countries like Oman would be how to respond to the rising tide of the ‘diseases of affluence.’23,35 Serious contemplation of these considerations should make clear the need to develop and allocate low-cost therapeutic interventions such as meditation that have potential to alleviate suffering and improve people’s functionality.
CONCLUSION
The results from this pilot study on participants of Vipassana meditation in Muscat, Oman, when juxtaposed with the results of studies in other parts of the world, suggest that this meditation technique may help mitigate psychological and psychosomatic distress. The study also implies that Vipassana meditation, with its simple method and controllable variables, offers a fertile field for future research, which should comprise invasive and non-invasive methods.
Figure 1.
The effect of Vipassana training on anxiety and depression
REFERENCES
- 1.Kahn M. Vipassana meditation and the psychobiology of Reich, Wilhelm. J Humanist Psychol. 1985;25:117–28. [Google Scholar]
- 2.Chandiramani K, Verma SK, Dhar PL. Psychological Effects of Vipassana on Tihar Jail Inmates. Maharashtra: Vipassana Research Institute; 1998. [Google Scholar]
- 3.Fleischman PR. The Experience of Impermanence. Maharashtra: Vipassana Research Institute; 1999. [Google Scholar]
- 4.Srinivasan S. Understanding the process of Vipassana meditation. Int J Psychol. 1992;27:447. [Google Scholar]
- 5.Emavardhana T, Tori CD. Changes in self-concept, ego defence mechanisms, and religiosity following seven-day Vipassana meditation retreats. J Sci Study Relig. 1997;36:194–206. [Google Scholar]
- 6.Khurana A, Dhar PL. Effects of Vipassana Meditation on Quality of Life, Subjective Wellbeing, and Criminal Propensity Among Inmates of Tihar Jail, Delhi. 2000. Monograph submitted to Indian Institute of Technology. [Google Scholar]
- 7.Hirai T. Zen Meditation and Psychotherapy. Tokyo: Japan Publication Inco; 1989. [Google Scholar]
- 8.Morris JS, Ohman A, Dolan RJ. Conscious and unconscious emotional learning in the human amygdale. Nature. 1998;393:467–70. doi: 10.1038/30976. [DOI] [PubMed] [Google Scholar]
- 9.Aftanas LI, Golocheikine SA. Human anterior and frontal midline theta and lower alpha reflect emotionally positive state and internalized attention: high-resolution EEG investigation of meditation. Neurosci Lett. 2001;310:57–60. doi: 10.1016/s0304-3940(01)02094-8. [DOI] [PubMed] [Google Scholar]
- 10.Reibel DK, Greeson JM, Brainard GC, Rosenzweig S. Mindfulness-based stress reduction and health-related quality of life in a heterogeneous patient population. Gen Hosp Psychiatry. 2001;23:183–92. doi: 10.1016/s0163-8343(01)00149-9. [DOI] [PubMed] [Google Scholar]
- 11.Studer UM. Vipassana, Professional Therapy and Science. Taipei: Torch of Wisdom; 1977. [Google Scholar]
- 12.Sinnott JD. A time for the condor and the eagle to fly together”: Relations between spirit and adult development in healing techniques in several cultures. J Adult Dev. 2001;8:241–47. [Google Scholar]
- 13.Goldberg DP, Hillier VFA. Scaled version of the General Health Questionnaire. Psychol Med. 1979;9:139–45. doi: 10.1017/s0033291700021644. [DOI] [PubMed] [Google Scholar]
- 14.Goldberg DP, Gater R, Sartorius N, Ustun TB, Piccinelli M, Gureje O, Rutter C. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med. 1997;27:191–7. doi: 10.1017/s0033291796004242. [DOI] [PubMed] [Google Scholar]
- 15.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 16.Kabat-Zinn J, Wheeler E, Light T, Skillings A, Scharf MJ, Cropley TG, et al. Influence of a mindfulness meditation-based stress reduction intervention on rates of skin clearing in patients with moderate to severe psoriasis undergoing phototherapy (UVB) and photochemotherapy (PUVA) Psychosom Med. 1998;60:625–32. doi: 10.1097/00006842-199809000-00020. [DOI] [PubMed] [Google Scholar]
- 17.Mason O, Hargreaves L. A qualitative study of mindfulness-based cognitive therapy for depression. Bri J Med Psychol. 2001;74:197–212. [PubMed] [Google Scholar]
- 18.Gillani NB, Smith JC. Zen meditation and ABC relaxation theory: An exploration of relaxation states, beliefs, dispositions, and motivations. J Clin Psychol. 2001;57:839–46. doi: 10.1002/jclp.1053. [DOI] [PubMed] [Google Scholar]
- 19.Smith R. Oman: leaping across the centuries. BMJ. 1988;297:540–4. doi: 10.1136/bmj.297.6647.540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Coleman D. The psychology of meditation. In: Kwee MGT, editor. Psychotherapy, Meditation and Health. The Hague: East-West Publications; 1990. [Google Scholar]
- 21.Williams KA, Kolar MM, Reger BE, Pearson JC. Evaluation of a wellness-based mindfulness stress reduction intervention: a controlled trial. Am J Health Promot. 2001;15:422–32. doi: 10.4278/0890-1171-15.6.422. [DOI] [PubMed] [Google Scholar]
- 22.Baerentsen KB, Hartvig NV, Stokilde-Jorgensen H, Mammen J. Onset of meditation explored with fMRI. Neuroimage. 2001;13:S297. [Google Scholar]
- 23.Al-Adawi S, Salmi A, Martin RG, Ghassani H. Zar: group distress and healing. Ment Health Rel Cult. 2000;4:47–61. [Google Scholar]
- 24.Al-Adawi S. A glimpse into traditional outlook towards health: A literature review. J Med Humanit. 1993;14:67–79. [Google Scholar]
- 25.Malasi TH, Mirza IA, El-Islam MF. Validation of the Hospital Anxiety and Depression Scale in Arab patients. Acta Psychiatr Scand. 1991;84:323–6. doi: 10.1111/j.1600-0447.1991.tb03153.x. [DOI] [PubMed] [Google Scholar]
- 26.El-Rufaie OF, Daradkeh TK. Validation of the Arabic versions of the thirty- and twelve-item General Health Questionnaires in primary care patients. Br J Psychiatry. 1996;169:662–4. doi: 10.1192/bjp.169.5.662. [DOI] [PubMed] [Google Scholar]
- 27.Ministry of National Economy . The Statistical YearBook, Sultanate of Oman. 28 Edition. Muscat: Information and Publication Centre; 2000. [Google Scholar]
- 28.Easterlin RA. Birth and Fortune: the Impact of Numbers on Personal Welfare. New York: Basic Books Easter; 1980. [Google Scholar]
- 29.Kleinman A, Cohen A. Psychiatry’s global challenge. Sci Am. 1997;276:86–9. doi: 10.1038/scientificamerican0397-86. [DOI] [PubMed] [Google Scholar]
- 30.Smith R. Oman: leaping across the centuries. BMJ. 1988;297:540–4. doi: 10.1136/bmj.297.6647.540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ernst E. Complementary medicine for disease and illness prevention? A research perspective. Forsch Komplementarmed. 1999;6:181–3. doi: 10.1159/000021246. [DOI] [PubMed] [Google Scholar]
- 32.Calderon R, Jr, Schneider RH, Alexander CN, Myers HF, Nidich SI, Haney C. Stress, stress reduction and hypercholesterolemia in African Americans: a review. Ethn Dis. 1999;9:451–62. [PubMed] [Google Scholar]
- 33.World Health Organization . World Health Report 2000. Geneva: 2000. [Google Scholar]
- 34.Weinman J. An Outline of Psychology as Applied to Medicine. 2 edition. Oxford: Butterworth Heinemann; [Google Scholar]
- 35.Martin R, Al-Adawi S. Psychiatric treatments: an exciting new century. Hosp Med. 2000;61:524–5. doi: 10.12968/hosp.2000.61.8.1391. [DOI] [PubMed] [Google Scholar]