Abstract
Despite the well-established contribution of neurohumoral activation to morbidity and mortality in heart failure (HF) patients, relatively little is known about the underlying central nervous system mechanisms. In this study, we aimed to determine whether changes in GABAergic inhibitory and glutamatergic excitatory synaptic function contribute to altered hypothalamic magnocellular neurosecretory cell (MNC) activity in HF rats. Patch-clamp recordings were obtained from MNCs in brain slices from sham and HF rats. Glutamate excitatory (EPSCs) and GABAergic inhibitory postsynaptic currents (IPSCs) were simultaneously recorded, and changes in their strengths, as well as their interactions, were evaluated. We found a diminished GABAergic synaptic strength in MNCs of HF rats, reflected as faster decaying IPSCs and diminished mean IPSC charge transfer. Opposite changes were observed in glutamate EPSC synaptic strength, resulting in a shift in the GABA-glutamate balance toward a relatively stronger glutamate influence in HF rats. The prolongation of glutamate EPSCs during HF was mediated, at least in part, by an enhanced contribution of AMPA receptor desensitization to the EPSC decay time course. EPSC prolongation, and consequently increased unitary strength, resulted in a stronger AMPA receptor-mediated excitatory drive to firing discharge in MNCs of HF rats. Blockade of GABAA synaptic activity diminished the EPSC waveform variability observed among events in sham rats, an effect that was blunted in HF rats. Together, our results suggest that opposing changes in postsynaptic properties of GABAergic and glutamatergic synaptic function contribute to enhanced magnocellular neurosecretory activity in HF rats.
Keywords: supraoptic, paraventricular, hypothalamus
the neurohypophysial hormones vasopressin (VP) and oxytocin (OT) play critical roles in the regulation of body fluid homeostasis (Hatton 1990; Silverman and Zimmerman 1983). VP is a potent antidiuretic and vasoconstrictor hormone, known also to influence baroreflex inhibition of sympathetic activity (Hasser et al. 1997; Johnson and Thunhorst 1997), whereas OT is a potent natriuretic factor (Haanwinckel et al. 1995; Verbalis et al. 1991). In addition to its well-established role in homeostasis, VP also has been implicated in pathological conditions involving altered fluid balance, particularly congestive heart failure (HF) (Chatterjee 2005). In this sense, chronically elevated plasma VP levels have been reported in both animal models and human patients with HF (Francis et al. 1990; Goldsmith et al. 1983; Riegger et al. 1985; Szatalowicz et al. 1981), being a critical component of neurohumoral activation, a hallmark in this disease (Cohn et al. 1981; Hodsman et al. 1988; Schrier and Abraham 1999). The elevated release of VP in the presence of low cardiac output during HF has important detrimental consequences, including enhanced kidney water reabsorption, arterial vasoconstriction, and persistent hypernatremia, all of which contribute to detrimental myocardial effects (Goldsmith et al. 1986a, 1986b; Nakamura et al. 2000; Packer et al. 1987; Rouleau et al. 1994). The importance of VP in HF is further emphasized by the fact that VP receptor antagonism improves water balance and hemodynamic parameters in both experimental models (Arnolda et al. 1986; Wang et al. 1991) and human patients (Creager et al. 1986; Nicod et al. 1985) with HF. Despite the well-established contribution of neurohumoral activation and, in particular, elevated VP levels to the morbidity and mortality in HF patients (Francis et al. 1990; Rouleau et al. 1994), relatively little is known about the precise underlying mechanisms regulating VP release.
OT and VP release from neurohypophysial terminals is directly dependent on the degree and pattern of electrical activity of OT and VP magnocellular neurosecretory cells (MNCs), located in the hypothalamic supraoptic (SON) and paraventricular nuclei (PVN) (Cazalis et al. 1985; Poulain and Wakerley 1982; Silverman and Zimmerman 1983). MNC firing activity is in turn controlled by the combined action of intrinsic membrane properties and synaptic inputs (Bourque et al. 1993). Among the later, glutamate and GABA are the main excitatory and inhibitory hypothalamic neurotransmitters, respectively (Decavel and Van den Pol 1990; van den Pol et al. 1990), which closely interact with each other to fine-tune MNC neuronal activity and hormone release (Li et al. 2007; Nissen et al. 1995; Park et al. 2006; Randle and Renaud 1987; Sladek 1998). For example, VP release in response to an osmotic challenge requires activation of glutamate receptors within the SON/PVN (Sladek 1998), whereas GABA mediates baroreceptor- and cardiac-dependent inhibition of VP release (Grindstaff and Cunningham 2001; Jhamandas and Renaud 1986).
A growing body of evidence supports an important contribution of elevated SON and PVN neuronal activation (Patel et al. 1993, 2000; Vahid-Ansari and Leenen 1998; Zhang et al. 2002b) to increased neurohumoral drive during HF, which could result in turn from facilitation of excitatory synaptic inputs and/or suppression of inhibitory synaptic inputs. In fact, altered SON and PVN glutamate and GABAergic function has been reported in rats with HF (Han et al. 2010; Kleiber et al. 2008, 2010; Li et al. 2003; Zhang et al. 2002a). For example, an enhanced glutamate N-methyl-d-aspartate (NMDA) type 1 receptor expression and function was reported in rats with HF (Li et al. 2003). Conversely, blunted inhibitory mechanisms, mediated by GABA and nitric oxide, were also shown to contribute to increased sympathetic activity in HF (Zhang et al. 2001; 2002a). Moreover, manipulations that improve neurohumoral drive during HF, including exercise, modify the efficacy of these neurotransmitter systems (Kleiber et al. 2008; Zheng et al. 2005). Despite this evidence, the precise mechanisms contributing to altered excitatory and inhibitory synaptic function in MNCs in HF remain largely unknown. In this study, we obtained patch-clamp recordings from identified SON and PVN MNCs in brain slices from sham and HF rats. We simultaneously monitored glutamate and GABAergic synaptic activity within individual MNCs and evaluated their independent strengths as well as their interactions. Our results support a diminished GABA and enhanced glutamate synaptic strengths in HF rats, mediated by altered postsynaptic mechanisms, including changes in α-amino-3-hydroxy-5-methylisoxazole-4-propionic acid (AMPA) receptor desensitization. We propose the reported shift in the inhibitory/excitatory balance in MNCs during HF to contribute to elevated neurohumoral activation in this prevalent cardiovascular disease.
MATERIALS AND METHODS
Animals and induction of HF.
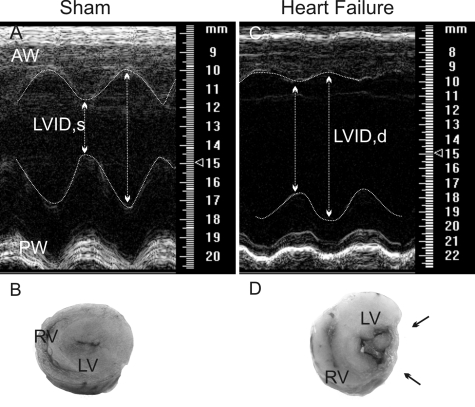
Male Wistar rats (150–180 g) were purchased from Harlan Laboratories (Indianapolis, IN). Rats were housed at room temperature (24–26°C) in a room with a 12:12-h light-dark cycle and given free access to food and water. All procedures were approved by the Medical College of Georgia Institutional Animal Care and Use Committee (IACUC) and carried out in agreement with the IACUC guidelines. HF was induced by coronary artery ligation as previously described (Patel et al. 2000). Briefly, animals were anesthetized with isoflurane (4%) and intubated for mechanical ventilation. A left thoracotomy was performed and the heart exteriorized. The ligation was placed on the main diagonal branch of the left anterior descending coronary artery. Buprenorphine (Bruprenex C3, 0.3 mg/kg sc; Butler Schein/NLS, Dublin, OH) was given immediately after surgery to minimize postsurgical pain. Sham animals underwent the same procedure, but the coronary artery was not occluded. All animals were used 6–7 wk after surgery. Transthoracic echocardiography (Vevo 770 system; Visual Sonics, Toronto, ON, Canada) was performed 4 wk after surgery under light anesthesia. The left ventricle internal diameter, as well as that of the left ventricle posterior and anterior walls, was obtained throughout the cardiac cycle from the short-axis motion imaging mode. Automatic calculation using the parameters measured was obtained for ejection fraction and fractional shortening. Representative echocardiography images are shown in Fig. 1, and mean cardiac function values obtained from sham and HF rats are summarized in Table 1.
Fig. 1.
Echocardiographic assessment of left ventricular function. Representative echocardiograph images are movement-mode, parasternal short-axis views of a sham (A) and a heart failure (HF) rat (C). Macroscopic, transverse sections from representative hearts in a sham (B) and HF rat (D) are also shown. Note the thinning of the left ventricle infarcted wall (between arrows). AW, anterior wall; LVID,d and LVID,s: left ventricle internal dimension in diastole and systole; PW, posterior wall; LV, left ventricle; RV, right ventricle.
Table 1.
Summary data of echocardiography parameters obtained from sham and HF rats
| Group | EF, % | FS, % | LVIDd, mm | LVIDs, mm |
|---|---|---|---|---|
| Sham | 81.7 ± 1.8 | 53.2 ± 2.1 | 8.15 ± 0.2 | 3.95 ± 0.2 |
| HF | 43.6 ± 1.6* | 22.6 ± 1.0* | 8.16 ± 0.2 | 6.38 ± 0.2* |
Data are means ± SE of echocardiography parameters obtained from sham (n = 16) and heart failure (HF; n = 27) rats. EF, ejetion fraction; FS, fractional shortening; LVIDd and LVIDs, left ventricle internal dimension diastole and systole.
P < 0.0001 vs. sham.
Immunohistochemistry.
In a subpopulation of recordings, SON and PVN neurons were intracellularly filled with biocytin (0.2%) and processed for immunohistochemical detection of oxytocin and vasopressin immunoreactivities, as previously described (Stern et al. 1999). Briefly, slices were fixed overnight in 4% paraformaldehyde, then rinsed in 0.01 M PBS with 0.5% Triton X-100 (TX) for 10 min, and incubated for 45 min in 10% normal horse serum with 0.01 M PBS, 0.5% TX, and 0.04% NaN3. Slices were then thoroughly rinsed with 0.01 M PBS, 0.5% TX, and 0.04% NaN3, followed by a 48-h incubation with a guinea pig anti-oxytocin and a rabbit anti-vasopressin primary antibody (both used at 1:50,000 dilution; Bachem, Torrance, CA) in 0.01 M PBS, 0.5% TX, and 0.04% NaN3. Slices were then rinsed in 0.01 M PBS, 0.5% TX, and 0.04% NaN3 for 30 min and incubated 4 h with anti-guinea pig Cy3-labeled and anti-rabbit fluorescein isothiocyanate (FITC)-labeled secondary antibodies (1:400 dilution; both from Jackson ImmunoResearch Laboratories, West Grove, PA) in 0.01 M PBS, 0.5% TX, and 0.04% NaN3. Cy5-streptavidin (1:10,000) was added to reveal the biocytin-filled neuron. Slices were then thoroughly rinsed in 0.01 M PBS for 20 min, mounted, and visualized using fluorescence microscopy (×20 magnification; Olympus America, Melville, NY). Slices were then thoroughly rinsed in 0.01 M PBS for 20 min, mounted, and visualized using confocal microscopy (Zeiss LSM 510 confocal scanning microscope; Carl Zeiss, Oberkochen, Germany). A helium-neon laser was used to excite FITC and Cy3 fluorochromes at 488 and 561 nm, respectively, and an argon-krypton laser was used to excite Cy5 fluorochrome at 633 nm. Fluorescent signal cross talk among the channels was avoided by setting image acquisition parameters with individually labeled sections.
Hypothalamic slices preparation.
Hypothalamic brain slices were prepared according to methods previously described (Stern 2001). Briefly, rats were deeply anesthetized with pentobarbital sodium (40 mg/kg ip) and perfused through the heart with an ice-cold sucrose solution containing (in mM) 200 sucrose, 2.5 KCl, 3 MgSO4, 26 NaHCO3, 1.25 NaH2PO4, 20 d-glucose, 0.4 ascorbic acid, 1 CaCl2, and 2 pyruvic acid (290–310 mosmol/l). Rats were then quickly decapitated, brains dissected out, and coronal slices cut (300 μm thick) using a vibroslicer (DSK Microslicer; Ted Pella, Redding, CA). An oxygenated ice-cold artificial cerebrospinal fluid (ACSF) was used during slicing containing (in mM) 119 NaCl, 2.5 KCl, 1 MgSO4, 26 NaHCO3, 1.25 NaH2PO4, 20 d-glucose, 0.4 ascorbic acid, 2 CaCl2, and 2 pyruvic acid, pH 7.4 (290–310 mosmol/l). Slices were placed in a holding chamber containing ACSF and kept at room temperature until used.
Patch-clamp electrophysiology.
Slices were bathed with solutions (∼2.0 ml/min) that were continuously bubbled with 95% O2-5% CO2 and maintained at 32°C. Patch pipettes (3–4 MΩ) composed of thin-walled (1.5-mm outer diameter, 1.17-mm inner diameter) borosilicate glass (GC150T-7.5; Clark, Reading, UK), were pulled on a horizontal electrode puller (P-97; Sutter Instruments, Novato, CA). The internal solution contained (in mM) 135 Cs-methanesulfonate, 10 KCl, 10 HEPES, 1 MgCl, 0.2 EGTA, 4 MgATP, 0.3 GTP, and 20 phosphocreatine. Biocytin (0.2%) was added for cell labeling. For current-clamp recordings, Cs-methanesulfonate was replaced with K-gluconate. Recordings were obtained with an Axopatch 200B amplifier (Axon Instruments, Foster City, CA) from SON/PVN neurons using infrared differential interference contrast videomicroscopy. The voltage-output was digitized at 16-bit resolution, 10 kHz, and was filtered at 2 kHz (Digidata 1320A; Axon Instruments). Data was discarded if the series resistance was not stable throughout the entire recording (>20% change) or if neuronal input resistance was lower than 350 MΩ at the beginning of the recording. Spontaneous GABA inhibitory (sIPSCs) and glutamate excitatory postsynaptic currents (sEPSCs) were simultaneously recorded at a holding potential of −55 mV. At this membrane potential, and based on their different reversal potentials, IPSCs and EPSCs were distinguished by their outward and inward polarity, respectively (see Fig. 3A). Synaptic events were detected using Mini Analysis software (Synaptosoft, Leonia, NJ). The detection threshold was set at 10 and 8 pA for GABA IPSCs and glutamate EPSCs, respectively. Individual PSCs were aligned at the 50% crossing of the rising phase before averaging. PSC frequency and waveform parameters were analyzed using the same software. Charge transfer (Q) was calculated by integrating the area under the PSC waveform. The mean PSC synaptic current was calculated as the charge transfer of the averaged IPSC multiplied by mean PSC frequency (Park et al. 2006). IPSC bursts were detected using an algorithm included in the Mini Analysis software, using the following empirical criteria: rapid burst onset and a minimum of 5 clustered IPSCs with an inter-event interval <100 ms. To study the effect of gabazine (GBZ) on spontaneous EPSC frequency and properties, we analyzed events in 4-min periods before and after bath application of the drug. Firing discharge was recorded in the current-clamp mode in continuous mode. The mean firing frequency (2- to 3-min period) obtained before and after bath application of 15 μM 6,7-dinitroquinoxaline-2,3-dione (DNQX) was calculated and compared using Mini Analysis software. Cell capacitance was calculated by integrating the area under the transient capacitive phase of a 5-mV depolarizing step pulse in the voltage-clamp mode. DNQX, 6,7-dinitroquinoxaline-2,3-dione (d-AP5), GBZ, and tetrodotoxin (TTX) were purchased from Tocris Cookson (Bristol, UK). All drugs were dissolved directly in the ACSF, except for DNQX, which was dissolved in dimethyl sulfoxide (DMSO). The final concentration of DMSO was less than 0.1%.
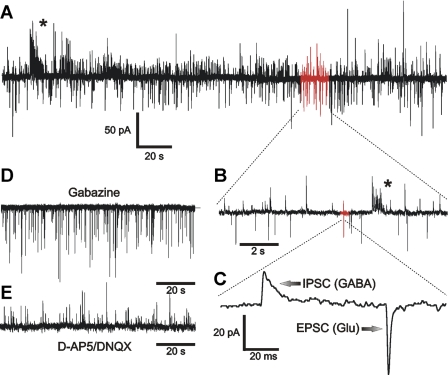
Fig. 3.
Simultaneous recordings of GABA inhibitory (IPSCs) and glutamate excitatory postsynaptic currents (EPSCs) in MNCs. A: representative trace showing inward EPSCs and outward IPSCs in a SON neuron from a sham rat. The red portion of the trace is further expanded in B, a red portion of which is then further expanded in C. Asterisks in A and B denote bursts of IPSCs. D: outward IPSCs were completely blocked by the GABAA receptor blocker gabazine (GBZ). E: inward EPSCs were completely blocked by the N-methyl-d-aspartate (NMDA) and α-amino-3-hydroxy-5-methylisoxazole-4-propionic acid (AMPA) receptor blockers 6,7-dinitroquinoxaline-2,3-dione (d-AP5; 100 μM) and 6,7-dinitroquinoxaline-2,3-dione (DNQX; 10 μM), respectively. Glu, glutamate.
Statistical analysis.
Numerical data are means ± SE. Student's paired t-tests were used to compare the effects of a drug treatment. Analysis of variance (ANOVA), followed by Bonferroni's post hoc tests, were used as needed.
RESULTS
Simultaneous recordings of GABAA IPSCs and glutamate EPSCs in identified MNC.
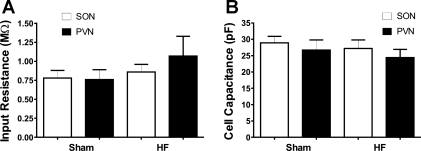
Patch-clamp electrophysiological recordings were obtained from a total of 87 MNCs obtained from sham (n = 45 MNCs from 16 rats) and HF rats (n = 42 MNCs from 27 rats). MNCs were located either in the SON (n = 70) or in the lateral magnocellular subnucleus of the PVN (n = 17). No differences in mean input resistance and cell capacitance were observed among groups (Fig. 2, A and B). Moreover, the basic properties of GABAA IPSCs and glutamate EPSCs, including amplitude, decay kinetics, and charge transfer Q in MNCs from the SON and PVN, were similar (Table 2). Finally, as summarized below, the main change found in IPSC and EPSC parameters in HF rats similarly affected both SON and PVN MNCs. Thus, for simplicity, data obtained from MNCs in these two nuclei were pooled together for subsequent analysis.
Fig. 2.
Basic membrane properties of magnocellular neurosecretory cells (MNCs) in sham and HF rats. Group data (means ± SE) show the mean input resistance (A) and cell capacitance (B) in supraoptic (SON) and paraventricular nuclei (PVN) MNCs in sham and HF rats.
Table 2.
Summary data of mean GABA IPSC and glutamate EPSC parameters in MNCs recorded from the SON and PVN in sham rats
| Amplitude, pA |
Decay Kinetics, ms |
Frequency, Hz |
||||
|---|---|---|---|---|---|---|
| MNCs | IPSC | EPSC | IPSC | EPSC | IPSC | EPSC |
| SON | 19.7 ± 1.9 | 19.6 ± 1.0 | 18.7 ± 2.5 | 2.3 ± 0.2 | 2.2 ± 0.6 | 1.7 ± 0.2 |
| PVN | 19.6 ± 0.9 | 17.0 ± 1.7 | 12.2 ± 1.3 | 2.9 ± 0.6 | 2.2 ± 0.4 | 1.5 ± 0.6 |
Data are means ± SE of mean GABA inhibitory postsynaptic current (IPSC) and glutamate excitatory postsynaptic current (EPSC) parameters in magnocellular neurosecretory cells (MNCs) recorded from the supraoptic (SON; n = 14) and paraventricular nuclei (PVN; n = 9) in sham rats.
GABAA-mediated IPSCs and glutamate-mediated EPSCs were simultaneously recorded within a recorded neuron (see methods). As shown in Fig. 3, at a recording holding potential of −55 mV, GABAA IPSCs appeared as outward currents and were completely blocked by GBZ or bicuculine (15 μM for both), whereas glutamate EPSCs appeared as inward currents and were completely blocked by a combination of AMPA and NMDA receptor antagonists d-AP5 (100 μM) and DNQX (10 μM), respectively. Thus GABAA and glutamate synaptic currents were distinguished on the basis of their polarity and pharmacological sensitivity.
Bath application of TTX (1 μM) failed to affect mean IPSC and EPSC frequencies in both sham and HF rats (P > 0.3 in all cases), indicating that in our recording conditions, spontaneous synaptic activity represented, for the most part, miniature synaptic currents (see more below).
Diminished GABAA synaptic strength in MNCs of HF rats.
The mean frequency of GABAA IPSCs did not differ between SON neurons from sham (n = 24) and HF (n = 29) rats (sham: 2.2 ± 0.3 Hz; HF: 1.7 ± 0.3 Hz; P > 0.2). Interestingly, bursts of GABAA IPSCs were observed in about one-half of SON neurons (25/49) (see Fig. 4A). In sham rats, ∼57% of MNCs (12/21) displayed IPSC bursts, with an average of 14.9 ± 3.6 bursts/cell (total number of bursts = 104) detected within a recording period of 10 min. IPSC bursts lasted on average 1.1 ± 0.1 s, contained 29.4 ± 2.2 clustered IPSCs, and displayed an intraburst frequency of 28.4 ± 1.2 Hz (n = 104 in all parameters). The mean charge transfer (i.e., area under the curve) per MNC mediated by GABAA IPSC bursts in sham rats was 198.5 ± 43.5 pA/ms. Importantly, although the overall mean frequency of GABAA IPSCs was not affected when action potentials were blocked with TTX (1 μM), GABA IPSC bursts were undetected in the presence of TTX (Fig. 4, A and B). In HF rats, ∼46% of MNCs (13/28) displayed IPSC bursts. However, the mean number of bursts per cell was significantly lower than that observed in sham rats (6.5 ± 1.3 bursts/cell, P < 0.05 vs. sham; total number of bursts = 52). The mean burst duration was also significantly shorter in MNCs from HF rats (0.78 ± 0.1 s, P < 0.02 vs. sham). All other IPSC burst parameters were not different from those observed in sham rats (not shown). Overall, the mean charge transfer per MNC mediated by GABAA IPSC bursts in HF rats was significantly lower than that in sham rats (97.0 ± 19.3 pA/ms, P < 0.05).
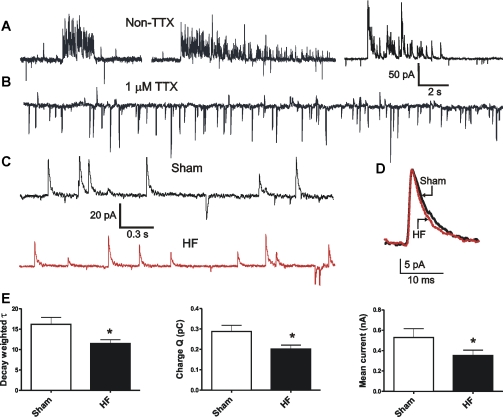
Fig. 4.
Diminished GABA IPSC strength in MNCs during HF. A: representative examples of GABA IPSC bursts recorded in MNCs from sham rats. B: GABAA IPSC bursts were absent in the presence of tetrodotoxin (TTX; 1 μM). C: representative examples of GABA IPSCs recorded in MNCs from a sham and a HF rat (red). D: averaged IPSCs obtained from the same MNCs as in C are shown superimposed. E: group data (means ± SE) showing differences in GABA IPSCs properties between sham and HF rats. *P < 0.05. τ, decay time constant; Q, charge transfer.
Representative examples of averaged IPSCs obtained from sham and HF rats are shown in Fig. 4D. As we previously reported (Park et al. 2006), the decay time course of the GABAA IPSC was best described by the sum of two exponentials. We found the IPSC mean weighted decay time constant τ to be significantly faster in SON neurons from HF rats than in those from sham rats (sham: 16.2 ± 1.7 ms; HF: 11.5 ± 0.9 ms, P < 0.02). Although the mean IPSC peak amplitude was not different between groups (sham: 19.8 ± 1.1 pA; HF: 19.4 ± 1.0 pA, P > 0.5), the mean IPSC charge transfer Q was significantly smaller in MNCs from HF rats (sham: 0.29 ± 0.03 pC; HF: 0.20 ± 0.02 pC; P < 0.02). Moreover, the mean current (i.e., charge transfer per unit of time) was also significantly smaller in HF rats (sham: 0.58 ± 0.03 pA; HF: 0.33 ± 0.04 pA; P < 0.02) (Fig. 4E). When analyzed separately according to nuclei location, the mean GABAA current in HF rats was significantly diminished in both SON (sham: 0.69 ± 0.12; HF: 0.32 ± 0.05, P < 0.01) and PVN MNCs (sham: 0.50 ± 0.08; HF: 0.27 ± 0.03, P < 0.05). No differences in IPSC rise time between sham and HF rats were observed (P > 0.5 in both cases; not shown).
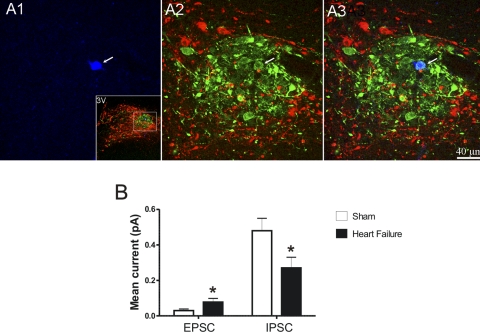
In a limited number of cases, we successfully immunoidentified recorded MNCs as VP in sham and HF rats (n = 9 and 7, respectively; see Fig. 6). Our results show that the mean GABAA current was significantly diminished in VP neurons from HF rats (sham: 0.48 ± 0.07; HF: 0.27 ± 0.06, P < 0.05).
Fig. 6.
Changes in GABAA IPSCs and glutamate EPSCs in immunoidentified vasopressin (VP) MNCs during HF. A: representative example of recorded and immunoidentified VP MNC in the PVN. In A1, the intracellularly labeled MNC revealed with Cy5-streptavidin is shown (blue, arrow). In A2, the same section was stained with antibodies against VP (green) and oxytocin (red). Note the ball-shaped lateral magnocellular subnucleus. In A3, the 2 images are superimposed to show colocalization of blue and green (white color, arrow). The inset in A1 shows the same section at a lower magnification (3V, third ventricle). B: group data (means ± SE) showing differences in EPSC and IPSC mean current in immunoidentified VP MNCs between sham and HF rats. *P < 0.05.
Enhanced glutamate synaptic strength in MNCs of HF rats.
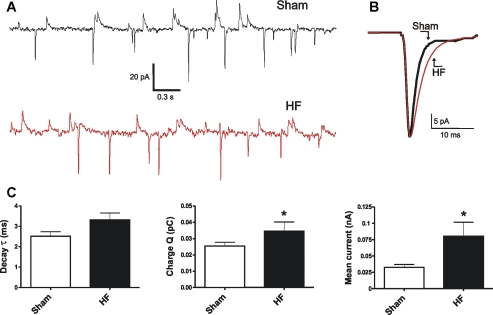
Representative examples of glutamate EPSCs recorded in MNCs in sham (n = 20) and HF rats (n = 24) are shown in Fig. 5A. Differently from GABAA IPSCs, glutamate EPSCs occurred in a rather irregular manner, and bursts of events were rarely observed only in a few cells, preventing any further analysis of this phenomenon. No differences in the frequency of glutamate EPSCs were observed between sham and HF rats (sham: 1.38 ± 0.16 Hz; HF: 1.37 ± 0.17 Hz; P > 0.2). However, and in contrast to GABAA IPSCs, the strength of the glutamate EPSCs was enhanced in MNCs from HF rats. Thus the averaged EPSC in HF rats displayed slower decay kinetics, although values did not reach statistical significance: monoexponential decay τ (sham: 2.5 ± 0.2 ms; HF: 3.3 ± 0.3 ms, P = 0.07), larger Q (sham: 0.02 ± 0.002 pC; HF: 0.03 ± 0.005 pC; P < 0.05), and larger mean current (sham: 0.03 ± 0.004 pA, HF: 0.08 ± 0.02 pA, P < 0.05). When analyzed separately according to nuclei location, the mean glutamate current in HF rats was significantly larger in MNCs from both the SON (sham: 0.04 ± 0.001; HF: 0.08 ± 0.02, P < 0.05) and the PVN (sham: 0.03 ± 0.09; HF: 0.12 ± 0.05, P < 0.05). No differences in EPSC rise time or amplitude between sham and HF rats were observed (P > 0.5 in both cases; not shown). In the case of immunoidentified VP MNCs, we also observed a significant increase in the mean glutamate current in HF compared with sham rats (see Fig. 6; sham: 0.03 ± 0.01; HF: 0.08 ± 0.02, P < 0.05, n = 7 and 8, respectively).
Fig. 5.
Enhanced glutamate EPSC strength in MNCs of HF rats. A: representative examples of glutamate EPSCs recorded in MNCs from a sham and a HF rat (red). B: averaged EPSCs obtained from the same MNCs as in A are shown superimposed. C: group data (means ± SE) showing differences in glutamate EPSCs properties between Sham and HF rats. *P < 0.05.
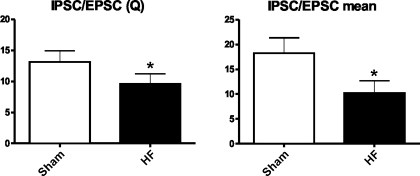
Altered inhibitory-excitatory balance in MNCs of HF rats.
By simultaneously recording GABAA IPSCs and glutamate EPSCs within individual neurons, we were able to calculate the relative contribution and changes in balance between these opposing synaptic inputs within individual neurons in both experimental conditions (see methods). As shown in Fig. 7, the ratios of IPSC-to-EPSC charge transfer Q and mean current indicate that in both conditions, GABA synaptic strength predominated over glutamate strength (i.e., ratios > 1). However, both the Q and mean current ratios were significantly diminished in MNCs of HF rats (P < 0.05 in both cases), supporting a shift in the GABA-glutamate balance toward more excitatory predominance.
Fig. 7.
Group data (means ± SE) showing a diminished IPSC-to-EPSC Q ratio (A) and a diminished IPSC-to-EPSC mean current ratio (B) in MNCs from HF rats. *P < 0.05.
GABA IPSCs differentially influence the variability of glutamate EPSCs in sham and HF rats.
We then tested for possible functional interactions between GABA and glutamate synaptic inputs and whether this interaction was altered in HF rats. First, we found no significant correlations between IPSC and EPSC frequency, amplitude, decay kinetics, and Q within individual MNCs in both sham and HF rats (Pearson r value range: −0.3–0.3, P > 0.5 in all cases). We then evaluated the effects of blockade of GABA synaptic activity on glutamate synaptic properties by comparing the properties of EPSCs before and after bath application of the GABAA receptor blocker GBZ (15 μM). A representative example is shown in Fig. 8A. Blockade of GABAergic synaptic activity had no effect on mean EPSC frequency (P > 0.1 and 0.5 for sham and HF, respectively), decay τ (P > 0.6 for both sham and HF), amplitude (P > 0.8 and 0.1 for sham and HF, respectively), Q (P > 0.8 and 0.3 for sham and HF, respectively), or mean current (P > 0.5 in both sham and HF).
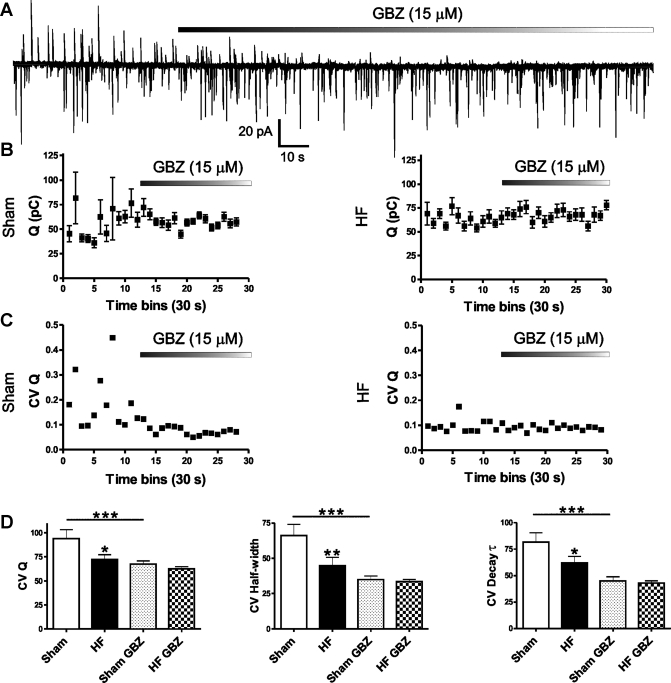
Fig. 8.
GABA IPSCs differentially influence the variability of glutamate EPSCs in sham and HF rats. A: representative example showing the effects of GBZ on GABA IPSCs and glutamate EPSCs obtained from a MNC in a sham rat. B: representative examples (means ± SE) of plots of mean EPSC Q over time (30-s bins) from a sham (left) and a HF rat (right) before and after bath application of GBZ. C: representative examples (means ± SE) of plots of coefficient of variation of EPSC charge transfer (CV Q) time (30-s bins) from the same MNCs shown in B, before and after bath application of GBZ. D: group data (means ± SE) showing mean CV for EPSC Q (left), EPSC half-width (middle), and EPSC decay τ (right) in sham and HF rats before and after GBZ. *P < 0.05; **P < 0.01 vs. sham. ***P < 0.001.
On the other hand, blockade of GABA function significantly and differentially affected glutamate EPSC waveform variability in sham and HF rats. Representative examples for EPSC Q in MNCs from sham and HF rats are shown in Fig. 8B. A plot of the mean EPSC Q value as a function of time (30-s bins) in a sham rat (Fig. 8B, left) shows a high basal Q variability over time, which was largely diminished when GBZ was added to the bath. The same phenomenon was observed when the coefficient of variation (CV) of Q was plotted over time (Fig. 8C, left). Conversely, a recording from a typical MNC in a HF rat showed a much lower basal variability in Q, which was not modified by blockade of GABAergic synaptic function (Fig. 8, B and C, right). Results from two-way ANOVA (Fig. 8D) showed that in MNCs from sham rats (n = 24), GBZ significantly diminished the CV for EPSC Q, half-width, and decay τ (P < 0.001 in all cases, Bonferroni posttest). The basal variability of these EPSC parameters in MNCs from HF rats (n = 27) was already smaller than that of sham rats (P < 0.05 for Q and decay τ, and P < 0.01 for half-width, Bonferroni posttest). Finally, blockade of GABA synaptic activity in MNCs of HF rats failed to affect the already lower EPSC variability (P > 0.5 for all parameters). No effects of GBZ or differences between sham and HF rats were observed in any other EPSC parameter studied (not shown).
Mechanisms contributing to prolonged EPSC kinetics in HF rats.
To determine whether a more pronounced electrotonic filtering contributed to the EPSC slower decay kinetics and enhanced charge transfer in HF rats, we measured first the correlation between EPSC rise time and decay time, a well-established index of dendritic filtering PSCs due to membrane cable properties. Our results show a lack of significant correlation between EPSC rise time and decay time in both sham and HF groups (mean r2 sham: 0.12 ± 0.03; mean r2 HF: 0.11 ± 0.01). Moreover, we arbitrarily divided glutamate EPSCs into fast (rise time <1 ms) and slow (rise time >1 ms) currents and compared the ratio of slow-to-fast EPSCs within individual neurons in sham and HF rats. Our results show similar ratios in sham and HF rats (sham: 2.0 ± 0.2; HF: 2.4 ± 0.6, P > 0.2, n = 23 in each group). Together, these results argue against enhanced electrotonic dendritic filtering as a factor contributing to slower mean EPSC kinetics in MNCs of HF rats.
We then tested the effects of d-AP5, an NMDA receptor blocker, on EPSC decay kinetics. Bath application of d-AP5 (100 μM) failed to alter EPSC decay τ in MNCs from both sham and HF rats (P > 0.5 in both cases, paired t-test, n = 6 in each group), suggesting that an enhanced, slow NMDA EPSC component did not contribute to EPSC prolongation in MNCs of HF rats.
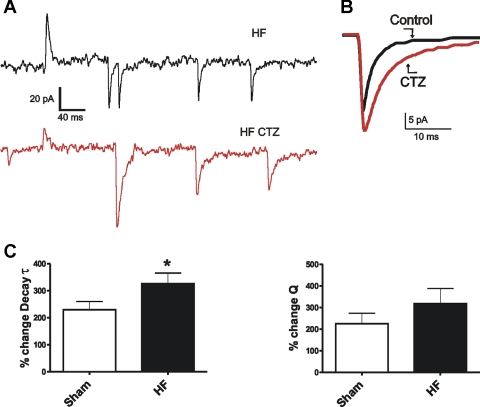
Finally, we assessed whether differences in AMPA receptor desensitization, a prominent factor known to dictate glutamate EPSC decay kinetics (Jones and Westbrook 1996), contributed to slower EPSC decay kinetics in HF rats. Results are summarized in Fig. 9, A–C. Bath application of cyclothiazide (CTZ; 200 μM), a blocker of AMPA receptor desensitization (Yamada and Tang 1993), resulted in a robust prolongation of EPSC decay kinetics in both sham and HF rats. However, the CTZ effect on EPSC decay τ was on average significantly larger in MNCs from HF rats (%change in EPSC τ sham: 207.1 ± 23.5; %change in EPSC τ HF: 325.9 ± 39.6, P < 0.02, n = 10 and 8, respectively; Fig. 9C). Similar differences between sham and HF rats were observed when comparing the effects of CTZ on EPSC Q; however, results did not reach statistical significance (P = 0.08).
Fig. 9.
Differences in EPSC desensitization between MNCs in sham and HF rats. A: representative traces obtained from a MNC in a HF rat showing glutamate EPSCs before and after (red) bath application of the AMPA receptor desensitization blocker cyclothiazide (CTZ; 200 μM). B: averaged EPSCs before and after CTZ application, obtained from the same MNC, are shown superimposed. C: group data (means ± SE) showing CTZ-mediated mean %changes in EPSC decay τ (left) and EPSC Q (right) in MNCs obtained from sham and HF rats. *P < 0.02.
Enhanced contribution of glutamate EPSCs to firing activity in MNCs of HF rats.
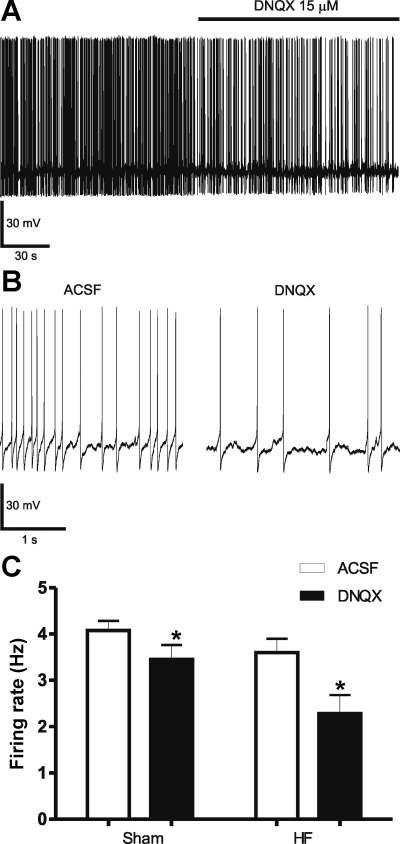
To determine whether the enhanced EPSC charge transfer observed in MNCs of HF rats had an impact on firing activity, we obtained current-clamp recordings and monitored changes in firing activity evoked by the AMPA receptor blocker DNQX. Basal firing rate was highly variable among recorded neurons in both sham and HF rats. Thus DC current was injected in an attempt to homogenize basal firing rate within a range of 3.5–4.5 Hz. Under this condition, bath application of DNQX (15 μM) significantly diminished MNC firing discharge in both sham (basal: 4.07 ± 0.21 Hz; DNQX: 3.45 ± 0.31, P < 0.01, n = 13, paired t-test) and HF rats (basal: 3.60 ± 0.30 Hz; DNQX: 2.28 ± 0.4, P < 0.01, n = 9, paired t-test) (Fig. 10, A–C). The magnitude of the DNQX effect, however, was significantly larger in HF compared with sham rats. Thus DNQX inhibited firing discharge by 13.4 ± 4.5% and 37.2 ± 11.3% in MNCs from sham and HF rats, respectively (P < 0.05). No differences in interspike interval CV were observed among experimental groups (P > 0.2, not shown).
Fig. 10.
Effect of AMPA receptor blockade on MNC firing activity in sham and HF rats. A: representative example of firing discharge in a MNC from a HF rat before and during bath application of the AMPA receptor blocker DNQX (15 μM). B: 2 segments of the same trace in A are shown at a more expanded time scale. C: group data (means ± SE) showing the effects of DNQX on MNCs from sham (n = 13) and HF rats (n = 9). *P < 0.01 vs. artificial cerebrospinal fluid (ACSF).
DISCUSSION
Diminished inhibitory GABAergic and enhanced excitatory glutamatergic synaptic strength in MNCs of HF rats.
In this work, we aimed to determine whether GABAergic inhibitory and glutamatergic excitatory synaptic activity and strength were altered in MNCs of HF rats. Our results support, on one hand, a diminished GABAergic synaptic strength in MNCs during HF. This is reflected by faster decaying GABAA IPSCs, diminished IPSC charge transfer Q, and diminished mean GABA current (i.e., charge transfer per unit of time) in HF rats. Conversely, we found an enhanced glutamate excitatory synaptic strength in MNCs during HF, reflected by slower decaying EPSCs, resulting in turn in an enhanced charge transfer Q and mean current in this condition. Although our results demonstrate significant changes in IPSC and EPSC waveform in HF rats, no differences in the mean frequency of spontaneous synaptic events (either inhibitory or excitatory) were observed between experimental groups. As previously reported in MNCs (Kabashima et al. 1997; Kombian et al. 2000b; Li et al. 2007; Stern et al. 1999), we found the mean frequency of IPSCs and EPSCs, in both sham and HF rats, to be unaffected when action potential-dependent activity was blocked with TTX (see, however, effects on IPSC bursts described below), suggesting that the great majority of PSCs in our slice preparation represented miniature synaptic events (mPSCs). Thus it is reasonable to conclude that the differences in mPSC waveform (but not in frequency) observed between MNCs in sham and HF rats support a postsynaptic locus underlying altered PSC strength in this condition (Redman and Silinsky 1995).
An important caveat related to this conclusion, however, is that the frequency of events recorded in the slice preparation is limited to the activity within the local networks of GABAergic and glutamatergic interneurons. These have been shown to be mostly located in perinuclear regions around the SON and PVN, as well as other intrahypothalamic areas (Boudaba et al. 1996, 1997; Roland and Sawchenko 1993), most of which are preserved in the slice preparation. On the other hand, more distal as well as peripheral afferent inputs are cut off from this preparation. Thus, although our studies cannot rule out potential differences in the degree of afferent input activity to MNCs between sham and HF rats, the postsynaptic mechanisms underlying blunted and enhanced GABA and glutamate strengths, respectively, are still expected to affect neuronal responses to afferent input activation during HF.
As previously reported in MNCs of female rats (Li et al. 2007), we found GABAergic synaptic activity and strength in male control rats to prevail over glutamatergic activity. This was reflected by a higher frequency of IPSCs over EPSCs (∼1.6-fold higher), as well as a larger IPSC-to-EPSC charge transfer (∼14-fold larger), even considering that in our recording conditions, the driving force for glutamate EPSCs (∼55 mV) was larger than that from GABA IPSCs (∼10 mV). Altogether, these differences result in a larger mean IPSC current compared with that of EPSC (IPSC/EPSC ∼19-fold larger). Although GABA strength still predominated over glutamate strength in HF rats, the opposing changes observed in GABA IPSC and glutamate EPSC waveforms resulted in a shift in the GABA-glutamate balance toward a relatively stronger glutamate influence in this disease condition. We confirmed these opposing changes in the strength of IPSCs and EPSCs in HF rats to occur in a subset of immunoidentified VP MNCs. Whether OT neurons are similarly affected remains to be determined.
Interestingly, the changes in GABA and glutamate synaptic function reported presently in MNCs during HF differ from those we recently reported in PVN presympathetic neurons that innervate either the rostral ventrolateral medulla (PVN-RVLM) or sympathetic preganglionic neurons in the intermediolateral column of the spinal cord (PVN-IML) (Han et al. 2010). In the case of PVN-RVLM neurons, GABA IPSC frequency (but not waveform) was diminished in HF rats, whereas no changes in glutamate EPSCs were observed. On the other hand, GABA and glutamate synaptic activity were unaffected in PVN-IML neurons in HF rats. Together, our studies suggest that synaptic function during HF is affected in a cell type-dependent manner, indicating that different mechanisms contribute to sympathetic and neuroendocrine activation in this condition.
Blunted GABAergic IPSC bursts in MNCs of HF rats.
In agreement with a recent study by Popescu et al. (2010), we found that in addition to occurring in a random stochastic manner, GABA IPSCs clustered in high-frequency bursts were also observed in ∼60% of MNCs in sham rats. These bursts of IPSCs were on average composed of ∼30 events and lasted for ∼1 s. Popescu et al. (2010) elegantly demonstrated that although IPSC bursts persisted when action potentials were blocked with TTX, the probability of burst generation was drastically diminished to a frequency of about 1 burst/h. Thus the fact that, in our case, IPSC bursts were absent in the presence of TTX during a 10-min recording period could simply reflect a diminished frequency, rather than a spike-dependent nature. Our results indicate that the incidence, duration, and overall charge transfer mediated by GABA IPSC bursts were significantly diminished in MNCs from HF rats. Given that GABA synaptic bursts were shown to efficiently terminate firing activity in active neurons (Popescu et al. 2010), it is reasonable to speculate that the diminished incidence and strength of GABA IPSC bursts in HF rats may also contribute to enhanced excitability and prolonged firing discharge of MNCs during this condition.
Differential contribution of GABAergic IPSCs to glutamate EPSCs irregularity during HF.
To gain insights into potential pre- and/or postsynaptic interactions between GABAergic and glutamatergic synaptic inputs in MNCs, we evaluated the impact of blocking GABAA IPSCs on various parameters of glutamate EPSCs. Our result show that blockade of GABA IPSCs failed to affect the mean EPSC frequency in either sham or HF rats. This is in contrast to the increased EPSC frequency induced by IPSC blockade that we recently reported in presympathetic PVN-RVLM neurons (Li et al. 2006), further supporting a differential organization of synaptic inputs among functionally distinct neuronal populations in the SON and PVN. Surprisingly, however, we found ongoing GABAergic synaptic activity in MNCs to influence the degree of heterogeneity of the postsynaptic glutamate EPSC waveform. Thus, although blockade of GABA IPSCs did not affect EPSC parameter mean values (e.g., frequency, amplitude, decay time course), the variance (expressed as CV) of the EPSC decay τ, half-width, and Q was significantly diminished, with EPSCs thus becoming largely more homogeneous. In line with our results showing diminished IPSC strength in HF rats, we found the basal variance of these same EPSC parameters to be significantly lower in HF rats. Moreover, the effect of GBZ on EPSC variability was blunted in HF rats. Together, these results suggest that ongoing GABA IPSCs impart irregularity to glutamate EPSCs and that blunted GABA strength results in more homogeneous EPSC in HF rats. What mechanism could underlie such a type of interaction between GABA and glutamate PSCs? Although counterintuitive, one possibility is that blockade of GABA results in the predominance of a restricted group of synapses (e.g., closer to soma), leading in turn to more homogeneous EPSCs. However, the fact that the mean EPSC rise time (which is partially dependent on the relative location of the EPSC occurrence relative to the recording site) and its CV did not change following IPSC blockade would argue against this possibility. Alternatively, GABAA-mediated IPSCs could postsynaptically affect the properties of glutamate EPSCs in a way that intermittent, stochastically occurring IPSCs result in high EPSC variance. Evidently, the underlying mechanism by which GABAergic activity influences regularity of EPSC properties remains to be determined.
AMPA receptor desensitization contributes to increased glutamate EPSC strength in HF rats.
A major finding emerging from our work is that prolongation of the EPSC time course is a major contributing factor to enhance glutamate EPSC strength in MNCs in HF rats. In our recording conditions, the EPSC in MNCs, in both sham and HF rats, was mediated by activation of AMPA receptors (i.e., AP5 failed to affect any EPSC property). The decay time course of AMPA EPSCs is largely determined by the relative contribution of channel deactivation and desensitization kinetics (the latter being typically a slower process than channel deactivation) (Jonas and Spruston 1994). Importantly, changes in their relative contribution can strongly affect AMPA decay kinetics. For example, a diminished contribution of AMPA receptor desensitization has been shown to result in developmental speeding of EPSCs in the calyx of Held (Koike-Tani et al. 2005) and auditory synapses in the cochlear nucleus (Brenowitz and Trussell 2001). Conversely, the contribution of AMPA receptor desensitization to the EPSC decay in cerebellar granule cell synapses increases during development (Wall et al. 2002). Thus one possible explanation for the prolongation of AMPA EPSC time course in MNCs of HF rats (and thus the enhanced unitary strength) is an increased contribution of channel desensitization. This is in fact supported by our results showing a more robust effect of CTZ in HF rats, a compound that blocks desensitization of AMPA receptors (Yamada and Tang 1993). This is in line, for example, with the enhanced CTZ effect on EPSC time course at early developmental stages at the calyx of Held, when stronger desensitization contributes to slower EPSCs (Koike-Tani et al. 2005). Multiple factors could potentially contribute to the increased AMPA receptor desensitization in MNCs of HF rats, including changes in their molecular configurations. AMPA receptors are multimeric assemblies of four different subunits (GLUR1–GLUR4), and their relative expression, as well as splice variants (e.g., Flip/Flop forms), affects AMPA receptor functional properties, including desensitization (Lambolez et al. 1996; Mosbacher et al. 1994). Alternatively, prolongation of glutamate time course in the synaptic cleft due to diminished transmitter clearance could also result in enhanced AMPA receptor desensitization and slower EPSCs (Barbour et al. 1994; Trussell et al. 1993). An increased glutamate release probability, resulting in multivesicular release from individual sites, could also contribute to prolongation of AMPA decay time course (Otis et al. 1996; Trussell et al. 1993). Thus future studies are needed to address the specific mechanisms underlying enhanced AMPA receptor desensitization in MNCs of HF rats. Similarly, although our studies focused on glutamate EPSCs, it will be important to elucidate in future studies whether changes in deactivation/desensitization properties (known to efficiently influence GABAA IPSC waveform; Modi et al. 1994) also contribute to blunted IPSC strength in HF rats.
Enhanced glutamate EPSC strength contributes to firing activity in MNCs in HF rats.
The functional relevance of the changes in glutamate EPSCs reported presently is highlighted by our results showing a more pronounced inhibitory effect of AMPA receptor blockade on firing discharge in MNCs from HF compared with sham rats. Given that hormone release from the pituitary is largely influenced by the firing discharge of MNCs (Cazalis et al. 1985; Poulain and Wakerley 1982; Silverman and Zimmerman 1983), our results showing a stronger contribution of AMPA receptors to firing discharge in HF rats are in line with the reported elevated plasma VP levels in HF (Francis et al. 1990; Goldsmith et al. 1983; Riegger et al. 1985; Szatalowicz et al. 1981), as well as an in vivo study showing increased firing discharge of nonidentified PVN neurons in HF rats (Zhang et al. 2002b). We acknowledge, however, that factors other than MNC firing discharge may also influence pituitary hormone release, contributing in turn to elevated plasma VP levels during HF. Unfortunately, to the best of our knowledge, studies directly assessing changes in VP and OT pituitary hormone release during HF, both under basal conditions or in response to osmotic or visceral afferent inputs, are still missing. These studies are undoubtedly needed to more comprehensively evaluate mechanisms leading to altered neurohypophysial regulation in HF conditions.
Given the lack of differences in EPSC frequency between these two conditions, our results suggest that postsynaptic mechanisms underlying an enhanced AMPA receptor unitary charge transfer contribute to an enhanced excitatory drive in MNCs of HF rats. Although we did not directly record isolated NMDA-mediated currents, we failed to detect a contribution of NMDA receptors to the prolonged kinetics and enhanced strength of glutamate inputs to MNCs in HF rats. Interestingly, Li et al. 2003 previously reported an enhanced expression and activation of NMDA receptors in the PVN, as underlying mechanisms contributing to sympathoexcitation in HF rats. On the other hand, the expression of AMPA receptors in HF rats was not changed. Thus these results may suggest a differential contribution of AMPA and NMDA receptors to neuroendocrine and sympathetic activation in HF rats.
The functional significance of basal differences in AMPA EPSC waveform variability between sham and HF rats (more homogeneous properties in the later), as well as the differential effect of GABAA receptor blockade on EPSC variability between conditions, are more difficult to assess and to interpret. In this sense, spontaneous GABA IPSCs, but not glutamate EPSCs, were recently shown to impart irregularity to spiking activity in SON MNCs (Li et al. 2007). The lack of changes in action potential firing regularity (i.e., interspike interval CV) following AMPA receptor blockade, in both sham and HF rats, is in line with these previous results. However, in addition to influencing spike frequency variability, differences in EPSC waveforms could also affect the temporal precision and the reliability of spike firing, as shown in cortical neurons (Mainen and Sejnowski 1995; Rodriguez-Molina et al. 2007; Softky and Koch 1993). Whether this is also the case in MNCs, however, is at present unknown.
The lack of effects of TTX on EPSC and IPSC frequencies indicate that changes in synaptic activity and function reported in this study during HF reflect differences in spontaneous miniature currents. Importantly, spontaneous synaptic activity has recently emerged as a functionally meaningful communication modality in the central nervous system (Kavalali et al. 2011; Otsu and Murphy 2003). In fact, spontaneous synaptic activity has been shown to influence both the degree and pattern of firing discharge in MNCs (Kombian et al. 2000a; Li et al. 2007; Popescu et al. 2010). Our results further support this notion and suggest that changes in postsynaptic efficacy following spontaneous release of neurotransmitter may be of sufficient magnitude to mediate changes in neuronal activity during pathological conditions, such as HF. Whether this occurs also in vivo, however, and the extent to which hormone release is affected by changes in spontaneous synaptic efficacy, remains to be determined.
Perspectives
Regulation of VP release is a multifactorial and tightly regulated process. The primary stimulus for VP release is an increase in plasma osmolality, conveyed to VP neurons largely via glutamate excitatory osmosensitive inputs (McKinley et al. 1992). VP release can also be stimulated by hypotension or plasma volume depletion, via cardiopulmonary volume/pressure-sensitive visceral inputs, resulting in local modulation of GABAergic inhibitory function (disinhibition) (Cunningham et al. 2002). Thus changes in the glutamate-GABA balance reported in this work are expected to affect neuronal responsiveness to these visceral afferent stimuli, contributing ultimately to the enhanced VP release characteristic of HF. For example, it is reasonable to speculate that an enhanced excitatory glutamate function, along with a diminished inhibitory GABA function in VP neurons, will diminish the efficacy of inhibitory afferent reflexes, such as the volume expansion reflex inhibition of VP release (Cunningham et al. 2002). In fact, numerous studies support blunted volume-dependent reflexes in HF (DiBona et al. 1988; Packer 1988; Patel et al. 1996), a mechanism that would explain persistently elevated VP levels in a volume-expanded condition such as HF. Conversely, osmosensitive, glutamate-dependent VP responses are expected to be exacerbated by the same synaptic balance shift. Thus, even though hyperosmolality is not commonly observed in HF patients, an increased efficacy of osmosensitive afferent pathway could reset the osmotic regulation of VP, contributing in turn to enhanced VP release in this condition. Clearly, future studies evaluating osmoregulation of VP release in animal models and patients with HF are warranted.
GRANTS
This work was supported National Heart, Lung, and Blood Institute Grant HL085767 (to J. E. Stern).
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the author(s).
REFERENCES
- Arnolda L, McGrath BP, Cocks M, Johnston CI. Vasoconstrictor role for vasopressin in experimental heart failure in the rabbit. J Clin Invest 78: 674–679, 1986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbour B, Keller BU, Llano I, Marty A. Prolonged presence of glutamate during excitatory synaptic transmission to cerebellar Purkinje cells. Neuron 12: 1331–1343, 1994 [DOI] [PubMed] [Google Scholar]
- Boudaba C, Schrader LA, Tasker JG. Physiological evidence for local excitatory synaptic circuits in the rat hypothalamus. J Neurophysiol 77: 3396–3400, 1997 [DOI] [PubMed] [Google Scholar]
- Boudaba C, Szabo K, Tasker JG. Physiological mapping of local inhibitory inputs to the hypothalamic paraventricular nucleus. J Neurosci 16: 7151–7160, 1996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourque CW, Oliet SH, Kirkpatrick K, Richard D, Fisher TE. Extrinsic and intrinsic modulatory mechanisms involved in regulating the electrical activity of supraoptic neurons. Ann NY Acad Sci 689: 512–519, 1993 [DOI] [PubMed] [Google Scholar]
- Brenowitz S, Trussell LO. Maturation of synaptic transmission at end-bulb synapses of the cochlear nucleus. J Neurosci 21: 9487–9498, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cazalis M, Dayanithi G, Nordmann JJ. The role of patterned burst and interburst interval on the excitation-coupling mechanism in the isolated rat neural lobe. J Physiol 369: 45–60, 1985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatterjee K. Neurohormonal activation in congestive heart failure and the role of vasopressin. Am J Cardiol 95: 8B–13B, 2005 [DOI] [PubMed] [Google Scholar]
- Cohn JN, Levine TB, Francis GS, Goldsmith S. Neurohumoral control mechanisms in congestive heart failure. Am Heart J 102: 509–514, 1981 [DOI] [PubMed] [Google Scholar]
- Creager MA, Faxon DP, Cutler SS, Kohlmann O, Ryan TJ, Gavras H. Contribution of vasopressin to vasoconstriction in patients with congestive heart failure: comparison with the renin-angiotensin system and the sympathetic nervous system. J Am Coll Cardiol 7: 758–765, 1986 [DOI] [PubMed] [Google Scholar]
- Cunningham JT, Bruno SB, Grindstaff RR, Grindstaff RJ, Higgs KAN, Mazzella D, Sullivan MJ. Cardiovascular regulation of supraoptic vasopressin neurons. Prog Brain Res 139: 257–273, 2002 [PubMed] [Google Scholar]
- Decavel C, Van den Pol AN. GABA: a dominant neurotransmitter in the hypothalamus. J Comp Neurol 302: 1019–1037, 1990 [DOI] [PubMed] [Google Scholar]
- DiBona G, Herman PJ, Sawin LL. Neural control of renal function in edema-forming states. Am J Physiol Regul Integr Comp Physiol 254: R1017–R1024, 1988 [DOI] [PubMed] [Google Scholar]
- Francis GS, Benedict C, Johnstone DE, Kirlin PC, Nicklas J, Liang CS, Kubo SH, Rudin-Toretsky E, Yusuf S. Comparison of neuroendocrine activation in patients with left ventricular dysfunction with and without congestive heart failure. A substudy of the Studies of Left Ventricular Dysfunction (SOLVD). Circulation 82: 1724–1729, 1990 [DOI] [PubMed] [Google Scholar]
- Goldsmith SR, Francis GS, Cowley AW., Jr Arginine vasopressin and the renal response to water loading in congestive heart failure. Am J Cardiol 58: 295–299, 1986a [DOI] [PubMed] [Google Scholar]
- Goldsmith SR, Francis GS, Cowley AW, Jr, Goldenberg IF, Cohn JN. Hemodynamic effects of infused arginine vasopressin in congestive heart failure. J Am Coll Cardiol 8: 779–783, 1986b [DOI] [PubMed] [Google Scholar]
- Goldsmith SR, Francis GS, Cowley AW, Jr, Levine TB, Cohn JN. Increased plasma arginine vasopressin levels in patients with congestive heart failure. J Am Coll Cardiol 1: 1385–1390, 1983 [DOI] [PubMed] [Google Scholar]
- Grindstaff RR, Cunningham JT. Lesion of the perinuclear zone attenuates cardiac sensitivity of vasopressinergic supraoptic neurons. Am J Physiol Regul Integr Comp Physiol 280: R630–R638, 2001 [DOI] [PubMed] [Google Scholar]
- Haanwinckel MA, Elias LK, Favaretto AL, Gutkowska J, McCann SM, Antunes-Rodrigues J. Oxytocin mediates atrial natriuretic peptide release and natriuresis after volume expansion in the rat. Proc Natl Acad Sci USA 92: 7902–7906, 1995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han TH, Lee K, Park JB, Ahn D, Park JH, Kim DY, Stern JE, Lee SY, Ryu PD. Reduction in synaptic GABA release contributes to target-selective elevation of PVN neuronal activity in rats with myocardial infarction. Am J Physiol Regul Integr Comp Physiol 299: R129–R139, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasser EM, Bishop VS, Hay M. Interactions between vasopressin and baroreflex control of the sympathetic nervous system. Clin Exp Pharmacol Physiol 24: 102–108, 1997 [DOI] [PubMed] [Google Scholar]
- Hatton GI. Emerging concepts of structure-function dynamics in adult brain: the hypothalamo-neurohypophysial system. Prog Neurobiol 34: 437–504, 1990 [DOI] [PubMed] [Google Scholar]
- Hodsman GP, Kohzuki M, Howes LG, Sumithran E, Tsunoda K, Johnston CI. Neurohumoral responses to chronic myocardial infarction in rats. Circulation 78: 376–381, 1988 [DOI] [PubMed] [Google Scholar]
- Jhamandas JH, Renaud LP. A gamma-aminobutyric-acid-mediated baroreceptor input to supraoptic vasopressin neurones in the rat. J Physiol 381: 595–606, 1986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson AK, Thunhorst RL. The neuroendocrinology of thirst and salt appetite: visceral sensory signals and mechanisms of central integration. Front Neuroendocrinol 18: 292–353, 1997 [DOI] [PubMed] [Google Scholar]
- Jonas P, Spruston N. Mechanisms shaping glutamate-mediated excitatory postsynaptic currents in the CNS. Curr Opin Neurobiol 4: 366–372, 1994 [DOI] [PubMed] [Google Scholar]
- Jones MV, Westbrook GL. The impact of receptor desensitization on fast synaptic transmission. Trends Neurosci 19: 96–101, 1996 [DOI] [PubMed] [Google Scholar]
- Kabashima N, Shibuya I, Ibrahim N, Ueta Y, Yamashita H. Inhibition of spontaneous EPSCs and IPSCs by presynaptic GABAB receptors on rat supraoptic magnocellular neurons. J Physiol 504: 113–126, 1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavalali ET, Chung C, Khvotchev M, Leitz J, Nosyreva E, Raingo J, Ramirez DM. Spontaneous neurotransmission: an independent pathway for neuronal signaling? Physiology (Bethesda) 26: 45–53, 2011 [DOI] [PubMed] [Google Scholar]
- Kleiber AC, Zheng H, Schultz HD, Peuler JD, Patel KP. Exercise training normalizes enhanced glutamate-mediated sympathetic activation from the PVN in heart failure. Am J Physiol Regul Integr Comp Physiol 294: R1863–R1872, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleiber AC, Zheng H, Sharma NM, Patel KP. Chronic AT1 receptor blockade normalizes NMDA-mediated changes in renal sympathetic nerve activity and NR1 expression within the PVN in rats with heart failure. Am J Physiol Heart Circ Physiol 298: H1546–H1555, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koike-Tani M, Saitoh N, Takahashi T. Mechanisms underlying developmental speeding in AMPA-EPSC decay time at the calyx of Held. J Neurosci 25: 199–207, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kombian SB, Hirasawa M, Mouginot D, Chen X, Pittman QJ. Short-term potentiation of miniature excitatory synaptic currents causes excitation of supraoptic neurons. J Neurophysiol 83: 2542–2553, 2000a [DOI] [PubMed] [Google Scholar]
- Kombian SB, Mouginot D, Hirasawa M, Pittman QJ. Vasopressin preferentially depresses excitatory over inhibitory synaptic transmission in the rat supraoptic nucleus in vitro. J Neuroendocrinol 12: 361–367, 2000b [DOI] [PubMed] [Google Scholar]
- Lambolez B, Ropert N, Perrais D, Rossier J, Hestrin S. Correlation between kinetics and RNA splicing of alpha-amino-3-hydroxy-5-methylisoxazole-4-propionic acid receptors in neocortical neurons. Proc Natl Acad Sci USA 93: 1797–1802, 1996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C, Tripathi PK, Armstrong WE. Differences in spike train variability in rat vasopressin and oxytocin neurons and their relationship to synaptic activity. J Physiol 581: 221–240, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li YF, Cornish KG, Patel KP. Alteration of NMDA NR1 receptors within the paraventricular nucleus of hypothalamus in rats with heart failure. Circ Res 93: 990–997, 2003 [DOI] [PubMed] [Google Scholar]
- Li YF, Jackson KL, Stern JE, Rabeler B, Patel KP. Interaction between glutamate and GABA systems in the integration of sympathetic outflow by the paraventricular nucleus of the hypothalamus. Am J Physiol Heart Circ Physiol 291: H2847–H2856, 2006 [DOI] [PubMed] [Google Scholar]
- Mainen ZF, Sejnowski TJ. Reliability of spike timing in neocortical neurons. Science 268: 1503–1506, 1995 [DOI] [PubMed] [Google Scholar]
- McKinley MJ, Bicknell RJ, Hards D, McAllen RM, Vivas L, Weisinger RS, Oldfield BJ. Efferent neural pathways of the lamina terminalis subserving osmoregulation. Prog Brain Res 91: 395–402, 1992 [DOI] [PubMed] [Google Scholar]
- Modi I, De Koninck Y, Otis TS, Soltesz I. Bridging the cleft at GABA synapses in the brain. Trends Neurosci 17: 517–525, 1994 [DOI] [PubMed] [Google Scholar]
- Mosbacher J, Schoepfer R, Monyer H, Burnashev N, Seeburg PH, Ruppersberg JP. A molecular determinant for submillisecond desensitization in glutamate receptors. Science 266: 1059–1062, 1994 [DOI] [PubMed] [Google Scholar]
- Nakamura Y, Haneda T, Osaki J, Miyata S, Kikuchi K. Hypertrophic growth of cultured neonatal rat heart cells mediated by vasopressin V1A receptor. Eur J Pharmacol 391: 39–48, 2000 [DOI] [PubMed] [Google Scholar]
- Nicod P, Waeber B, Bussien JP, Goy JJ, Turini G, Nussberger J, Hofbauer KG, Brunner HR. Acute hemodynamic effect of a vascular antagonist of vasopressin in patients with congestive heart failure. Am J Cardiol 55: 1043–1047, 1985 [DOI] [PubMed] [Google Scholar]
- Nissen R, Hu B, Renaud LP. Regulation of spontaneous phasic firing of rat supraoptic vasopressin neurones in vivo by glutamate receptors. J Physiol 484: 415–424, 1995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otis TS, Wu YC, Trussell LO. Delayed clearance of transmitter and the role of glutamate transporters at synapses with multiple release sites. J Neurosci 16: 1634–1644, 1996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otsu Y, Murphy TH. Miniature transmitter release: accident of nature or careful design? Sci STKE 2003: pe54, 2003 [DOI] [PubMed] [Google Scholar]
- Packer M, Lee WH, Kessler PD, Gottlieb SS, Bernstein JL, Kukin ML. Role of neurohormonal mechanisms in determining survival in patients with severe chronic heart failure. Circulation 75: IV80–IV92, 1987 [PubMed] [Google Scholar]
- Packer M. Neurohormonal interactions and adaptations in congestive heart failure. Circulation 77: 721–730, 1988 [DOI] [PubMed] [Google Scholar]
- Park JB, Skalska S, Stern JE. Characterization of a novel tonic gamma-aminobutyric acid(A) receptor-mediated inhibition in magnocellular neurosecretory neurons and its modulation by glia. Endocrinology 147: 3746–3760, 2006 [DOI] [PubMed] [Google Scholar]
- Patel KP, Zhang K, Kenney MJ, Weiss M, Mayhan WG. Neuronal expression of Fos protein in the hypothalamus of rats with heart failure. Brain Res 865: 27–34, 2000 [DOI] [PubMed] [Google Scholar]
- Patel KP, Zhang PL, Krukoff TL. Alterations in brain hexokinase activity associated with heart failure in rats. Am J Physiol Regul Integr Comp Physiol 265: R923–R928, 1993 [DOI] [PubMed] [Google Scholar]
- Patel KP, Zhang PL, Carmines PK. Neural influences on renal responses to acute volume expansion in rats with heart failure. Am J Physiol Heart Circ Physiol 271: H1441–H1448, 1996 [DOI] [PubMed] [Google Scholar]
- Popescu IR, Morton LA, Franco A, Di S, Ueta Y, Tasker JG. Synchronized bursts of miniature inhibitory postsynaptic currents. J Physiol 588: 939–951, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poulain DA, Wakerley JB. Electrophysiology of hypothalamic magnocellular neurones secreting oxytocin and vasopressin. Neuroscience 7: 773–808, 1982 [DOI] [PubMed] [Google Scholar]
- Randle J, Renaud L. Actions of gamma-aminobutyric acid in rat supraoptic nucleus neurosecretory neurons in vitro. J Physiol 387: 629–647, 1987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redman RS, Silinsky EM. On the simultaneous electrophysiological measurements of neurotransmitter release and perineural calcium currents from frog motor nerve endings. J Neurosci Methods 57: 151–159, 1995 [DOI] [PubMed] [Google Scholar]
- Riegger GA, Liebau G, Bauer E, Kochsiek K. Vasopressin and renin in high output heart failure of rats: hemodynamic effects of elevated plasma hormone levels. J Cardiovasc Pharmacol 7: 1–5, 1985 [DOI] [PubMed] [Google Scholar]
- Rodriguez-Molina VM, Aertsen A, Heck DH. Spike timing and reliability in cortical pyramidal neurons: effects of EPSC kinetics, input synchronization and background noise on spike timing. PLoS One 2: e319, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roland BL, Sawchenko PE. Local origins of some GABAergic projections to the paraventricular and supraoptic nuclei of the hypothalamus in the rat. J Comp Neurol 332: 123–143, 1993 [DOI] [PubMed] [Google Scholar]
- Rouleau JL, Packer M, Moye L, de Champlain J, Bichet D, Klein M, Rouleau JR, Sussex B, Arnold JM, Sestier F, Parker JO, McEwan P, Bernstein V, Cuddy E, Lamas GA, Gottlieb SS, McCans J, Nadeau C, Delage F, Wun CC, Pfeffer MA. Prognostic value of neurohumoral activation in patients with an acute myocardial infarction: effect of captopril. J Am Coll Cardiol 24: 583–591, 1994 [DOI] [PubMed] [Google Scholar]
- Schrier RW, Abraham WT. Hormones and hemodynamics in heart failure. N Engl J Med 341: 577–585, 1999 [DOI] [PubMed] [Google Scholar]
- Silverman AJ, Zimmerman EA. Magnocellular neurosecretory system. Annu Rev Neurosci 6: 357–380, 1983 [DOI] [PubMed] [Google Scholar]
- Sladek B, Morsette, Sidorowicz Role of non-NMDA receptors in osmotic and glutamate stimulation of vasopressin release: effect of rapid receptor desensitization. J Neuroendocrinol 10: 897–903, 1998 [DOI] [PubMed] [Google Scholar]
- Softky WR, Koch C. The highly irregular firing of cortical cells is inconsistent with temporal integration of random EPSPs. J Neurosci 13: 334–350, 1993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern JE. Electrophysiological and morphological properties of pre-autonomic neurones in the rat hypothalamic paraventricular nucleus. J Physiol 537: 161–177, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern JE, Galarreta M, Foehring RC, Hestrin S, Armstrong WE. Differences in the properties of ionotropic glutamate synaptic currents in oxytocin and vasopressin neuroendocrine neurons. J Neurosci 19: 3367–3375, 1999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szatalowicz VL, Arnold PE, Chaimovitz C, Bichet D, Berl T, Schrier RW. Radioimmunoassay of plasma arginine vasopressin in hyponatremic patients with congestive heart failure. N Engl J Med 305: 263–266, 1981 [DOI] [PubMed] [Google Scholar]
- Trussell LO, Zhang S, Raman IM. Desensitization of AMPA receptors upon multiquantal neurotransmitter release. Neuron 10: 1185–1196, 1993 [DOI] [PubMed] [Google Scholar]
- Vahid-Ansari F, Leenen FH. Pattern of neuronal activation in rats with CHF after myocardial infarction. Am J Physiol Heart Circ Physiol 275: H2140–H2146, 1998 [DOI] [PubMed] [Google Scholar]
- van den Pol AN, Wuarin JP, Dudek FE. Glutamate, the dominant excitatory transmitter in neuroendocrine regulation. Science 250: 1276–1278, 1990 [DOI] [PubMed] [Google Scholar]
- Verbalis JG, Mangione MP, Stricker EM. Oxytocin produces natriuresis in rats at physiological plasma concentrations. Endocrinology 128: 1317–1322, 1991 [DOI] [PubMed] [Google Scholar]
- Wall MJ, Robert A, Howe JR, Usowicz MM. The speeding of EPSC kinetics during maturation of a central synapse. Eur J Neurosci 15: 785–797, 2002 [DOI] [PubMed] [Google Scholar]
- Wang YX, Franco R, Gavras I, Gavras H. Effects of chronic administration of a vasopressin antagonist with combined antivasopressor and antiantidiuretic activities in rats with left ventricular dysfunction. J Lab Clin Med 117: 313–318, 1991 [PubMed] [Google Scholar]
- Yamada KA, Tang CM. Benzothiadiazides inhibit rapid glutamate receptor desensitization and enhance glutamatergic synaptic currents. J Neurosci 13: 3904–3915, 1993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang K, Li YF, Patel KP. Blunted nitric oxide-mediated inhibition of renal nerve discharge within PVN of rats with heart failure. Am J Physiol Heart Circ Physiol 281: H995–H1004, 2001 [DOI] [PubMed] [Google Scholar]
- Zhang K, Li YF, Patel KP. Reduced endogenous GABA-mediated inhibition in the PVN on renal nerve discharge in rats with heart failure. Am J Physiol Regul Integr Comp Physiol 282: R1006–R1015, 2002a [DOI] [PubMed] [Google Scholar]
- Zhang ZH, Francis J, Weiss RM, Felder RB. The renin-angiotensin-aldosterone system excites hypothalamic paraventricular nucleus neurons in heart failure. Am J Physiol Heart Circ Physiol 283: H423–H433, 2002b [DOI] [PubMed] [Google Scholar]
- Zheng H, Li YF, Cornish KG, Zucker IH, Patel KP. Exercise training improves endogenous nitric oxide mechanisms within the paraventricular nucleus in rats with heart failure. Am J Physiol Heart Circ Physiol 288: H2332–H2341, 2005 [DOI] [PubMed] [Google Scholar]