Abstract
Study Objectives:
To assess the effects of early and late bedtimes and wake up times on use of time and weight status in Australian school-aged children.
Design:
Observational cross-sectional study involving use of time interviews and pedometers.
Setting:
Free-living Australian adolescents.
Participants:
2200 9- to 16-year-olds from all states of Australia
Interventions:
NA.
Measurements and Results:
Bedtimes and wake times were adjusted for age and sex and classified as early or late using median splits. Adolescents were allocated into 4 sleep-wake pattern groups: Early-bed/Early-rise; Early-bed/Late-rise; Late-bed/Early-rise; Late-bed/Late-rise. The groups were compared for use of time (screen time, physical activity, and study-related time), sociodemographic characteristics, and weight status. Adolescents in the Late-bed/Late-rise category experienced 48 min/d more screen time and 27 min less moderate-to-vigorous physical activity (MVPA) (P < 0.0001) than adolescents in the Early-bed/Early-rise category, in spite of similar sleep durations. Late-bed/Late-rise adolescents had a higher BMI z-score (0.66 vs. 0.45, P = 0.0015). Late-bed/Late-rise adolescents were 1.47 times more likely to be overweight or obese than Early-bed/Early-rise adolescents, 2.16 times more likely to be obese, 1.77 times more likely to have low MVPA, and 2.92 times more likely to have high screen time. Late-bed/Late-rise adolescents were more likely to come from poorer households, to live in major cities, and have fewer siblings.
Conclusions:
Late bedtimes and late wake up times are associated with an unfavorable activity and weight status profile, independent of age, sex, household income, geographical remoteness, and sleep duration.
Citation:
Olds TS; Maher CA; Matricciani L. Sleep duration or bedtime? Exploring the relationship between sleep habits and weight status and activity patterns. SLEEP 2011;34(10):1299-1307.
Keywords: Child, screen time, physical activity, bedtime, wake up time
INTRODUCTION
Childhood overweight and obesity are undeniable concerns both globally and locally, and the identification of factors contributing to their etiology is an important part of developing successful strategies for future prevention and treatment. Sleep is among the factors that have been hypothesized to play a role, with a growing body of evidence to suggest that shorter sleep durations are associated with increased fatness.1–3
A number of mechanisms have been proposed to explain how short sleep duration may increase the risk of being overweight or obese. Several studies have found that rhythms in the levels of hormones cortisol, ghrelin, and leptin are altered by sleep restriction.4–8 In many cases,4–7 but not all,8 these hormonal changes have been accompanied by decreased energy expenditure and/or increased energy intake by increasing appetite, thereby causing weight gain. Sleep restriction has also been linked with altered food preferences (specifically, increased snack consumption, particularly snacks with high carbohydrate content) in an absence of hormonal changes.9 While experimental studies are limited for children, cross-sectional studies indicate children with short sleep tend to be less physically active10 and consume greater quantities of high-calorie foods and beverages.11–13 These findings lend support to the hypothesis that short sleep may facilitate weight gain by altering energy expenditure and intake.
The link between short sleep duration and childhood overweight or obesity has been shown by several studies.3,14–16 In a meta-analysis of 30,002 children from 11 different countries and 19 separate studies, Cappuccio and colleagues demonstrated that cross-sectional studies have consistently shown children with short sleep to be at increased risk of obesity.2 Similar findings have also been identified in longitudinal studies. Reilly and colleagues17 found 3-year-old British children with short sleep durations were 45% more likely to be obese at age 7, while US children with short sleep in third grade were more likely to be overweight in sixth grade.18 Similarly, a longitudinal study of 2,281 US children aged 3-12 years at baseline found that those who slept less had higher BMIs and were more likely to be overweight 5 years later.19 In light of such findings, it has been suggested that increasing children's sleep duration may be an effective strategy for preventing and/or treating obesity.20
However, the link between sleep duration and weight status has also been questioned. In reviewing the available evidence, Horne argues that the association between short sleep duration and childhood obesity is weaker than commonly believed.21,22 One recent study of 13,568 US adolescents has also found no significant longitudinal association between sleep duration and obesity, once data were adjusted for confounding factors.23 There was, however, an association between obesity and depression and excessive television watching.23
Although studies examining the relationship between children's sleep patterns and weight status tend to focus on sleep duration, it has recently been suggested that sleep timing behavior may be a better predictor of obesity than sleep duration alone.12 Limited research has been conducted in this area. Some indication may be drawn from sleep “chronotype” literature, which examines sleep pattern preference (i.e., “morning-type individuals,” who prefer to wake up early in the morning and are most alert during the early part of the day, versus “evening-type” individuals, who prefer to go to bed late in the evening and are most alert in the late evening hours).24 Note that sleep pattern preference is distinct from sleep pattern behavior, since behavior is influenced by preference in addition to external factors, such as parental regulation and the need to rise to attend school. Chronotype studies25,26 have shown that morning-type children tend to have a lower BMI than evening-type children. It is plausible that this may be due to differing opportunities for physical activity and sedentary behaviors in these time slots, with the evening offering relatively few opportunities for physical activity and relatively more opportunities for sedentary behaviors, such as television viewing, which has been shown to be associated with increased snacking behavior27 and exposure to advertisements for energy-dense foods28–30 in young people.
Dietary differences on the basis of sleep chronotype have also been identified; in general, morning-type individuals have been found to consume fewer fast foods and caffeinated drinks12 and have less disposition to eating disorders such as overeating26 compared to evening-type people. Caffeine consumption can lead to increased alertness31 and sleep disruption.11 It is unclear whether the relationship between unfavorable sleep behavior patterns and caffeinated drink consumption exists due to the caffeine disturbing sleep or because caffeine is consumed to counteract the daytime effect of interrupted sleep.11
It is difficult to disentangle the independent effects of bedtime and sleep duration, as shorter sleep duration can frequently be linked to a delay in bedtime,32,33 and the relationship between sleep pattern behavior and children's weight status has been largely unexplored to date. It is plausible that delayed bedtime may be linked to different use of time patterns, such as increased television time. This in turn may have a flow-on impact on weight status, given that time watching television has been linked to increased energy intake, as already described. Indeed, this theory may help explain why the recent study by Calamaro did not find an association between sleep duration and BMI, but did find an association between excessive television viewing and BMI.34 Early rise times may also impact weight status through different use of time patterns. Children who wake up early in the morning may, for example, may be more physically active as a result of needing to wake early to walk or ride to school. These examples may also explain why previous studies have found morning-type children to have a lower BMI compared to evening-type children.
As already described, some studies have examined possible relationships between sleep timing behavior (by the way of chronotype) and weight status through dietary patterns, however there do not appear to be any studies exploring possible links between sleep timing behavior and weight status through physical activity.
A methodological consideration for examining the relationship between sleep timing behavior and other variables is the classification of sleep timing itself. A limitation of classifying sleep timing behavior in the context of sleep chronoypes is that individuals are grouped at the extreme ends of the chronotype continuum, whereas most individuals lie within these extremes.35 Classification on the basis of chronotypes assumes that morning type people go to bed early and rise early, and that evening-type people both go to bed late and rise late, whereas it is quite possible that these behaviors many not necessarily be coupled (i.e., someone may go to bed late and rise early). Therefore, it may be useful to classify individuals into one of the four sleep timing behavior categories: Early to bed early to rise (Early-bed/Early-rise), early to bed late to rise (Early-bed/Late-rise), late to bed late to rise (Late-bed/Late-rise), and late to bed early to rise (Late-bed/Early-rise), as done in 2 previous studies.36,37
The purpose of this study was therefore 2-fold: first, to determine whether sleep timing behavior, as classified in the preceding paragraph, and sleep duration were related to weight status, and second, to determine whether sleep timing behavior was related to physical activity and sedentary behaviors (operationalized as screen time, i.e., time spent watching televisions, playing video games, and using computers), in a nationally representative sample of 9- to 16-year-olds.
METHODS
Subjects
Subjects were 2200 randomly selected Australians aged between 9 and 16 years, who took part in the 2007 Australian National Children's Nutrition and Physical Activity Survey. Clusters of postal code areas were randomly selected throughout Australia, with the exception of very remote areas. Random-digit dialing was used to contact households within each postcode cluster, and eligible households (those which had a child aged between 2 and 16 years) were invited to participate. Only one child was surveyed from each household to prevent clustering and therefore bias in the data. In those families where more than one child met the inclusion criteria, the child with the birthday closest to the date of initial contact was used to randomly choose which eligible child would be involved.
The response rate (ratio of households providing complete data to eligible households contacted) was 41%. While data could not be gathered on the characteristics of non-responders, participants appeared to be representative of the Australian population of young people on the basis of geographic location (except for 3% of Australia's population classified as very remote, who were excluded for feasibility reasons),38 weight status,39 and socioeconomic status (based upon the Australian Bureau of Statistics Socioeconomic indicators for areas index, SEIFA).40 Families for whom English was a second language were included, with interpreters present during interviews.
The ensuing analyses are based upon participants aged 9 years and older, since they provided detailed use of time data, whereas younger participants in the Australian National Children's Nutrition and Physical Activity Survey did not provide these data.
Outcome Measures and Procedure
Computer-assisted, face-to-face interviews were conducted in participants' homes by trained research assistants. Demographic data, including reported annual household income, place of residence, family structure, sex, and age of the target child were gathered (see Table 1).
Table 1.
Subject characteristics
| EE | EL | LE | LL | All | P-value | |
|---|---|---|---|---|---|---|
| n = 719 | n = 453 | n = 378 | n = 650 | n = 2200 | ||
| Boys | 356 | 221 | 182 | 327 | 1086 | |
| Girls | 363 | 232 | 196 | 323 | 1114 | |
| Age (years) | 13.4 (2.2) | 13.5 (2.2) | 13.2 (2.3) | 13.6 (2.2) | 13.4 (2.2) | 0.21 |
| BMI (kg/m2) | 20.4 (4.0) | 20.5 (3.8) | 20.8 (4.0) | 21.2 (4.3) | 20.7 (4.1) | 0.002 |
| % Obese | 4.6 | 5.7 | 7.1 | 8.8 | 6.5 | 0.001 |
| % Overweight (not including obese) | 16.8 | 19.2 | 22.0 | 19.7 | 19.0 | 0.01 |
| SEIFA | 1002 (59) | 1004 (67) | 1003 (62) | 999 (71) | 1002 (65) | 0.58 |
| Household income (%) | ||||||
| > AUD104,000 | 30.0 | 27.9 | 32.4 | 29.2 | 29.7 | |
| AUD75,000-104,000 | 21.7 | 16.4 | 17.2 | 20.1 | 19.4 | |
| AUD52,000-75,000 | 20.7 | 21.5 | 25.9 | 18.3 | 21.1 | |
| < AUD52,000 | 27.6 | 34.2 | 24.5 | 32.3 | 29.8 | 0.01 |
| Remoteness (%) | ||||||
| Major city | 47.7 | 58.3 | 56.9 | 61.5 | 55.5 | |
| Inner regional | 26.3 | 20.5 | 18.5 | 18.9 | 21.6 | |
| Outer regional | 20.2 | 16.1 | 19.6 | 15.5 | 17.9 | |
| Remote | 5.8 | 5.1 | 5.0 | 4.0 | 5.0 | 0.0002 |
| Number of children in home | 2.2 | 2.1 | 2.1 | 2.1 | 2.1 | 0.006 |
| Young person in part-time work (min/d) | 8.0 | 6.0 | 14.0 | 10.0 | 9.2 | 0.003 |
Values are shown as percentages or means (SDs).
EE, Early-bed/Early-rise; EL, Early-bed/Late-rise; LE, Late-bed/Early-rise; LL, Late-bed/Late-rise; BMI, body mass index; SEIFA, Socioeconomic indicators for areas. SEIFA is a series of indices of socioeconomic status devised by the Australian Bureau of Statistics using a range of indicators such as educational and employment status.
The index used here is the Index of Relative Disadvantage, calculated at the postal area level. The national average is 1000 and the SD is 100. Higher values indicate more advantaged areas.
Height, body mass, and waist girth were measured according to the protocols of the International Society for the Advancement of Kinanthropometry,41 and body mass index (BMI) was calculated.
Use of time data were collected using the Multimedia Activity Recall for Children and Adults (MARCA).42 This software allowed young people to recall everything they did on the previous day from wake-up to bedtime, in time-slices as fine as 5 minutes, using a segmented day format. Young people chose from a list of 250 activities grouped under 7 rubrics (Inactivity, Transport, Sport and Play, School, Self-Care, Chores and Other). The MARCA has a same-day test-retest reliability of r = 0.84-0.92 for major outcome variables (moderate to vigorous physical activity [MVPA], physical activity level [PAL] and screen time). The criterion validity of the MARCA has been assessed with reference to accelerometry42 and pedometry,43 and the Spearman rho for PAL was 0.45 and 0.54, respectively.
The MARCA was administered on 2 occasions—once during the face-to-face interview in participants' homes, and once in a follow-up phone call 1-3 weeks later. Each time, young people recalled their activities over the 2 previous days (a total of 4 days were sampled). Wherever possible, at least one school day and one non-school day were sampled. For the total sample, 14% of sampled days were Mondays, 15% were Tuesdays, 14% Wednesdays, 15% Thursdays, 15% Fridays, 14% Saturdays, and 14% Sundays. Taking into account weekends and holidays, 48% of sampled days were school days and 52% were non-school days.
Objective physical activity was recorded using NL-1000 pedometer for 7 days, and the number of daily steps was averaged. The days on which the pedometer was worn usually, but not always, included at least one of the days recalled using the MARCA.
Statistical Analyses
Bedtime and wake up time were extracted from the MARCA recalls. Bedtime was defined as the time the young person “turned out the light and went to sleep” (distinct from other activities performed while lying down, which are recorded by the MARCA, such as “listening to music while lying,” “reading while lying,” “lying awake,” or “watching television while lying”). Wake time was defined as the time the young person reported they woke up (distinct from the time that they actually got out of bed). Sleep duration was the amount of time reported sleeping in each 24-h period (including intra-day naps).
Moderate to vigorous physical activity (MVPA) was calculated as the number of minutes spent in activities expected to elicit ≥ 3 METs (METs are units of rates of energy expenditure, which are multiples of basal metabolic rate) as listed in the MARCA compendium,44 and vigorous physical activity (VPA) as the time spent in activities requiring ≥ 6 METs. The number of minutes spent in key MVPA subsets was also calculated (sport, free play and active transport (i.e., the use of physical activities such as walking and cycling to get somewhere), as defined by lists of MARCA codes published elsewhere.43,45 Compliance with Australian government recommendations regarding physical activity (≥ 60 min/d of MVPA)46 was assessed by averaging MVPA over the 4 days. Non-sleep physical activity level (non-sleep PAL) was defined as the average rate of energy expenditure during waking hours, calculated by the factorial method, that is, by multiplying the number of minutes spent in waking activities by the estimated energy expenditure for each activity, summing the products and dividing by the total number of waking minutes.
Screen time was the number of minutes the young people reported watching television, playing videogames, or using a computer. Compliance with Australian government recommendations regarding screen time (< 120 min/d)46 was assessed by averaging screen time over the 4 days. Non-screen sedentary time (NSST) was calculated as the number of minutes the young person reported being involved in activities when seated or lying down expected to elicit < 3 METs, with the exception of sleep. Total sedentary time was calculated as the sum of screen time and NSST.
Values for bedtime, wake-up time, and all use of time variables were adjusted for age and sex by regressing them against decimal age and fitting a fourth-order polynomial. This was done separately for boys and girls, and the residuals were used in analysis. These values represented the degree to which an individual young person deviated from the expected value for young people of the same age and sex. Since Australian children spend about 1 day in 2 at school (taking into account weekends, holidays, and student-free days), all use of time variables were calculated as the average of school day and non-school day values.
Participants were classified into one of 4 categories, using median splits for age- and sex-adjusted bedtimes and wake-up times: Early-bed/Early-rise; Early-bed/Late-rise; Late-bed/Early-rise; and Late-bed/Late-rise.
Reported household income was stratified into 4 bands: > AUD104,000; AUD75,000-104,000; AUD52,000-75,000; and < AUD52,000. Remoteness of residence was stratified into 4 bands using the Accessibility/Remoteness Index for Australia (ARIA+) method38: major city, inner regional, outer regional, and remote. Weight status category (normal weight, overweight, or obese) was calculated using the criteria of Cole et al.,47 and BMI scores were also expressed as z-scores using the UK 1990 reference.48
Differences in mean values for continuous dependent variables (physical activity and components, sedentary behaviors and components, BMI z-score) were tested using factorial ANOVA with sleep-wake patterns (Early-bed/Early-rise, Early-bed/Late-rise, Late-bed/Early-rise, and Late-bed/Late-rise) as the grouping factor. Chi-squared tests were used to test for differences in categorical dependent variables (weight status category, compliance with physical activity and screen guidelines, household income, and remoteness).
Multivariate logistic regressions were conducted to assess the relationships between sleep-wake patterns and weight status, screen time and MVPA (compliance with Australian guidelines). Age, sex, household income, remoteness, and sleep duration were entered as covariates (and weight status when screen time and MVPA were the dependent variables).
Multivariate logistic regressions were also used to identify sociodemographic characteristics of young people in the Late-bed/Late-rise group (participation of the young person in part-time work, family composition [i.e., number of siblings], remoteness of residence category, and household income category).
Alpha was set at 0.05. No corrections were made for multiple comparisons, but exact P-values have been reported. Readers are encouraged to focus on patterns of differences.
RESULTS
Sleep Patterns
One-third of all participants fell into the Early-bed/Early-rise group, compared to 21% in the Early-bed/Late-rise, 17% in the Late-bed/Early-rise, and 30% in the Late-bed/Late-rise groups. As planned, there were significant differences in bedtime, wake up time and sleep duration (Table 2). The Early-bed/Early-rise and Late-bed/Early-rise groups woke 60-80 minutes earlier than the Early-bed/Late-rise and Late-bed/Late-rise groups, while the Early-bed/Early-rise and Early-bed/Late-rise groups went to bed 70-90 minutes earlier than the Late-bed/Early-rise and Late-bed/Late-rise groups. There were statistically significant differences in sleep duration across all 4 groups; however, the difference between the Early-bed/Early-rise group (averaging 9h 43 sleep over a 24-h period) and the Late-bed/Late-rise group (9h 36) was quantitatively small. The Early-bed/Late-rise group slept about 1 h longer (10h 41), while the Late-bed/Early-rise group slept more than an hour less (8h 29).
Table 2.
Comparison of bedtimes, wake up times and sleep durations across four groups of adolescents
| Characteristic | EE | EL | LE | LL | P-value |
|---|---|---|---|---|---|
| n = 719 | n = 453 | n = 378 | n = 650 | ||
| Bedtime | 9:20PMab | 9:28 PMcd | 10:40 PMac | 10:46PMbd | < 0.0001 |
| ± 29 min | ± 25 min | ± 28 min | ± 38 min | ||
| Wake up time | 7:03 AMab | 8:09 AMac | 7:09 AMcd | 8:22 AMbd | < 0.0001 |
| ± 30 min | ± 26 min | ± 30 min | ± 34 min | ||
| Sleep (min/d) | 9h43a | 10h41a | 8h39a | 9h36a | < 0.0001 |
| ± 44 min | ± 45 min | ± 45 min | ± 54 min |
Values with the same superscript in the same row are significantly different. For example, adolescents from the Early-bed/Early-rise group have significantly different bedtimes from adolescents in the Late-bed/Early-rise and Late-bed/Late-rise groups.
EE, Early-bed/Early-rise; EL, Early-bed/Late-rise; LE, Late-bed/Early-rise; LL, Late-bed/Late-rise. ±, SD.
Physical Activity
There were significant differences in the amount of physical activity performed by young people from the different groups (Table 3). In general, early risers, particularly in the Early-bed/Early-rise group, were more physically active. Participants in the Early-bed/Early-rise group had non-sleep PALs 7% higher than LL participants (P < 0.0001). They accumulated 27 min more MVPA, 12 minutes more VPA, 16 min more free play, 10 min more sport, and 5 min more active transport, and took 927 more steps than Late-bed/Late-rise participants, in spite of being awake only 7 min more each day. While 83% of Early-bed/Early-rise participants met the MVPA guidelines of ≥ 60 min/day, 75% of Late-bed/Late-rise participants met the guidelines.
Table 3.
Comparison of physical activity across four groups of adolescents
| Characteristic | EE | EL | LE | LL | P-value |
|---|---|---|---|---|---|
| n = 719 | n = 453 | n = 378 | n = 650 | ||
| Non-sleep PAL (METs*) | 2.23a | 2.19b | 2.18c | 2.08abc | < 0.0001 |
| MVPA (min/d) | 133ab | 118acd | 132cde | 106be | < 0.0001 |
| VPA (min/d) | 53ab | 47ac | 51d | 41bcd | < 0.0001 |
| Meeting MVPA guidelines (%) | 83 | 79 | 81 | 75 | 0.0005 |
| Sport (min/d) | 48a | 44b | 45c | 38abc | 0.0003 |
| Play (min/d) | 77ab | 66a | 71c | 61bc | < 0.0001 |
| Active transport (min/d) | 46ab | 41ac | 47cd | 41bd | 0.012 |
| Daily pedometer steps | 11,395ab | 10,821a | 11,090c | 10,468bc | < 0.0001 |
Values with the same superscript in the same row are significantly different.
EE, Early-bed/Early-rise; EL, Early-bed/Late-rise; LE, Late-bed/Early-rise; LL, Late-bed/Late-rise; PAL, Physical Activity Level; MVPA, moderate-to-vigorous physical activity; VPA, vigorous physical activity.
METs are units of rates of energy expenditure, which are multiples of basal metabolic rate.
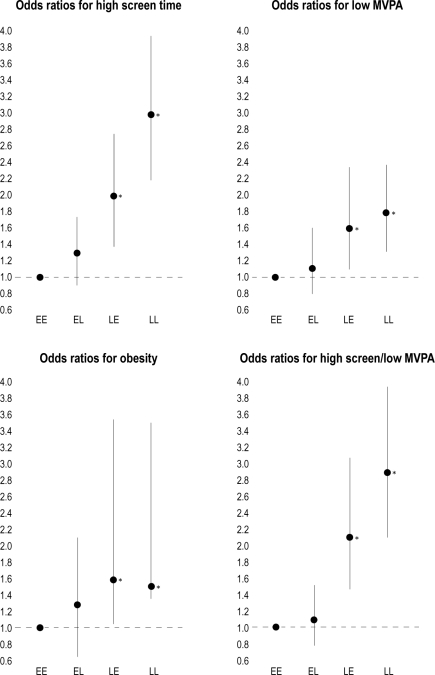
Adjusted for age, sex, household income, remoteness, sleep duration, and weight status, the odds ratios for low MVPA (i.e., < 60 min/day on average) were 1.00 for Early-bed/Early-rise (reference category), 1.12 (95% CI 0.79-1.60) for Early-bed/Late-rise, 1.58 (1.07-2.34, P = 0.02) for Late-bed/Early-rise, and 1.77 (1.31-2.38, P = 0.002) for Late-bed/Late-rise (Figure 1). These patterns were broadly similar when the sample was analyzed by age and sex subsets.
Figure 1.
Odds ratios (and 95% confidence intervals) for high screen time, low MVPA, obesity, and high screen and low MVPA by sleep-wake group. Odds ratios have been adjusted for age, sex, household income, remoteness, sleep duration, and (except for obesity) weight status. *P < 0.05; EE, Early-bed/Early-rise; EL, Early-bed/Late-rise; LE, Late-bed/Early-rise; LL, Late-bed/Late-rise.
Sedentary Behaviors
There were also significant differences in the time devoted to sedentary behaviors by participants from the different groups (Table 4). In general, those with a late bedtime, particularly in the Late-bed/Late-rise group, accumulated more screen time. Participants in the Late-bed/Late-rise group experienced 48 min more screen time than the Early-bed/Early-rise group, of which 19 min was TV viewing, and 16 min was passive videogame playing (i.e., videogames which use a traditional controller and involve little physical activity), and 11 min computer use. These patterns were broadly similar when the data were analyzed by age and sex subsets. Only 12% of Late-bed/Late-rise participants met the screen guidelines of < 120 min/day, compared to 28% of the Early-bed/Early-rise group. There were no differences in study time (P = 0.45) or reading (P = 0.84). On the other hand, Late-bed/Late-rise participants accumulated 22 fewer min of non-screen sedentary time than Early-bed/Early-rise participants. In spite of this, the Late-bed/Late-rise group experienced 25 more min of sedentary time in toto. All of these differences persisted when adjusted for household income, and the same gradients were seen within each household income band.
Table 4.
Comparison of sedentary behaviors across four groups of adolescents
| Characteristic | EE | EL | LE | LL | P-value |
|---|---|---|---|---|---|
| n = 719 | n = 453 | n = 378 | n = 650 | ||
| Total sedentary time (min/d) | 564a | 541a | 613a | 589a | < 0.0001 |
| Non-screen sedentary time (min/d) | 353abc | 329ad | 372bde | 334ce | < 0.0001 |
| Screen time (min/d) | 210ab | 213cd | 241ace | 258bde | < 0.0001 |
| Meeting screen guidelines (%) | 28 | 24 | 20 | 12 | < 0.0001 |
| TV (min/d) | 148a | 150b | 155c | 167abc | 0.0004 |
| Videogames (min/d) | 31ab | 30cd | 44ac | 47bd | < 0.0001 |
| Computer (min/d) | 30ab | 31cd | 44ac | 41bd | < 0.0001 |
| Study and homework (min/d) | 19 | 18 | 19 | 17 | 0.45 |
| Reading (min/d) | 24 | 23 | 24 | 22 | 0.84 |
| Meeting both screen and MVPA guidelines (%) | 25 | 21 | 16 | 10 | < 0.0001 |
Values with the same superscript in the same row are significantly different.
EE, Early-bed/Early-rise; EL, Early-bed/Late-rise; LE, Late-bed/Early-rise; LL, Late-bed/Late-rise.
When adjusted for age, sex, household income, remoteness, sleep duration, and weight status, the odds ratios for high screen time (i.e., > 120 min/day on average) were 1.00 for Early-bed/Early-rise (reference category), 1.28 (0.93-1.76) for Early-bed/Late-rise, 1.94 (1.36-2.77, P = 0.0003) for Late-bed/Early-rise, and 2.92 (2.16-3.94, P < 0.0001) for Late-bed/Late-rise. The odds ratios for both high screen time and low MVPA were 1.00 for Early-bed/Early-rise (reference category), 1.09 (0.78-1.52) for Early-bed/Late-rise, 2.10 (1.44-3.06, P < 0.0001) for Late-bed/Early-rise, and 2.87 (2.08-3.95, P < 0.0001) for Late-bed/Late-rise (Figure 1).
Weight Status
BMI z-score was higher in those with late bedtimes (P = 0.0015; Early-bed/Early-rise and Early-bed/Late-rise = 0.45; Late-bed/Early-rise = 0.63; Late-bed/Late-rise = 0.65), and again, this pattern was consistent when the data were analyzed by age and sex subsets (data not presented here). Those with late bedtimes were also more likely to be overweight or obese (P = 0.007; 29% in Late-bed/Early-rise and Late-bed/Late-rise vs. 21% in Early-bed/Early-rise and 25% in Early-bed/Late-rise; Table 5).
Table 5.
Comparison of weight status across four groups of adolescents
| Characteristic | EE | EL | LE | LL | P-value |
|---|---|---|---|---|---|
| n = 719 | n = 453 | n = 378 | n = 650 | ||
| BMI z-score | 0.45ab | 0.45cd | 0.63ac | 0.66bd | 0.0015 |
| % overweight or obese | 21 | 25 | 29 | 29 | 0.007 |
Values with the same superscript in the same row are significantly different.
EE, Early-bed/Early-rise; EL, Early-bed/Late-rise; LE, Late-bed/Early-rise; LL, Late-bed/Late-rise.
Adjusted for age, sex, household income, remoteness, and sleep duration, the odds ratios for overweight or obesity were 1.00 for Early-bed/Early-rise (reference category), 1.25 (0.92-1.69, P = 0.16) for Early-bed/Late-rise, 1.55 (1.12-2.14, P = 0.008) for Late-bed/Early-rise, and 1.47 (1.14-1.90, P = 0.003) for Late-bed/Late-rise. Adjusted for age, sex, household income, remoteness, and sleep duration, the odds ratios for obesity were 1.00 for Early-bed/Early-rise (reference category), 1.18 (0.65-2.12, P = 0.59) for Early-bed/Late-rise, 1.89 (1.02-3.48, P = 0.04) for Late-bed/Early-rise, and 2.16 (1.35-3.46, P = 0.001) for Late-bed/Late-rise (Figure 1).
Sociodemographic Characteristics
The sociodemographic characteristics of young people in the various sleep timing behavior groups differed (Table 1). Post hoc analyses revealed that, in particular, participants from the Late-bed/Late-rise group were likely to have fewer siblings (P = 0.006; 2.09 vs. 2.24 for the Early-bed/Early-rise group), to live in major cities (P = 0.0002; 62% vs. 48% for the Early-bed/Early-rise group), to come from the lowest household income band (P = 0.013; 32% vs. 28% for the Early-bed/Early-rise group), and to participate in part-time work compared with the Early-bed/Early-rise group (P = 0.003).
DISCUSSION
Main Findings
There were large and significant differences in time use according to sleeping pattern group. Young people in the Late-bed/Late-rise group were 1.5 times more likely to be obese than the Early-bed/Early-rise group, 1.8 times more likely to be insufficiently active, and 2.9 times more likely to have excessive screen time. Broadly speaking, each day the Late-bed/Late-rise group replaced about 30 minutes of MVPA with 30 minutes of sedentary behavior relative to the Early-bed/Early-rise group. These differences are in spite of the Early-bed/Early-rise and Late-bed/Late-rise groups having approximately the same sleep durations.
Much previous research has emphasized the relationship between short sleep duration and unfavorable weight status.16,19,32,49 On the basis of such research, one may have expected the greatest differences in the current study to be observed between the Early-bed/Late-rise and the Late-bed/Early-rise groups (which on average, differed in mean sleep duration by > 2 h; 641 min for the Early-bed/Late-rise group vs. 509 min for the Late-bed/Early-rise group). On the contrary, the greatest differences by and large were found between the Early-bed/Early-rise and Late-bed/Late-rise groups, which had reasonably similar sleep durations (583 min vs. 576 min, respectively, a difference of only 7 min, which is likely to be of minimal clinical significance, despite achieving statistical significance). Furthermore, adjusted results confirmed that sleep pattern type had important relationships with weight status and activity patterns independent of sleep duration.
Strengths and Weaknesses
Before considering the implications of these findings, the study's strengths and limitations must be acknowledged. This study used a large, randomly chosen national sample of young Australian, and a validated, high-resolution use of time instrument with strong test-retest reliability. While the use of a 24-h recall instrument in this study minimized the risk of under- or over-reporting,50 self-report is subject to the vagaries of memory, particularly in younger adolescents, and social desirability bias.51 In addition, young people's behaviors are extremely variable, and the use of a 4-day sample may not precisely capture typical individual behaviors. While this will increase variability and introduce statistical noise, it will not bias parameter estimates.
While analyses were adjusted to account for age, the study that it did not measure pubertal stage, which has recognized associations with sleep patterns.52
Implications
While it is clear that the Early-bed/Early-rise sleep pattern is associated with a more favorable use of time profile, the direction of the relationship, and possible pathways of causation, can only be hypothesized from this cross-sectional study. One possibility is that adolescents may voluntarily adjust their sleep-waking patterns to accommodate their personal activity interests. For example, young people who are attracted to physical activity may choose to get up early to maximize their participation, for example, by taking part in early morning training sessions, riding or walking to school, or spending more time before school in active play. Similarly, young people who prefer screen time may choose to stay up late to watch favorite shows on television. In this way, young people may be adjusting their time budgets to match the rhythms of the world around them.
Alternatively, it is possible that individuals have an inherent disposition towards a particular sleep-waking pattern (psychological and/or genetic in basis), and thence when they are awake, they participate in what the world has to offer at that time. Considerable evidence supports the existence of a circadian clock regulating sleep and other physiological processes.53 Young people who are “naturally” morning-type people will experience a larger portion of discretionary time in the mornings—a time that may be conducive to physical activity due to daylight and safety issues. In contrast, young people who are “naturally” night-type people will experience a larger portion of their discretionary time in the late evening—a time slot when physical activity options are somewhat restricted, and relatively more sedentary and screen-based activities are on offer (with prime-time television programming and greater opportunities for computer-based social networking). We re-examined the use of time data to see whether young people in the different sleep timing behavior groups differed in their physical and sedentary activity patterns during the early morning and late evening time slots. These analyses (not shown) revealed that the young people who went to bed late did indeed accrue more screen time in the 7 pm to midnight time slot (22-53 min more, P < 0.0001), and that this difference entirely accounted for differences in total daily screen time between sleep timing behavior groups. Similarly, young people who woke early experienced more MVPA between 05:00 and 10:00 (8-12 min more, P < 0.0001), and this difference partly, but not entirely, accounted for differences in total daily MVPA time between groups (i.e., young people who work up early accrued more MVPA during the day in addition to accruing more MVPA in the morning time slot).
It is also important to consider that some external factors may oblige or encourage young people to have a particular sleep-wake pattern, with resultant impacts on the types of activities they can participate in. These external factors may relate to the culture of the home, such as the parental activity patterns (for example, parents who need to leave early for work, or who get home late), siblings' activity and sleep-wake patterns, and household rules around bedtime. It is possible that homes which have more rules and greater parental control and discipline may encourage early bedtimes and early rising times.54 Late bedtimes may be an indicator of poor parental control, which is also associated with increased weight.55 Some young people are likely to be involved in sporting activities which oblige them to rise early to attend training session scheduled before school. External factors may also include environmental noise or light-dark cycles. In this study, young people with a Late-bed/Late-rise sleep-wake pattern were more likely to reside in metropolitan areas. It is possible that the noise and bustle of a big city keeps them awake later.56 A young person who is kept awake at night by traffic noise, for example, is more likely to play videogames or watch TV than to go for a run or ride.
It is somewhat concerning that the sleep-wake pattern identified in this study as being associated with the most favorable activity and weight-status outcomes (the Early-bed/Early-rise sleep-wake pattern) is the opposite of the age-related trend towards later bedtimes and later wake times57 that is characteristically observed during adolescence. In recent years, there has been a suggestion that cultural changes should be made to better fit daily demands to adolescents' natural sleep/wake preferences (such as later school start times)58; however, results from this study suggest that this may lead to unfavorable changes in other activities (such as physical activity and screen time) which would have flow-on consequences for the health of young people.
Certainly, longitudinal research is needed to confirm the direction of associations between bed and wake time habits and time use and weight status, in addition to other outcomes of importance for young people (such as psychological health and academic performance). Results from this study indicate that the importance of bed time, as opposed to sleep duration, may have been relatively overlooked to date. Results suggest that health professionals working with young people on issues pertaining to sleep behavior should consider bedtime and wake time in addition to total sleep duration.
Furthermore, there is growing interest in intervention studies to educate children about sleep, with a view to it impacting on their sleep behavior and related variables.59,60 Findings from the current study suggest that bedtime would be an important variable to target in such studies. Intervention studies which manipulate bedtime would provide vital information on causal mechanisms and may lead to beneficial changes in use of time and weight status.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
Data in the study was drawn from the 2007 Australian National Children's Nutrition and Physical Activity Survey – a major survey commission by the Australian Commonwealth Department of Health and Ageing and the Department of Agriculture, Fisheries and Forestry ($2 million). An industry body also contributed financially to the study: the Australian Food and Grocery Council ($1 million). The industry sponsor had no role in the preparation of this manuscript; the study authors undertook all analyses and wrote this manuscript.
REFERENCES
- 1.Marshall N, Glozier N, Grunstein R. Is sleep duration related to obesity? A critical review of the epidemiological evidence. Sleep Med Rev. 2008;12:289–98. doi: 10.1016/j.smrv.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 2.Cappuccio F, Taggart F, Kandala N, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31:619–26. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel S, Hu F. Short sleep duration and weight gain: a systematic review. Obesity. 2008;16:643–53. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spiegel K, Tasali E, Penev P, Van Cauter E. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141:846–50. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- 5.Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354:1435–9. doi: 10.1016/S0140-6736(99)01376-8. [DOI] [PubMed] [Google Scholar]
- 6.Spiegel K, Leproult R, L'hermite-Balériaux M, Copinschi G, Penev P, Van Cauter E. Leptin levels are dependent on sleep duration: relationships with sympathovagal balance, carbohydrate regulation, cortisol, and thyrotropin. J Clin Endocrinol Metab. 2004;89:5762–71. doi: 10.1210/jc.2004-1003. [DOI] [PubMed] [Google Scholar]
- 7.Schmid SM, Hallschmid M, Jauch-Chara K, Born J, Schultes B. A single night of sleep deprivation increases ghrelin levels and feelings of hunger in normal-weight healthy men. J Sleep Res. 2008;17:331–4. doi: 10.1111/j.1365-2869.2008.00662.x. [DOI] [PubMed] [Google Scholar]
- 8.Omisade A, Buxton OM, Rusak B. Impact of acute sleep restriction on cortisol and leptin levels in young women. Physiol Behav. 2010;99:651–6. doi: 10.1016/j.physbeh.2010.01.028. [DOI] [PubMed] [Google Scholar]
- 9.Nedeltcheva AV, Kilkus JM, Imperial J, Kasza K, Schoeller DA, Penev PD. Sleep curtailment is accompanied by increased intake of calories from snacks. Am J Clin Nutr. 2009;89:126–33. doi: 10.3945/ajcn.2008.26574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1:e62. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pollak C, Bright D. Caffeine consumption and weekly sleep patterns in US seventh-, eighth-, and ninth-graders. Pediatrics. 2003;111:42–57. doi: 10.1542/peds.111.1.42. [DOI] [PubMed] [Google Scholar]
- 12.Fleig D, Randler C. Association between chronotype and diet in adolescents based on food logs. Eat Behav. 2009;10:115–8. doi: 10.1016/j.eatbeh.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 13.Patel S, Malhotra A, Gottlieb D, White D, Hu F. Correlates of long sleep duration. Sleep. 2006;29:881–9. doi: 10.1093/sleep/29.7.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eisenmann J, Ekkekakis P, Holmes M. Sleep duration and overweight among Australian children and adolescents Acta Paediatr. 2006;95:956–63. doi: 10.1080/08035250600731965. [DOI] [PubMed] [Google Scholar]
- 15.Knutson KL. Sex differences in the association between sleep and body mass index in adolescents. J Pediatr. 2005;147:830–4. doi: 10.1016/j.jpeds.2005.07.019. [DOI] [PubMed] [Google Scholar]
- 16.Olds T, Blunden S, Dollman J, Maher C. Day type and the relationship between weight status and sleep duration in children and adolescents. Aust N Z J Public Health. 2010;34:165–71. doi: 10.1111/j.1753-6405.2010.00502.x. [DOI] [PubMed] [Google Scholar]
- 17.Reilly J, Armstrong J, Dorosty A, et al. Early life risk factors for obesity in childhood: cohort study. BMJ. 2005;330:1–7. doi: 10.1136/bmj.38470.670903.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lumeng J, Somashekar D, Appugliese D, Kaciroti N, Corwyn R, Bradley R. Shorter sleep duration is associated with increased risk for being overweight at ages 9 to 12 years. Pediatrics. 2007;120:1020–9. doi: 10.1542/peds.2006-3295. [DOI] [PubMed] [Google Scholar]
- 19.Snell E, Adam E, Duncan G. Sleep and the body mass index and overweight status of children and adolescents. Child Dev. 2007;78:309–23. doi: 10.1111/j.1467-8624.2007.00999.x. [DOI] [PubMed] [Google Scholar]
- 20.Chaput J-P, Brunet M, Tremblay A. Relationship between short sleeping hours and childhood overweight/obesity: results from the ‘Que’bec en Forme' Project. Int J Obes (Lond) 2006;30:1080–5. doi: 10.1038/sj.ijo.0803291. [DOI] [PubMed] [Google Scholar]
- 21.Horne J. Too weighty a link between short sleep and obesity? Sleep. 2008;31:595–6. doi: 10.1093/sleep/31.5.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Horne J. Short sleep is a questionable risk factor for obesity and related disorders: statistical versus clinical significance. Biol Psychol. 2008;77:266–76. doi: 10.1016/j.biopsycho.2007.12.003. [DOI] [PubMed] [Google Scholar]
- 23.Calamaro CJ, Park S, Mason TB, et al. Shortened sleep duration does not predict obesity in adolescents. J Sleep Res. 2010;19:559–66. doi: 10.1111/j.1365-2869.2010.00840.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Werner H, Le Bourgeois MK, Geiger A, Jenni OJ. Assessment of chronotype in four- to eleven-year-old children: reliability and validity of the children's chronotype questionnaire (CCTQ) Chronobiol Int. 2009;26:992–1014. doi: 10.1080/07420520903044505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gaina A, Sekine M, Kanayama H, et al. Morning-evening preference: sleep pattern spectrum and lifestyle habits among Japanese junior high school pupils. Chronobiol Int. 2006;23:607–21. doi: 10.1080/07420520600650646. [DOI] [PubMed] [Google Scholar]
- 26.Schubert E, Randler C. Association between chronotype and the constructs of the Three-Factor-Eating-Questionnaire. Appetite. 2008;51:501–5. doi: 10.1016/j.appet.2008.03.018. [DOI] [PubMed] [Google Scholar]
- 27.Salmon J, Campbell K, Crawford D. Television viewing habits associated with obesity risk factors: a survey of Melbourne schoolchildren. Med J Aust. 2006;184:64–7. doi: 10.5694/j.1326-5377.2006.tb00117.x. [DOI] [PubMed] [Google Scholar]
- 28.Lewis M, Hill A. Food advertising on British children's television: a content analysis and experimental study with nine-year olds. Int J Obes Relat Metab Disord. 1998;22:206–14. doi: 10.1038/sj.ijo.0800568. [DOI] [PubMed] [Google Scholar]
- 29.Neville L, Thomas M, Bauman A. Food advertising on Australian television: the extent of children's exposure. Health Promot Int. 2005;20:105–12. doi: 10.1093/heapro/dah601. [DOI] [PubMed] [Google Scholar]
- 30.Stitt C, Kunkel D. Food advertising during children's television programming on broadcast and cable channels. Health Commun. 2008;23:573–84. doi: 10.1080/10410230802465258. [DOI] [PubMed] [Google Scholar]
- 31.Smith A. Effects of caffeine on human behavior. Food Chem Toxicol. 2002;40:1243–55. doi: 10.1016/s0278-6915(02)00096-0. [DOI] [PubMed] [Google Scholar]
- 32.Kathrotia R, Rao P, Paralikar S, Shah C, Oommen E. Late sleeping affects sleep duration and body mass index in adolescents. Iranian J Med Sci. 2010;35:57–60. [Google Scholar]
- 33.Touchette E, Mongrain V, Petit D, Tremblay R, Montplaisir J. Development of sleep-wake schedules during childhood and relationship with sleep duration. Arch Pediatr Adolesc Med. 2008;162:343–9. doi: 10.1001/archpedi.162.4.343. [DOI] [PubMed] [Google Scholar]
- 34.Calamaro C, Mason T, Ratcliffe S. Adolescents living the 24/7 lifestyle: effects of caffeine and technology on sleep duration and daytime functioning. Pediatrics. 2009;123:e1005–e10. doi: 10.1542/peds.2008-3641. [DOI] [PubMed] [Google Scholar]
- 35.Natale V, Cicogna P. Morningness-eveningness dimension: is it really a continuum? Pers Individ Dif. 2002;32:809–16. [Google Scholar]
- 36.Putilov A. Association of morning and evening lateness with self-scored health: late to bed and early to rise makes a man healthy in his own eyes. Biol Rhythm Res. 2008;39:321–33. [Google Scholar]
- 37.Leopold-Levi M. Le lever matinual precoce. Bulletin et memoires de la Societe de Medicine de Paris. 1932:117–21. [Google Scholar]
- 38.Commonwealth Department of Health and Aged Care. Measuring remoteness: Accessibility/Remoteness Index of Australia (ARIA) Revised edition. Canberra: Commonwealth of Australia; 2001. [Google Scholar]
- 39.Olds T, Tomkinson G, Maher C, Ferrar K. Trends in the prevalence of childhood overweight and obesity in Australia between 1985 and 2008. Int J Obes. 2010;34:57–66. doi: 10.1038/ijo.2009.211. [DOI] [PubMed] [Google Scholar]
- 40.Australian Bureau of Statistics. Socio-economic indexes for areas (SEIFA) - Index of relative disadvantage. Australia: Commonwealth of Australia; 2001. [Google Scholar]
- 41.Marfell-Jones M, Olds T, Stewart A, Carter L. International standards for anthropometric assessment. Potchefstroom, RSA: North-West University; 2006. [Google Scholar]
- 42.Ridley K, Olds TS, Hill A. The Multimedia Activity Recall for Children and Adolescents (MARCA): development and evaluation. Int J Behav Nutr Phys Act. 2006;3 doi: 10.1186/1479-5868-3-10. Epub 26 May. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Olds TS, Ridley K, Dollman J, Maher CA. The validity of a computerized use of time recall, the multimedia activity recall for children and adolescents. Pediatr Exerc Sci. 2010;22:34–43. doi: 10.1123/pes.22.1.34. [DOI] [PubMed] [Google Scholar]
- 44.Ridley K, Olds T. Assigning energy costs to activities in children: a review and synthesis. Med Sci Sport Exerc. 2008;40:1439–46. doi: 10.1249/MSS.0b013e31817279ef. [DOI] [PubMed] [Google Scholar]
- 45.Department of Health and Ageing. 2007 Australian National Children's Nutrition and Physical Activity Survey - Main Findings. Canberra: Department of Health and Ageing; 2008. [Google Scholar]
- 46.Department of Health and Ageing. Australia's Physical Activity Recommendations for Children and Young People. 2005. cited 2005 31 Jan. Available from: http://www.health.gov.au/internet/wcms/publishing.nsf/Content/health-pubhlth-strateg-active-recommend.html.
- 47.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–3. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cole TJ, Freeman JV, Preece MA. Body mass index reference curves for the UK, 1990. Arch Dis Child. 1995;73:25–9. doi: 10.1136/adc.73.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sekine M, Yamagami T, Handa K, et al. A dose-response relationship between short sleeping hours and childhood obesity: results of the Toyama Birth Cohort Study. Child Care Health Dev. 2002;28:163–70. doi: 10.1046/j.1365-2214.2002.00260.x. [DOI] [PubMed] [Google Scholar]
- 50.Ridley K. Adelaide: University of South Australia; 2005. The Multimedia Activity Recall for Children and Adolescents (MARCA): development and validation [PhD] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Trost SG, Morgan A, Saunders R, Felton G, Ward D, Pate R. Children's understanding of the concept of physical activity. Pediatr Exerc Sci. 2000;12:293–9. [Google Scholar]
- 52.Carskadon MA, Acebo C, Jenni OG. Regulation of adolescent sleep: implications for behavior. Ann N Y Acad Sci. 2004;1021:276–91. doi: 10.1196/annals.1308.032. [DOI] [PubMed] [Google Scholar]
- 53.Garaulet M, Ordovás JM, Madrid JA. The chronobiology, etiology and pathophysiology of obesity. Int J Obes. 2010 doi: 10.1038/ijo.2010.118. Epub ahead of print, Jun 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Takeuchi H, Inoue M, Watanabe N, et al. Parental enforcement of bedtime during childhood modulates preference of Japanese junior high school students for eveningness chronotype. Chronobiol Int. 2001;18:823–9. doi: 10.1081/cbi-100107517. [DOI] [PubMed] [Google Scholar]
- 55.Garasky S, Stewart S, Gundersen C, Lohman B, Eisenmann J. Family stressors and child obesity. Soc Sci Res. 2009;38:755–66. doi: 10.1016/j.ssresearch.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 56.Owens JA, Stahl J, Patton A, Reddy U, Crouch M. Sleep practices, attitudes, and beliefs in inner city middle school children: a mixed-methods study. Behav Sleep Med. 2006;4:114–34. doi: 10.1207/s15402010bsm0402_4. [DOI] [PubMed] [Google Scholar]
- 57.Wolfson AR, Carskadon MA. Sleep schedules and daytime functioning in adolescents. Child Dev. 1998;69:875–87. [PubMed] [Google Scholar]
- 58.Wahlstrom K. Changing times: findings from the first longitudinal study of later high school start times. NASSP Bull. 2002;86:3–22. [Google Scholar]
- 59.Moseley L, Gradisar M. Evaluation of a school-based intervention for adolescent sleep problems. Sleep. 2009;32:334–41. doi: 10.1093/sleep/32.3.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.De Sousa IC, Araujo JF, De Azevedo CVM. The effect of a sleep hygiene education program on the sleep–wake cycle of Brazilian adolescent students. Sleep Biol Rhythms. 2007;5:251–8. [Google Scholar]