Abstract
Study Objectives:
Sleep problems are experienced by a large part of the population. Work characteristics are potential determinants, but limited longitudinal evidence is available to date, and reverse causation is a plausible alternative. This study examines longitudinal, bidirectional relationships between work characteristics and sleep problems.
Design:
Prospective cohort/two-wave panel.
Setting:
Sweden.
Participants:
3065 working men and women approximately representative of the Swedish workforce who responded to the 2006 and 2008 waves of the Swedish Longitudinal Occupational Survey of Health (SLOSH).
Interventions:
N/A.
Measurements and Results:
Bidirectional relationships between, on the one hand, workplace demands, decision authority, and support, and, on the other hand, sleep disturbances (reflecting lack of sleep continuity) and awakening problems (reflecting feelings of being insufficiently restored), were investigated by structural equation modeling. All factors were modeled as latent variables and adjusted for gender, age, marital status, education, alcohol consumption, and job change. Concerning sleep disturbances, the best fitting models were the “forward” causal model for demands and the “reverse” causal model for support. Regarding awakening problems, reciprocal models fitted the data best.
Conclusions:
Cross-lagged analyses indicates a weak relationship between demands at Time 1 and sleep disturbances at Time 2, a “reverse” relationship from support T1 to sleep disturbances T2, and bidirectional associations between work characteristics and awakening problems. In contrast to an earlier study on demands, control, sleep quality, and fatigue, this study suggests reverse and reciprocal in addition to the commonly hypothesized causal relationships between work characteristics and sleep problems based on a 2-year time lag.
Citation:
Magnusson Hanson LL; Åkerstedt T; Näswall K; Leineweber C; Theorell T; Westerlund H. Cross-lagged relationships between workplace demands, control, support, and sleep problems. SLEEP 2011;34(10):1403-1410.
Keywords: Workplace, demand, control, support, sleep, sleep disturbances, causation, structural equation modeling, reverse, reciprocal
INTRODUCTION
About one-third of all adults in Europe have complaints of sleep problems, such as difficulties falling asleep, maintaining sleep, early morning awakenings, and non-restorative sleep several times a week. And as much as 9% of the population fulfill the criteria for an insomnia diagnosis, with complaints lasting for at least a month, accompanied by impairment in social, occupational, or other areas of functioning.1 A core symptom of insomnia is non-restorative sleep, a subjective feeling at awakening of having had an unrestful sleep or not being refreshed upon awakening.2 A considerable part of the population experiences non-restorative or unrefreshing sleep which is not due to lack of sleep.2 Non-restorative sleep can thus occur independently of other insomnia symptoms.3 Although sleep problems may be caused by health deficits, they might also precede health problems like poor mental health,4,5 heart disease,6 obesity,7 diabetes,8 and increase mortality risk.9
Chronic stress associated with hyperactivity of the hypothalamic-pituitary-adrenocortical (HPA) and sympatho-adreno-medullary (SAM) systems might lead to impaired sleep.10 A number of working conditions that may constitute stressors such as long work hours, shift work, high workload/demands/job strain, poor social support, effort-reward imbalance, organizational injustice, and workplace bullying have been linked to sleep problems;11–20 whereas retirement has been shown to be followed by a substantial decrease in sleep disturbances.21 In a survey in the US, the most frequent self-reported cause of sleeping difficulties was indeed work-related stress,22 and an increase of work-related sleep problems has been demonstrated among the Swedish working population during the 1990s.23 Some recent investigations using the demand-control and effort-reward imbalance models show prospective relationships between work characteristics and sleep disturbances and/or insomnia.17,20 Thus far, however, evidence from longitudinal studies is limited,10,16,17,20,24 and more evidence is needed to elucidate causality and the directions of the relationships. De Lange et al. recently investigated associations between job demands and control on the one hand, and sleep quality and fatigue on the other hand, and found no reverse or reciprocal patterns.24 However, their sample consisted of a relatively young and predominantly male population. Furthermore, with fewer measurements on sleep quality and fatigue, the chance of detecting reverse or reciprocal associations was lower than of relationships in the hypothesized direction.
In the present study we investigate the longitudinal relationships between the components of the demand-control-support model and sleep problems (sleep disturbances and awakening problems). The study examines both the effects of work characteristics on later sleep problems (subsequently referred to as “forward” causation, i.e., in the direction most often assumed in the literature), and the relationship between sleep problems and work characteristics (referred to as “reverse” causation) two years later.
METHODS
Study Participants
The study was based on the Swedish Longitudinal Occupational Survey of Health (SLOSH).25 In SLOSH, participants in the Swedish Work Environment Survey (SWES) from 2003 are followed up by postal questionnaires every second year. SWES is in turn a subsample of respondents to the Swedish Labor Force Survey (LFS), including gainfully employed men and women from different labor market sectors and occupations. Accordingly, SLOSH is approximately representative of the Swedish working population in 2003. The first follow-up (Wave 1) of SWES 2003 was conducted in 2006, with 5985 (65%) respondents: 5141 “gainfully employed” and 844 “not gainfully employed.” Respondents were categorized as gainfully employed if they had responded to the questionnaire for those who had worked on average ≥ 30% during the past 3 months. In 2008 (Wave 2), participants in SWES 2003 were again followed up, with a total of 5557 (61%) respondents: 4672 gainfully employed and 885 not gainfully employed. The present study included those individuals who took part in the 2006 as well as the 2008 follow-up survey (n = 4690; 78% of all participants in Wave 1), and who were categorized as gainfully employed at both occasions (n = 3644; see Figure 1). Subjects with incomplete data on any of the questions of interest were excluded, resulting in a study sample of 3041 individuals. Compared to all participants in SWES 2003 (n = 9214), a higher proportion of the respondents included in the final study sample were in the age range 40-59 in 2003, and a higher proportion had university education. However, the gender distribution was virtually the same, as were the mean scores on demand, control, and support proxy measures from SWES 2003, and the mean scores on items measuring if respondents get enough sleep, have a hard time sleeping because of thoughts of work, and feel tired and listless after work.23,25 The study was based on informed consent and has been approved by the Regional Research Ethics Board in Stockholm.
Figure 1.
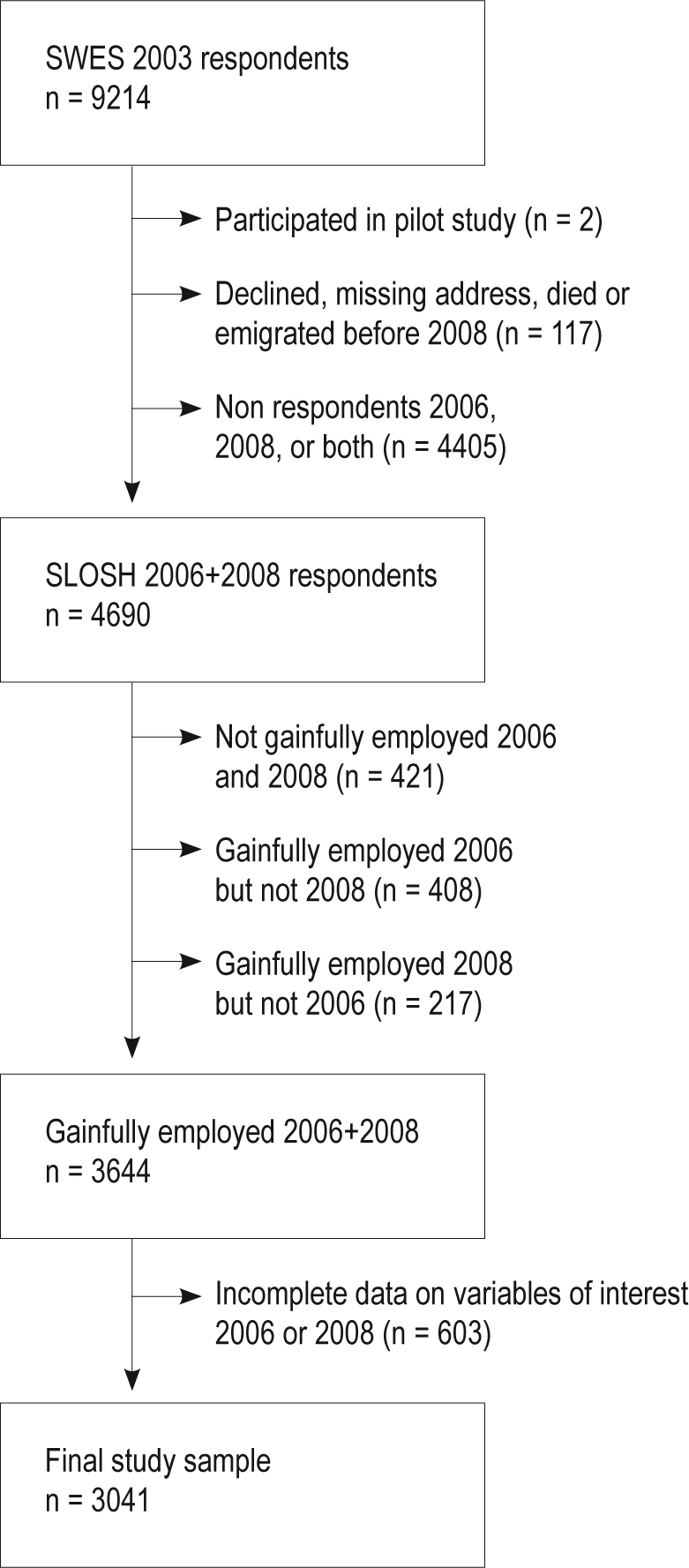
Participants from the Swedish Work Environment Survey (SWES) 2003 and in the Swedish Longitudinal Occupational Survey of Health 2006 and 2008 included in the final study sample.
Measures
The questionnaires for gainfully employed in Wave 1 and 2 included numerous questions about the psychosocial work environment, work organization, health, and health-related complaints. Demands, control and support at work were measured by the Swedish version of the Demand-Control Questionnaire (DCQ).11 Demands at work were assessed by 5 questions (working fast, working intensively, too much effort, enough time, and conflicting demands) with 5 response options (1 = Never/almost never – 4 = Often). Cronbach α was 0.75 at Time 1 and 0.72 at Time 2. Decision authority was assessed with 2 questions (choice in how you do your work and what you do) with 4 response options (1 = To a very small extent/not at all – 4 = To a very great extent). Cronbach α was 0.77 at Time 1 and 0.73 at Time 2. Social support was measured with 6 questions (calm and pleasant atmosphere, good spirit of unity, colleagues are there for me, people understand a bad day, get on well with my colleagues, get on well with my superiors) with 4 response options (1 = Strongly disagree – 4 = Strongly agree). Cronbach α was 0.85 at both time points. A question about working hours was modified from SWES and categorized into 1 = day work; 2 = evening, shift work (2 shifts), discretionary/unregulated working hours or other; and 3 = night work and shift work (3 shifts). Physical strain was assessed by another question from SWES: Does your work sometimes involve physical labor, that is, do you physically exert yourself more than one does when walking and standing and moving around in a normal way? (response options 1 = No, not at all – 6 = Nearly all the time). Sleep disturbances (reflecting lack of sleep continuity) were assessed with 4 questions (difficulty falling asleep, repeated awakenings, early awakening, disturbed sleep); whereas awakening problems (reflecting feelings of being insufficiently restored) were measured with 3 questions (difficulty awakening, not well-rested, exhausted at awakening), all from the Karolinska Sleep Questionnaire.12,26,27 The following response options were used: 1 = Never – 6 = Always/5 times a week or more. Cronbach α was 0.85 for disturbed sleep and 0.80 for awakening problems at both time points. Information about gender and age was retrieved from baseline register data. The questionnaires further included information about marital status (1 = single, 2 = married or cohabiting), small children (0-5 years of age) at home (1 = yes, 2 = no), educational level (1 = compulsory, 2 = 2-year upper secondary/vocational training, 3 = 3 or 4-year upper secondary education, 4 = university or equivalent < 3 years, 5 = university or equivalent ≥ 3 years), as well as life style factors such as smoking (1 = yes daily, 2 = yes sometimes, 3 = no), alcohol consumption (1 = never, 2 = once a month or less, 3 = 2-4 times a month, 4 = 2-3 times a week, 5 = 4 times/week or more), and exercise (1 = never, 2 = not very much, 3 = now and again, 4 = regularly). Body mass index (BMI) was calculated from measurements of length and weight and categorized into underweight, normal, overweight, and obese according to the World Health Organization (WHO) standards. Finally, we took into consideration job change, whether subjects had changed their job between the surveys (1 = yes, 2 = no), as well as Time 1 self-rated health (general health status),28 symptoms of emotional exhaustion as measured by the emotional exhaustion subscale of Maslach Burnout Inventory General Survey (MBI-GS),25 and depressive symptoms by means of a brief depression subscale based on Hopkins Symptom Checklist 90 (SCL-90).29
Analytic Strategy
The data were first analyzed by means of the Predictive Analytics Software (PASW) Statistics 18.0. A missing value analysis was performed to assess the pattern of missing data. As Little's missing completely at random (MCAR) test was nonsignificant, indicating that data were missing completely at random, deletion of individuals with missing data was presumed to result in a random subsample of the original target sample. The distribution of the items measuring work characteristics and sleep problems was inspected and found approximately symmetric for the majority of the items. The sleep items exhibited some skewness, but since most of them were only moderately skewed we did not use any transformation. The bivariate relationships between component scores at Time 1 were also checked and were approximately linear. Structural equation models were then fitted using the LISREL 8.8 Software. Estimations were based on covariance matrices using the robust maximum likelihood method. We first tested the measurement model for sleep problems. A confirmatory factor analysis based on data from Time point 1 supported further analyses of sleep problems by the 2 indices: sleep disturbances and awakening difficulties. Compared to a null model with 7 distinct factors, a model with all sleep items as one factor, a model with 2 orthogonal factors (sleep disturbances and awakening problems), the 2-factor oblique solution provided significantly (P < 0.001) better fit to the data.
Next, cross-lagged relationships were estimated, including latent variables for demands, decision authority, support, sleep disturbances, and awakening problems. Preliminary analyses indicated different effects of the different work stress variables on the different sleep indices. Separate models were thus tested (one for each combination of work characteristics and sleep measure). Several competing models for each combination were tested. First, a model only including auto-regressions within factors over time (i.e., paths between the work stress variables at Time 1 (T1) and Time 2 (T2), as well as between the sleep indices T1 and T2) was fitted and regarded as the null model (Model 0). Then competing models were tested, including (1) forward paths (T1 work characteristics to T2 sleep problems, Model 1), (2) reverse paths (T1 sleep problem to T2 work characteristics, Model 2), and (3) reciprocal paths (both forward and reverse, i.e., paths from the work characteristics at baseline to sleep problems at follow-up as well as from sleep problems at baseline to the work characteristics at follow-up, Model 3). The models all allowed for correlations between item-specific error terms over time as well as between latent variable error terms within time, and were adjusted for the covariates gender, age, marital status, education, alcohol consumption from T1, and change of jobs between the surveys. Preliminary bivariate analyses indicated no need to control for shift work, physical strain at work, presence of small children at home, body mass index, exercise, or smoking. Potential confounding effects of health measures were examined by additional adjustment for self-rated health, depressive symptoms, and/or emotional exhaustion scores.
Various fit indices were used to assess model fit based on recommendations by Kelloway as well as Hu and Bentler.30,31 The χ2 test, the root mean squared error of approximation (RMSEA), and the goodness of fit index (GFI) were used as indicators of absolute fit, and the comparative fit index (CFI) as a measure of comparative fit. RMSEA values < 0.05 are regarded to indicate a very good fit to the data,31,32 while GFI and CFI values > 0.90 indicate a good fit to the data. Finally a smaller value on the Akaike Information Criterion (AIC) was used to indicate a more parsimonious model.31 Local fit was also considered for structural paths in terms of standardized beta regression coefficients (β) and t-values. Moreover, the χ2 difference test was used to determine which of the competing models that provided the best fit to the data. Models 1-3 were all compared to the null model. If Models 1 or 2 as well as Model 3 showed significantly better fit than the null model, Model 3 was subsequently compared to the better-fitting of Models 1 and 2.
RESULTS
The participants who answered both questionnaires and were working at both time points were on average 47.1 years old, and the majority were married or cohabiting (Table 1.). A relatively large proportion of the respondents reported a high level of education.
Table 1.
Characteristics of the study sample
| Number | % | |
|---|---|---|
| Sex | ||
| Men | 1442 | 47.4 |
| Women | 1599 | 52.6 |
| Age | ||
| 20-29 | 140 | 4.6 |
| 30-39 | 625 | 20.6 |
| 40-49 | 876 | 28.8 |
| 50-59 | 1057 | 34.8 |
| 60-68 | 343 | 11.3 |
| Marital Status | ||
| Single | 663 | 21.8 |
| Married/cohabiting | 2378 | 78.2 |
| Education | ||
| Compulsory | 471 | 15.5 |
| 2-year upper secondary/vocational training | 707 | 23.2 |
| 3 or 4-year upper secondary education | 584 | 19.2 |
| University < 3 years or equivalent | 446 | 14.7 |
| University ≥ 3 years or equivalent | 833 | 27.4 |
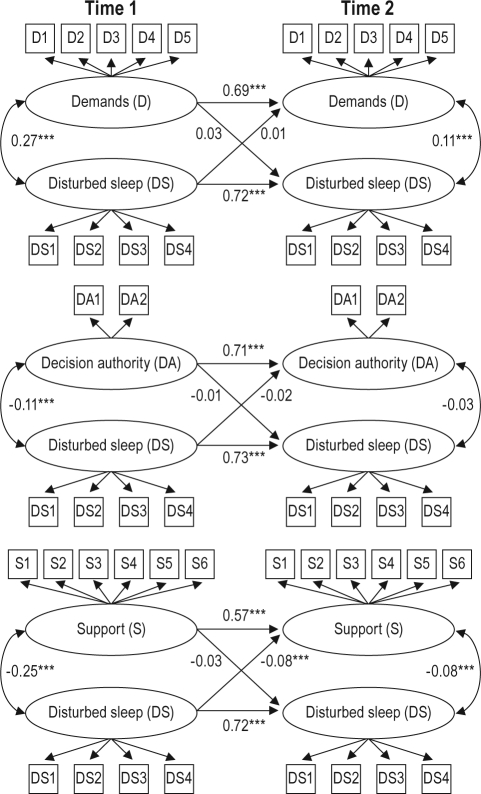
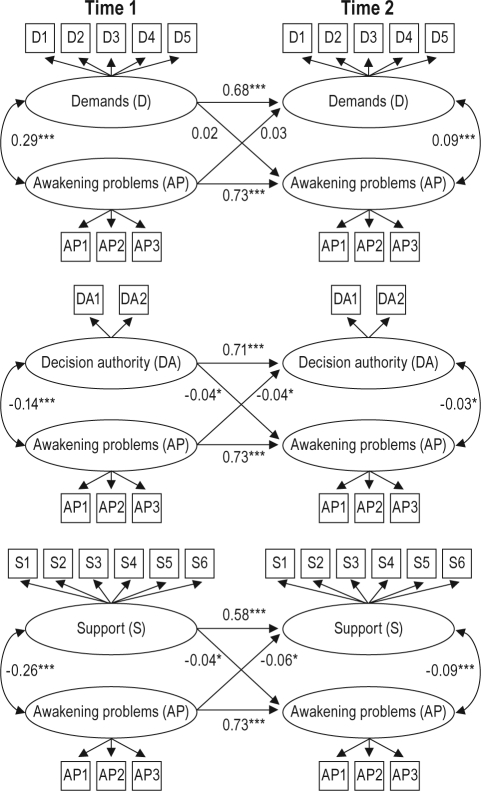
The stability of the investigated constructs was high. The auto-regressions varied from 0.57-0.58 for support, 0.68-0.69 for demand, 0.71 for decision authority, 0.72-0.73 for disturbed sleep, to 0.73 for awakening problems, according to the reciprocal causation model (Figures 2–3).
Figure 2.
A simplified illustration of latent variable path analyses and main paths of interest, including standardized regression coefficients (β) for the forward and reverse relationships between demands, decision authority, support, and sleep disturbances derived from the reciprocal causation model (Model 3). The models are adjusted for sex, age, marital status, education, alcohol consumption, and job change. *P < 0.05, **P < 0.01, ***P < 0.001.
Figure 3.
A simplified illustration of latent variable path analyses and main paths of interest, including standardized regression coefficients (β) for the forward and reverse relationships between demands, decision authority, support and awakening problems derived from the reciprocal causation model (Model 3). The models are adjusted for sex, age, marital status, education, alcohol consumption, and job change. *P < 0.05, **P < 0.01, ***P < 0.001.
Sleep Disturbances
In Table 2 fit statistics and model comparisons are presented for the competing models of the demand-control-support components and sleep disturbances. According to the RMSEA, GFI, and CFI fit statistics, all models concerning sleep disturbances provided a good or very good fit to the data. However, the χ2 comparison test of the competing models including demands and sleep disturbances showed that the fit of Model 1, including forward paths, and Model 3, including reciprocal paths, were significantly better than the fit of the null model. A comparison of the former 2 models further showed that Model 3 did not provide significantly better fit to the data than Model 1. Consequently, the models including the forward path from Time 1 demands to Time 2 sleep disturbances provided the best fit to the data. The competing models for decision authority and sleep disturbances did not differ significantly from the null model, indicating that the model with only auto-regressions best described the relationships between the variables. Model 2 (with reverse paths) and 3 (with reciprocal paths) including support differed significantly from Model 0. However, Model 3 did not differ significantly from Model 2, indicating that the models, including the reverse causal path from Time 1 sleep disturbances to Time 2 support, provided the best fit to the data.
Table 2.
Model fit and comparison for structural equation models of work characteristics in relation to sleep disturbances
| Model | Model Fit# |
Model Comparison |
||||||
|---|---|---|---|---|---|---|---|---|
| df | χ2 | RMSEA | AIC | Model | Δ χ2 | Model | Δ χ2 | |
| Demands | ||||||||
| Model 0 (M0) | 218 | 1260.16 | 0.040 | 1424.16 | ||||
| Model 1 (M1) Forward | 217 | 1255.33 | 0.040 | 1421.33 | M1 vs M0 | 4.83* | ||
| Model 2 (M2) Reverse | 217 | 1258.60 | 0.040 | 1424.60 | M2 vs M0 | 1.56 | ||
| Model 3 (M3) Reciprocal | 216 | 1253.84 | 0.040 | 1421.84 | M3 vs M0 | 6.32* | M3 vs M1 | 1.49 |
| Decision Authority | ||||||||
| Model 0 (M0) | 104 | 401.77 | 0.031 | 535.77 | ||||
| Model 1 (M1) Forward | 103 | 400.69 | 0.031 | 536.69 | M1 vs M0 | 1.08 | ||
| Model 2 (M2) Reverse | 103 | 400.03 | 0.031 | 536.03 | M2 vs M0 | 1.74 | ||
| Model 3 (M3) Reciprocal | 102 | 398.93 | 0.031 | 536.93 | M3 vs M0 | 2.84 | ||
| Support | ||||||||
| Model 0 (M0) | 264 | 1300.16 | 0.036 | 1474.16 | ||||
| Model 1 (M1) Forward | 263 | 1297.11 | 0.036 | 1473.11 | M1 vs M0 | 3.05 | ||
| Model 2 (M2) Reverse | 263 | 1285.46 | 0.036 | 1461.46 | M2 vs M0 | 14.7*** | ||
| Model 3 (M3) Reciprocal | 262 | 1282.74 | 0.036 | 1460.74 | M3 vs M0 | 17.42*** | M3 vs M2 | 2.72 |
Analyses are controlled for sex, age, marital status, education, alcohol consumption, and job change.
df, degrees of freedom; RMSEA, root mean squared error of approximation; AIC, The Akaike Information Criterion.
Goodness of fit index (GFI) and comparative fit index (CFI) are not presented here as they did not change for M0-M3.
P < 0.05,
P < 0.001.
The regression coefficients for the forward and reverse structural paths for models concerning work stress and sleep disturbances are presented in Figure 2. The path from T1 demands to T2 sleep disturbances was borderline significant, but not the path from T1 sleep disturbances to T2 demands. T1 sleep disturbances, on the other hand, showed a significant positive β coefficient in relation to T2 support, whereas the effect of support on subsequent sleep disturbances did not reach statistical significance. Factor loadings can be found in the Supplemental Appendix (Table S1). Graphs of the full basic LISREL models are also in the supplement (Figures S1–S6).
The regression coefficients were virtually unaltered and the results of the model comparisons were the same when self-rated health, emotional exhaustion and/or depression symptoms, one measure at a time or several simultaneously, were added as covariates at T1.
Awakening Problems
Table 3 presents the model fit and model comparisons for models on demand, control, support and awakening problems. All models concerning awakening problems also provided a good or very good fit to the data. The only model including demands that differed significantly from the null model was the reciprocal model. In contrast, all competing models on decision authority and support showed significantly better fit to the data than Model 0. For both decision authority and support, again Model 3, with reciprocal paths, demonstrated the best fit to the data by means of the χ2 difference test. Neither the forward nor the reverse paths for demands reached statistical significance, whereas both paths were significant and negative in the case of decision authority and support (Figure 3.) For decision authority the standardized coefficients were of equal magnitude, while there was a stronger negative association between T1 awakening problems and T2 support than between T1 support and T2 awakening problems. All significant coefficients were in the expected direction. Factor loadings can be found in the Appendix (Table S1). As for disturbed sleep, the results were not markedly affected by additional adjustment for health measures.
Table 3.
Model fit and comparison for structural equation models of work characteristics in relation to awakening problems
| Model | Model Fit# |
Model Comparison |
||||||
|---|---|---|---|---|---|---|---|---|
| df | χ2 | RMSEA | AIC | Model | Δ χ2 | Model | Δ χ2 | |
| Demands | ||||||||
| Model 0 (M0) | 176 | 1142.10 | 0.042 | 1296.10 | ||||
| Model 1 (M1) Forward | 175 | 1140.00 | 0.043 | 1296.00 | M1 vs M0 | 2.1 | ||
| Model 2 (M2) Reverse | 175 | 1139.98 | 0.043 | 1295.98 | M2 vs M0 | 2.12 | ||
| Model 3 (M3) Reciprocal | 174 | 1137.92 | 0.043 | 1295.92 | M3 vs M0 | 4.18* | ||
| Decision Authority | ||||||||
| Model 0 (M0) | 74 | 264.63 | 0.029 | 388.63 | ||||
| Model 1 (M1) Forward | 73 | 259.85 | 0.029 | 385.85 | M1 vs M0 | 4.78* | ||
| Model 2 (M2) Reverse | 73 | 260.24 | 0.029 | 386.24 | M2 vs M0 | 4.39* | ||
| Model 3 (M3) Reciprocal | 72 | 255.47 | 0.029 | 383.47 | M3 vs M0 | 9.16** | M3 vs M1 | 4.38* |
| Support | ||||||||
| Model 0 (M0) | 218 | 1135.14 | 0.037 | 1299.14 | ||||
| Model 1 (M1) Forward | 217 | 1130.69 | 0.037 | 1296.69 | M1 vs M0 | 4.45* | ||
| Model 2 (M2) Reverse | 217 | 1127.46 | 0.037 | 1293.46 | M2 vs M0 | 7.68** | ||
| Model 3 (M3) Reciprocal | 216 | 1123.33 | 0.037 | 1291.33 | M3 vs M0 | 11.81*** | M3 vs M2 | 4.13* |
Analyses are controlled for sex, age, marital status, education, alcohol consumption, and job change.
df, degrees of freedom; RMSEA, root mean squared error of approximation; AIC, The Akaike Information Criterion.
Goodness of fit index (GFI) and comparative fit index (CFI) are not presented here as they did not change for M0-M3.
P < 0.05,
P < 0.01,
P < 0.001.
DISCUSSION
The results indicated forward as well as reverse and reciprocal relationships between work characteristics and sleep problems 2 years later.
Our finding of a close to significant positive association between demands and later sleep disturbances is in accordance with the recent study by de Lange et al.,24 as well as with a study by Ota et al. which showed a positive prospective relationship between job strain and insomnia.20 Contrary to De Lange et al., however, who found positive effects of both demands and control on sleep quality and fatigue, our results did not indicate a forward effect of job control, measured by decision authority, on sleep disturbances. We did, on the other hand, find a forward effect on awakening problems. Although the measures of fatigue by de Lange et al. and our measure of awakening problems have one item in common (not well rested at awakening), fatigue in their study otherwise seem to refer to daytime fatigue rather than non-restorative sleep. Concerning support, Ota et al. did not find a prospective relationship with insomnia among those who were not insomniacs at baseline. However, among those with insomnia at baseline, low support was associated with insomnia two years later. No significant forward effect on sleep disturbances could be demonstrated in the present study either, although a tendency was observed, as well as a weak but significant direct effect of support on awakening problems. Ota et al. interpret their results as indicating no association between support and onset of insomnia, but an association between support and persistence of insomnia. They suggest that sufficient support may facilitate recovery from insomnia and further discuss a vicious circle of stress and insomnia through hyperreactivity of the HPA and SAM systems. However, the only study we have found that specifically investigated reverse and reciprocal associations between work stress and sleep problems did not find support for reverse or reciprocal links between demand or control and sleep quality/fatigue, using a 3-year time lag.24 Conversely, our present study, based on an approximately representative sample drawn from the working age population and with different measures of sleep problems/fatigue, indicates a reciprocal pattern for decision authority and awakening problems. In our study, a 2-year instead of a 3-year time lag is used, which may explain the differences in results. In the present study, reverse and reciprocal patterns were also demonstrated for support, which was not investigated by De Lange et al.24 The reverse paths related to support actually showed the strongest regression coefficients in the present study. This is in line with research showing that people with insomnia usually report more daytime problems, including problems with social functioning/social relationships.1,33,34 A prospective association between insomnia and low social support has also been shown among adolescents.35 Yet, to our knowledge a prospective association between sleep problems and social support at work has not been clearly demonstrated in previous research.
Future studies will have to reveal whether our findings on reverse/reciprocal associations are spurious or due to a changed experience of the work environment. There is, however, some evidence of reverse or reciprocal relationships for related health problems like poor mental health, suggesting that poor mental health may affect the experience of work stress.36–38 A few studies on support prospectively link affective strains like irritation, depression, anger, and loneliness to decreased workplace support,39 as well as emotional exhaustion to social support from supervisors.37,40 No reverse causation in relation to emotional exhaustion, however, was demonstrated for support in a study using a 1-year interval41 or in another with a 2-year time lag,42 though the study samples were small. Different mechanisms explaining reverse effects of mental health on work have also been put forward.38 First, two types of changes or a combination of the two can occur as a result of poor health—either a change in the perception of the same work environment, or an actual change in the work environment. The authors further speculate that people may perceive their work in either a rosier or gloomier light depending on their health status. There may also be an upward selection mechanism into more favorable job situations or a drift mechanism, according to which people with poor mental health would drift to more unfavorable jobs. All but the drift mechanism were supported in an analysis of healthy and unhealthy job changers versus stayers.38
Both perceptional and environmental changes could be hypothesized to be consequences of sleep problems. Poor sleep may be associated with mood changes, as well as decreased cognitive abilities,33 which could influence how the work environment is perceived. Difficulties with social relationships have also been demonstrated.33,34 Reduced productivity/efficiency and work ability are other probable consequences of sleep problems.33,43 Changes in mood, social functioning, or decreased work efficiency could in turn influence the behavior of superiors/colleagues. As a result, the employee may experience actual changes in support from superiors/colleagues, control at work, or in work demands, within the same job or through job transfer. Awakening problems in particular, which may by a stronger indicator of inadequate sleep/fatigue, could be suspected to be linked to a more negative perception of the work environment or changed behaviors by superiors/coworkers. It is also interesting that both social support and decision authority showed significant reciprocal relationships with awakening problems. This may be an illustration of a negative spiral, with low decision authority and poor support causing awakening problems, which in turn cause reduced experience of decision authority and social support.
The present study has a number of advantages compared with much of the previous literature on work characteristics and sleep problems. It is not restricted to specific segments of the labor market, but based on a large, approximately representative sample of the Swedish workforce. This contributes to good generalizability, and allows the examination of a wide range of scores on job stress and sleep problems. Even more importantly, it is longitudinal with repeat measures of both work stressors and sleep problems. By examining different types of plausible causal relationships, the study contributes to a more comprehensive understanding of causality between work stress and sleep problems. There are, however, some methodological limitations. All measures are based on survey data. Thanks to the longitudinal design, some problems associated with using self-report data are avoided, such as influence by occasion factors (e.g., mood at the time of survey).36 However, other unmeasured third variables, such as negative affectivity and social desirability, may still affect our results. Health problems could be a common cause of work stress and sleep problems and create spurious associations. However, health problems at Time 1 did not seem to influence the results. As in most longitudinal studies, attrition may bias the results, possibly resulting in an underestimation of true relationships. No major bias due to drop-out was indicated in a comparison between the study sample and all SWES participants. It is, however, unclear if non-response to the SWES and LFS could have any influence on results.
The results show relatively low regression coefficients. This is to be expected, as the stability of the estimates, which was relatively high, was adjusted for by the inclusion of auto-regressions over time, in effect adjusting for the effects of previous work stress and sleep problems. A large part of the variability is thus already explained, and only changes are predicted. By allowing correlations also between measures at the same time point, cross-sectional relationships between work stress and sleep are additionally accounted for by the models. Moreover, the present modeling approach does not account for hypothesized interaction between demands, decision authority, and support and stress reactions. According to the strain and iso-strain hypotheses, stronger associations may be expected between job strain (a combination of high demands and low control), especially in combination with poor support (iso-strain) and sleep problems. The fact that all variables are modeled as linear variables may also reduce the estimates of the associations, for instance if a certain degree of work stress is necessary for an effect on sleep.
Another issue concerns whether the measures represent transient or enduring problems with stress and sleep. Cumulative exposures to strain and active work have been shown to have relevance for sleep problems, and an improvement in these working conditions does not necessarily results an immediate reduction in sleep problems.24 The causes and consequences of persistent problems may be different from those of temporary problems as indicated by Ota et al.20 Finally, the time lag in the present study could be discussed. A 2-year time lag has been found appropriate when studying the effect of social stressors on irritation and depressive symptoms.44 However, if the true causal lag time concerning sleep problems is shorter or longer than 2 years, the study is not optimally designed for detecting those particular associations. Most of the effects of transient stress on sleep are likely to be immediate, mediated by worrying thoughts.10 The true time lag for forward and reverse effects, or for different types of reverse effects, may also differ, which could influence the results. Reverse effects explained by perceptional changes may have short time lag, whereas other changes may take longer.
CONCLUSIONS
The findings of this cross-lagged analysis indicate a weak effect of demands on later sleep disturbances, an effect of sleep disturbances on later ratings on social support, and reciprocal relationship between awakening problems and work characteristics. In contrast to an earlier study on demands, control, sleep quality, and fatigue, this study suggests that there are reverse and reciprocal causal relationships, in addition to associations in the usually hypothesized direction, between work characteristics and sleep problems based on a 2-year time lag. Further studies should investigate these relationships with varying time lags and several waves of data.
DISCLOSURE STATEMENT
This was not an industry supported study. Prof Åkerstedt has consulted for Johnson & Johnson The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
Funding for this work was provided by the Swedish Council for Working Life and Social Research (FAS), who also supported research through the Stockholm Stress Center.
APPENDIX
Table S1.
Factor loadings derived from the reciprocal models
| Latent Variable | Item | Item Content | Factor Loadings Time 1 |
|---|---|---|---|
| Demands | 1 | Enough time | 0.60, 0.59# |
| Demands | 2 | Working fast | 0.59 |
| Demands | 3 | Working intensively | 0.71 |
| Demands | 4 | Too much effort | 0.73 |
| Demands | 5 | Conflicting demands | 0.41, 0.42# |
| Decision authority | 1 | Choice in how you do your work | 0.84, 0.82# |
| Decision authority | 2 | Choice in what you do at work | 0.75, 0.77# |
| Support | 1 | Calm and pleasant atmosphere | 0.62 |
| Support | 2 | Good spirit of unity | 0.80 |
| Support | 3 | Colleagues are there for me | 0.81 |
| Support | 4 | People understand a bad day | 0.72 |
| Support | 5 | Get on well with my superiors | 0.52 |
| Support | 6 | Get on well with my colleagues | 0.76 |
| Disturbed sleep | 1 | Difficulties falling asleep | 0.66 |
| Disturbed sleep | 2 | Repeated awakenings | 0.89 |
| Disturbed sleep | 3 | Premature awakening | 0.71 |
| Disturbed sleep | 4 | Disturbed sleep | 0.81 |
| Awakening problems | 1 | Difficulties awakening | 0.59 |
| Awakening problems | 2 | Not well rested at awakening | 0.89, 0.90$ |
| Awakening problems | 3 | Exhausted at awakening | 0.81, 0.80$ |
Factor loadings derived from the reciprocal model of work characteristics in relation to awakening problems.
Factor loadings derived from the reciprocal model of awakening problems in relation to decision authority and support.
Basic LISREL model with standard solution estimates for the model including reciprocal paths between demands (D) and disturbed sleep (DS). Please observe that the time points are aligned from top to bottom of the figure. Variables ending with 1 refer to variables measured at time point 1 (2006) while variables ending with 2 refer to variables measured at time point 2 (2008). a-e denotes the specific items included in the latent variables: Da, enough time; Db, working fast; Dc, working intensively; Dd, too much effort; De, conflicting demands; DSa, difficulty falling asleep; DSb, repeated awakenings; DSc, early awakening; DSd, disturbed sleep. Sex, Gender (women vs men); Age, Age; Marit, Marital status (married/cohabiting vs single); Educ, Education; Alcoh, Alcohol consumption; Jobch, Job change between 2006 and 2008.
Basic LISREL model with standard solution estimates for the model including reciprocal paths between decision authority (DA) and disturbed sleep (DS). Please observe that the time points are aligned from top to bottom of the figure. Variables ending with 1 refer to variables measured at time point 1 (2006) while variables ending with 2 refer to variables measured at time point 2 (2008). a-d denotes the items included in the latent variables: DAa, choice in how you do your work; DAb, choice in what you do at work; DSa, difficulty falling asleep; DSb, repeated awakenings; DSc, early awakening; DSd, disturbed sleep. Sex, Gender (women vs men); Age, Age; Marit, Marital status (married/cohabiting vs single); Educ, Education; Alcoh, Alcohol consumption; Jobch, Job change between 2006 and 2008.
Basic LISREL model with standard solution estimates for the model including reciprocal paths between social support (S) and disturbed sleep (DS). Please observe that the time points are aligned from top to bottom of the figure. Variables ending with 1 refer to variables measured at time point 1 (2006) while variables ending with 2 refer to variables measured at time point 2 (2008). a-f denotes the items included in the latent variables: Sa, calm and pleasant atmosphere; Sb, good spirit of unity; Sc, colleagues are there for me; Sd, people understand a bad day; Se, get on well with my superiors; Sf, get on well with my colleagues; DSa, difficulty falling asleep; DSb, repeated awakenings; DSc, early awakening; DSd, disturbed sleep. Sex, Gender (women vs men); Age, Age; Marit, Marital status (married/cohabiting vs single); Educ, Education; Alcoh, Alcohol consumption; Jobch, Job change between 2006 and 2008.
Basic LISREL model with standard solution estimates for the model including reciprocal paths between demands (D) and awakening problems (AP). Please observe that the time points are aligned from top to bottom of the figure. Variables ending with 1 refer to variables measured at time point 1 (2006) while variables ending with 2 refer to variables measured at time point 2 (2008). a-e denotes the specific items included in the latent variables: Da, enough time; Db, working fast; Dc, working intensively; Dd, too much effort; De, conflicting demands; APa, difficulty awakening; APb, not well-rested; APc, exhausted at awakening. Sex, Gender (women vs men); Age, Age; Marit, Marital status (married/cohabiting vs single); Educ, Education; Alcoh, Alcohol consumption; Jobch, Job change between 2006 and 2008.
Basic LISREL model with standard solution estimates for the model including reciprocal paths between decision authority (DA) and awakening problems (AP). Please observe that the time points are aligned from top to bottom of the figure. Variables ending with 1 refer to variables measured at time point 1 (2006) while variables ending with 2 refer to variables measured at time point 2 (2008). a-d denotes the items included in the latent variables: DAa, choice in how you do your work; DAb, choice in what you do at work; APa, difficulty awakening; APb, not well-rested; APc, exhausted at awakening. Sex, Gender (women vs men); Age, Age; Marit, Marital status (married/cohabiting vs single); Educ, Education; Alcoh, Alcohol consumption; Jobch, Job change between 2006 and 2008.
Basic LISREL model with standard solution estimates for the model including reciprocal paths between social support (S) and awakening problems (AP). Please observe that the time points are aligned from top to bottom of the figure. Variables ending with 1 refer to variables measured at time point 1 (2006) while variables ending with 2 refer to variables measured at time point 2 (2008). a-f denotes the items included in the latent variables: Sa, calm and pleasant atmosphere; Sb, good spirit of unity; Sc, colleagues are there for me; Sd, people understand a bad day; Se, get on well with my superiors; Sf, get on well with my colleagues; APa, difficulty awakening; APb, not well-rested; APc, exhausted at awakening. Sex, Gender (women vs men); Age, Age; Marit, Marital status (married/cohabiting vs single); Educ, Education; Alcoh, Alcohol consumption; Jobch, Job change between 2006 and 2008.
REFERENCES
- 1.Ohayon MM, Reynolds CF., 3rd Epidemiological and clinical relevance of insomnia diagnosis algorithms according to the DSM-IV and the International Classification of Sleep Disorders (ICSD) Sleep Med. 2009;10:952–60. doi: 10.1016/j.sleep.2009.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stone KC, Taylor DJ, McCrae CS, Kalsekar A, Lichstein KL. Nonrestorative sleep. Sleep Med Rev. 2008;12:275–88. doi: 10.1016/j.smrv.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 3.Roth T, Zammit G, Lankford A, et al. Nonrestorative sleep as a distinct component of insomnia. Sleep. 2010;33:449–58. doi: 10.1093/sleep/33.4.449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lustberg L, Reynolds CF. Depression and insomnia: questions of cause and effect. Sleep Med Rev. 2000;4:253–62. doi: 10.1053/smrv.1999.0075. [DOI] [PubMed] [Google Scholar]
- 5.Taylor DJ, Lichstein KL, Durrence HH, Reidel BW, Bush AJ. Epidemiology of insomnia, depression, and anxiety. Sleep. 2005;28:1457–64. doi: 10.1093/sleep/28.11.1457. [DOI] [PubMed] [Google Scholar]
- 6.Schwartz S, Anderson W McDowell, Cole SR, Cornoni-Huntley J, Hays JC, Blazer D. Insomnia and heart disease: a review of epidemiologic studies. J Psychosom Res. 1999;47:313–33. doi: 10.1016/s0022-3999(99)00029-x. [DOI] [PubMed] [Google Scholar]
- 7.Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity (Silver Spring) 2008;16:643–53. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barone MT, Menna-Barreto L. Diabetes Res Clin Pract. 2010. Diabetes and sleep: A complex cause-and-effect relationship. [DOI] [PubMed] [Google Scholar]
- 9.Kripke DF, Langer RD, Elliott JA, Klauber MR, Rex KM. Mortality related to actigraphic long and short sleep. Sleep Med. 2011;12:28–33. doi: 10.1016/j.sleep.2010.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Akerstedt T. Psychosocial stress and impaired sleep. Scand J Work Environ Health. 2006;32:493–501. [PubMed] [Google Scholar]
- 11.Theorell T, Perski A, Akerstedt T, et al. Changes in job strain in relation to changes in physiological state. A longitudinal study. Scand J Work Environ Health. 1988;14:189–96. doi: 10.5271/sjweh.1932. [DOI] [PubMed] [Google Scholar]
- 12.Akerstedt T, Knutsson A, Westerholm P, Theorell T, Alfredsson L, Kecklund G. Sleep disturbances, work stress and work hours: a cross-sectional study. J Psychosom Res. 2002;53:741–8. doi: 10.1016/s0022-3999(02)00333-1. [DOI] [PubMed] [Google Scholar]
- 13.Akerstedt T, Fredlund P, Gillberg M, Jansson B. Work load and work hours in relation to disturbed sleep and fatigue in a large representative sample. J Psychosom Res. 2002;53:585–8. doi: 10.1016/s0022-3999(02)00447-6. [DOI] [PubMed] [Google Scholar]
- 14.Linton SJ. Does work stress predict insomnia? A prospective study. Br J Health Psychol. 2004;9:127–36. doi: 10.1348/135910704773891005. [DOI] [PubMed] [Google Scholar]
- 15.Utsugi M, Saijo Y, Yoshioka E, et al. Relationships of occupational stress to insomnia and short sleep in Japanese workers. Sleep. 2005;28:728–35. doi: 10.1093/sleep/28.6.728. [DOI] [PubMed] [Google Scholar]
- 16.Virtanen M, Ferrie JE, Gimeno D, et al. Long working hours and sleep disturbances: the Whitehall II prospective cohort study. Sleep. 2009;32:737–45. doi: 10.1093/sleep/32.6.737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rugulies R, Norborg M, Sorensen TS, Knudsen LE, Burr H. Effort-reward imbalance at work and risk of sleep disturbances. Cross-sectional and prospective results from the Danish Work Environment Cohort Study. J Psychosom Res. 2009;66:75–83. doi: 10.1016/j.jpsychores.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 18.Elovainio M, Ferrie JE, Gimeno D, et al. Organizational justice and sleeping problems: The Whitehall II study. Psychosom Med. 2009;71:334–40. doi: 10.1097/PSY.0b013e3181960665. [DOI] [PubMed] [Google Scholar]
- 19.Niedhammer I, David S, Degioanni S, et al. Workplace bullying and sleep disturbances: findings from a large scale cross-sectional survey in the French working population. Sleep. 2009;32:1211–9. doi: 10.1093/sleep/32.9.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ota A, Masue T, Yasuda N, et al. Psychosocial job characteristics and insomnia: a prospective cohort study using the Demand-Control-Support (DCS) and Effort-Reward Imbalance (ERI) job stress models. Sleep Med. 2009;10:1112–7. doi: 10.1016/j.sleep.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 21.Vahtera J, Westerlund H, Hall M, et al. Effect of retirement on sleep disturbances: the GAZEL prospective cohort study. Sleep. 2009;32:1459–66. doi: 10.1093/sleep/32.11.1459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ancoli-Israel S, Roth T. Characteristics of insomnia in the United States: results of the 1991 National Sleep Foundation Survey. I. Sleep. 1999;22(Suppl 2):S347–53. [PubMed] [Google Scholar]
- 23.Westerlund H, Alexanderson K, Akerstedt T, Magnusson Hanson L, Theorell T, Kivimaki M. Work-related sleep disturbances and sickness absence in the Swedish working population, 1993-1999. Sleep. 2008;31:1169–77. [PMC free article] [PubMed] [Google Scholar]
- 24.de Lange AH, Kompier MA, Taris TW, et al. A hard day's night: a longitudinal study on the relationships among job demands and job control, sleep quality and fatigue. J Sleep Res. 2009;18:374–83. doi: 10.1111/j.1365-2869.2009.00735.x. [DOI] [PubMed] [Google Scholar]
- 25.Magnusson Hanson LL, Theorell T, Oxenstierna G, Hyde M, Westerlund H. Demand, control and social climate as predictors of emotional exhaustion symptoms in working Swedish men and women. Scand J Public Health. 2008;36:737–43. doi: 10.1177/1403494808090164. [DOI] [PubMed] [Google Scholar]
- 26.Kecklund G, Akerstedt T. The psychometric properties of the Karolinska Sleep Questionnaire. J Sleep Res. 1992;1(Suppl 1):113. [Google Scholar]
- 27.Akerstedt T, Ingre M, Broman JE, Kecklund G. Disturbed sleep in shift workers, day workers, and insomniacs. Chronobiol Int. 2008;25:333–48. doi: 10.1080/07420520802113922. [DOI] [PubMed] [Google Scholar]
- 28.Leineweber C, Wege N, Westerlund H, Theorell T, Wahrendorf M, Siegrist J. How valid is a short measure of effort-reward imbalance at work? A replication study from Sweden. Occup Environ Med. 2010;67:526–31. doi: 10.1136/oem.2009.050930. [DOI] [PubMed] [Google Scholar]
- 29.Magnusson Hanson LL, Theorell T, Bech P, et al. Psychosocial working conditions and depressive symptoms among Swedish employees. Int Arch Occup Environ Health. 2009;82:951–60. doi: 10.1007/s00420-009-0406-9. [DOI] [PubMed] [Google Scholar]
- 30.Hu L-T, Bentler PM. Evaluating model fit. In: Hoyle RH, editor. Structural equation modeling: concepts, issues, and applications. Vol. 1995. Thousand Oaks, CA: Sage; pp. 76–99. [Google Scholar]
- 31.Kelloway EK. Using LISREL for structural equation modeling: a researcher's guide. SAGE Publications, Inc; 1998. [Google Scholar]
- 32.Steiger JH. Structural model evaluation and modification: An interval estimation approach. Multivariate Behav Res. 1990;25:173–80. doi: 10.1207/s15327906mbr2502_4. [DOI] [PubMed] [Google Scholar]
- 33.Jansson-Frojmark M, Linton SJ. The course of insomnia over one year: a longitudinal study in the general population in Sweden. Sleep. 2008;31:881–6. doi: 10.1093/sleep/31.6.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roth T, Ancoli-Israel S. Daytime consequences and correlates of insomnia in the United States: results of the 1991 National Sleep Foundation Survey. II. Sleep. 1999;22(Suppl 2):S354–8. [PubMed] [Google Scholar]
- 35.Roberts RE, Roberts CR, Chen IG. Impact of insomnia on future functioning of adolescents. J Psychosom Res. 2002;53:561–9. doi: 10.1016/s0022-3999(02)00446-4. [DOI] [PubMed] [Google Scholar]
- 36.Zapf D, Dormann C, Frese M. Longitudinal studies in organizational stress research: a review of the literature with reference to methodological issues. J Occup Health Psychol. 1996;1:145–69. doi: 10.1037//1076-8998.1.2.145. [DOI] [PubMed] [Google Scholar]
- 37.De Lange AH, Taris TW, Kompier MA, Houtman IL, Bongers PM. The relationships between work characteristics and mental health: Examining normal, reversed and reciprocal relationships in a 4-wave study. Work Stress. 2004;18:149–66. [Google Scholar]
- 38.de Lange AH, Taris TW, Kompier MA, Houtman IL, Bongers PM. Different mechanisms to explain the reversed effects of mental health on work characteristics. Scand J Work Environ Health. 2005;31:3–14. doi: 10.5271/sjweh.843. [DOI] [PubMed] [Google Scholar]
- 39.Marcelissen FH, Winnubst JA, Buunk B, de Wolff CJ. Social support and occupational stress: a causal analysis. Soc Sci Med. 1988;26:365–73. doi: 10.1016/0277-9536(88)90402-9. [DOI] [PubMed] [Google Scholar]
- 40.Leiter MP, Durup MJ. Work, home, and in-between: A longitudinal study of spillover. J Appl Behav Sci. 1996;32:29–47. [Google Scholar]
- 41.de Jonge J, Dormann C, Janssen PPM, Dollard MF, Landeweerd JA, Nijhuis FJN. Testing reciprocal relationships between job characteristics and psychological well-being: A cross-lagged structural equation model. J Occup Organ Psychol. 2001;74:29–46. [Google Scholar]
- 42.ter Doest L, de Jonge J. Testing causal models of job characteristics and employee well-being: A replication study using cross-lagged structural equation modelling. J Occup Organ Psychol. 2006;79:499–507. [Google Scholar]
- 43.Leger D, Guilleminault C, Bader G, Levy E, Paillard M. Medical and socio-professional impact of insomnia. Sleep. 2002;25:625–9. [PubMed] [Google Scholar]
- 44.Dormann C, Zapf D. Social stressors at work, irritation, and depressive symptoms: Accounting for unmeasured third variables in a multi-wave study. J Occup Organ Psychol. 2002;75:33–58. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1.
Factor loadings derived from the reciprocal models
| Latent Variable | Item | Item Content | Factor Loadings Time 1 |
|---|---|---|---|
| Demands | 1 | Enough time | 0.60, 0.59# |
| Demands | 2 | Working fast | 0.59 |
| Demands | 3 | Working intensively | 0.71 |
| Demands | 4 | Too much effort | 0.73 |
| Demands | 5 | Conflicting demands | 0.41, 0.42# |
| Decision authority | 1 | Choice in how you do your work | 0.84, 0.82# |
| Decision authority | 2 | Choice in what you do at work | 0.75, 0.77# |
| Support | 1 | Calm and pleasant atmosphere | 0.62 |
| Support | 2 | Good spirit of unity | 0.80 |
| Support | 3 | Colleagues are there for me | 0.81 |
| Support | 4 | People understand a bad day | 0.72 |
| Support | 5 | Get on well with my superiors | 0.52 |
| Support | 6 | Get on well with my colleagues | 0.76 |
| Disturbed sleep | 1 | Difficulties falling asleep | 0.66 |
| Disturbed sleep | 2 | Repeated awakenings | 0.89 |
| Disturbed sleep | 3 | Premature awakening | 0.71 |
| Disturbed sleep | 4 | Disturbed sleep | 0.81 |
| Awakening problems | 1 | Difficulties awakening | 0.59 |
| Awakening problems | 2 | Not well rested at awakening | 0.89, 0.90$ |
| Awakening problems | 3 | Exhausted at awakening | 0.81, 0.80$ |
Factor loadings derived from the reciprocal model of work characteristics in relation to awakening problems.
Factor loadings derived from the reciprocal model of awakening problems in relation to decision authority and support.
Basic LISREL model with standard solution estimates for the model including reciprocal paths between demands (D) and disturbed sleep (DS). Please observe that the time points are aligned from top to bottom of the figure. Variables ending with 1 refer to variables measured at time point 1 (2006) while variables ending with 2 refer to variables measured at time point 2 (2008). a-e denotes the specific items included in the latent variables: Da, enough time; Db, working fast; Dc, working intensively; Dd, too much effort; De, conflicting demands; DSa, difficulty falling asleep; DSb, repeated awakenings; DSc, early awakening; DSd, disturbed sleep. Sex, Gender (women vs men); Age, Age; Marit, Marital status (married/cohabiting vs single); Educ, Education; Alcoh, Alcohol consumption; Jobch, Job change between 2006 and 2008.
Basic LISREL model with standard solution estimates for the model including reciprocal paths between decision authority (DA) and disturbed sleep (DS). Please observe that the time points are aligned from top to bottom of the figure. Variables ending with 1 refer to variables measured at time point 1 (2006) while variables ending with 2 refer to variables measured at time point 2 (2008). a-d denotes the items included in the latent variables: DAa, choice in how you do your work; DAb, choice in what you do at work; DSa, difficulty falling asleep; DSb, repeated awakenings; DSc, early awakening; DSd, disturbed sleep. Sex, Gender (women vs men); Age, Age; Marit, Marital status (married/cohabiting vs single); Educ, Education; Alcoh, Alcohol consumption; Jobch, Job change between 2006 and 2008.
Basic LISREL model with standard solution estimates for the model including reciprocal paths between social support (S) and disturbed sleep (DS). Please observe that the time points are aligned from top to bottom of the figure. Variables ending with 1 refer to variables measured at time point 1 (2006) while variables ending with 2 refer to variables measured at time point 2 (2008). a-f denotes the items included in the latent variables: Sa, calm and pleasant atmosphere; Sb, good spirit of unity; Sc, colleagues are there for me; Sd, people understand a bad day; Se, get on well with my superiors; Sf, get on well with my colleagues; DSa, difficulty falling asleep; DSb, repeated awakenings; DSc, early awakening; DSd, disturbed sleep. Sex, Gender (women vs men); Age, Age; Marit, Marital status (married/cohabiting vs single); Educ, Education; Alcoh, Alcohol consumption; Jobch, Job change between 2006 and 2008.
Basic LISREL model with standard solution estimates for the model including reciprocal paths between demands (D) and awakening problems (AP). Please observe that the time points are aligned from top to bottom of the figure. Variables ending with 1 refer to variables measured at time point 1 (2006) while variables ending with 2 refer to variables measured at time point 2 (2008). a-e denotes the specific items included in the latent variables: Da, enough time; Db, working fast; Dc, working intensively; Dd, too much effort; De, conflicting demands; APa, difficulty awakening; APb, not well-rested; APc, exhausted at awakening. Sex, Gender (women vs men); Age, Age; Marit, Marital status (married/cohabiting vs single); Educ, Education; Alcoh, Alcohol consumption; Jobch, Job change between 2006 and 2008.
Basic LISREL model with standard solution estimates for the model including reciprocal paths between decision authority (DA) and awakening problems (AP). Please observe that the time points are aligned from top to bottom of the figure. Variables ending with 1 refer to variables measured at time point 1 (2006) while variables ending with 2 refer to variables measured at time point 2 (2008). a-d denotes the items included in the latent variables: DAa, choice in how you do your work; DAb, choice in what you do at work; APa, difficulty awakening; APb, not well-rested; APc, exhausted at awakening. Sex, Gender (women vs men); Age, Age; Marit, Marital status (married/cohabiting vs single); Educ, Education; Alcoh, Alcohol consumption; Jobch, Job change between 2006 and 2008.
Basic LISREL model with standard solution estimates for the model including reciprocal paths between social support (S) and awakening problems (AP). Please observe that the time points are aligned from top to bottom of the figure. Variables ending with 1 refer to variables measured at time point 1 (2006) while variables ending with 2 refer to variables measured at time point 2 (2008). a-f denotes the items included in the latent variables: Sa, calm and pleasant atmosphere; Sb, good spirit of unity; Sc, colleagues are there for me; Sd, people understand a bad day; Se, get on well with my superiors; Sf, get on well with my colleagues; APa, difficulty awakening; APb, not well-rested; APc, exhausted at awakening. Sex, Gender (women vs men); Age, Age; Marit, Marital status (married/cohabiting vs single); Educ, Education; Alcoh, Alcohol consumption; Jobch, Job change between 2006 and 2008.