Abstract
Objective
To identify characteristics that predict resolution of placenta previa and to develop a clinical model for likelihood of resolution.
Methods
We conducted a retrospective study of 366 singleton pregnancies complicated by placenta previa diagnosed with resolution of the previa as the primary outcome. Regression analyses were performed to determine variables associated with resolution, and optimal timing for repeat sonographic evaluation. A likelihood of resolution model was created using a parametric survival model with Weibull hazard function.
Results
Of the 366 cases, 84% of complete placenta previas and 98% of marginal placenta previas resolved at a mean gestational age of 28.6 ±5.3 weeks. Only gestational age and distance from the internal cervical os at the time of diagnosis were significantly associated with resolution (p<0.01). Likelihood of resolution was not significantly associated with any other variables.
Conclusion
Only gestational age and distance from the internal os at time of diagnosis predict likelihood of resolution of placenta previa. Marginal previas diagnosed in the 2nd trimester do not appear to warrant repeat ultrasound evaluation for resolution.
Keywords: Placenta previa, marginal previa, bleeding, pregnancy, resolution
INTRODUCTION
While placenta previa was classically diagnosed when a patient presented with painless third trimester bleeding, asymptomatic placenta previas are now diagnosed more frequently since the advent of routine second trimester ultrasonography, with a reported incidence of 1–15%.1–4 At present, there is no consensus regarding guidelines for timing and frequency of ultrasound surveillance of incidentally diagnosed, asymptomatic previas. This creates the potential for unnecessary ultrasound examinations, with associated cost and patient inconvenience.
Established risk factors for placenta previa include advanced maternal age, multiparity, and history of prior cesarean delivery or other full thickness uterine incision.5,6 Although existing literature indicates a high resolution rate for placenta previas diagnosed early in pregnancy, there is limited data on factors associated with this phenomenon. 4, 7–9
Therefore, our primary objective was to identify clinical and sonographic characteristics associated with resolution of placenta previa. Our secondary objective was to develop a clinically applicable likelihood of resolution model based on those variables significantly associated with resolution.
METHODS
A retrospective cohort analysis of all obstetric ultrasound examinations at the University of North Carolina (UNC) Hospitals between December 2003 and December 2007 was completed. We included all singleton pregnancies complicated by placenta previa diagnosed after 14 weeks and with follow up surveillance data available for analysis. Resolution of previa was defined as a follow-up ultrasound demonstrating that the leading edge of the placenta was ≥20 mm away from the internal os; in the absence of ultrasound data, successful vaginal delivery was used as a surrogate marker. Patients without follow-up ultrasound who were delivered via cesarean were excluded from our analysis. We further excluded cases of placenta accreta, percreta, and multifetal pregnancy, as no study has described previa resolution patterns as they relate to these diagnoses. 10 This study was approved by the Institutional Review Board at the University of North Carolina at Chapel Hill prior to data collection.
All ultrasound examinations were performed by registered diagnostic medical sonographers (RDMS) in the UNC Prenatal Diagnosis Center using ATL Ultramark 5000 (National Ultrasound, Duluth, GA), GE Voluson Expert or GE Voluson E8 (GE Healthcare, Milwaukee, WI) ultrasound machines. Per institutional protocol, the distance of the leading placental edge either away from or over the internal cervical os was measured first by a 4–7 MHz curvilinear transabdominal probe and later confirmed by a 5–9 MHz endovaginal probe, if transabdominal visualization was considered limited. The time interval between ultrasound during which placenta previa was initially diagnosed and subsequent follow-up ultrasound was based on the discretion of either the attending physician interpreting the initial ultrasound or the patient’s primary obstetric provider, or as deemed necessary by a change in clinical status (i.e., symptomatic placenta previas). Ultrasound examinations were interpreted by board certified or board eligible maternal fetal medicine physicians.
Sonographic variables of interest included gestational age at diagnosis, type of previa (“marginal,” defined as the leading edge of the placenta being 0–20 mm away from the internal cervical os, or “complete,” defined as the leading edge of the placenta overlapping the internal cervical os), placental location (on either the anterior or posterior wall), and absolute distance away from or over the internal cervical os (in mm). For our statistical analysis and the creation of Figure 1, the distance from the leading edge of the placenta to the internal cervical os was measured in mm and described as positive values when located over the os, and in negative values when located away from the os. When available, delivery data was recorded, including gestational age at delivery, mode of delivery, and indication for cesarean, when applicable. Maternal demographic data were abstracted from the paper and electronic medical records by the investigators using a standard data collection sheet. Gestational age (GA) was based on last menstrual period (LMP). Per our institutional protocol, in cases of uncertain LMP or where there was a > 8% discordance between menstrual and ultrasound dating, ultrasound dating alone was used.
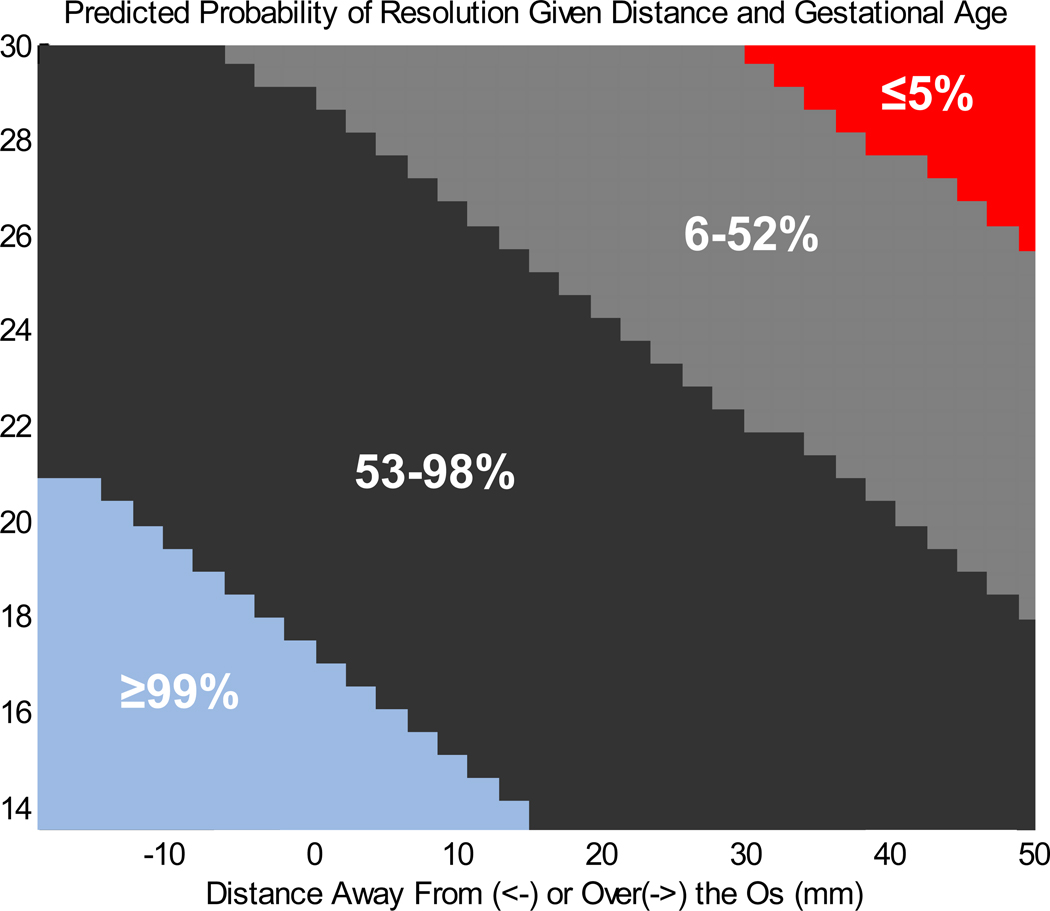
FIGURE 1. Likelihood of Resolution Modeling.
Predicted probability of resolution given distance from os and gestational age at diagnosis
X axis represents the distance away from or over the internal cervical os (point 0) in mm. Negative numbers represent distance away from the os, and positive numbers represent distance over the os.
Y axis represents gestational age in weeks at time of scan.
Statistical analyses were performed using SAS 8.01 (SAS Institute, Cary, NC). Cases were initially separated into two study groups, resolved and unresolved placenta previas. Maternal demographics and ultrasound characteristics were then compared between these groups using Fisher exact test for categorical variables and Wilcoxon rank sum for continuous variables. Stepwise variable selection was used to arrive at a final logistic regression model, through which we estimated the probability of resolution conditional on both gestational age at given scan and distance away from or over the internal os. Finally, a model for time to resolution of a given placenta previa was created using a parametric survival model with a Weibull hazard function. 12
RESULTS
During the study period, 23,971 ultrasound examinations were performed during the second trimester, of which 670 (2.8%) diagnosed a placenta previa. Of these, 304 were excluded as multiple gestations (n=46), placenta accreta or percreta (n=12), or because no resolution data was available (n=246). Maternal demographics of the 366 included patients are presented in Table 1 and did not differ between the two study groups.
TABLE 1.
Maternal demographic characteristics of the two study groups
| Resolved previa N=324 |
Unresolved previa N=42 |
p value | |
|---|---|---|---|
| Age (year) | 31.83 (±5.75) | 32.98 (±5.30) | 0.22 |
| Race Caucasian Non-caucasian |
166 (51) 158 (49) |
24 (57) 18 (43) |
0.51 |
| Multigravity | 290 (90) | 34 (81) | 0.12 |
| Multiparity | 310 (96) | 38 (90) | 0.14 |
| Prior cesarean | 215 (84) | 28 (80) | 0.63 |
Data presented at number (percentage) with standard deviation where available; Fisher’s exact test used for analysis of categorical variables, Student T-test and Wilcoxon rank sum used for analysis of group means
The cases included 67% complete and 33% marginal previas. Of these, 35% were anterior and 65% were posterior in location. The mean gestational age at first scan was 18.6 ±3.4 weeks. The median distance over the internal cervical os at first ultrasound examination was 10 mm (range, −19 to +85 mm) and a median of 2 ultrasound examinations were performed for each patient (range, 1 – 5).
As presented in Table 2, greater than 80% (203/243) of complete placenta previas and 98% (121/123) of marginal placenta previas ultimately resolved. The two marginal placenta previas that did not resolve were both diagnosed in the early third trimester. Anterior and posterior placenta previas resolved with comparable frequency. Of the patients for whom resolution of placenta previa was confirmed sonographically, the mean gestational age at documented resolution was 28 4/7 weeks; 90% of placenta previas had resolved by 34 4/7 weeks gestation.
TABLE 2.
Ultrasound characteristics of the two study groups
| Resolved previa N=324 |
Unresolved previa N=42 |
p value | |
|---|---|---|---|
| Type of previa Complete Marginal |
203 (63) 121 (37) |
40 (95) 2 (5) |
<0.01 |
| Placental location Anterior Posterior |
116 (36) 208 (64) |
14 (33) 28 (67) |
0.86 |
| Distance from os (mm) | 7.7 (±15.0) | 26.7 (±5.9) | <0.01 |
| Gestational age at diagnosis (weeks) | 17.9 (±2.3) | 22.9 (±5.9) | <0.01 |
Data presented at number (percentage) with standard deviation where available; Fisher’s exact test used for analysis of categorical variables, Student T-test and Wilcoxon rank sum used for analysis of group means
Using logistic regression analysis to control for each of our demographic and clinical variables, we found that the likelihood of resolution was not impacted by maternal age, gravidity, parity, history of a prior cesarean section, nor placental location on either the anterior or posterior uterine walls.
Figure 1 depicts our likelihood of resolution model created using a parametric survival model with a Weibull hazard function. Zone 1 represents the combination of gestational age and distance away from or over the os where the probability of spontaneous resolution of a placenta previa is greater than or equal to 99%. Zone 4 represents the combination of gestational age and distance over the internal cervical os where the probability of resolution is less than 5%. Zones 2 and 3 represent the combination of gestational age and distance over the os where the probability of resolution is 53–99% and 6–52%, respectively.
DISCUSSION
The lack of consensus on guidelines for the sonographic management of incidentally diagnosed placenta previa has the potential to result in unnecessary ultrasound examinations with an associated cost burden to patients and the healthcare system at large. Our results demonstrate that greater than 98% of marginal placenta previas resolved, with complete resolution of those diagnosed in the second trrimester. This is consistent with the work of Ghourab et al, 7 as well as Dasche et al, who conducted a retrospective studies reporting that the later in gestation a placenta previa is diagnosed, the higher the likelihood of persistence, and that marginal placenta previas resolve more frequently than complete placenta previas.8 Furthermore, our data suggest that only gestational age and distance from the internal os at time of diagnosis are significantly associated with resolution of early diagnosed placenta previas, consistent with the findings of Lauria et al in 1996.4 Maternal age, race, parity, history of cesarean section, and location of the placenta on the uterine wall (anterior or posterior) are not associated with likelihood of resolution.
Our negative findings regarding history of cesarean delivery and location on placental wall contradict the previous findings of smaller studies. In 2005, Laughon et al performed a case control study and reported that although a history of cesarean section did not increase the odds for detecting a previa on second trimester ultrasound, a history of cesarean was associated with a three fold increased risk of placenta previa at term, reflecting decreased rates of resolution with advancing gestation.9 Finally, Cho et al performed a prospective observational study of 98 patients and found a trend toward higher rates of resolution for anterior previas. 10
While smaller studies have reported likelihood of previa persistence based on a fixed gestational age and distance over the os, 4,7 the strength of our study is that our large cohort allowed for the creation of a counseling tool, Figure 1, through which a provider can give patients a likelihood range for resolution based on their specific gestational age at diagnosis and distance of the leading placental edge over or away from the internal os. This likelihood of resolution data can also be used to decide if and when repeat ultrasonography should be performed.
From a public health standpoint, clinical use of this model has the potential to significantly decrease the number of repeat ultrasounds for patients diagnosed with a placenta previa. Based on our likelihood of resolution model, it appears that consideration could be given to deferring repeat ultrasound for patients diagnosed with a marginal previa in the second trimester or patients with complete previas overlapping the internal cervical os by 50 mm or more at or beyond 26 weeks. However, numbers in the latter subset of our study are relatively small and prospective or retrospective confirmation in a larger study is warranted. Balancing our finding of 90% resolution at 34 4/7 weeks with the clinical practice of cesarean delivery by 36–37 weeks for persistent placenta previas and the potential stress to parturients of prolonged pelvic rest, we suggest considering delaying repeat ultrasound to evaluate for resolution of zone 2 and 3 placenta previas in an asymptomatic patient until 30–32 weeks. Finally, in our cohort, 100 patients received 111 repeat ultrasounds during the study period for either marginal placenta previas in the second trimester or for complete placenta previas 50 mm or more over the os at 26 weeks or later (zones 1 and 4, respectively). Based on our institutional charges for limited repeat ultrasound, this practice cost our patients more than $57,000 during the study period. If we had not performed repeat scans, this would represent a savings of more than $500 per affected patient.
Our findings must be interpreted within the context of the study design. Because of the retrospective design, there were potential confounders for which we could not account (i.e., smoking, history of curettage or other uterine surgery). Similarly, although history of cesarean section was not found to be associated with persistence of placenta previa, we were not able to evaluate type of uterine incision. Therefore, it is possible that classical incisions evaluated independently could have a stronger relationship with persistence. Finally, there was a large subset of patients who received initial diagnostic ultrasound and for whom resolution data was not available, and who were therefore excluded from our analysis (n=246). Our institution is a large referral center and provides ultrasound services for multiple health departments, whose patients frequently deliver at outside facilities. Therefore, while we hypothesize that resolution in these excluded cases would mirror that in the included cohort, it is possible that this subset of patients included those who experienced large bleeds and delivered emergently at outside facilities, and that their inclusion may have impacted our likelihood of resolution model.
The findings of this study may be of clinical value to providers when deciding if and when to reimage asymptomatic placenta previa incidentally diagnosed during routine second trimester ultrasound, potentially decreasing the significant financial burden of unnecessary repeat ultrasounds. Prospective studies are needed to confirm the safety of such a practice change.
Footnotes
Presentation: 30th Annual Meeting of the Society for Maternal-Fetal Medicine, Chicago, IL (February 2010)
REFERENCES
- 1.Rosati P, Guariglia L. Clinical significance of placenta previa detected at early routine transvaginal scan. J Ultrasound Med. 2000;19:581–585. doi: 10.7863/jum.2000.19.8.581. [DOI] [PubMed] [Google Scholar]
- 2.Zelop CC, Bromley B, Frigoletto FD, Jr, Benacerraf BR. Second trimester sonographically diagnosed placenta previa: prediction of persistent previa at birth. Int J Gyneacol Obstet. 1994;44:207–210. doi: 10.1016/0020-7292(94)90167-8. [DOI] [PubMed] [Google Scholar]
- 3.Rizos N, Doran TA, Miskin M, Benzie RJ, Ford JA. Natural history of placenta previa ascertained by diagnostic ultrasound. Am J Obstet Gynecol. 1979;133:287–291. doi: 10.1016/0002-9378(79)90680-x. [DOI] [PubMed] [Google Scholar]
- 4.Lauria MR, Smith RS, Treadwell MC, Comstock CH, Kirk JS, Lee W, Bottoms SF. The use of second-trimester transvaginal sonography to predict placenta previa. Ultrasound Obstet Gynecol. 1996;8:337–340. doi: 10.1046/j.1469-0705.1996.08050337.x. [DOI] [PubMed] [Google Scholar]
- 5.Miller DA, Chollet JA, Goodwin TM. Clinical risk factors for placenta previa-placenta accreta. Am J Obstet Gynecol. 1997;177:210–214. doi: 10.1016/s0002-9378(97)70463-0. [DOI] [PubMed] [Google Scholar]
- 6.Zhang J, Savitz DA. Maternal age and placenta previa: a population-based, case-control study. Am J Obstet Gynecol. 1993;168:641–645. doi: 10.1016/0002-9378(93)90511-g. [DOI] [PubMed] [Google Scholar]
- 7.Ghourab S, Al-Jabari A. Placental migration and mode of delivery in placenta previa: transvaginal sonographic assessment during the third trimester. Ann Saudi Med. 2000;20:382–385. doi: 10.5144/0256-4947.2000.382. [DOI] [PubMed] [Google Scholar]
- 8.Dashe JS, McIntire DD, Ramus RM, Santos-Ramos R, Twickler DM. Persistence of placenta previa according to gestational age at ultrasound detection. Obstet Gynecol. 2002;99:692–697. doi: 10.1016/s0029-7844(02)01935-x. [DOI] [PubMed] [Google Scholar]
- 9.Laughon SK, Wolfe HM, Visco AG. Prior cesarean and the risk for placenta previa on second-trimester ultrasonography. Obestet Gynecol. 2005;105:962–965. doi: 10.1097/01.AOG.0000158114.47925.fa. [DOI] [PubMed] [Google Scholar]
- 10.Cho JY, Lee YH, Moon MH, Lee JH. Difference in migration of placenta according to the location and type of placenta previa. J Clin Ultrasound. 2008;36:79–84. doi: 10.1002/jcu.20427. [DOI] [PubMed] [Google Scholar]
- 11.Ananth CV, Demissie K, Smulian JC, Vintzileos AM. Placenta previa in singleton and twin births in the United States, 1989 through 1998: a comparison of risk factor profiles and associated conditions. Am J Obstet Gynecol. 2003;188(1):275–281. doi: 10.1067/mob.2003.10. [DOI] [PubMed] [Google Scholar]
- 12.Cox C, Chu H, Schneider MF, Muñoz A. Parametric survival analysis and taxonomy of hazard functions for the generalized gamma distribution. Stat Med. 2007;26:4352–4374. doi: 10.1002/sim.2836. [DOI] [PubMed] [Google Scholar]