Abstract
New genetic tests reveal risks for multiple conditions simultaneously, although little is understood about the psychological factors that affect testing uptake. We assessed a conceptual model called the Multiplex Genetic Testing Model (MGTM) using structural equation modeling (SEM). The MGTM delineates worry, perceived severity, perceived risk, response efficacy and attitudes toward testing as predictors of intentions and behavior. Participants were 270 healthy insured adults age 25–40 from the Multiplex Initiative conducted within a health care system in Detroit MI, USA. Participants were offered a genetic test that assessed risk for eight common health conditions. Confirmatory factor analysis revealed that worry, perceived risk and severity clustered into two disease domains: cancer or metabolic conditions. Only perceived severity of metabolic conditions was correlated with general response efficacy (β=0.13, p<0.05), which predicted general attitudes toward testing (β=0.24, p<0.01). Consistent with our hypothesized model, attitudes towards testing were the strongest predictors of intentions to undergo testing (β=0.49, p<0.01), which in turn predicted testing uptake (OR 17.7, β=0.97, p<0.01). The MGTM explained a striking 48% of the variance in intentions and 94% of the variation in uptake. These findings support use of the MGTM to explain psychological predictors of testing for multiple health conditions.
Keywords: Genetic testing, Multiplex Initiative, health behavior, common disease, structural equation modeling, personalized medicine, U.S.A.
INTRODUCTION
As genetic technologies have advanced, it has become possible to detect an increasing number of genetic variants simultaneously, an approach known as multiplex testing (LaFramboise, 2009). This approach has broadened the use of genetic testing beyond rare single-gene disorders to facilitate testing for common health conditions (e.g., type 2 diabetes and cardiovascular disease) (Panoutsopoulou & Zeggini, 2009). Currently, multiplex testing is available online directly to consumers (Hogarth, Javitt, & Melzer, 2008; McBride, Wade, & Kaphingst, 2010). Because common conditions have a high prevalence and broad public health effects, multiplex testing soon may be integrated into primary prevention interventions and general medical care (Avard & Knoppers, 2009). Yet multiplex testing differs from traditional genetic testing in several important ways: the nature and complexity of the resulting genetic risk information, the scope of diseases involved, and the ways in which it is offered and accessed. Given these distinctions, it is important to understand how individuals consider testing and how their cognitive and affective perceptions influence their decisions whether to undergo multiplex genetic susceptibility testing (Cameron & Muller, 2009; McBride et al., 2008;Gooding, Organista, Burack, & Biesecker, 2006). Research findings may inform clinical interactions and ultimately be used to study interventions aimed at enhancing informed choice (Michie, Dormandy, & Marteau, 2002). While studies have previously examined uptake of genetic testing, these have generally focused on single-gene or single disease tests and have been largely atheoretical in design (Marteau & Croyle, 1998, Marteau & Lerman 2001).
Some researchers have begun to address the need for theory-based evidence by examining genetic testing decisions using variables from established health behavior theories (e.g. the Theory of Planned Behavior (TPB), Protection Motivation Theory (PMT) and the Health Belief Model (HBM) (Ajzen, 1991; Rogers & Prentice-Dunn; Janz et al., 2002)). Among studies exploring variables from the TBP, attitudes were found to be important in the process of making a testing decision and the forming of intentions (Dormandy et al., 2006; Lakeman et al., 2009; Nordin et al., 2004), as well as in the actual uptake of testing (Dormandy et al., 2006). Measures of perceived risk and worry (from the HBM and PMT), and response efficacy (from the PMT), have significantly, but not completely, predicted intentions to undergo genetic susceptibility testing for breast cancer risk (Helmes, 2002). Similarly, perceived risk, perceived severity, and worry about breast cancer (from the HBM and PMT) have been shown to predict genetic testing behaviors, although to a limited degree (Cameron & Diefenbach, 2001, Cameron & Reeve, 2006).
In light of these findings, it has been recommended that future research develop and test expanded conceptual models based on variables from key health behavior theories that have been previously used to explain genetic testing decisions (T.M. Marteau, NIH NHGRI Symposium, 2008). These expanded models may offer: a) a better understanding of the relationships among relevant variables; b) stronger predictions of uptake of genetic testing; and c) explain more of the variance in testing decisions. The following investigation aims to test the combined effects of established variables in the context of multiplex genetic testing.
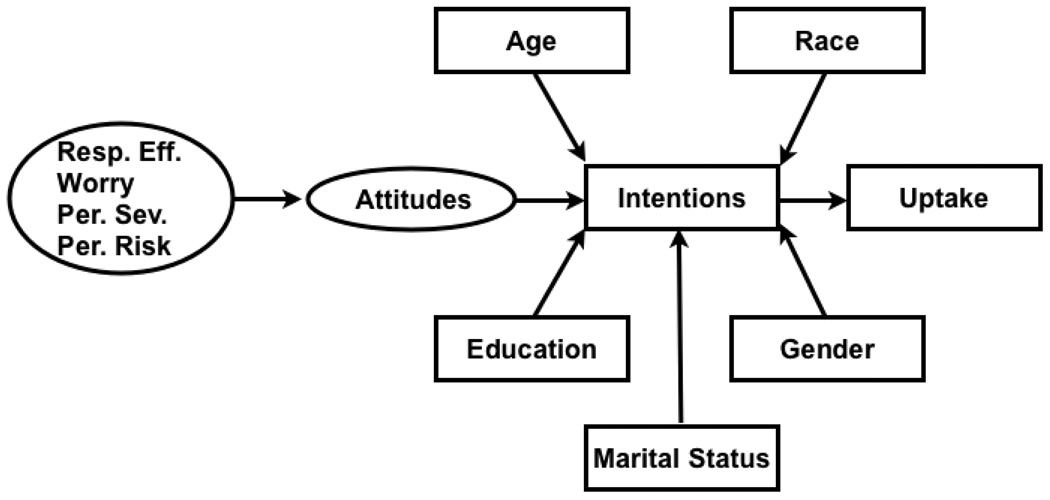
This study analyzes data collected from a subgroup of participants in the Multiplex Initiative, wherein participants were offered a multiplex genetic test for eight different health conditions. While theoretical health behavior research to date has been concerned with behavior aimed at avoiding a single health threat, the Multiplex Initiative provided an unusual opportunity to study uptake of a test that assessed risk for eight conditions simultaneously. The conceptual model tested in our study (see Figure 1), the Multiplex Genetic Testing Model (MGTM) included: worry, perceived severity, perceived risk, response efficacy, attitudes towards multiplex testing, intentions to undergo testing and test uptake. Based on assertions from the parent theories, our hypothesized model predicts that attitudes and intentions will mediate the effects of worry, perceived seriousness, perceived risk, and response efficacy on testing uptake.
Figure 1.
Proposed Multiplex Genetic Testing Model. Arrows indicate paths of influence, ovals indicate constructs, and boxes indicate measured variables.
We used SEM to analyze the relationships among the psychological constructs and to test their effect on intentions and on the primary dependent variable, test uptake. Measuring each of the constructs in the model with eight items, one for each of the diseases included in Multiplex test, enabled the evaluation of the validity of the constructs. We hypothesized that participants’ perceptions about each of the eight conditions would group together as single domains. This was based on previously reported findings showing that perceived risk across several diseases was associated with perceived risk for a specific disease (DiLorenzo, et al 2006; Gerend, 2004), and that worry about a specific disease generalized to other similar diseases (DiLorenzo et al., 2006; Schnur, et al., 2006).
The ability of the MGTM to predict uptake of multiplex testing for susceptibility across several common health conditions would suggest that it comprises a higher-order model for this health behavior. Thus, using model testing, we address theory development alongside the identification of psychological correlates to testing uptake.
METHODS
Recruitment
Participants in this study comprise a subset of those enrolled in a parent project, the Multiplex Initiative (McBride et al., 2008; McBride et al., 2009). The goals, procedures, and structure of the Multiplex Initiative are described elsewhere (Alford et al., 2010; McBride et al., 2008; McBride et al., 2009). In brief, the Multiplex Initiative was designed to examine the uptake and impact of multiplex (multi-gene) genetic testing for eight common health conditions (Wade, McBride, Kardia, & Brody, 2009). This was a collaborative effort among the National Human Genome Research Institute (Bethesda, MD), the Group Health Cooperative (Seattle, WA), and the Henry Ford Health System (Detroit, MI). The participants were recruited from a sample of 350,000 members of the Henry Ford Health System. Enrollment required that participants be 25–40 years old, self-identified as white or African American, and not affected with type 2 diabetes, atherosclerotic cardiovascular disease, osteoporosis, or cancer.
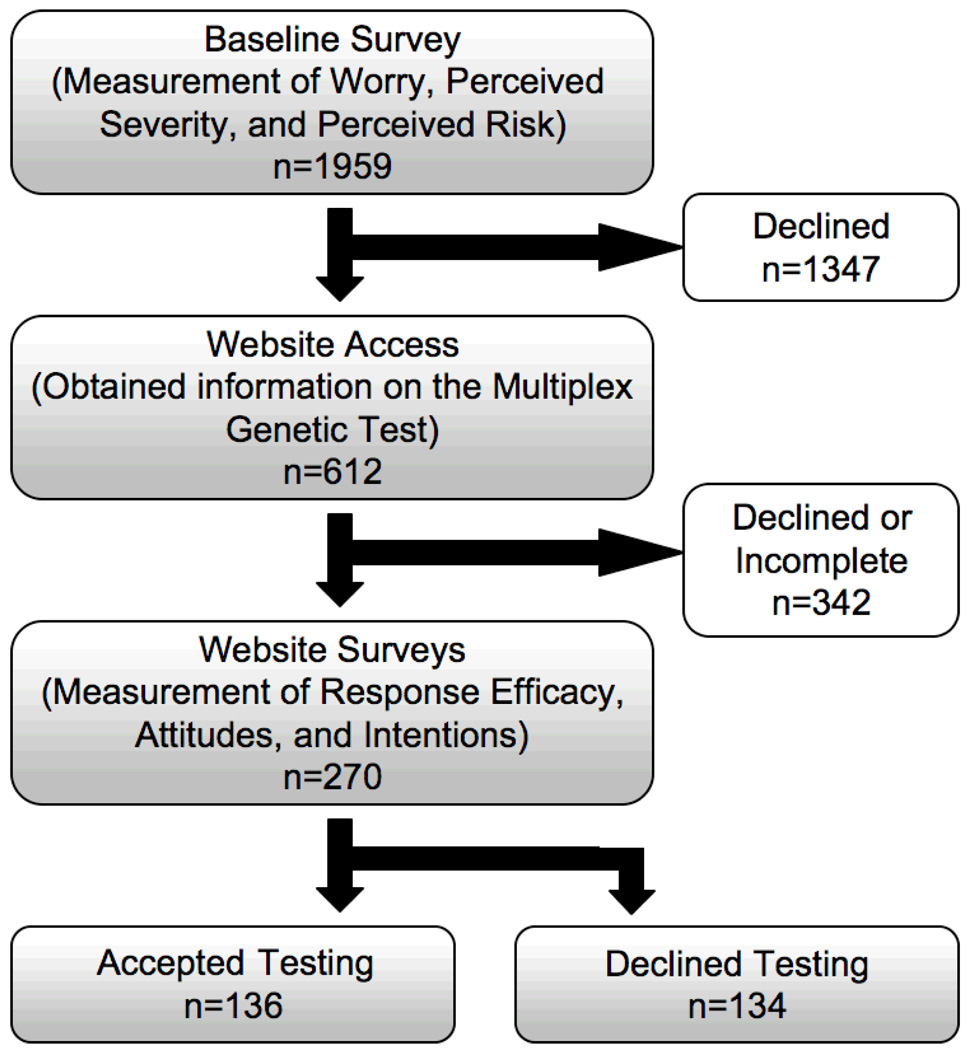
Multiplex participants within the Henry Ford Health Care System were recruited by telephone. Participants completed a baseline survey of demographics, family history of diseases, and perspectives on health (see Figure 2). They were sent a brochure introducing the multiplex genetic test and referred to the Multiplex Initiative website. Interested participants could access the website to learn more about testing. The information available included what testing would and would not mean, and the health conditions and associated genes tested (Kaphingst et al., 2010). The test assessed 15 genetic variants that contributed to the risk for eight health conditions: heart disease, hypercholesterolemia, high blood pressure, type 2 diabetes, osteoporosis, colorectal cancer, lung cancer, and skin cancer (Wade et al., 2009). On the website, participants were asked whether they were interested in taking the multiplex genetic test. Regardless of their response, they were then asked to complete a number of additional surveys, including the ancillary survey particular to this study for which they were offered a $20.00 financial incentive. Those who expressed interest in multiplex genetic testing were invited to schedule a visit to a Henry Ford Health System clinic to discuss the test with a research educator to decide whether to undergo testing. An appointment to meet with an educator could be made at the end of completing the web-based survey. The vast majority of participants who underwent testing followed this protocol, although it was possible for participants to schedule an appointment later as long as it was within the 200 days window that the study was open. Uptake was recorded at the time blood was drawn for testing. Following a multiplex genetic analysis, participants received mailed results informing them of their risk status. A research educator contacted participants to discuss their test results, and a follow-up survey was conducted three months later. This analysis focused on the subset of Multiplex Initiative participants (n=270) who completed all relevant questions on the baseline telephone survey and the ancillary study surveys found on the Multiplex Initiative website.
Figure 2.
Flow diagram of participant recruitment and data collection for this ancillary study of the Multiplex Initiative.
Model
The expanded conceptual model that was tested, the Multiplex Genetic Testing Model, is diagramed in Figure 1. The relationships of the variables parallel their relationships in their theories of origin. SEM assesses whether the relationships exist as we have hypothesized in the model.
Measures
The measures used in this analysis are summarized below. The psychometric data for the measures will be reported within the measurement model data presented in the Results section.
Baseline measures
Socio-demographic characteristics
Gender and age were obtained from the Henry Ford Health System electronic health record. Age was treated as a continuous variable. The race of participants, marital status, and educational level were obtained from the baseline survey (Alford et al., 2010).
Perceived risk
Perceived risk of a disease measured the perceived lifetime likelihood of developing each of the eight health conditions. The text of the question was: “On a scale from 1 to 7, where 1 is certain not to happen and 7 is certain to happen, what do you think your chance is of getting the following conditions in your lifetime?” (Asked for each condition).
Perceived seriousness
Perceived seriousness of the disease was assessed for each of the eight health conditions. The text of the question was: “On a scale from 1 to 7, where 1 is not at all serious and 7 is very serious, how serious do you think it is to have the following diseases?” (Asked for each condition).
Worry
Participant worry was assessed individually for each of the eight health conditions. The text of the question was: “On a scale from 1 to 7, where 1 is not at all worried and 7 is very worried, how worried are you about getting the following conditions in your lifetime?” (Asked for each condition).
Multiplex Initiative Web-based Measures
Intentions
Intentions were assessed using one question: “Are you interested in taking the genetic test?” Three responses were offered: “Yes,” “No,” and ”Maybe,” chosen by 50%, 29%, and 21% of the participants respectively.
Ancillary Study Web-based Measures
Response efficacy
Response efficacy was assessed using a series of statements about whether multiplex testing can reduce participants' chances of acquiring each of the eight health conditions and common disease in general. The text of the question was: “Multiplex testing can help reduce my chances of getting (each condition)” (1- strongly disagree to 5 -strongly agree).
Attitudes toward multiplex testing
Attitudes were assessed using a semantic differential scale of four items based on values and beliefs about multiplex genetic testing (e.g., harmful vs. not harmful, beneficial vs. not beneficial) using a 7-point scale. The text of the question was: “For me, having genetic testing for (each disease name) would be:” (A good thing to Not a good thing, and A bad thing to Not a bad thing). An attitude score on testing for each condition was obtained by reverse scoring one answer and averaging responses. Higher scores represent more positive attitudes towards undergoing multiplex testing.
Outcome Measure at Clinic Visit
Test Uptake
Test choice was the primary dependent variable. Appointments were made with participants who expressed interest in undergoing testing. During the clinic visit, participants could obtain further information about testing, undergo a testing consent process and have a blood sample drawn for testing. Uptake was defined as having completed the blood draw.
Data Analysis
A two-step structural equation model (SEM) analysis was applied to assess whether the data supported our hypothesized model (Figure 1). The first step used a confirmatory factor analysis to establish a measurement model that defines latent model constructs (e.g. worry, perceived severity, perceived risk, attitudes and response efficacy) in terms of the associated observed survey items. Using latent constructs allows for the assessment of the measurement error associated with each construct and the measurement model analysis provides a number of diagnostics to evaluate the validity of the constructs. Once an adequate fit for the measurement model was established, the structural model was assessed in a second step that related the latent constructs and linked them to testing intentions and test uptake.
The measurement models were fit using AMOS™ 16 (Arbuckle, 2007). The binary nature of the variables for intention and test uptake required a more general modeling algorithm (Skrondal & Rabe-Hesketh, 2005) than was available in AMOS™ 16, so Mplus version 4.1 was used to fit the structural model (Muthén & Muthén, 1998–2007).
The measurement model was assessed using several measures including the chi-square goodness of fit statistic and, due to the sensitivity of this statistic to sample size, the comparative fit index (CFI) and the root mean square error of approximation (RMSEA). Additional diagnostics of the fit included the communalities of the manifest variables with the constructs, the convergent validity (factor loadings, variance extracted and construct reliability), discriminant validity and the modification indices. When an adequate fit, consistent with theoretical considerations, was established for the measurement model, the structural model was developed. Due to the mixed nature of the variables used in the structural model, the adequacy of the fit was determined using the Akaike Information Criterion (AIC) and sample-size adjusted Bayesian Information Criterion (BIC).
Sample Population
A total of 1959 participants completed the baseline questionnaire in the Multiplex Initiative parent study. About a third (n=612) of the enrolled participants accessed the Multiplex Initiative website to obtain more information about the multiplex genetic test (McBride et al., 2009). Of these, 270 declared their intentions to be tested and completed our ancillary survey.
The 270 participants were 52% female, and 53% self-identified as African American or “Other.” Forty-eight percent of participants completed college, while the rest attended some college (33%) or completed high school (19%). The age of participants was skewed towards the higher end of the range (35 years on average, SE 0.25), and 63% were members of a married or unmarried couple. Fifty-two percent of participants expressed an intention to undergo multiplex genetic testing, and 50% ultimately chose to be tested. The characteristics of these participants did not differ significantly from the 612 participants who accessed the website in the parent Multiplex Initiative. Our sample had slightly higher intentions to undergo multiplex testing and slightly more had testing than the larger sample of those who accessed the website (612). See Table 1.
Table 1.
Study Demographic Information
| Completed Baseline Survey |
Visited Website |
Completed Ancillary Study Survey |
|
|---|---|---|---|
| (n=1959) | (n=612) | (n=270) | |
| Age (mean) | 35 | 35 | 35 |
| Gender | |||
| Male | 47% | 44% | 47% |
| Female | 53% | 56% | 52% |
| Race | |||
| White | 37% | 48% | 47% |
| Black and Other | 63% | 52% | 53% |
| Education | |||
| ≤12th Grade | 25% | 18% | 19% |
| Some college | 38% | 35% | 33% |
| ≥Graduated college | 37% | 46% | 48% |
| Marital Status | |||
| Married or partnered | 63% | 64% | 63% |
| Other | 37% | 36% | 37% |
| Genetic Test Intentions (Yes) | 14% | 45% | 52%* |
| Genetic Test Uptake (Yes) | 14% | 43% | 50%* |
P-value < 0.5 for a one-sample t-test comparison of means between participants who visited the website and means for those who completed the ancillary study surveys.
RESULTS
The SEM set out to assess the MGTM using a measurement model followed by a structural model (Bollen, 1989).
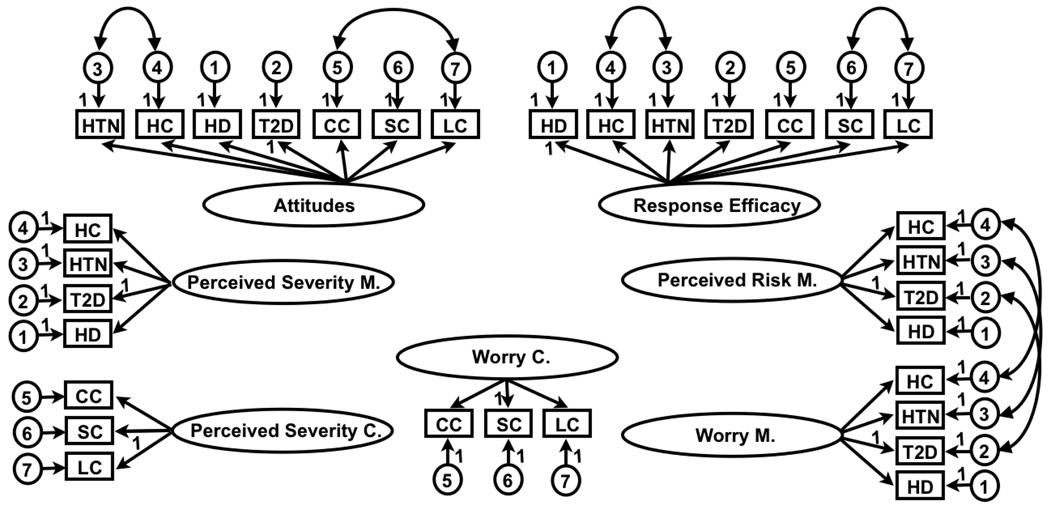
Measurement Model
A confirmatory factor analysis (CFA) was conducted for the SEM measurement model associated with the latent constructs in the MGTM: worry, perceived risk, perceived seriousness, response efficacy and attitudes (see Fig. 1). Each of the constructs was initially associated with the eight questionnaire items (representing the conditions) used to measure the construct. For the purposes of analysis, we postulated that all the latent constructs were correlated. The initial measurement model indicated problems with the fit for the constructs representing worry, perceived risk and perceived severity and suggested that these latent constructs were better represented by two constructs, one associated with the metabolic conditions: heart disease, hypercholesterolemia, high blood pressure, and type2 diabetes and the other by the cancers: skin, colorectal and lung. Osteoporosis did not load consistently on either of these constructs. These results are consistent with those reported elsewhere (Noyes et al., 2005) where osteoporosis represented a third cluster of diseases, along with bone and joint conditions. Attitudes and response efficacy, on the other hand, each measured as a single domain. We excluded osteoporosis from further analysis and continued the analysis with the eight constructs represented by Worry (Metabolic), Worry (cancer), Perceived Risk (Metabolic), Perceived Risk (Cancer), Perceived Severity (Metabolic), Perceived Severity (Cancer), Response Efficacy and Attitudes.
A subsequent CFA using all eight constructs suggested that the construct Perceived Risk (Cancer) was not well supported. It was noted that the responses to the items used to measure Perceived Risk (Cancer) had low averages and standard deviations indicating that these respondents did not perceive skin, lung or colorectal cancer to be a significant risk. Deleting Perceived Risk (Cancer) and incorporating correlations between the error terms as indicated by the modification indices, we obtained a satisfactory fit for the CFA of the constructs as shown in Figure 3.
Figure 3.
The measurement model for study constructs. Curved arrows indicate correlations (correlations between constructs are not shown for simplicity). Boxes indicate observable variables, ovals indicate constructs, and circles indicate error terms. Constructs specific to cancer and metabolic conditions are labeled using “C” and “M” respectively. Variables for each health condition are indicated by: HD (Heart Disease), Hypercholesterolemia (HC), Hypertension (HTN), Type 2 Diabetes (T2D), Colorectal Cancer (CC), Skin Cancer (SC), and Lung Cancer (LC).
The resulting CFA fit statistics included a chi-sq=919.3 with df=436 (p=0, ratio=2.1), CFI=0.94 and RMSEA=0.06 which were all within acceptable ranges. In addition, convergent validity was satisfied (all the factor loadings are significant, all standardized loadings are greater than 0.7 except four which are larger than 0.5, the variances extracted are 0.5 or greater, and reliabilities are all greater than 0.7) and discriminant validity was supported for all constructs (except Worry (Cancer) and Worry (Metabolic)). The error covariances were all significant and there were no additional meaningful model improvements suggested by the modification indices. These results indicated that the measurement model associated with the constructs in Figure 3 was supported by the data at this stage of the analysis.
Structural Model
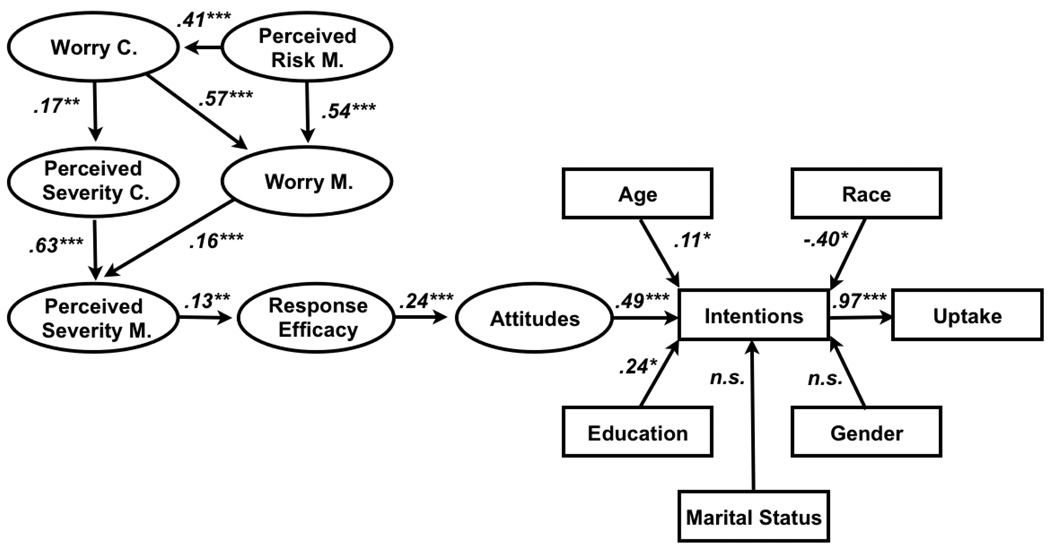
Once the measurement model was established, a SEM structural model of the latent variables was fit utilizing the significant correlations between constructs in the measurement model and the model in Figure 1. The result was that several of the regression links were statistically insignificant (a significance level of 0.1 was required to be included in the model). Insignificant paths were removed from the model one by one starting with the least significant and the model was refit. The resulting model was deemed an improvement if it resulted in an improvement in the AIC and sample-size adjusted BIC. This process resulted in the final model shown in Figure 4 with the indicated standardized regression weights and associated significance levels.
Figure 4.
Structural model for the uptake of multiplex genetic testing. Weights for each path are standardized coefficients. Stars indicate the significance of the association (*:p<.1; **:p<.05;***:p<.01). Arrows indicate paths of influence, ovals indicate constructs, and boxes indicate measured variables. Constructs specific to cancer and metabolic conditions are marked by “C” and “M” respectively.
For the purposes of SEM structural model analysis, intentions were dichotomized between participants who are interested in the test versus others, who declined or were unsure. Sixty one percent of the participants who selected “maybe” eventually declined testing, as compared to 100% and 21% among those declined or were interested in testing respectively. The model explains 48% of the variance in intentions and 94% of the variation in uptake. Moreover, the model indicates that the odds of acting are 17.7 times higher for those with intent to undergo testing than for those without1. All else being held constant, the odds of intending to get tested are 3.1 times higher for a respondent having a latent attitude score that is one unit more positive, 1.1 times higher for a person one year older, 0.6 times lower for an African American than a white participant and 1.4 times higher for someone with some college than for someone with no college education.
DISCUSSION
The Multiplex Genetic Testing Model proved useful in predicting test uptake among participants in a multiplex testing study. Having a positive attitude towards testing was the strongest predictor of test interest, which in turn predicted test uptake, as conceptualized in the model. Demographic characteristics predicted testing, with older participants being more interested in testing, suggesting that as participants approach middle age they may be increasingly motivated to learn about future health risks. There were trends toward white participants and college graduates having greater interest in testing. Our hypothesis that worry, perceived risk, and perceived severity would each be represented by a single domain that independently predicted attitudes was not confirmed.
Our findings suggest that study participants grouped their perceptions about the health threats generated from the eight conditions into two primary domains, cancers: lung, colorectal and skin, and metabolic conditions: type II diabetes, hypertension, coronary artery disease and high cholesterol. Perceived risk for the metabolic conditions was significantly correlated with worry in each of the domains, for metabolic conditions and for cancer. This suggests that while the domains were distinct, a higher perceived risk for the metabolic conditions was generalized to worry about cancer as well as worry about the metabolic conditions. Each of the two worry domains was separately correlated with perceived severity. So more worry about cancer predicted greater perceived severity of cancer and more worry about the metabolic conditions predicted greater perceived severity of the metabolic conditions.
Further, as was expected, perceived severity of one domain of conditions was significantly correlated with the other, and worry about one domain was also significantly correlated with worry about the other domain. The effect of illness representations and worry about one disease on another have been reported in other studies (DiLorenzo, et al, 2006, Gerend, 2004, Schnur, et. al., 2006)
The remainder of our model constructs; response efficacy and attitudes all represented a single domain each suggesting measurement of an overarching psychological construct for all eight of the conditions combined. It is notable that initial perceptions are generated by two large categories of conditions (metabolic and cancer) but the variables that pertain more directly to multiplex testing measure a single construct domain. The findings may be explained by the context of multiplex testing. The closer one gets to the decision to undergo testing, all considerations about testing must be channeled into one choice as there was no option to be tested for only one of the categories of conditions.
Yet it was only perceived severity of the metabolic conditions that was correlated with general response efficacy and the remainder of the key variables in predicting uptake. Remarkably, perceived risk for cancer did not make a significant contribution and was dropped from the model. This supports recent evidence demonstrating that worry has an advantage over risk perception in predicting health behaviors (Cameron, et al, 2009, Schmiege et al, 2009). Our findings suggest that while perceived risk, perceived severity and worry are key to the initial processing of information about a health threat, they are less important in predicting response-efficacy and don’t predict attitudes toward testing as we had hypothesized.
Importantly, response efficacy was seen to directly influence attitudes towards testing, consistent with similar results found by van den Berg and colleagues who used PMT to frame decisions about prenatal screening (van den Berg et al., 2008). Related beliefs about perceived control have been seen as motivators for undergoing a variety of health screening tests (Decruyenaere, Evers-Kiebooms, Welkenhuysen, Denayer, & Claes, 2000; Gooding et al., 2006; Lagerlund, Hedin, Sparen, Thurfjell, & Lambe, 2000; McClenahan, Shevlin, Adamson, Bennett, & O'Neill, 2007; Newell, Modeste, Marshak, & Wilson, 2009; Shiloh, Petel, Papa, & Goldman, 1998; Wong, 2009), suggesting a significant role for perceived confidence in one’s ability to control health outcomes.
Response efficacy was operationally defined as the belief that multiplex testing can help reduce the chances of getting each of the diseases included in the test. It is remarkable that it was found to predict attitudes towards testing since multiplex genetic testing per se cannot reduce risk for any of the conditions. The explanation for our finding assumes the existence of two further beliefs: that the diseases being tested can be prevented effectively by early detection and application of appropriate behavioral or medical interventions; and that one has the ability to perform behaviors related to decreasing the risk (self-efficacy beliefs). It is possible that the prominent role of response efficacy in predicting attitudes lies partly with the web-based Multiplex Initiative educational materials. They may have left participants feeling confident in their ability to use the test results to reduce their health risks. On the website it stated: “People who have risk versions of genes may be more harmed by their health habits than their genes; You cannot change your genes, but you can change your health habits; We do not know much about how having risk versions of genes affects how our body responds to health habits, such as our diet, exercise and cigarette smoking.”
From a practical perspective, it is important to understand the source of positive beliefs in the outcomes of testing. Do they originate from educational materials about testing? Or do they stem from belief in the power of medical information and the value of new medical technology and its promise for reducing disease? Some of these values and beliefs may be subject to persuasion or influence and others may be intrinsic to the individuals making decisions whether to undergo testing. This study was not designed to answer the question about the relationship between the information provided and response efficacy, but results from the larger Multiplex Initiative cohort revealed that a majority of participants had high levels of confidence that behavior change could reduce their disease risk (McBride et al., 2009).
Overall, our results offer powerful evidence for associations among key constructs from prevalent theories of health behavior, with a significant role for constructs from the TPB: attitudes and intentions. These constructs were highly predictive of testing intent and ultimately test uptake and accounted for the majority of the variance in test choice offering evidence for the importance of an expanded conceptual model for multiplex genetic testing uptake. The decision to undergo testing for multiple common conditions was an intentional, planned behavior, with attitudes toward testing as a major predictor of intent and uptake.
Strengths and Limitations
SEM analysis offers an advantage over other methods by measuring unobserved constructs, simultaneously addressing multiple relationships between constructs, and accommodating relationships of dependence that integrate covariance (DiLalla, 2008). Furthermore, this is the first report to model decisions about obtaining genetic testing for multiple common health conditions.
Our study is, however, limited in several respects. We examined a subset of the larger group of Multiplex Initiative participants. Although the sub-sample used in this study was not significantly different from participants accessing the website based on socio-demographic variables, they did have slightly higher intentions and test uptake. Thus, our subset may not be fully representative of the larger group. The fact that most of the variables in our model were measured using an additional survey on the Multiplex Initiative website suggests that the participants selected for inclusion may have been more highly motivated or otherwise distinct. Additionally, the measure of intentions was assessed just prior to response efficacy and attitudes, which may have introduced an order effect on how the latter variables were assessed.
Our study was correlational in nature. A recent review of the experimental literature (Webb & Sheeran, 2006) suggested that intentional control of health behavior may be more limited than correlational studies suggest. Thus, future studies that manipulate attitudes and intentions in experimental groups (compared to a control group) should be designed to further validate our findings about the predictors of multiplex testing uptake.
Future studies should carefully examine underlying values and beliefs that may determine positive attitudes towards testing. These constructs, including response efficacy, may offer important understanding of the origins of positive attitudes towards multiplex testing. They also may represent relevant constructs to influence. For example, if in the future multiplex genetic testing were shown to provide health benefits, it would be useful to enhance positive beliefs in the ability of testing to reduce disease risk through providing information on risk-reducing activities and the ways that others have successfully adopted them.
Table 2.
Construct Correlations in the Measurement Model
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1) Perceived Severity M | 1 | 0.652* | 0.057 | 0.129* | 0.199* | 0.246* | 0.109 |
| 2) Perceived Severity C | 1 | 0.048 | 0.065 | 0.177* | 0.11 | −0.013 | |
| 3) Attitudes | 1 | 0.238* | 0.088 | 0.098 | 0.02 | ||
| 4) Response Efficacy | 1 | 0.106 | 0.033 | −0.01 | |||
| 5) Worry C | 1 | 0.789* | 0.415* | ||||
| 6) Worry M | 1 | 0.769* | |||||
| 7) Perceived Risk M | 1 |
P-value <0.5.
Abbreviations: M=Metabolic, C=Cancers.
Acknowledgements
This research was supported by the Intramural Research Program of the National Human Genome Research Institute, National Institutes of Health. The proposed research was made possible through a collaboration with the Cancer Research Network funded by the National Cancer Institute (U19CA 079689). Group Health Research Institute and Henry Ford Hospital provided additional resources. Genotyping services were provided by the Center for Inherited Disease Research (CIDR). CIDR is fully funded through a federal contract from the National Institutes of Health to The Johns Hopkins University (HHSN268200782096C). Additionally, this research was supported in part by an appointment to the Senior Fellowship Program at the National Institutes of Health. This program is administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the US Department of Energy and the National Institutes of Health.
We would like to thank the study participants, members of the Henry Ford Health System and members of the Multiplex Initiate Steering Committee for their efforts in making the Multiplex Initiative Ancillary Studies possible. We would also like to thank the anonymous reviewers for their very useful feedback on an earlier draft of this manuscript.
Footnotes
Combining uninterested and unsure participants may have inflated the intention-uptake link to some extent, but in view of the strong effect, even without dichotomizing the link would still be high
REFERENCES
- Ajzen I. The theory of planned behavior. Organisational Behaviour and Human Decision Processes. 1991;50:179–211. [Google Scholar]
- Alford SH, McBride CM, Reid RJ, Larson EB, Baxevanis AD, Brody LC. Participation in genetic testing research varies by social group. Public Health Genomics. 2010 doi: 10.1159/000294277. epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arbuckle JL. AMOS™ 16 user's guide. fifth edition. Chicago, IL: SPSS; 2007. [Google Scholar]
- Avard D, Knoppers BM. Genomic medicine: Considerations for health professionals and the public. Genome Medicine. 2009;1(2):25. doi: 10.1186/gm25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bollen KA. Structural Equations with Latent Variables. New York: Wiley; 1989. [Google Scholar]
- Cameron LD, Diefenbach MA. Responses to information about psychosocial consequences of genetic testing for breast cancer susceptibility: Influences of cancer worry and risk perceptions. J Health Psych. 2001;6(1):47–59. doi: 10.1177/135910530100600104. [DOI] [PubMed] [Google Scholar]
- Cameron LD, Reeve J. Risk perceptions, worry, and attitudes about genetic testing for breast cancer susceptibility. Psych & Health. 2006;21(2):211–230. doi: 10.1080/14768320500230318. [DOI] [PubMed] [Google Scholar]
- Cameron LD, Muller C. Psychosocial aspects of genetic testing. Curr Opin Psychiatry. 2009;22(2):218–223. doi: 10.1097/YCO.0b013e3283252d80. [DOI] [PubMed] [Google Scholar]
- Decruyenaere M, Evers-Kiebooms G, Welkenhuysen M, Denayer L, Claes E. Cognitive representations of breast cancer, emotional distress and preventive health behaviour: A theoretical perspective. Psychooncology. 2000;9(6):528–536. doi: 10.1002/1099-1611(200011/12)9:6<528::aid-pon486>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- DiLalla LF. A structural equation modeling overview for medical researchers. J Dev Behav Pediatr. 2008;29(1):51–54. doi: 10.1097/DBP.0b013e31815f250c. [DOI] [PubMed] [Google Scholar]
- DiLorenzo TA, Schnur J, Montgomery GH. A model of disease-specific worry in heritable disease: The influence of family history, perceived risk and worry about other illnesses. J Beh Med. 2006;29(1):37–49. doi: 10.1007/s10865-005-9039-y. [DOI] [PubMed] [Google Scholar]
- Dormandy E, Hankins M, Marteau T. Attitudes and uptake of a screening test: The moderating role of ambivalence. Psychology and Health. 2006;21(4):499–511. [Google Scholar]
- Gerend MA, Aiken LS, West SG. Personality factors in older women’s perceived susceptibility to diseases of aging. J Personal. 2004;72(2):243–270. doi: 10.1111/j.0022-3506.2004.00262.x. [DOI] [PubMed] [Google Scholar]
- Gooding HC, Organista K, Burack J, Biesecker BB. Genetic susceptibility testing from a stress and coping perspective. Soc Sci Med. 2006;62(8):1880–1890. doi: 10.1016/j.socscimed.2005.08.041. [DOI] [PubMed] [Google Scholar]
- Helmes AW. Application of the protection motivation theory to genetic testing for breast cancer risk. Prev Med. 2002;35(5):453–462. doi: 10.1006/pmed.2002.1110. [DOI] [PubMed] [Google Scholar]
- Hogarth S, Javitt G, Melzer D. The current landscape for direct-to-consumer genetic testing: Legal, ethical, and policy issues. Annual Review of Genomics and Human Genetics. 2008;9:161–182. doi: 10.1146/annurev.genom.9.081307.164319. [DOI] [PubMed] [Google Scholar]
- Janz NK, Champion VL, Strecher VJ. The Health Belief Model. In: Glanz K, Rimer BK, Lewis FM, editors. Health behavior and health education: Theory, research, and practice. San Francisco: Jossey-Bass; 2002. pp. 45–66. [Google Scholar]
- Kaphingst KA, McBride CM, Wade CH, Alford SH, Brody LC, Baxevanis AD. Consumer’s use of web-based information and their decisions about multiplex genetic susceptibility testing. J Med Internet Res. 2010;12(3):e41. doi: 10.2196/jmir.1587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaFramboise T. Single nucleotide polymorphism arrays: A decade of biological, computational and technological advances. Nucleic Acids Res. 2009;37(13):4181–4193. doi: 10.1093/nar/gkp552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakeman P, Plass AM, Henneman L, Bezemer PD, Cornel MC, ten Kate LP. Preconceptional ancestry-based carrier couple screening for cystic fibrosis and haemoglobinopathies: What determines the intention to participate or not and actual participation? Eur J Hum Genet. 2009;17(8):999–1009. doi: 10.1038/ejhg.2009.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marteau TM, Croyle RT. The new genetics. psychological responses to genetic testing. BMJ. 1998;316(7132):693–696. doi: 10.1136/bmj.316.7132.693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marteau TM, Lerman C. Genetic risk and behavioural change. BMJ. 2001;322(7293):1056–1059. doi: 10.1136/bmj.322.7293.1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride CM, Alford SH, Reid RJ, Larson EB, Baxevanis AD, Brody LC. Putting science over supposition in the arena of personalized genomics. Nat Genet. 2008;40(8):939–942. doi: 10.1038/ng0808-939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride CM, Alford SH, Reid RJ, Larson EB, Baxevanis AD, Brody LC. Characteristics of users of online personalized genomic risk assessments: Implications for physician-patient interactions. Genet Med. 2009;11(8):582–587. doi: 10.1097/GIM.0b013e3181b22c3a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride CM, Wade CH, Kaphingst KA. Consumers’ views of direct-to-consumer genetic information. Annu Rev Genomics Hum Genet. 2010;11:427–446. doi: 10.1146/annurev-genom-082509-141604. [DOI] [PubMed] [Google Scholar]
- McClenahan C, Shevlin M, Adamson G, Bennett C, O'Neill B. Testicular self-examination: A test of the health belief model and the theory of planned behaviour. Health Educ Res. 2007;22(2):272–284. doi: 10.1093/her/cyl076. [DOI] [PubMed] [Google Scholar]
- Michie S, Dormandy E, Marteau TM. The multi-dimensional measure of informed choice: A validation study. Patient Educ Couns. 2002;48(1):87–91. doi: 10.1016/s0738-3991(02)00089-7. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user's guide. fifth edition. Los Angeles, CA: Muthén & Muthén; 1998–2007. [Google Scholar]
- Newell M, Modeste N, Marshak HH, Wilson C. Health beliefs and the prevention of hypertension in a black population living in london. Ethn Dis. 2009;19(1):35–41. [PubMed] [Google Scholar]
- Nordin K, Bjork J, Berglund G. Factors influencing intention to obtain a genetic test for a hereditary disease in an affected group and in the general public. Prev Med. 2004;39(6):1107–1114. doi: 10.1016/j.ypmed.2004.04.021. [DOI] [PubMed] [Google Scholar]
- Noyes R, Jr, Carney CP, Hillis SL, Jones LE, Langbehn DR. Prevalence and correlates of illness worry in the general population. Psychosomatics. 2005;46:529–539. doi: 10.1176/appi.psy.46.6.529. [DOI] [PubMed] [Google Scholar]
- Panoutsopoulou K, Zeggini E. Finding common susceptibility variants for complex disease: Past, present and future. Brief Funct Genomic Proteomic. 2009;8(5):345–352. doi: 10.1093/bfgp/elp020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers RW, Prentice-Dunn S. Protection motivation theory. In: Gochman DS, editor. Handbook of health behavior research I: Personal and social determinants. New York, NY: Plenum Press; 1997. pp. 113–132. [Google Scholar]
- Schnur JB, DiLorenzo TA, Montgomery GH, et al. Perceived risk and worry about prostate cancer: A proposed conceptual model. Beh Med. 2006;32(3):89–96. doi: 10.3200/BMED.32.3.89-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmiege SJ, Broaddus MR, Levine M, Bryan AD. Randomized trial of group interventions to reduce HIV/STD risk and change theoretical mediators among detained adolescents. J Consult Clin Psychol. 2009;77(1):38–50. doi: 10.1037/a0014513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiloh S, Petel Y, Papa M, Goldman B. Motivations, perceptions and interpersonal differences associated with interest in genetic testing for breast cancer susceptibility among women at high and average risk. Psychol Health. 1998;13(6):1071–1086. [Google Scholar]
- Skrondal A, Rabe-Hesketh S. In: Structural equation modeling: Categorical variables. Everitt B, Howell D, editors. London, UK: Wiley; 2005. [Google Scholar]
- van den Berg M, Timmermans DR, Knol DL, van Eijk JT, de Smit DJ, van Vugt JM, van der Wal G. Understanding pregnant women's decision making concerning prenatal screening. Health Psychol. 2008;27(4):430–437. doi: 10.1037/0278-6133.27.4.430. [DOI] [PubMed] [Google Scholar]
- Wade CH, McBride CM, Kardia SL, Brody LC. Considerations for designing a prototype genetic test for use in translational research. Public Health Genomics. 2009;13(3):217–226. doi: 10.1159/000236061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb TL, Sheeran P. Does changing behavioral intentions engender behavior change? A meta-analysis of the experimental evidence. Psychol Bull. 2006;132(2):249–268. doi: 10.1037/0033-2909.132.2.249. [DOI] [PubMed] [Google Scholar]
- Wong N. Investigating the effects of cancer risk and efficacy perceptions on cancer prevention adherence and intentions. Health Commun. 2009;24(2):95–105. doi: 10.1080/10410230802676474. [DOI] [PMC free article] [PubMed] [Google Scholar]