Abstract
Introduction
To describe the clinical and surgical outcomes among patients under 20 years of age diagnosed with glaucoma in a defined population over a 40-year period.
Methods
The medical records of all patients (<20 years) diagnosed with glaucoma in Olmsted County, Minnesota, from January 1, 1965, through December 31, 2004, were retrospectively reviewed.
Results
Thirty children (45 eyes) were diagnosed with various forms of glaucoma during the 40-year study period. During a mean follow-up of 12.5 years (range, 7 days to 32 years), 18 (60%) of the 30 children underwent a mean of 2.7 surgeries (range, 1 to 10), including 6 (20%) patients whose sole surgery consisted of enucleation or evisceration for a blind, painful eye. Twenty-eight (93%) of the 30 children required medical management during the follow-up period, including 14 (47%) treated before their first surgery. At the final follow-up examination, 11 (37%) had a visual acuity of 20/200 or worse. The 10-year Kaplan-Meier risk of vision declining below 20/200 in all glaucoma patients was 22.7% (95% CI, 0-40.9), and patients requiring any glaucoma surgery was 68.3% (95% CI, 42.4-82.6).
Conclusions
In this population-based study of children diagnosed with glaucoma over a 40-year period, the majority of patients required surgery, with few being successfully controlled by medications alone. A poor visual outcome or the loss of an eye was relatively common.
Introduction
Childhood glaucoma is an uncommon ocular condition often associated with significant visual loss.1,2 The heterogeneity of the diseases encompassing childhood glaucoma makes a single unifying treatment approach impractical. For example, while the treatment of choice for primary congenital glaucoma includes trabeculotomy or goniotomy,3,4 acquired forms, such as uveitic glaucoma may be medically managed.5,6 The medical and surgical outcomes of childhood glaucoma within a defined population in the United States have not been reported. The purpose of this study is to describe the outcomes of children <20 years of age diagnosed with glaucoma as residents of Olmsted County, Minnesota, during a 40-year period.
Subjects and Methods
The medical records of all patients younger than 20 years of age who were residents of Olmsted County when diagnosed with glaucoma between January 1, 1965, and December 31, 2004 were retrospectively reviewed. Institutional review board approval was obtained for this study. Potential cases of glaucoma were identified using the resources of the Rochester Epidemiology Project, a medical record linkage system designed to capture data on any patient–physician encounter in Olmsted County.7 The population of this county is relatively isolated from other urban areas and virtually all medical care is provided by our institution, Olmsted Medical Group, and their affiliated hospitals. Patients not residing in Olmsted County at the time of their diagnosis were excluded from the study. Childhood glaucoma was defined until age 20 instead of the traditional age limit of 18 to ensure that the juvenile primary open-angle glaucoma patients, which can occur up to 40 years, were included.
Glaucoma was defined generally in this study as an optic neuropathy and/or a visual field change, frequently associated with elevated intraocular pressure (IOP). Clinical signs, such as elevated IOP (>21 mm Hg), optic nerve cupping, asymmetric or progressive disk cupping, visual field defects, or anterior segment changes, such as buphthalmos or Haab striae (alone or in combination), were used to make the diagnosis of glaucoma. Primary congenital glaucoma included patients presenting with ocular signs of corneal enlargement combined with one or more of the classic findings, such as photophobia, epiphora, Haab striae, corneal clouding, or optic nerve cupping and ranging in age from birth to early childhood. Primary open-angle glaucoma diagnosed during childhood and early adulthood was defined as juvenile glaucoma. Secondary glaucoma included patients with a systemic or ocular condition present at birth, while acquired glaucoma referred to those patients with secondary processes occurring after birth. No retrospective diagnosis of glaucoma was made, and all patients included had been diagnosed by the ophthalmologists who participated in their care. The medical records of all Olmsted County patients diagnosed with glaucoma were reviewed for medical and surgical treatment and followed to July 2008.
Continuous data is presented as a mean (minimum-maximum) and categorical data is presented as counts and percentages. The rates of developing visual acuity <20/200 and of requiring at least one glaucoma surgery 5-10 years after diagnosis were calculated using the Kaplan-Meier method.8
Results
A total of 30 patients (16 males) under 20 years of age were diagnosed with glaucoma in Olmsted County during the 40-year study period, yielding an annual age and gender-adjusted incidence of 2.29/100,000 residents (95% CI, 1.47-3.12).9 Of the total number of glaucoma cases, 50% were bilateral, affecting a total of 45 eyes. Ethnicities were reported as follows: 18 white (60%), 4 black (13.3%), 2 Asian (6.7%), 1 American Indian (3.3%), and 5 of unknown race (16.7%). Patients were diagnosed at a mean age of 10.4 years (range, 15 days-19.7 years). A family history of glaucoma was present in 20% of the study patients. Mean presenting intraocular pressure was 30.8 mm Hg (range, 14 to 56 mm Hg) and mean cup/disk ratio at the first visit was 0.5 (range, 0.1 to 1.0) in the glaucomatous eye.
Of the 30 study patients, 28 (93%) received topical medications at one point during their management, among which 11 (39%) were managed with medications alone. Of the 11 children who were managed medically, 9 had an acquired glaucoma. For all glaucoma subtypes, beta blockers were the most commonly used medication during the years of this study. Of the 30 patients, 22 (73%) were treated with a beta blocker, 15 (50%) with a prostaglandin, 9 (30%) with dorzolamide-timolol, 7 (23%) with a parasympathomimetic, and 6 (20%) with a noncombination carbonic anhydrase inhibitor either in topical, oral, or intravenous form. Patients diagnosed in the 1970s were more likely to be managed with beta blockers and carbonic anhydrase inhibitors, while those in the 1980s were also treated with prostaglandins and parasympathomimetics.
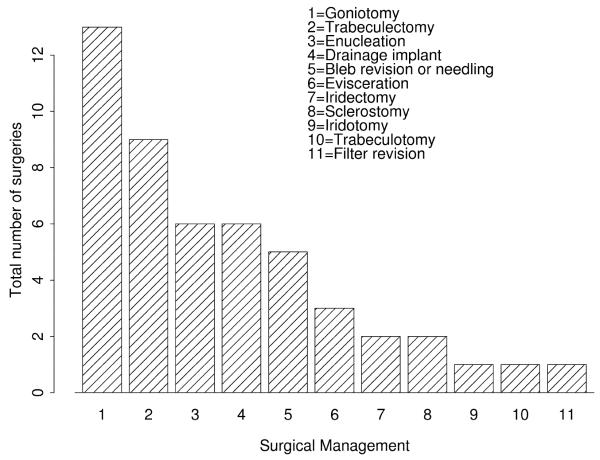
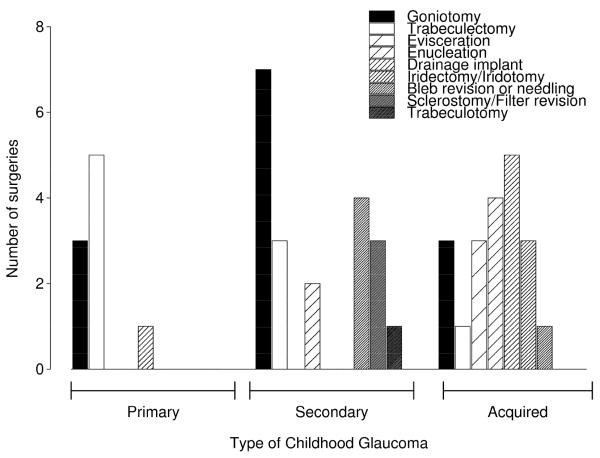
During a mean follow-up of 12.5 years (range, 7 days to 32 years), 18 (60%) of the 30 children underwent a mean of 2.7 glaucoma procedures (range, 1-10), including 6 patients (20%) whose sole surgery consisted of an enucleation or evisceration for a painful blind eye. Fourteen of the 18 patients who underwent surgery were initially managed with topical medications. Surgical management consisted of 49 glaucoma procedures, including 13 goniotomies, 9 trabeculectomies, 6 enucleations, 6 glaucoma drainage implants, 5 bleb repairs or needling, 3 eviscerations, 2 peripheral iridectomies, 2 thermal sclerostomies, and 1 each of a trabeculotomy, a yttrium aluminium garnet (YAG) laser iridotomy and a filter revision (Figures 1 and 2).
Figure 1.
The Surgical Management of 18 Patients < 20 Years old Diagnosed with Glaucoma in Olmsted County, MN 1965-2004
Figure 2.
Types of Surgeries Performed, by Glaucoma Subtype, for 18 Children with Glaucoma in Olmsted County, MN, 1965-2004
Goniotomy was the principal procedure performed during the early years of the study, followed by trabeculectomy in the middle years, while drainage implants became more common in the most recent decade.
Primary childhood glaucoma was diagnosed in 4 children with juvenile glaucoma; 1 child had primary congenital glaucoma (PCG). The average number of surgeries for these patients was 1.80, ranging from 1.25 in juvenile glaucoma to 4.0 for the single patient with PCG. At a mean follow-up of 15.6 years (range, 3.8-31.9 years), the average IOP was 17.3 mm Hg (range, 15.5-20) and 75% of the primary childhood glaucoma patients were on medications. Our case of PCG was diagnosed in a 15-day-old boy who presented with IOPs of 25 mm Hg in the right eyes and 40 mm Hg in the left eyes and cup/disk ratios of 0.1 in the right and 0.8 in the left. The patient underwent bilateral goniotomy and a Baerveldt drainage implant in the right eye. At the final follow-up (age 13), his IOP was 14 mm Hg in the right eye and 17 mm Hg in the left while on IOP-reducing medications. The final visual acuities were 20/20 in the right and 20/30 in the left.
Of the 30 children, 6 (20%) were diagnosed with secondary glaucoma, including 2 with Sturge-Weber syndrome, 2 with neovascular glaucoma (1 patient with Coats disease and 1 with retinopathy of prematurity), and 1 each with Rubinstein-Taybi and cutis marmorata telangiectatica congenita (CMTC). These patients had the highest average number of surgeries, with a mean of 3.33 surgeries per patient, ranging from no surgery in the patient with Coats disease to 10 surgeries in the child with CMTC. At a mean follow-up of 16.7 years (range, 9 days to 28.3 years), the average IOP was 16.1 mm Hg (range, 8.5 to 22) and 50% of secondary glaucoma patients were on IOP-lowering medications. The final visual acuity was <20/200 in 2 of the 6 patients with secondary glaucoma.
Of the 30 children, 19 (63%) were diagnosed with acquired glaucoma at a mean age of 11.1 years (range, 3.0-18.8 years). Fourteen developed glaucoma secondary to trauma or surgery, including aphakic and pseudophakic patients, 4 from uveitis, and 1 following topical steroid use. These patients underwent an average of 1.05 (range, 1-4) glaucoma procedures. At a mean final follow-up of 10.3 years (range, 54 days to 31.1 years), the average IOP was 16.4 mm Hg (range, 7.5-27) and 11 (58%) were on IOP-lowering drugs. Patients with uveitic glaucoma had the highest average number of surgeries in the acquired glaucoma diagnostic group (1.75 per patient) and all were on glaucoma medications at the final visit. In comparison, only 50% of traumatic/aphakic patients were on IOP-lowering drugs at the final follow-up visit.
Increasing the age limit to 20 years did not lead to an increased prevalence of acquired cases in our sample. All but one of our glaucoma patients was <19 when diagnosed. This patient had juvenile open-angle glaucoma. Three other patients were between 18 and 19 years old, including 1 with Coats disease and 2 with traumatic/surgical glaucoma. Even without these 2 acquired glaucoma patients older than 18 but younger than 19, acquired glaucoma would still be the most common type of glaucoma in our population.
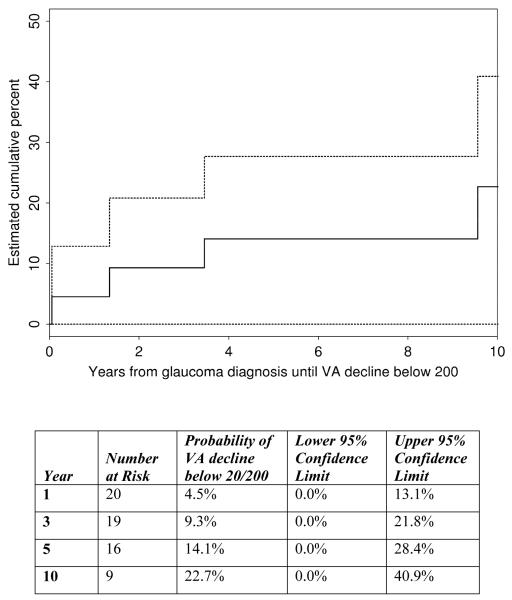
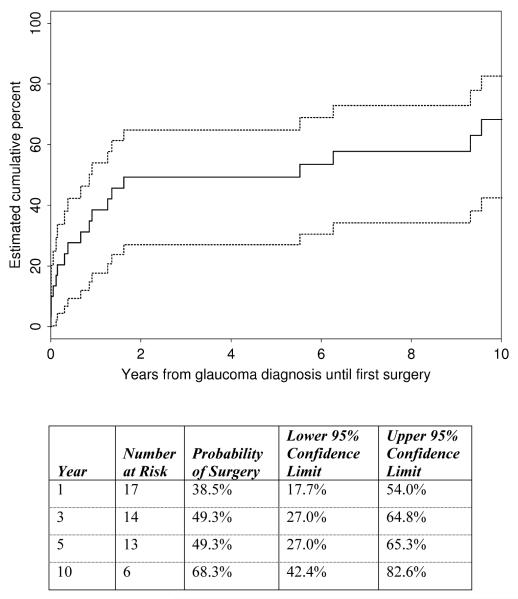
At the final follow-up examination, 11 of the 30 patients (37%) with glaucoma had a visual acuity of 20/200 or worse. The Kaplan-Meier risk of vision declining below 20/200 in all pediatric glaucoma patients was 14.1% (95% CI, 0-28.4 ) at 5 years and 22.7% (95% CI, 0-40.9) at 10 years (Figure 3). The Kaplan-Meier risk of undergoing a glaucoma surgery, including evisceration and enucleation, was 49.3% at 5 years and 68.3% (95% CI, 42.4-82.6) at 10 years (Figure 4).
Figure 3.
The Kaplan-Meier Probability of Vision Declining below 20/200 [95% Confidence Intervals] in a Cohort of Patients (<20 years old) Diagnosed with Glaucoma in Olmsted County, MN, 1965-2004
Figure 4.
The Kaplan-Meier Probability of Requiring a Glaucoma Surgery [95% Confidence Intervals] in a Cohort of Patients (<20 years old) Diagnosed with Glaucoma in Olmsted County, MN, 1965-2004
Discussion
Childhood glaucoma was diagnosed in 30 (1 in 43,575) patients who were younger than 20 years old as residents of Olmsted County during the 40-year study period. Beta blockers and goniotomy were the most common treatment modalities used during the years of the study. Approximately half the children required glaucoma surgery after 5 years and two-thirds by 10 years, with significant visual loss occurring in one-fourth of the study patients one decade after their diagnosis.
The prevalent use of beta blockers in this population of children with glaucoma is consistent with prior studies.10,11 Beta blockers were commonly used in this study in part because they were introduced in 1978,12 while other medications, such as topical carbonic anhydrase inhibitors, prostaglandins, and dorzolamide-timolol, are newer. Prior to the development of beta blockers, the treatment options for glaucoma were limited and consisted of oral acetazolamide, topical epinephrine borate, or pilocarpine.10 No significant complications were found regarding topical treatment, which is consistent with prior reports.11,13 Medical management alone was successful in the treatment of 11 of the 19 patients with acquired glaucoma. Of the 30 patients, 60% were on IOP-lowering medications at the final examination. The mean IOP at the last examination was 16.5 mm Hg (range, 7.5-27) for all glaucoma patients.
Most of the study patients also underwent a glaucoma procedure, most often a goniotomy (Figures 1 and 2). The preference for this procedure may be due to the known success rate of goniotomy in childhood glaucoma, especially in PCG.4,14-16 Goniotomy has the advantage of preserving the conjunctiva for future surgeries, since children with childhood glaucoma have a significant risk for relapse.14 However, other procedures, like trabeculectomy, are also effective in the treatment of childhood glaucoma.16-18 All of our juvenile glaucoma patients were successfully managed with trabeculectomy alone. Glaucoma drainage implants were only used in 4 of our glaucoma patients, generally following a failed goniotomy or trabeculectomy. These procedures have been reported to be safe in childhood glaucoma.19,20
While primary glaucoma was treated with an average of 1.80 surgeries, syndrome-related secondary glaucoma was more difficult to manage in this cohort. The disease tended to occur earlier and required a greater number of surgeries per patient, 5 compared to 1 surgery per patient in nonsyndromic cases and primary glaucoma. While these observations may underline the importance of early and close monitoring of patients with systemic syndromes known to cause glaucoma,21 generalizations derived from these findings are problematic due to the small numbers of patients.
Acquired glaucoma was the most common type of glaucoma diagnosed at a mean age of 11.6 years. In our study, with its homogeneous population, patients with acquired glaucoma required fewer surgeries compared to primary and secondary glaucoma patients. The majority of children with uveitic glaucoma were managed successfully by topical medications alone; however, when managed surgically, uveitic glaucoma required an average of 1.75 surgeries per patient, which made it the most difficult acquired glaucoma to manage. In our population, 100% of our uveitic patients were on an IOP-lowering medication at the final follow-up, which is consistent with prior reports that show the majority of uveitic glaucoma patients requiring medical management following surgical intervention.22
There are several limitations to the findings in this study. The retrospective design is limited by the nonstandardized and incomplete data collection. In addition, the low incidence of childhood glaucoma in our population makes extrapolating the findings of glaucoma subtypes difficult. Our ability to generalize these findings is further limited by the demographics of Olmsted County, a relatively homogeneous semiurban, white population. This homogeneity may explain our low incidence of primary congenital glaucoma, a recessive genetic disorder with increased frequency in populations with consanguineous marriages. Moreover, the understanding and management of childhood glaucoma has evolved over the study years, making it difficult to assess outcomes for a specific treatment regimen. Furthermore, although a large number of reports from this population attest to the well-defined nature and medical isolation of this cohort, some residents of Olmsted County (less than 5%)23 may have sought care outside the region, potentially skewing the outcome of glaucoma in this population. Finally, additional cases of glaucoma may have been missed or misdiagnosed due to changing definitions of glaucoma during the 40-year study period.24
Acknowledgments
Supported in part by an unrestricted grant from Research to Prevent Blindness, Inc., New York, NY, and by the Rochester Epidemiology Project (Grant # RO1-AR30582) through the National Institute of Arthritis and Musculoskeletal and Skin Diseases.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors have no financial or conflicting interests to disclose.
References
- 1.Gould DB, John SW. Anterior segment dysgenesis and the developmental glaucomas are complex traits. Hum Mol Genet. 2002;11:1185–93. doi: 10.1093/hmg/11.10.1185. [DOI] [PubMed] [Google Scholar]
- 2.Quigley HA. Number of people with glaucoma worldwide. Br J Ophthalmol. 1996;80:389–93. doi: 10.1136/bjo.80.5.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Giampani J, Jr, Borges-Giampani AS, Carani JC, Oltrogge EW, Susanna R., Jr Efficacy and safety of trabeculectomy with mitomycin C for childhood glaucoma: A study of results with long-term follow-up. Clinics (Sao Paulo) 2008;63:421–6. doi: 10.1590/S1807-59322008000400002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Broughton WL, Parks MM. An analysis of treatment of congenital glaucoma by goniotomy. Am J Ophthalmol. 1981;91:566–72. doi: 10.1016/0002-9394(81)90054-4. [DOI] [PubMed] [Google Scholar]
- 5.Maris PJ, Jr, Mandal AK, Netland PA. Medical therapy of pediatric glaucoma and glaucoma in pregnancy. Ophthalmol Clin North Am. 2005;18:461–8. vii. doi: 10.1016/j.ohc.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 6.Beck AD. Diagnosis and management of pediatric glaucoma. Ophthalmol Clin North Am. 2001;14:501–12. doi: 10.1016/s0896-1549(05)70248-0. [DOI] [PubMed] [Google Scholar]
- 7.Kurland LT, Molgaard CA. The patient record in epidemiology. Sci Am. 1981;245:54–63. doi: 10.1038/scientificamerican1081-54. [DOI] [PubMed] [Google Scholar]
- 8.Kaplan EME. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–81. [Google Scholar]
- 9.Aponte EP, Diehl N, Mohney BG. Incidence and clinical characteristics of childhood glaucoma: A population-based study. Arch Ophthalmol. 2010;128:478–82. doi: 10.1001/archophthalmol.2010.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stamper RL, Wigginton SA, Higginbotham EJ. Primary drug treatment for glaucoma: Beta-blockers versus other medications. Surv Ophthalmol. 2002;47:63–73. doi: 10.1016/s0039-6257(01)00286-7. [DOI] [PubMed] [Google Scholar]
- 11.Coppens G, Stalmans I, Zeyen T, Casteels I. The safety and efficacy of glaucoma medication in the pediatric population. J Pediatr Ophthalmol Strabismus. 2009;46:12–18. doi: 10.3928/01913913-20090101-05. [DOI] [PubMed] [Google Scholar]
- 12.Radius RL, Diamond GR, Pollack IP, Langham ME. Timolol: A new drug for management of chronic simple glaucoma. Arch Ophthalmol. 1978;96:1003–8. doi: 10.1001/archopht.1978.03910050527005. [DOI] [PubMed] [Google Scholar]
- 13.Moore W, Nischal KK. Pharmacologic management of glaucoma in childhood. Paediatr Drugs. 2007;9:71–9. doi: 10.2165/00148581-200709020-00001. [DOI] [PubMed] [Google Scholar]
- 14.Russell-Eggitt I. In defence of goniotomy. Br J Ophthalmol. 1995;79:709. doi: 10.1136/bjo.79.7.709-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khaw PT. What is the best primary surgical treatment for the infantile glaucomas? Br J Ophthalmol. 1996;80:495–6. doi: 10.1136/bjo.80.6.495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ho CL, Walton DS. Primary congenital glaucoma: 2004 update. J Pediatr Ophthalmol Strabismus. 2004;41:271–88. doi: 10.3928/01913913-20040901-11. quiz 300-301. [DOI] [PubMed] [Google Scholar]
- 17.Alsheikheh A, Klink J, Klink T, Steffen H, Grehn F. Long-term results of surgery in childhood glaucoma. Graefes Arch Clin Exp Ophthalmol. 2007;245:195–203. doi: 10.1007/s00417-006-0415-2. [DOI] [PubMed] [Google Scholar]
- 18.Wallace DK, Plager DA, Snyder SK, Raiesdana A, Helveston EM, Ellis FD. Surgical results of secondary glaucomas in childhood. Ophthalmology. 1998;105:101–11. doi: 10.1016/s0161-6420(98)91519-6. [DOI] [PubMed] [Google Scholar]
- 19.Autrata R, Helmanova I, Oslejskova H, Vondracek P, Rehurek J. Glaucoma drainage implants in the treatment of refractory glaucoma in pediatric patients. Eur J Ophthalmol. 2007;17:928–37. doi: 10.1177/112067210701700610. [DOI] [PubMed] [Google Scholar]
- 20.Budenz DL, Gedde SJ, Brandt JD, Kira D, Feuer W, Larson E. Baerveldt glaucoma implant in the management of refractory childhood glaucomas. Ophthalmology. 2004;111:2204–10. doi: 10.1016/j.ophtha.2004.05.017. [DOI] [PubMed] [Google Scholar]
- 21.Papadopoulos M, Cable N, Rahi J, Khaw PT. The British Infantile and Childhood Glaucoma (BIG) Eye Study. Invest Ophthalmol Vis Sci. 2007;48:4100–106. doi: 10.1167/iovs.06-1350. [DOI] [PubMed] [Google Scholar]
- 22.Freedman SF, Rodriguez-Rosa RE, Rojas MC, Enyedi LB. Goniotomy for glaucoma secondary to chronic childhood uveitis. Am J Ophthalmol. 2002;133:617–21. doi: 10.1016/s0002-9394(02)01344-2. [DOI] [PubMed] [Google Scholar]
- 23.Kremers HM, Myasoedova E, Crowson CS, Savova G, Gabriel SE, Matteson EL. The Rochester Epidemiology Project: Exploiting the capabilities for population-based research in rheumatic diseases. Rheumatology. 2011;50:6–15. doi: 10.1093/rheumatology/keq199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wolfs RC, Borger PH, Ramrattan RS, et al. Changing views on open-angle glaucoma: definitions and prevalences—the Rotterdam Study. Invest Ophthalmol Vis Sci. 2000;41:3309–21. [PubMed] [Google Scholar]