Abstract
AIM
To evaluate whether selective serotonin re-uptake inhibitor (SSRI) exposure influences the risk of myocardial infarction (MI) in patients with depression.
METHODS
This study included 693 patients with MI (cases) and 2772 controls. Conditional logistic regression was used to calculate the odds ratio (OR).
RESULTS
SSRI exposure may be associated with a reduced MI risk (OR = 0.77, 95% CI 0.57, 1.03). However, reduced risk was only observed with longer term use (OR = 0.73, 95% CI 0.53, 1.00) and not with shorter term use (OR = 1.15, 95% CI: 0.65, 2.05).
CONCLUSIONS
Only longer term use of SSRIs was associated with reduced MI risk, suggesting that other mechanisms, besides an acute anti-platelet effect, may reduce MI risk.
Keywords: antidepressant medication, epidemiology, myocardial infarction, serotonin re-uptake inhibitors
WHAT IS ALREADY KNOWN ABOUT THIS SUBJECT
Depression is associated with an increased risk of cardiovascular disease. Some studies, but not all, have identified an association between use of selective serotonin re-uptake inhibitors (SSRIs) and reduced risk of myocardial infarction (MI). There may be a difference among SSRIs based on their affinity for the serotonin receptor.
WHAT THIS STUDY ADDS
Current use of SSRIs by patients with depression may be associated with a reduced risk of MI. However, the risk seemed to be reduced only with longer term use of SSRIs. In addition, we did not observe a relationship between the affinity of SSRIs for the serotonin transporter and risk of MI.
Introduction
Depression is associated with an increased risk of cardiovascular morbidity and mortality [1]. Proposed mechanisms for the increased risk in people with depression, include life-style factors (such as smoking) and increased platelet activation [2]. Long term treatment with antidepressants might reduce cardiovascular risk by alleviating depression. In addition, selective serotonin re-uptake inhibitor (SSRI) antidepressants may provide additional benefit by inhibiting the increased platelet activation in depressed patients [3]. Some studies [4–6], but not all [7–10], have identified an association between SSRIs compared with non-use and reduced risk of MI. A potential limitation of these studies is that the results might have been biased by confounding by depression.
Therefore, we sought to determine, in a population of patients with a diagnosis of depression, the association of SSRI use with MI and whether there are differences among SSRIs. Our hypothesis was that shorter term exposure to SSRIs would reduce the risk of MI via their acute antiplatelet effects.
Methods
Study population
Data for this case-control study were derived from the UK General Practice Research Database (GPRD) from 1989 to 2002. GPRD is a computerized database of anonymized longitudinal medical records of over 8 million residents in the UK. All patients with a first diagnosis of depression that was recorded at least 1 year after registration with a practice were included in this study. The rationale for including only patients with a diagnosis of depression was to reduce confounding by disease indication. Patients whose first depression diagnosis was recurrent depression or who had a diagnosis for another severe mental health disorder (e.g. schizophrenia) prior to or on the same day as their first diagnosis of depression were excluded.
This study was approved by the University of Pennsylvania Institutional Review Board and the Scientific and Ethical Advisory Group of the GPRD.
Selection of cases and controls
The cohort was followed forward in time after the first diagnosis of depression until one of three events occurred: the subject had a first-recorded diagnosis of MI (cases), follow-up ended or the subject had a censoring event. Censoring events included death and diagnoses of ventricular arrhythmias or sudden death, hypertrophic cardiomyopathy, heart transplantation, myocarditis, infiltrative cardiomyopathies, malignancy of the heart and diagnoses of other severe mental health disorders.
The recorded date of the MI event was considered the index date. For each case, we identified, at random, four controls matched on age in 5 year increments, gender and duration of follow-up from the first diagnosis of depression until the index date using incidence density sampling.
Exposure definition
Antidepressant (SSRI and non-SSRI) users were defined as people whose antidepressant prescription lasted until the index date. All other patients were considered to be non-antidepressant users.
Paroxetine, sertraline, fluoxetine, citalopram and fluvoxamine were classified as SSRIs. SSRIs were also categorized by their affinity for the serotonin transporter, i.e. high affinity: paroxetine, sertraline and fluoxetine and moderate affinity: citalopram and fluvoxamine [11]. All other antidepressants were considered to be non-SSRI agents. Because venlafaxine exhibits serotonin inhibition, as well as other actions, we performed a sensitivity analysis in which we included venlafaxine along with SSRIs.
Patients simultaneously exposed to both SSRIs and non-SSRIs at their index date were excluded.
Analysis
Conditional logistic regression was used to estimate the odds of MI in SSRI users compared with non-users of any antidepressant. Known risk factors for MI as well as variables that changed the unadjusted OR by at least 10% after adjustment were included in the multivariable models to adjust for confounding [12].
Results
There were 128 116 subjects identified with a first diagnosis of depression who did not meet the exclusion criteria. Among them, 693 patients had a subsequent MI (cases) and they were matched to 2772 controls.
The adjusted OR for MI among current SSRI users vs. non-users was 0.77 (95% confidence interval [CI] 0.57, 1.03, P = 0.08) (Table 1). The adjusted OR was essentially unchanged when including venlafaxine with SSRIs (OR 0.76, 95% CI 0.57, 1.01) (Table 1). Among users of non-SSRI antidepressants the adjusted OR was 0.89 (95% CI 0.67, 1.19, P = 0.44).
Table 1.
Odds ratio for myocardial infarction by SSRI use
| Current antidepressant use | Cases (n = 693) | Controls (n = 2772) | Adjusted odds ratio* (95% confidence interval) | P |
|---|---|---|---|---|
| None | 497 | 1985 | 1.00 (Reference) | |
| SSRI | 89 | 360 | 0.77 (0.57, 1.03) | 0.08 |
Adjusted for: history of hypertension, diabetes, hypercholesterolaemia, congestive heart failure, stroke, ischaemic heart disease, rheumatoid arthritis, obstructive lung disease or aortic stenosis, use of aspirin or nitrates and number of prior medication prescriptions. Other variables, such as smoking and body mass index, did not alter the ORs. SSRI, selective serotonin re-uptake inhibitors.
Current SSRI users without a second SSRI prescription in the 90 days prior to the index date (‘shorter term use’) had an OR of 1.15 (95% CI 0.65, 2.05), while current SSRI users with ≥1 additional SSRI prescription in the preceding 90 days (‘longer term use’) had an OR of 0.73 (95% CI 0.53, 1.00).
No consistent relationship was observed between SSRI affinity and odds of MI (moderate affinity OR 0.53, 95% CI 0.29, 0.99 and high affinity OR 0.83, 95% CI 0.61, 1.14 vs. non-users; multiplicative interaction P = 0.18). In addition, although the ORs among individual SSRIs seemed to vary (Figure 1), the global test of any differences among the different SSRIs was not statistically significant (P = 0.11).
Figure 1.
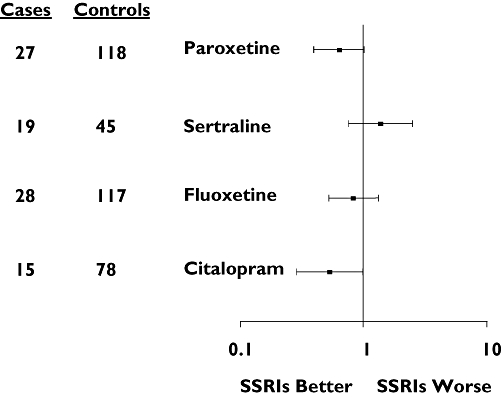
Adjusted odds ratio (squares) and 95% confidence intervals (bars) for myocardial infarction comparing selective serotonin re-uptake inhibitor use with no antidepressant use. Odds ratios are adjusted for all variables as described in the text
Discussion
In this study, depressed patients who were longer term users of SSRIs had lower odds of MI than depressed patients without an active antidepressant prescription. Shorter term use of SSRIs was not associated with reduced risk of MI, suggesting that longer term use may be required for beneficial effects of SSRIs. Further, no relationship was observed between affinity for the serotonin receptor and odds of MI.
There are three primary limitations of the study. First, GPRD relies on physician prescribing and therefore, some of the ‘current users’ of SSRIs in our study may not have been taking the prescribed antidepressant, which may have led to underestimation of the protective effects of SSRIs on MI risk. Second, because other antidepressants may have adverse effects among those with existing cardiovascular disease, it is possible that SSRIs were used in higher risk patients which could have biased our results towards the null, despite adjustment for available confounders. Third, our results may have been confounded by the severity of depression, biasing the results away from demonstrating a protective effect of SSRIs.
Within the context of the limitations of observational research, our results suggest that there may be a difference between shorter term and longer term use of SSRIs and the risk of MI. These results raise the possibility that an inhibition of platelet effect by SSRIs may not be primarily or solely responsible for the reduction of the risk of MI among depressed patients.
Acknowledgments
The authors acknowledge Sandy Barile for editorial assistance. This work was supported by a grant from GlaxoSmithKline (GSK). The funding agency was not involved in the conduct of the study, nor were they directly involved with the analysis or interpretation of the data.
Competing Interests
Dr Kimmel has received research funding from Pfizer and GlaxoSmithKline and served as a consultant for Pfizer and GlaxoSmithKline, all unrelated to SSRIs. Dr Schelleman has had travel to scientific conferences paid for by pharmacoepidemiology training funds contributed by pharmaceutical manufacturers. Drs Berlin and Weinstein are full-time employees of Johnson & Johnson Pharmaceutical Research and Development. Both were full-time employees of the University of Pennsylvania at the time this work was conducted. Dr. Berlin is a shareholder in Johnson & Johnson. Dr Lewis has received research funding from Pfizer and GlaxoSmithKline and served as a consultant for Pfizer and GlaxoSmithKline. Ms Kinman and Drs Oslin and Sauer have no conflicts to declare.
REFERENCES
- 1.Ford DE, Mead LA, Chang PP, Cooper-Patrick L, Wang NY, Klag MJ. Depression is a risk factor for coronary artery disease in men: the Precursors Study. Arch Intern Med. 1998;158:1422–6. doi: 10.1001/archinte.158.13.1422. [DOI] [PubMed] [Google Scholar]
- 2.Musselman DL, Marzec UM, Manatunga A, Penna S, Reemsnyder A, Knight BT, Baron A, Hanson SR, Nemeroff CB. Platelet reactivity in depressed patients treated with paroxetine: preliminary findings. Arch Gen Psychiatry. 2000;57:875–82. doi: 10.1001/archpsyc.57.9.875. [DOI] [PubMed] [Google Scholar]
- 3.Hergovich N, Aigner M, Eichler HG, Entlicher J, Drucker C, Jilma B. Paroxetine decreases platelet serotonin storage and platelet function in human beings. Clin Pharmacol Ther. 2000;68:435–42. doi: 10.1067/mcp.2000.110456. [DOI] [PubMed] [Google Scholar]
- 4.Sauer WH, Berlin JA, Kimmel SE. Selective serotonin reuptake inhibitors and myocardial infarction. Circulation. 2001;104:1894–8. doi: 10.1161/hc4101.097519. [DOI] [PubMed] [Google Scholar]
- 5.Sauer WH, Berlin JA, Kimmel SE. Effect of antidepressants and their relative affinity for the serotonin transporter on the risk of myocardial infarction. Circulation. 2003;108:32–6. doi: 10.1161/01.CIR.0000079172.43229.CD. [DOI] [PubMed] [Google Scholar]
- 6.Schlienger RG, Fischer LM, Jick H, Meier CR. Current use of selective serotonin reuptake inhibitors and risk of acute myocardial infarction. Drug Saf. 2004;27:1157–65. doi: 10.2165/00002018-200427140-00006. [DOI] [PubMed] [Google Scholar]
- 7.Meier CR, Schlienger RG, Jick H. Use of selective serotonin reuptake inhibitors and risk of developing first-time acute myocardial infarction. Br J Clin Pharmacol. 2001;52:179–84. doi: 10.1046/j.0306-5251.2001.01426.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Monster TB, Johnsen SP, Olsen ML, McLaughlin JK, Sorensen HT. Antidepressants and risk of first-time hospitalization for myocardial infarction: a population-based case-control study. Am J Med. 2004;117:732–7. doi: 10.1016/j.amjmed.2004.06.027. [DOI] [PubMed] [Google Scholar]
- 9.Tata LJ, West J, Smith C, Farrington P, Card T, Smeeth L, Hubbard R. General population based study of the impact of tricyclic and selective serotonin reuptake inhibitor antidepressants on the risk of acute myocardial infarction. Heart. 2005;91:465–71. doi: 10.1136/hrt.2004.037457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blanchette CM, Simoni-Wastila L, Zuckerman IH, Stuart B. A secondary analysis of a duration response association between selective serotonin reuptake inhibitor use and the risk of acute myocardial infarction in the aging population. Ann Epidemiol. 2008;18:316–21. doi: 10.1016/j.annepidem.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 11.van Walraven C, Mamdani MM, Wells PS, Williams JI. Inhibition of serotonin reuptake by antidepressants and upper gastrointestinal bleeding in elderly patients: retrospective cohort study. BMJ. 2001;323:655–8. doi: 10.1136/bmj.323.7314.655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mickey RM, Greenland S. The impact of confounder selection criteria on effect estimation. Am J Epidemiol. 1989;129:125–37. doi: 10.1093/oxfordjournals.aje.a115101. [DOI] [PubMed] [Google Scholar]


