Obstructive sleep apnea (OSA) is a common condition characterized by recurrent collapse of the upper airway during sleep. Clinical studies performed over the last decade have shown that OSA is associated with cardiovascular morbidity and mortality (1, 2). The pathogenesis of cardiovascular complications of OSA is not fully understood, but several mechanisms have been implicated, including increased sympathetic activity, oxidative stress, systemic inflammation resulting in insulin resistance, hypertension, and endothelial dysfunction (3). Recent studies in animal models have identified dysregulation of lipid metabolism and dyslipidemia as a potentially important mediator of accelerated atherogenesis in OSA (4, 5). However, clinical evidence on causal relationships between OSA and dyslipidemia remains contradictory.
There are several reports related to the impact of OSA on fasting lipid levels; however, post-prandial levels of plasma lipids have not been previously assessed.
Post-prandial hypertriglyceridemia has recently been linked to increased cardiovascular morbidity and mortality (6–8) that is attributed to accumulation of atherogenic remnants of triglyceride-rich chylomicrons. In contrast, fasting triglycerides have not been attributed to significant cardiovascular risk (9). Therefore, examining the effect of OSA and subsequent treatment on post-prandial lipid levels is of significant research interest.
In this issue, Phillips and colleagues (pp. 355) provided the first data on the impact of moderate to severe OSA on lipid metabolism in humans (10). The authors conducted the first randomized placebo-controlled crossover trial measuring the effect of continuous positive pressure (CPAP) therapy for 2 months on plasma lipids over 24 hours as a primary outcome. The participants received standard meals in the controlled environment, and the effects of therapeutic and sham CPAP treatments were compared. Assessment of lipid metabolism during both waking and sleep was undertaken with seven blood samples drawn across the 24-hour study period. CPAP treatment did not modify fasting lipid levels. In both treatment groups, 24-hour triglyceride levels peaked at 2:00 p.m., 5 to 6 hours after breakfast, and at 3:00 a.m., 6 to 7 hours after dinner. Therapeutic levels of CPAP markedly decreased post-prandial hypertriglyceridemia. In addition, CPAP therapy lowered fasting and nonfasting total cholesterol levels.
It should be noted that the effect of CPAP on post-prandial hyperlipidemia was relatively modest and mostly attributable to a reduction of triglyceride levels at two time points, 2:00 p.m. and 3:00 a.m. The effects of CPAP could have been impacted by the following methodological issues. First, the compliance with CPAP treatment was not ideal with the mean use of 4.4 hours/night. Second, the usual peak of triglyceride concentration is 4 hours after a meal (7). Unfortunately, no single blood draw coincided with the potential biological peak of post-prandial triglycerides. Finally, patients were awakened from sleep for the blood draws resulting in sleep fragmentation and possibly stress related to the venipuncture. This could have been avoided if an indwelling venous catheter was utilized.
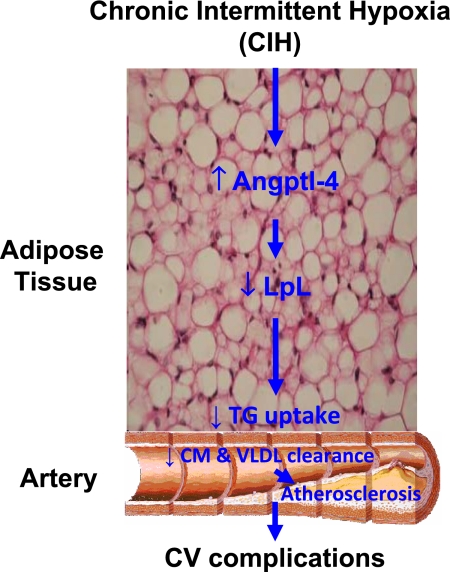
How could OSA promote post-prandial hyperlipidemia? Recent translational research provides some clues. Post-prandial lipid levels are determined by the degree of chylomicron intestinal absorption and clearance. Our group has recently examined post-prandial lipid metabolism in a mouse model of chronic intermittent hypoxia (CIH) that mimics the oxygen profile in patients with severe OSA (11). Mice were exposed to 4 weeks of CIH or control conditions followed by gavage of retinyl palmitate to measure chylomicron clearance. Compared with control, CIH caused a rapid peak of retinol ester concentration with a slow decline suggesting that intestinal absorption remained intact, whereas clearance of chylomicrons from bloodstream was impaired. Poor clearance of chylomicrons during CIH was accompanied by elevation of fasting very-low-density lipoproteins, suggesting that CIH inhibits clearance of triglyceride-rich lipoproteins through a common pathway. This common pathway is likely mediated by lipoprotein lipase (LPL), a key enzyme responsible for the hydrolysis of core triglycerides in chylomicrons and very-low-density lipoproteins (12). CIH induced a striking 80% decrease in LPL activity in adipose tissue. CIH also increased mRNA and protein levels of a potent LPL inhibitor, angiopoietin-like protein 4, in adipose tissue, suggesting a potential mechanism of LPL inactivation (Figure 1).
Figure 1.
Effects of chronic intermittent hypoxia (CIH) on lipoprotein clearance. CIH inhibits triglyceride-rich lipoprotein clearance (chylomicrons [CM] and very-low-density lipoprotein [VLDL]) by activating angiopoietin-like protein-4 (Angptl-4), a potent inhibitor of lipoprotein lipase (LpL) in the adipose tissue. The decrease in the LpL activity, an enzyme that is anchored at the capillary endothelium, promotes a significant decrease in the hydrolysis of triglycerides into free fatty acids from CM and VLDL particles. The consequence of the LpL inhibition is the prolonged circulation of CM and VLDL in the bloodstream that may favor the progression of atherosclerosis.
In conclusion, Phillips and colleagues (10) have shown that in humans with OSA, post-prandial lipids are elevated and favorably impacted by CPAP. Emerging translational research suggests that dysregulation of lipid metabolism in OSA is an important additional mediator of atherosclerotic burden. Treatment with CPAP may modify this atherosclerotic risk in addition to the previously reported effects on pathways mediating sympathetic activity, oxidative stress, and systemic inflammation.
Footnotes
Author Disclosure: V.P.’s institution has received a grant from the American Heart Association, and the ResMed Foundation. L.D. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript.
References
- 1.Punjabi NM, Caffo BS, Goodwin JL, Gottlieb DJ, Newman AB, O'Connor GT, Rapoport DM, Redline S, Resnick HE, Robbins JA, et al. Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med 2009;6:e1000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marin JM, Carrizo SJ, Vicente E, Augusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 2005;365:1046–1053 [DOI] [PubMed] [Google Scholar]
- 3.Bradley TD, Floras JS. Obstructive sleep apnoea and its cardiovascular consequences. Lancet 2009;373:82–93 [DOI] [PubMed] [Google Scholar]
- 4.Savransky V, Nanayakkara A, Li J, Bevans S, Smith PL, Rodriguez A, Polotsky VY. Chronic intermittent hypoxia induces atherosclerosis. Am J Respir Crit Care Med 2007;175:1290–1297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Savransky V, Jun J, Li J, Nanayakkara A, Fonti S, Moser AB, Steele KE, Schweitzer MA, Patil SP, Bhanot S, et al. Dyslipidemia and atherosclerosis induced by chronic intermittent hypoxia are attenuated by deficiency of stearoyl coenzyme A desaturase. Circ Res 2008;103:1173–1180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eberly LE, Stamler J, Neaton JD; Multiple Risk Factor Intervention Trial Research Group Relation of triglyceride levels, fasting and nonfasting, to fatal and nonfatal coronary heart disease. Arch Intern Med 2003;163:1077–1083 [DOI] [PubMed] [Google Scholar]
- 7.Nordestgaard BG, Benn M, Schnohr P, Tybjaerg-Hansen A. Nonfasting triglycerides and risk of myocardial infarction, ischemic heart disease, and death in men and women. JAMA 2007;298:299–308 [DOI] [PubMed] [Google Scholar]
- 8.Bansal S, Buring JE, Rifai N, Mora S, Sacks FM, Ridker PM. Fasting compared with nonfasting triglycerides and risk of cardiovascular events in women. JAMA 2007;298:309–316 [DOI] [PubMed] [Google Scholar]
- 9.Miller M, Stone NJ, Ballantyne C, Bittner V, Criqui MH, Ginsberg HN, Goldberg AC, Howard WJ, Jacobson MS, Kris-Etherton PM, et al. ; American Heart Association Clinical Lipidology Thrombosis, and Prevention Committee of the Council on Nutrition, Physical Activity, and Metabolism, Council on Arteriosclerosis, Thrombosis and Vascular Biology, Council on Cardiovascular N. Triglycerides and Cardiovascular Disease. A scientific statement from the American Heart Association. Circulation 2011;123:2292–2333 [DOI] [PubMed] [Google Scholar]
- 10.Phillips CL, Yee BJ, Marshall NS, Liu PY, Sullivan DR, Grunstein RR. Continuous positive airway pressure reduces post-prandial lipidemia in obstructive sleep apnea. A randomized, placebo-controlled crossover trial. Am J Respir Crit Care Med 2011;184:355–361 [DOI] [PubMed] [Google Scholar]
- 11.Drager LF, Li J, Shin MK, Reinke C, Aggarwal NR, Jun JC, Bevans-Fonti S, Sztalryd C, O'Byrne SM, Kroupa O, et al. Intermittent hypoxia inhibits clearance of triglyceride rich lipoproteins and inactivates adipose lipoprotein lipase in a mouse model of sleep apnea. Eur Heart J (In press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dallinga-Thie GM, Franssen R, Mooij HL, Visser ME, Hassing HC, Peelman F, Kastelein JJ, Péterfy M, Nieuwdorp M. The metabolism of triglyceride-rich lipoproteins revisited: new players, new insight. Atherosclerosis 2010;211:1–8 [DOI] [PMC free article] [PubMed] [Google Scholar]