Abstract
Objective. To provide doctor of pharmacy (PharmD) students with highly integrated, comprehensive and up-to-date instruction related to the pharmacology of antiarrhythmic drugs.
Design. Students were taught the medicinal chemistry, pharmacology, and therapeutics of antiarrhythmic agents in the cardiology module presented in quarter 7 of the PharmD curriculum. Important foundational information for this topic was presented to students in prerequisite physiology courses and pathophysiology courses offered earlier in the curriculum. Emphasis was placed on student critical thinking and active involvement. Weekly recitation sessions afforded students the opportunity to apply the information they learned regarding arrhythmia pharmacotherapy to comprehensive patient cases.
Assessment. Student comprehension was measured using class exercises, short quizzes, case write-ups, comprehensive examinations, group exercises, and classroom discussion. Students were afforded the opportunity to evaluate the course, and the instructors as well as rate the degree to which the course achieved its educational outcomes.
Conclusion. Students learned about cardiac arrhythmias through a high-quality, interdisciplinary series of classes presented by faculty members with extensive experience related to the pharmacology and pharmacotherapy of cardiac arrhythmias.
Keywords: arrhythmia, antiarrhythmic agents, pharmacology, integrated curriculum
INTRODUCTION
Death rates from cardiovascular causes have declined steadily over the last 25 years, however, death from cardiovascular disease remains the number one killer in developed countries. Sudden cardiac death from cardiac arrhythmia still accounts for several hundred thousand deaths each year, despite advances in emergency medicine.1 Atrial fibrillation remains the most common cardiac arrhythmia and is expected to affect nearly 30 million individuals in North America and Europe by 2050.2 Patients with atrial fibrillation have a significantly increased risk of stroke and thromboembolic events, which results in an overall increase in mortality.2,3
Factors that can lead to the development of cardiac arrhythmias include myocardial ischemia, electrolyte abnormalities, cardiomyopathy, and altered autonomic tone. The role of genetic variability in ion channels also has been linked to the development of arrhythmias in otherwise healthy individuals.4,5 Also, numerous drugs, including many antiarrhythmic agents, can cause cardiac arrhythmia.
The pharmacotherapy of cardiac arrhythmia is a complex topic. There are many different types of cardiac arrhythmias and often the etiology of these arrhythmias may be uncertain. In addition, patients can present with more than one type of arrhythmia or conduction defect that may be superimposed upon myocardial ischemia or altered cardiac function. There are dozens of drugs used to treat cardiac arrhythmias. Many of these agents have complex pharmacokinetic profiles, multiple mechanisms of action, and numerous potential side effects.
All of these factors highlight the important role that knowledgeable pharmacists can play in managing arrhythmia pharmacotherapy. In addition to extensive knowledge about the drugs themselves, pharmacists’ expertise in drug pharmacokinetics can be vital to the safe and effective dosing of antiarrhythmic drugs. Many patients with cardiac arrhythmias also are likely to have other cardiovascular comorbidities and, as a result, may be taking numerous other medications for angina, hypertension, anticoagulation, etc. Pharmacists can be of great value in identifying potential drug interactions and preventing possible adverse effects in patients taking multiple medications.
An integrated approach to teaching PharmD students about cardiac arrhythmias is presented. To have a thorough understanding of cardiac arrhythmias, students must be competent in their knowledge of cardiovascular physiology and pathophysiology, as well as the medicinal chemistry, pharmacology, pharmacokinetics, and therapeutics of cardiovascular agents. Emphasis is placed on active student learning and extensive application of their knowledge to patient-based case studies. In order for this integrated instructional approach to work effectively, there must be excellent communication and interaction among the instructors teaching the various disciplines and multiple points of student/knowledge assessment to ensure that the topic is being delivered effectively throughout the curriculum.
DESIGN
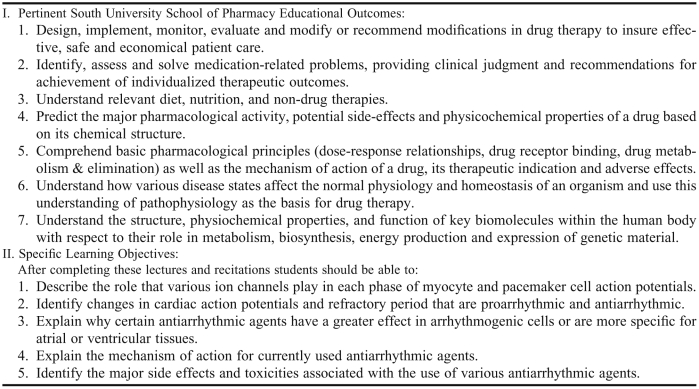
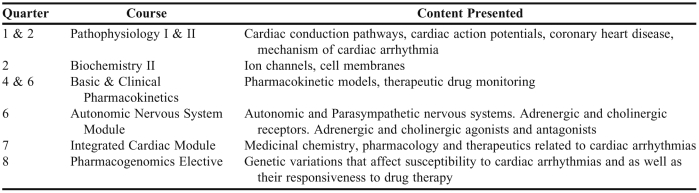
The South University School of Pharmacy's educational outcomes related to content on the pharmacotherapy of arrhythmias are listed in Table 1, along with the course-specific learning objectives for content on the pharmacology of antiarrhythmic drugs. Students entering the PharmD program were required to complete prerequisite courses in anatomy and physiology, where they learned the basics of cardiac structure and function. In quarters 1 and 2 of the PharmD program, students completed 9 quarter hours of pathophysiology (Table 2). Twenty classroom hours of pathophysiology were dedicated to diseases of the cardiovascular system, including arrhythmia. In pathophysiology, a review of cardiac conduction pathways and action potentials of pacemaker and myocyte cells was presented to the students. Emphasis was placed on the role that specific ions play in each phase of the action potentials of both cell types as many of the antiarrhythmic drugs to be discussed have their actions at these ion channels. Students then learned about the various molecular and cellular mechanisms responsible for the occurrence of arrhythmias, as well as factors that can predispose a patient to the development of arrhythmias. The various types of atrial and ventricular arrhythmias also were discussed along with sample electrocardiogram tracings showing the characteristic changes that are observed with each arrhythmia. Some antiarrhythmic agents exhibit complex pharmacokinetic profiles. In quarter 4, students also began the pharmacokinetics sequence, which provided them with a detailed knowledge of both theoretical and clinical drug kinetics. Much of the material in the pharmacokinetics sequence was taught using a problem-based learning model that emphasized student critical thinking and clinical application.
Table 1.
General Educational Outcomes and Specific Learning Objectives for the Pharmacology of Cardiac Arrhythmias
Table 2.
Content in the Curriculum at the South University School of Pharmacy Related to Cardiac Arrhythmias
Study of integrated sequence modules based on specific organ systems began in quarter 3 and presented students with integrated content on the pharmacology, medicinal chemistry, and therapeutics of various related drug classes and disease states. The integrated sequence module on the autonomic nervous system was completed in quarter 6 and served as an important precursor to the integrated sequence cardiology module in quarter 7, where the bulk of information related to cardiac arrhythmia pharmacotherapy was presented. In the autonomic nervous system module, students learned about the autonomic regulation of the heart as well as the pharmacology, medicinal chemistry, and therapeutics of drugs, such as beta blockers, catecholamines, lidocaine, and atropine, which have application in the treatment of cardiac arrhythmia's.
The cardiology integrated sequence module was presented in quarter 7 of the curriculum. It was the largest module in the integrated sequence and was allotted 7 quarter hours. Topics covered in the module included, hypertension, dyslipidemia, coronary heart disease, coagulation, heart failure, and cardiac arrhythmias. Content in each area was presented in a highly integrated format that included pharmacology, medicinal chemistry, and therapeutics. Content related to cardiac arrhythmias was presented at the end of this module and included 8 hours of classroom time. The cardiology integrated sequence module was offered in the same quarter as the renal integrated sequence module. This was planned because drug classes such as diuretics, angiotensin-converting enzyme inhibitors, and angiotensin receptor blockers used to treat cardiovascular disease have their target of action at the kidney or through modulating the renin-angiotensin system. The renal integrated sequence module also addressed the correction of electrolyte disturbances, which also can exacerbate cardiac arrhythmias. In the Pharmacogenomics elective course (quarter 8), students learn about various genetic variations in enzymes and targets that can affect the occurrence of cardiac arrhythmias, as well as their responsiveness to drug therapy.
Each of the integrated sequence modules also included a weekly 3-hour recitation session in which students worked thorough patient-based case studies in small groups. Faculty members from the Department of Pharmaceutical Sciences were responsible for delivering the pharmacology and medicinal chemistry of drugs used to treat cardiac arrhythmia, while clinical faculty members from the Department of Pharmacy Practice presented the therapeutics of arrhythmia. A clinical pharmacist who specialized in treating cardiac arrhythmia came in from a local university teaching hospital to present this therapeutic block.
Pedagogy
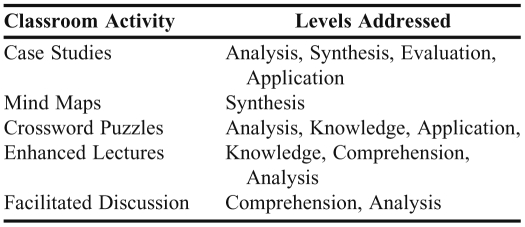
Starting with the quarter 1 course in pathophysiology and continuing into the pharmacology lecture in the cardiology integrated sequence module, a concerted effort was made to incorporate classroom and recitations strategies designed to target multiples levels of student learning (Table 3). These activities included interactive case vignettes, mind-mapping exercises, flowchart fill-in-the-blank items, comprehension check questions, crossword puzzles, and facilitated discussions. Mind maps and flow charts are well-suited to cardiology topics and allow students to visually make key connections and integrate related concepts. The case vignettes that were embedded in the lecture presentation were designed to emphasize a certain point in the material being discussed and usually took no more than 5 to 10 minutes of class time to work through. Crossword puzzles were generally used to help teach students important definitions and terminology. Several other active-learning exercises have been used in other integrated sequence courses, including the Aronson's jigsaw puzzle cooperative learning technique6-9 and the “Wall of Excellence”10 and could be incorporated into the cardiology module in the future.
Table 3.
Classroom Activities and Critical Thinking
A Klickerz (Turning Technologies, Youngstown, Ohio) audience response system was added to the classroom in 2010. This user-friendly system allowed faculty members to embed various types of review questions into their PowerPoint presentations and receive instant feedback regarding student comprehension of a particular topic. These devices were particularly valuable for engaging students at the distance campus as the instructor could verbally direct questions to that particular campus and encourage students’ feedback and involvement.11 In cardiology, the audience response system was used with embedded review questions to check class understanding of key case study points, to review old examination questions, and to give in-class quizzes. Students on both campuses were able to view a graphical representation of how many individuals chose each of the answers for a particular question, along with the highlighted correct answer.
Each week, the integrated sequence modules included a 3-hour recitation session. These recitation sections were facilitated by a cardiology clinical faculty member and required students to work through patient cases in a small-group setting. Often, case studies and related literature was posted prior to the recitation so students could begin reviewing the case and gathering the resources they would need for the recitation sessions. Generally, students were required to submit their final work from recitation for review and grading. In the 2011 iteration of the cardiology module, 10-question quizzes were added to the beginning of the recitation sessions. These questions related to material covered in the prior week's lectures as well as questions from material that would be covered that day to encourage students to review past material and prepare for the recitation session.
The Pharmacology of Antiarrhythmic Drugs – Overview of Lecture Content
Cardiac Action Potentials and Conduction Pathways. The pathophysiology and underlying mechanisms by which cardiac arrhythmia occur were covered in detail in the pathophysiology sequence. Students were given access to pathophysiology notes at the beginning of the integrated sequence cardiology portion related to treating cardiac arrhythmias. Approximately 30 minutes of class time at the beginning of the antiarrhythmic drugs section was dedicated to reviewing cardiac action potentials and the cardiac conduction pathways. In order for the students to comprehend the mechanism(s) by which many antiarrhythmic drugs exert their effect, students must thoroughly understand different phases of cardiac myocyte action potentials and the ions/channels that are involved in each phase. Likewise, students must be able to differentiate action potentials of cardiac myocytes (muscle cells) from those of cardiac pacemaker cells sinoatrial and atriventricular nodes because different agents affect different cardiac cell types based on their specificity for various ion channels. Emphasis also was placed on the concept of relative and absolute refractory periods in cardiac cells. Before the presentation of antiarrhythmic agents began, the instructor presented several PowerPoint slides on “modified” action potentials (ie, increased slope of phase 4, increased duration of absolute refractory period, etc) and asked students if the highlighted changes would be pro-arrhythmic or anti-arrhythmic. The goal of this exercise was for students to analyze action potential changes and determine whether those changes would increase activity (ie, firing rate, depolarization rate, repolarization rate, etc) of the cardiac myocytes or pacemaker cells. The class then matched the changes seen in the action potentials with the ion channels that would have to be altered to achieve those changes. This served as an effective lead in to a discussion of the antiarrhythmic agents because they exert their actions at the same channels and yield the same effects on cardiac action potentials.
Antiarrhythmic agents are classified based on their electrophysiologic effect and the various ion channels with which they interact. While this scheme has merit, it is also flawed in that many drugs belonging to the same antiarrhythmic class can have highly diverse actions. This point was emphasized to students as they are most comfortable with neat and clean classification schemes, in which antiarrhythmic drugs unfortunately do not fit.
Agents that Block Sodium Channels (Class I Agents). Antiarrhythmic agents that block sodium channels do so in a state and frequency-dependent manner. State dependent-binding makes many sodium channel blockers more specific for rapidly depolarizing (arrhythmogenic) myocytes because the sodium channels in the membranes of such cells have a greater frequency of activation and inactivation. Some sodium channel blockers (eg, quinidine, procainamide, disopyramide) also block potassium channels, which has the added effect of prolonging the action potential duration and increasing the effective refractory period of cardiac myocytes. These agents are usually classified as belonging to subgroup 1A. Class 1A agents are useful for a variety of atrial and ventricular arrhythmias, but cause a number of potential side effects that limits their overall usefulness.
Sodium channel blockers such as lidocaine and its oral derivative mexiletine are subclassified as 1B agents. They may shorten the duration of the action potential somewhat but do not significantly affect the absolute refractory period. Class 1B agents have little effect on atrial tissues and are mainly used to treat ventricular arrhythmias.
The third subclass of sodium channel blockers is 1C agents, typified by flecanide and propafenone. Both of these agents are potent and long duration sodium channel blockers. Both flecanide and propafenone are used for the treatment of supraventricular arrhythmias.
Agents that block β-adrenergic receptors (Class II Agents). Beta blockers antagonize sympathetic input to pacemaker cells of the heart and thus prolong the refractory period of the AV node. This mechanism makes them particularly useful in terminating re-entrant arrhythmias that involve the AV node as well as in reducing ventricular responsiveness to atrial tachyarrhythmias. These agents also are useful for preventing arrhythmias and decreasing mortality in postmiocardial infarction patients.14
Agents that Prolong the Action Potential (Class III Agents). Drugs that prolong the action potential usually do so by blocking potassium channels and thus slowing the rate of repolarization. Both dofetilide and ibutilide are approved for the treatment of atrial flutter and fibrillation. Sotalol, for example, exerts clear class 3 effects on potassium channels but also exhibits beta receptor blockade. Sotalol is approved for the treatment of ventricular arrhythmias and maintenance of sinus rhythm in patients with atrial fibrillation. Amiodarone is one of the most effective and broad-acting antiarrhythmic agents. Despite its broad range of antiarrhythmic actions, amiodarone use is limited by the potential for multiple, severe toxicities. Dronendarone, a structural analog of amiodarone with similar actions, has been approved for clinical use. The toxicities observed with amiodarone, such as pulmonary fibrosis and corneal deposits, have not been observed with dronendarone. Amiodarone and dronendarone are both used to treat atrial fibrillation and prevent episodes of recurrent ventricular tachycardia.
Agents that Block Calcium Channels (Class IV Agents). Because the depolarization of nodal tissues, such as the SA and AV nodes, are dependent upon the movement of calcium ions, calcium channel blockers such as verapamil and diltiazem exert preferential effects in these tissues. As a result, they both prolong AV node conduction time and refractory. Both also may slow SA node activity to some extent as well. Calcium channel blockers are mainly used in patients with supraventricular tachycardia.
Miscellaneous Agents. There are several antiarrhythmic agents used clinically that have unique modes of action. Adenosine is a naturally occurring nucleoside that is administered intravenously for the conversion of paroxysmal supraventricular tachycardia to sinus rhythm.
Digoxin is a positive inotrope agent that exerts a prominent vagotonic effect. This effect can increase the refractory period of the AV node and thus prevent the passage of reentry impulses or those from atrial fibrillation to the ventricles.
Several new targets and drugs are under investigation for the treatment of cardiac arrhythmias. One of these new agents is the multi-channel blocker vernakalant.15 Similar in action to amiodarone, vernakalant is an atrial-selective agent that appears to be highly effective for the treatment and conversion of atrial fibrillation.
One important new direction in the treatment of cardiac arrhythmias will be the identification of specific genes that encode for ion channels in the human heart. There is considerable evidence that a number of cardiac arrhythmias have a genetic basis that may be related to the expression of ion channel variants with different activities.4,5 Characterization of these genetic variations in ion channels would potentially allow for the development of highly specific agents that are tailored to treat the underlying cause of individual arrhythmias.
EVALUATION AND ASSESSMENT
Numerous in-class exercises to engage students and check their comprehension of the material presented were included during course lectures, eg, comprehension check questions, brief case vignettes, discussion questions, and diagrams/flowcharts with fill-in-the-blank items. These items were interspersed at roughly 20-to 30-minute intervals (a student's average attention span) to help retain student involvement and focus. For the 2010 iteration of the cardiology integrated sequence, the instructor pre-posted a number of “guiding” questions on E-College (Pearson, Centennial, CO) course software related to each block of lecture material. These questions focused on key points in the material and were written to address higher levels of student learning (ie, analyze, recommend, compare and contrast, etc). Students were asked to review and try to answer these questions before coming to class. These questions were then brought up with the class at the specified time in the lecture and served as the basis for higher-level classroom discussions. Examination questions also were based on these guiding questions. The guiding questions were useful to gauge students’ preparation for class and depth of understanding of the material, and to help students realize the level of understanding they would need to do well in the class.
Additional assessment tools included in-class examinations, unannounced quizzes, comprehensive final examinations, and formal written case submissions. Examinations contained a variety of question formats including K-type questions, matching tables, diagram fill-in-the-blank items, case based-questions, and modified K-type questions. Content on examinations in the cardiology integrated sequence was integrated to reflect the integrated nature of the course. Questions related to the pharmacology, medicinal chemistry, and therapeutics of anti-arrhythmic agents were asked. The examinations generally included multiple-choice, matching, and K-type questions. A number of questions were case-based. The mix of examination questions included on a particular test reflected the various levels of learning addressed by the instructors in their objectives. The science and practice course coordinators gathered examination questions from their respective faculty members at least 48 hours in advance, which allowed time for thorough proofreading of the examinations to eliminate typos, redundant questions, and poor questions.
The average score on in-class examinations in the 2010 cardiology module ranged from 78.2 to 82.0 (n = 89 students), while the recitation grade average was 86.0. The average grade for the 3-hour comprehensive examination given at the end of the course was 75%. Students who score below 75% on any of the examinations were required to complete an examination remediation session. A 3-hour period was set aside the week following each examination for students to correct any answers they got wrong on the examination and to write a sentence explaining why the choice they picked was wrong. Because all final examinations in the integrated sequence modules were comprehensive in nature, these remediation sessions gave students an opportunity to improve their comprehension of material that they may have struggled with before encountering it again on the final examination. Student evaluations at the end of the cardiology integrated sequence module were positive and averaged 4.3/5.0 for core course items.
DISCUSSION
Teaching material related to cardiac arrhythmias is definitely challenging. For students to come away with a thorough understanding of the pharmacotherapy of arrhythmias, they must have a solid understanding of cardiac electrophysiology, including conduction pathways and myocyte action potentials. The instructor does a thorough coverage of these topics in Pathophysiology I; however, that occurs in quarter 1 and the cardiology module is in quarter 7. It is helpful to repost the pathophysiology notes on E-College at the beginning of the cardiology module and the instructor has even added a review to this post that focuses specifically on cardiac conduction pathways, action potentials, and ion channels.
When teaching arrhythmias as part of a truly integrated cardiology module, there are logistical and academic issues that must be considered. One of these is redundant presentation of material; another is presentation of material that is not congruent. We generally present the pharmacology of antiarrhythmic agents first, followed by medicinal chemistry and therapeutics. Lecture notes related to arrhythmias are usually posted well in advance of the actual lectures. This gives faculty members teaching in all 3 disciplines time to review the notes of other instructors and remove redundant or faulty information. A second strategy to ensure effective coverage of material is to have course coordinators and faculty members from both the practice and science sides meet prior to the start of the course to decide on content and sequencing of lectures. It is quite helpful when clinical faculty members provide the science instructors with a list of drugs that they use most frequently for a particular condition as this allows the instructor to focus more of the presentation on drugs that students will encounter most frequently in practice. This is particularly true given the number of antiarrhythmic agents that are available and the fact that many are second- or third-line agents in clinical practice.
Because antiarrhythmic pharmacotherapy is a highly complex and evolving topic, it is important for students to be familiar with the latest clinical and pharmacologic studies. Throughout the cardiology integrated sequence module, students are given articles to read that are related to current classroom topics. These articles may be clinical studies, reviews, or science-based research. Students are informed that general questions from these readings may appear on examinations. One of the reasons for having students read these articles is to reemphasize that drug choices are based upon clinical evidence, and that over time drug choices will change as new clinical research data emerges. This is particularly evident with the treatment of cardiac arrhythmias. Required readings also help students realize that they need to become lifelong learners who strive to stay current with pertinent literature. Even the newest textbooks used in class often contain information about drugs that is already out of date or has undergone significant revision. Despite the challenges of teaching about the pharmacology of cardiac arrhythmias, the rewards are great, for example, when students are able to work through complex patient cases in recitation by applying the foundational knowledge they received in pharmacology.
SUMMARY
The pharmacotherapy of cardiac arrhythmias is a topic that many students struggle to master. The subject matter can be daunting due to its high level of complexity and detail. In order to fully understand the etiology of cardiac arrhythmias students need to have a solid understanding of cardiac anatomy, conduction pathways, and myocyte electrophysiology. The mechanism of action for the various classes of antiarrhythmic agents likewise can be difficult for students to comprehend if they do not fully understand cardiac myocyte action potentials and the roles various ions and the autonomic nervous system play in regulating these action potentials. Teaching students about the treatment of cardiac arrhythmias requires starting with basic fundamentals that gradually build upon one another and grow in complexity until, ultimately, students find themselves comfortable with the intricacies and interrelationships that characterize the study of cardiac arrhythmias. This kind of teaching should fully involve students and even be led by students. Fortunately, opportunities abound for stimulating student involvement and active learning with regards to teaching the pharmacology of cardiac arrhythmia.
REFERENCES
- 1.Haissaguerra M, Derval N, Sacher F. Sudden cardiac arrest associated with early repolarization. N Engl J Med. 2008;358(19):2016–2023. doi: 10.1056/NEJMoa071968. [DOI] [PubMed] [Google Scholar]
- 2.Miyasaka Y, Barnes ME, Gerbsch BJ. Secular trends in incidence of atrial fibrillation in Olmstead County Minnesota, 1980-2000 and implications on the projections for future prevalence. Circulation. 2006;114(2):119–125. doi: 10.1161/CIRCULATIONAHA.105.595140. [DOI] [PubMed] [Google Scholar]
- 3.Ohsawa M, Okayama A, Sakata K. Rapid increase in estimated number of persons with atrial fibrillation in Japan. An analysis from national surveys on cardiovascular disease in 1980, 1990 and 2000. J Epidemiol. 2005;15(5):194–196. doi: 10.2188/jea.15.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ruan Y, Liu N, Priori G. Sodium channel mutations and arrhythmias. Nat Rev Cardiol. 2009;6(5):337–348. doi: 10.1038/nrcardio.2009.44. [DOI] [PubMed] [Google Scholar]
- 5.Hedley P, Jorgensen P, Schlamowitz S. The genetic basis of long QT and short QT syndromes: a mutation update. Hum Mutation. 2009;30(11):1486–1511. doi: 10.1002/humu.21106. [DOI] [PubMed] [Google Scholar]
- 6.Aronson E, Patnoe S. The Jigsaw Classroom: Building Cooperation in the Classroom. 2nd ed. New York: Longman; 1997. [Google Scholar]
- 7.Earl GL. Using cooperative learning for a drug information assignment. Am J Pharm Educ. 2009;73(7):Article 132. doi: 10.5688/aj7307132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Persky AM, Pollack GM. A hybrid jigsaw approach to teaching renal clearance concepts. Am J Pharm Educ. 2009;73(3):Article 49. doi: 10.5688/aj730349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stiles AS. Cooperative learning: enhancing individual learning through positive group process. Ann Rev Nurs Ed. 2006;4:131–141. [Google Scholar]
- 10.Doymus K. Teaching chemical equilibrium with the jigsaw technique. Res Sci Educ. 2008;38(2):249–260. [Google Scholar]
- 11.Medina MS, Medina PJ, Wanzer DS, Wilson JE, Nelson E, Britton ML. Use of an audience response system (ARS) in a dual-campus classroom environment. Am J Pharm Educ. 2008;72(2):Article 38. doi: 10.5688/aj720238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cain J, Black EP, Rohr J. An audience response system strategy to improve student motivation, attention and feedback. Am J Pharm Educ. 2009;73(2):21. doi: 10.5688/aj730221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The Cardiac Arrhythmia Suppression Trial (CAST) Investigators. Preliminary report: effect of encainide and flecainide on mortality in a randomized trial of arrhythmia suppression after myocardial infarction. N Engl J Med. 1989;321(3):406–412. doi: 10.1056/NEJM198908103210629. [DOI] [PubMed] [Google Scholar]
- 14.Singh BN. Advantages of beta blockers versus antiarrhythmic agents and calcium antagonists in secondary prevention after myocardial infarction. Am J Cardiol. 1990;66(9):C9–20C. doi: 10.1016/0002-9149(90)90757-r. [DOI] [PubMed] [Google Scholar]
- 15.Dobrev D, Nattel S. New antiarrhythmic drugs for the treatment of atrial fibrillation. Lancet. 2010;375(9721):1212–1223. doi: 10.1016/S0140-6736(10)60096-7. [DOI] [PubMed] [Google Scholar]