Abstract
Objective. To compare student examination performance in pharmacotherapeutics before and after implementation of team-based learning.
Design. After the traditional lecture and workshop method for teaching pharmacotherapeutics was replaced with team-based learning in January 2009, students were expected to come to class having read assigned chapters in order to successfully complete an individual quiz, a group quiz, and group application exercises.
Assessment. Student learning was assessed using performance on individual quizzes, group quizzes, and the examination at the end of the psychiatry module. Students performed as well on the examination at the end of the module as they did prior to team-based learning implementation.
Conclusion. Substituting team-based learning for traditional lecture ensured that students prepared for class and increased student participation in class discussions.
Keywords: team-based learning, pharmacotherapeutics, psychiatry
INTRODUCTION
Team-based learning was initiated in medical education at Baylor College of Medicine in 2001 and has since garnered interest from other areas of health profession education, including nursing, physician assistant, dental, and veterinary schools.1 Colleges and schools of pharmacy also have implemented team-based learning with use reported in instruction within a musculoskeletal system and pain management module,3 cardiovascular and endocrine modules,4 and a pathophysiology and therapeutics sequence.5 Other colleges and schools of pharmacy have implemented team-based learning as part of their curriculum but have not published their experiences.
A faculty member at Drake University College of Pharmacy and Health Sciences became interested in team-based learning as a way in which students could become better learners and more actively engaged in the classroom. Most educators were taught via the lecture-based method and many had adopted this same approach in their teaching. Although many students at the college were comfortable with this method of learning and paid attention in class and took notes, others were observed sleeping, talking, and reading during lectures. In an effort to get students interested in and excited about course material, active-learning components including cases, games, and documentaries were developed for every lecture. The idea of team-based learning also was raised at this time as this method addressed many professional competencies, including communication, interpersonal skills, teamwork skills, knowledge acquisition, and application of knowledge, and seemed to meet many ACPE Standards.6,7 After much discussion, the faculty approved the transition from lecture-based delivery in pharmacotherapeutics courses to team-based learning in 2008, with formal implementation in January 2009. The objectives of team-based learning were to motivate students to become more engaged in the course and to make them better learners.
DESIGN
Prior to implementation of team-based learning, students in the pharmacotherapeutics course attended 2-hour lectures twice weekly. Students also met in smaller recitation groups once each week for 2 hours. Most students were satisfied with the lecture portion of the course as the faculty member (considered the content expert by his colleagues) told them what they needed to know and they could remain anonymous in a large lecture hall. However, some students were unhappy with the recitation portion of the course, which was led by faculty members who were not always comfortable with the material and could not answer the students’ questions immediately. A 2-3 day delay in responding to the students’ questions sometimes occurred while the recitation leader contacted the lecturer.
Standard team-based learning is comprised of 3 major steps.1 Step one is individual study and preparation that is completed prior to class. Students are assigned readings that contain information on concepts that must be understood in order to complete the next 2 steps.
Step 2 of standard team-based learning is the readiness assurance step in which students come to class and complete an individual (usually multiple-choice) test on the preclass reading.1 After the individual test (IRAT) is complete and students have turned in their answers, the students work with an assigned team to complete a group test (GRAT). The GRAT contains the same questions as the IRAT, but this time the team has to agree on 1 answer for each item. The groups may be able to see whether their answers are correct using immediate feedback assessment technique answer sheets. Following the GRAT, the group can submit a written appeal for one of their answers to a question (if needed) and the instructor will provide clarification on concepts presented in the preclass readings.
Step three of standard team-based learning consists of application exercises. Teams work together to solve problems using information gained through the previous 2 steps.1 An effective team assignment presents students with a significant problem that has one specific answer, presents the same problem to all groups, and requires all groups to report their answer simultaneously.
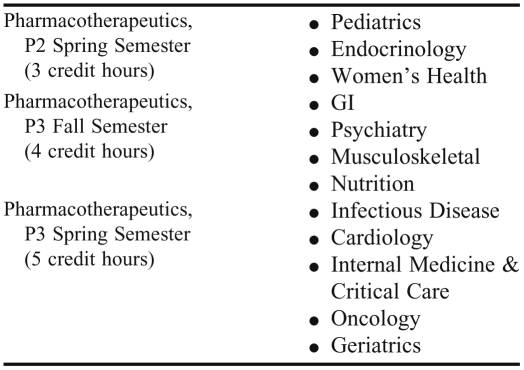
The College of Pharmacy and Health Sciences faculty at Drake University chose to develop a customized team-based learning format. Upon faculty approval to adopt a team-based learning curriculum, the course coordinators of the pharmacotherapeutics sequence decided to eliminate the recitation sections of the pharmacotherapeutics course and to limit the number of faculty members involved in teaching the course. The course was divided into 12 modules worth 12 credits earned over 3 semesters, and 1 instructor taught the entire module (Table 1). The faculty members teaching in the modules were considered the “content experts” in these respective areas. Students completed the pediatrics, endocrinology, and women's health modules during the spring semester of their second (P2) year. The gastrointestinal, psychiatry, musculoskeletal, and nutrition modules were taught in the fall semester of the third (P3) year, followed by the infectious disease, cardiology, critical care, oncology, and geriatrics modules in the spring of the P3 year.
Table 1.
Pharmacotherapeutics Team-based Learning Schedule
All faculty members teaching in the pharmacotherapeutics module wrote objectives for each topic with the idea that students could learn easier concepts by reading and studying on their own and that learning subsequently would be tested by the IRAT and GRAT. The more difficult and complex objectives could be taught via the application exercises completed during class time. Each faculty member distributed the learning objectives, study guide, and reading assignments to students at least 1 week prior to the IRAT/GRAT. The reading assignment consisted of 1 to 3 chapters in the course textbook. Faculty members were encouraged to assign no more than 30 pages of reading per section. Students were expected to come to class prepared to take the IRAT, followed immediately by administration of the GRAT, completion of written appeals (if needed), and clarification from the instructor.
Once the RAT process was completed, the students moved into pre-assigned groups of 5 to 7 students. In order to encourage participation, each student evaluated the other members of the group via a peer evaluation form twice a semester. The peer evaluation accounted for a small percentage of the students’ final grade. Additionally, many faculty members and their P4 advanced pharmacy practice experience (APPE) students continuously walked around the room to provide guidance and encourage student participation in finding the solution for the cases.
After students moved into their respective groups, the application exercises started, with most faculty members presenting a few cases or exercises per topic. Faculty members were encouraged to develop case-based materials with multiple-choice questions and several possible answers to encourage discussion. The case or activity needed to be difficult enough that 1 or 2 students could not answer them on their own. Depending on the topic and case, teams were given approximately 5 minutes to work through the case or activity and come up with an answer to the clinical question posed. After time was up, all groups simultaneously reported their results through the use of laminated cards labeled A through E, corresponding with the 5 possible answers to each question. After the results were reported, 1 or 2 groups were randomly selected to provide their rationale for the answer they selected. The instructor then reviewed the best answer or answers and addressed any additional student concerns.
Once the application exercise was finished, the instructor provided a few summary slides to emphasize the main learning point(s) of the previous application exercise. These slides were used to help students make the connection between what they were learning in class and the take-home message needed to complete the module objectives. Summary slides did not contain the detailed answer to the application exercise. Copies of the summary slides (not the application exercises) were posted on Blackboard after each class session.
At the end of each class period, the faculty member asked the teams to submit “muddiest points.” The faculty member then addressed these points through a forum discussion board in Blackboard, in e-mails to the entire class, or verbally to the class at the next meeting.
The Psychiatry Module
The psychiatry module within the Pharmacotherapeutics course is described here to illustrate the application of the team-based learning format. The psychiatry module is taught to the P3 class around the same time each year, after the students have completed a course on the pharmacology of psychiatric medications. For this module, the RAT and application exercises were divided into 3 respective sections: (1) depression, anxiety, and insomnia; (2) bipolar disorder and schizophrenia; and (3) substance use disorders and epilepsy. For the first section, students read the depression chapter, the anxiety chapter, and the insomnia section of the sleep disorders chapter from the course textbook. For the second section, they read the bipolar and schizophrenia chapters. For the third and final section, students read the substance use disorders and epilepsy chapters. The class met twice weekly for 2 hours, and the whole block was completed in 4 weeks. The students completed an examination on these topics at the end of the module.
In addition to writing the objectives for this section, the instructor created a detailed study guide in which students could fill in the answers to the questions while they were reading the chapters (Appendix 1). The goal was to make the reading a more active process while giving students an idea of which important concepts to draw from the readings. Creating their own study guides aided them in preparing for both the readiness assessment tests and the application exercises.
Once the readiness assessment test was completed, the application exercises started. Although encouraged to develop challenging cases for their module, some faculty members were hesitant to write cases having more than 1 answer as students often want only 1 answer and prefer topics to be “black and white.” However, the psychiatric module instructor felt that cases with more than one possible correct answer were more realistic and better prepared students to deal with the “gray areas” of pharmacy practice. Challenging cases also gave students an opportunity to apply what they had learned in the textbook and kept them more engaged in the class.
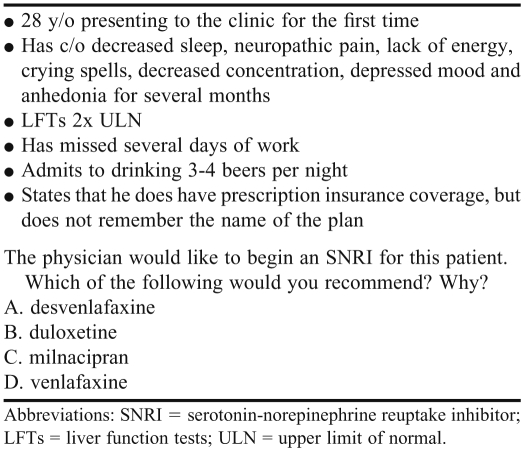
During the application exercises, the instructor and two P4 experiential students walked around the classroom, meeting with each group to listen to their discussion, answer their questions, and provide input when warranted. The psychiatry module contained 7 cases for depression, 5 cases for anxiety, 1 for insomnia, 5 for bipolar, 6 for schizophrenia, 5 for substance use, and 4 for epilepsy (example of question in Table 2).
Table 2.
Example of a Case Question Used in a Psychiatry Module of a Pharmacotherapeutics Course Taught Using Team-based Learning
Because the instructor of the psychiatry module was curious as to how the new teaching method would impact examination scores, examination questions were left similar in difficulty and complexity for the first few years after implementation of team-based learning. Students did not receive their examinations back after they took them and the answers to the questions were not posted anywhere.
EVALUATION AND ASSESSMENT
In the psychiatry module, individual quiz scores for 2010-2011 averaged in the 80%-85% range, while group scores have averaged in the 95-100% range. The class rarely agreed on the same answer for the application exercises. The end of the module examination average was the exact same in fall 2010 as it was in fall 2008 (prior to team-based learning).
Five other instructors teaching in the pharmacotherapeutics sequence also left their examination questions similar in complexity throughout the transition to team-based learning. Three of the 5 instructors reported having similar examination averages before and after implementing team-based learning, 1 reported a slight decrease in scores, and 1 reported a slight increase in scores.
DISCUSSION
The main strengths of team-based learning include that it holds students accountable for their learning, teaches teamwork, and addresses several professional competencies.1 Team-based learning is also suitable for large classes in lecture halls, engages students during class time, and offers students opportunities to develop clinical reasoning skills. Another advantage is that one faculty member, usually the content “expert,” can conduct the entire module. Nevertheless, some students may feel cheated that they are not being “taught,” and some faculty members may resist change.1
The transition to a team-based learning format was difficult at first for both students and faculty members, and still remains challenging. Faculty members teaching in the course meet a few times a year to discuss quality assurance issues and continue to assist one another in the development of clinical cases as well as examination questions. Faculty members also strive to follow the same basic structure and framework of TBL and remain strongly committed to the success of this method in the large classroom setting.
Although nervous and apprehensive about this major change in teaching methods, some individuals teaching this course have come to appreciate it and even enjoy it. Because students have to prepare for class, more active engagement in real-life cases and a higher level of discussion can occur during class time. This method also teaches students life-long learning skills. The lack of one correct answer not only prepares them for APPEs but also clinical practice. Being part of a team teaches them to work effectively with others. For the psychiatry section of the course, student learning, as measured by examination scores, appears to be at around the same level as prior to implementation of team-based learning methods.
The 2 major challenges to team-based learning that some instructors have noticed are students’ frustration with the lack of one correct answer and the difficulty for student groups to stay on topic. Some instructors have attempted to alleviate these challenges by having P4 students assist in facilitating the sessions. The P4 students and the instructor usually discuss the application exercises at length prior to the class session and then attempt to interact with all groups during the application exercises to ensure that questions regarding the application exercise are answered and the P3 students are kept on topic. As stated previously, a random group is selected in the psychiatry module to present their answer and rationale when the class is ready to discuss an application exercise. However, if the instructor and/or the P4 students come across a group that is not discussing the case, this group is typically selected to present their rationale for their answer choice to the class.
Team-based learning is currently used as the main teaching method in Drake's nonprescription medicines class. While other instructors of other courses in the college are intrigued and supportive of the use of team-based learning, there are no plans to use this method as the sole mode of curriculum delivery in any other classes at this time. Some instructors have added a team-based learning component to their classes, such as a preassigned reading followed by a short quiz at the beginning of class. Others have added a complex problem into a lecture and required students to work in teams for a few minutes to come up with an answer. Regardless of the course, faculty members agree that we need to get students more active in the classroom.
SUMMARY
In an attempt to get students more active and more engaged in the classroom, faculty members teaching the Pharmacotherapeutics course at Drake University College of Pharmacy and Health Sciences adopted the team-based learning method in January 2009. Students are now required to come to class having read assigned readings in order to successfully complete independent and group tests. Adequate preparation for the RATs aids students in deciding the best outcomes for the application exercises. These exercises further improve students’ clinical and teamwork skills, and gives them additional opportunities to prepare for the end of the module examination as well as for their pharmacy careers.
Appendix 1. Depression Study Guide
Depression
-
I. Required Reading
Cates M, Boggs AA, Feldman J. Major Depressive Disorder. In: Chisholm-Burns MA, Wells BG, Schwinghammer TL, Malone PM, Kolesar JM, Rotschafer JC, DiPiro JT editors. Pharmacotherapy: principles & practice. New York: McGraw-Hill; 2006:569-583.
-
II. Medications Discussed
Tricyclic antidepressants (TCAs)
Serotonin norepinephrine reuptake inhibitors (SNRIs) - Note: desvenlafaxine & milnacipran will be covered in application exercises; they will NOT be on the RAT since they are not in your text
Selective serotonin reuptake inhibitors (SSRIs)
Trazodone
Bupropion
Mirtazapine
Monoamine oxidase inhibitors (MAO-Is)
-
III. Learning Objectives
Recognize the symptoms of major depressive disorder (MDD). (Study question 6)
Describe the mechanism of action for all antidepressant drug classes. (Pharmacotherapy table on page 3 of this handout)
-
List antidepressants most likely associated with the following:
A. sedation (table on page 3 of this handout)
B. sexual dysfunction (table on page 3 of this handout)
C. weight gain (table on page 3 of this handout)
D. hepatotoxicity (study question 14)
E. increased blood pressure (study question 13)
F. seizures (study question 12)
Discuss time course to therapeutic effect for antidepressants as well as potential duration of therapy. (Study questions 21 & 23)
Recognize maximum doses of tricyclic antidepressants and bupropion. (Study question 19)
Review the symptoms of antidepressant withdrawal. (Study question 23)
-
IV. Study Questions
What is the lifetime prevalence of depression?
Which gender is more likely to develop depression?
What is the average age of onset of depression?
Which psychiatric comorbidities occur most frequently with depression?
What causes depression?
List the diagnostic criteria for depression.
Which medical conditions might cause/contribute/exacerbate depressive symptoms?
Which medications might cause/contribute/exacerbate depressive symptoms?
What are the goals of treatment?
What nonpharmacologic therapies are available for patients?
Which antidepressants produce the least amount of sexual dysfunction?
Which antidepressant is contraindicated in someone having a seizure disorder?
Which antidepressant may increase blood pressure at higher doses?
Which antidepressant should be used with caution in someone having hepatic dysfunction?
Which antidepressant is used primarily as a sleep aid?
Which antidepressant has been associated with priapism?
Which antidepressant has a long half-life?
What are the symptoms of serotonin syndrome?
-
List the maximum doses of the following:
Amitriptyline
Nortriptyline
Imipramine
Desipramine
Bupropion (immediate release)
How do we select an antidepressant?
How long does it take an antidepressant to work?
How is partial response managed?
How long should antidepressants be continued after treating the 1st depressive episode?
What are the symptoms of antidepressant withdrawal?
REFERENCES
- 1.Michealsen LK, Parmalee DX, McMahon LL, Revine RE. Team-Based Learning for Health Professions Education: A Guide to Using Small Groups for Improving Learning. Sterling. VA: Stylus Publishing; 2008. [Google Scholar]
- 2.Marshall LL, Nykamp D. Active-learning assignments to integrate basic science and clinical course material. Am J Pharm Educ. 2010;74(7):Article 119. doi: 10.5688/aj7407119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Conway SE, Johnson JL, Ripley TL. Integration of team-based learning strategies into a cardiovascular module. Am J Pharm Educ. 2010;74(2):Article 35. doi: 10.5688/aj740235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Letassy N, Fugate SE, Medina M, Stroup J, Britton M. Using team-based learning in an endocrine module for pharmacy students across two campuses. Am J Pharm Educ. 2008;72(5):Article 103. doi: 10.5688/aj7205103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beatty SJ, Kelley KA, Metzger AH, Bellebaum KL, McAuley JW. Team-based learning in therapeutics workshop sessions. Am J Pham Educ. 2009;73(6):Article 100. doi: 10.5688/aj7306100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Association of Colleges of Pharmacy. Center for the Advancement of Pharmaceutical Education. http://www.aacp.org/resources/education/Documents/CAPE2004.pdf Accessed July 18, 2011.
- 7.Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. http://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed July 18, 2011.