Abstract
Objective. To describe the development, implementation, and initial outcomes of a pharmaceutical care training-of-trainers course developed to assist Ethiopian pharmacy faculty members and graduate students in the development of curriculum and provision of pharmaceutical care services of relevance to this low-income country.
Design. In this collaboration, US and Ethiopian faculty members worked together in a week-long seminar and in hospital ward rounds to develop and offer a course to facilitate faculty members, curricular, and service development in pharmaceutical care in Ethiopia.
Assessment. Assessments were conducted during the seminar, immediately post-seminar, at 3 months post-seminar, and at 1 year post-seminar. An examination was administered at the conclusion of the course to assess immediate learning outcomes for the graduate students. Post-course assessments of short-term (3-month) and longer-term (12-month) impact were conducted to identify pharmaceutical care services that had been implemented to assess knowledge and skill gained during the seminar. Correspondence between seminar participants and the US faculty members as well as graduate student thesis projects provided further evidence of changes at 3 and 12 months post-course.
Conclusion. Pharmaceutical care training was developed for Ethiopian faculty members through a seminar and hospital ward rounds. Enhancements have been added to curricula for bachelor in pharmacy students and select pharmaceutical care services have been implemented through master's thesis projects.
Keywords: pharmaceutical care, global, collaborative, training, preceptor
INTRODUCTION
Ethiopia is an Eastern African country of approximately 80 million persons with a gross domestic product of US $900 per capita, classifying it as a low-income country.1 Infectious diseases that are highly prevalent in Ethiopia include human immunodeficiency virus (HIV) infection, malaria, tuberculosis, parasitic infestations, acute respiratory infections, and diarrheal disease. Issues related to maternal and newborn health and malnutrition also affect the people of Ethiopia. Additionally, Ethiopia, like many other sub-Saharan African countries, is experiencing an epidemiological transition with hypertension, cardiovascular disease, and diabetes mellitus becoming increasingly prevalent.2
There is a shortage of pharmacists and pharmacy technicians in Ethiopia. In 2007, there were 1,088 licensed pharmacists in Ethiopia, or only 0.14 per 10,000 population. The number of licensed pharmacies in the country in 2007 was 463, consisting of 143 hospital pharmacies and 320 community pharmacies. The effects of these and other challenges on the provision of health care in Ethiopia have been documented by others.3-6 The bachelor of pharmacy is the minimum professional degree required to be licensed as a pharmacist in Ethiopia, followed by a 1-year internship. This academic degree program emphasizes basic sciences and product-oriented training, with minimal integration of pharmacy practice training. The lack of faculty members with clinical pharmacy training is one of the biggest challenges facing the Ethiopian pharmacy degree programs as the profession moves toward the provision of pharmaceutical care services.
The importance of pharmaceutical care services in saving lives and protecting public health is particularly relevant in resource-limited settings with a high prevalence of major medicine-treatable diseases and systems-wide opportunities related to pharmaceutical care. Areas where the pharmaceutical care approach might be applied to sub-Saharan Africa include medicine use evaluation, medication adherence, and pharmacovigilance.7
Low-income countries have insufficient human resources for meeting their pharmaceutical care needs. Task-shifting has been proposed as a strategy to free-up the pharmacy workforce to provide pharmaceutical care services.8 Another possible solution for this problem is the establishment of partnerships between sub-Saharan Africa-based and Western or Northern hemisphere universities. The HIV/AIDS Twinning Center program is a collaboration between Howard University and Addis Ababa University (AAU). Funded by the President's Emergency Plan for AIDS Relief, the goal of this program is to strengthen AAU's capacity to train current and future pharmacists to support HIV-related care and treatment, including the provision of high-quality antiretroviral therapy (ART). Activities have included establishing an accredited continuing education program, provision of train-the-trainer workshops, and introducing a center of excellence for clinical training at Addis Ababa University School of Pharmacy.9
In March 2009, the School of Pharmacy of Jimma University launched the country's first graduate program in clinical pharmacy with an objective of training patient-centered pharmacy practitioners as well as training faculty members for the new undergraduate clinical pharmacy programs. Jimma University took the lead in clinical pharmacy in Ethiopia because of its unique experiential learning practice sites and its community-based approach to learning, which allow students to train in the university's teaching hospital and local training health centers. To launch the new pharmacy program, the school undertook a series of consultations and workshops to map the new curriculum and advocate for clinical pharmacy education with local and national stakeholders. This new graduate program, Masters of Science in Clinical Pharmacy, was developed in collaboration with partners from the Ethiopian Pharmaceutical Association, the Strengthening Pharmaceutical Systems program of Management Sciences for Health, and the University of Washington. Awarded to Management Sciences for Health by the US Agency for International Development, the Strengthening Pharmaceutical Systems program builds institutional and individual capacity in developing countries to effectively and efficiently manage pharmaceutical systems by improving the availability and use of quality-assured medicines. The University of Washington, one of the partners of the Strengthening Pharmaceutical Systems program, provides technical assistance in pharmacovigilance, pharmacoeconomics, drug policy, and pharmaceutical care. In this report, we describe the development, implementation, and initial outcomes of a pharmaceutical care training of trainers course, which was designed to assist with curricular development of pharmaceutical care in Ethiopian pharmacy education.
DESIGN
In November 2009, faculty members from the University of Washington and from Ethiopia conducted a training of trainers course at Jimma University pharmaceutical care for participants from the 4 colleges and schools of pharmacy in Ethiopia located in Addis Ababa, Gondar, Mekele, and Jimma. The primary goal of the course was to help participants build their capacity to teach about and potentially provide pharmaceutical care services that contribute to improved health outcomes. The specific objectives of the course were to provide pharmaceutical care training to faculty members and clinical pharmacy graduate students with particular emphasis on implementation of pharmaceutical care services in resource-constrained settings; and to assist the universities with identifying, prioritizing, and developing ideas for pharmaceutical care services to be initiated by participants in the hospital and community settings. The training of trainers course was designed to teach the skills required for clinical preceptorship at colleges and schools of pharmacy including ward rounds, review of medication charts, therapeutic drug monitoring, and assessment of trainee's performance.
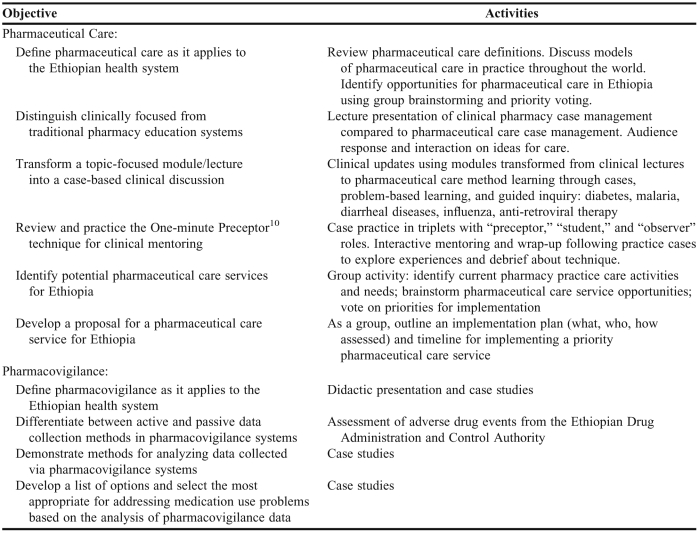
A collaborative and iterative approach was used to ensure that the training of trainers course curriculum was relevant and could be translated directly to meet the pharmacy education needs of the program participants in Ethiopia. The learning objectives (Table 1) and an initial agenda for the training of trainers course were developed by the University of Washington in close collaboration with faculty members from Jimma University, representatives from Management Sciences for Health, and the Ethiopian Pharmacists Association. Although the primary learning goal was knowledge enhancement, comprehension and application also were assessed through group interaction using cases and practice-site visits. A learner-centered approach for teaching was used throughout the program to promote a training of trainers that focused on achieving participant goals for learning. Standard lectures, using a teacher-centered format for instruction, were used to review terms, definitions, and key facts, as well as to demonstrate this instructional technique compared with other learner-centered techniques, such as the One Minute Preceptor.10
Table 1.
Ethiopia Pharmaceutical Care Training of Trainer Learning Objectives
Three strategies were used to ensure that the final training of trainers curriculum best met the learning needs of the local participants. Upon arrival in Ethiopia, the training of trainers agenda (Table 2) and curriculum were adapted based on direct input from the learners during on site tours of pharmacy, hospital, and clinics by University of Washington faculty members. Second, a baseline survey was administered on the first day of the training of trainers course to document selected demographics, participants' experience with and suggestions for pharmaceutical care services, curricular activities, goals for seminar learning, and system needs for improvement. Finally, daily post-workshop learning assessments were used to obtain feedback about and allow for adjustment of the training of trainers course, with curricular modifications occurring each evening. The workshop functioned as a live classroom for practice and experiential learning with each clinical topic presentation using a different educational technique. To promote pharmaceutical care learning and skills development, participants documented perceived advantages and challenges of using the learning techniques as well as which instructional methods they preferred to use in their classrooms following each presentation. Appendix 1 describes a case unit developed for the training of trainers curriculum.
Table 2.
Agenda for Pharmaceutical Care Training of Trainers Program, Jimma University, Ethiopia
The training of trainers course facilitated identification, prioritization, and program development of pharmaceutical care service needs. Participants were asked to identify 2 priority pharmaceutical care activities that they thought would benefit the Ethiopian healthcare system in their region. During a summative session of the workshop, the activities and goals outlined during the individual conference sessions were reviewed to identify and document one specific goal for implementing change and the related action plan for enhancing pharmaceutical care education or services. Participants also were asked to discuss the initial design of 2 new curricular activities that could be implemented to enhance the development of students' education and skills related to pharmaceutical care. The project was reviewed and granted a certificate of exemption by the University of Washington Human Subjects Division.
EVALUATION AND ASSESSMENT
Assessments were conducted during the seminar, immediately following the seminar (post-seminar), at 3 months post-seminar, and at 1 year post-seminar. A posttest examination was administered at the conclusion of the training of trainers course to assess immediate learning outcomes for the graduate students because they would have a lead instructional role in the pharmaceutical care curriculum. Post-seminar assessments of short-term (3-month) and longer-term (12-month) impact consisted of an e-mailed request for information from the SPS program's Ethiopia office on activities related to pharmaceutical care that might be attributable to knowledge or skill gained during the seminar. E-mail and Facebook correspondence between seminar participants and University of Washington faculty members, as well as graduate student thesis projects to implement pharmaceutical care services provided evidence of changes and pharmaceutical care-related activities at 3 and 12 months post-seminar.
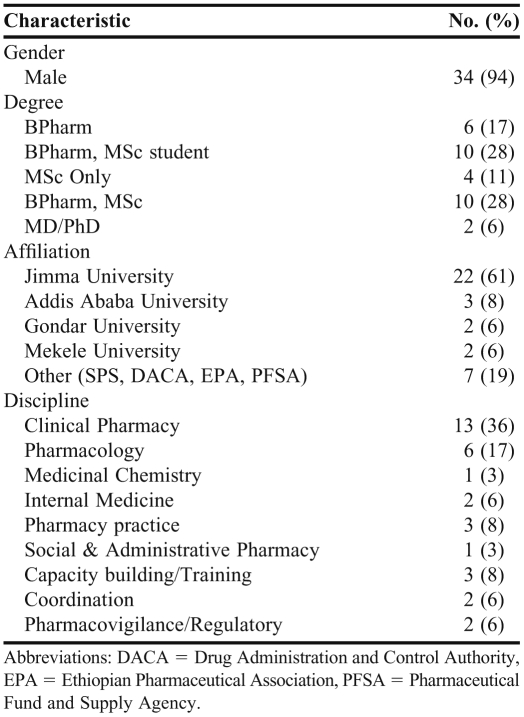
Training of trainers program participants provided baseline information about their demographics training, worksite, impressions about pharmaceutical care, and goals for the workshop (Table 3). Thirty-six faculty members and graduate students, representing 7 institutions across Ethiopia, completed the survey instruments, representing a 100% response rate. Participants' training ranged from a bachelor of science (BS) in pharmacy degrees to doctor of philosophy (PhD) degrees. The majority of participants (N = 18) were students enrolled in the new graduate clinical pharmacy program at Jimma University. These students reported that their goals for the training of trainers course were to develop pharmaceutical care knowledge and skills for use in the new curriculum. Ninety-three percent of respondents (N = 33) believed that pharmacists and pharmacy assistants or technicians have primary responsibility for dispensing medications to patients in Ethiopia. However, only 41% of participants believed that pharmacists should have primary responsibility for providing medication information to patients, followed by pharmacy assistants (23%), physicians (22%), nurses (12%), and drug sellers (2%). The most common work sites for pharmacists in Ethiopia ranked on a 4-point scale from 1 (most common) to 4 (least common) were hospital pharmacy (rank 1.6), community pharmacy (1.8), antiretroviral therapy (ART) dispensary (2.7), and rural health center (3.6).
Table 3.
Workshop Participant Characteristics (N = 36)
We assessed participants' written feedback regarding the agenda for the week, the need for additional information, and the learning competencies achieved at the end of the first full day of the training of trainers course to identify gaps in understanding or areas of the agenda and curriculum that need to be refined. Participants reported that the agenda outline matched their desired learning objectives, and after the second day of the training of trainers seminar, self-assessments indicated that participants were achieving daily seminar learning objectives. Therefore, only minor modifications to accommodate additional gaps in topic coverage or learning were subsequently made to the curriculum. These modifications included adding a section on implementation strategies consisting of action plan development and a prioritized list of actions needed to assist participants in implementing what they had learned in the pharmaceutical care seminar at their universities or practice sites.
The advantages and challenges of using various instructional methods (ie, lecture, lecture with cases, problem-based cases, guided cases, and precepting) were discussed throughout the seminar. Participants reported that using cases in the pharmaceutical care learning process encouraged questions and facilitated their ability to apply the material to an immediate situation; thus, it was deemed essential to learning and applying the material. The use of guided case inquiry was preferred as a method of directing learning. Problem-based learning was seen as advantageous when more time for inquiry was available; however, participants viewed this method as too challenging for rapid advancement toward a learning goal. The use of cases to start and summarize the learning in a lecture format was deemed a helpful method for increasing interest in lecture material, demonstrating relevance of the material (eg, potentially a strategy to be used by more basic science courses to generate interest and relevance to pharmacy practice) and for teaching large groups of learners.
At baseline, participants reported poor confidence in their ability to precept students. Trainees indicated that the One-Minute Preceptor training10 increased their level of comfort in being a clinical mentor to students, and they demonstrated improved skill during the pharmaceutical care workshop case practices. However, they indicated that they might benefit from continued access to consultation with an experienced preceptor to obtain feedback and advice on student training techniques.
Training of trainers course participants who were graduate students in the clinical pharmacy master's program completed the training of trainers knowledge posttest (Appendix 2) to assess readiness for pharmaceutical care teaching and practice. Participant performance on the examination was excellent, with scores ranging from 46 to 50 points out of a total possible score of 50 points, demonstrating that participants had adequate knowledge of pharmaceutical care definitions and interpretation of its components, such as drug-related problems. Comprehension and application were assessed throughout the training of trainers by means of interactive case discussions and question-and-answer sessions.
The training of trainers course participants identified 4 pharmaceutical care service priorities for implementation: (1) drug information services, (2) screening and reporting of drug interactions and adverse drug reactions in the inpatient setting, (3) public health and illness prevention education, and (4) screening, primary care services, and referral to care in the community setting.
By the 3-month post-training assessment in March 2010 there was evidence of progress toward the goals set by the training of trainers course attendees. These goals included meeting with hospital officials to discuss involvement of pharmacists on certain wards at least for part of a shift or for patient care rounds, and outlining specific drug information services to be offered by pharmacists. At 1 year post-training, clinical pharmacy graduate students who participated in the training of trainers course were developing and implementing their master's degree projects in relevant areas to facilitate pharmaceutical care service implementation and evaluation. These specific projects were in diabetes care, medication error prevention and surveillance, drug information, and medication adherence. Other training of trainers course participants had begun roles in clinical patient care rounds on the general wards and intensive care unit and were exploring additional ways to integrate pharmaceutical care services into their practices. To support these efforts, US-based training of trainers faculty members worked in an advisory capacity with local Ethiopian faculty advisors on the master's thesis projects.
DISCUSSION
Educational collaboration is a key step in introducing and improving pharmaceutical care throughout the world. The opportunity for US-based pharmacy faculty members to work together with pharmacy faculty members, graduate students, and health officials in Ethiopia to assist with building capacity and providing technical assistance to colleges and schools of pharmacy in Ethiopia was invaluable. During the training of trainers course, enthusiastic learners were highly interested in strengthening their pharmaceutical care knowledge and skills with added key learning centering in the area of capacity building and program implementation strategies. Training of trainers faculty members from the United States also gained invaluable insight into promoting, implementing, and providing pharmaceutical care in low-income settings and were inspired by the creativity in program ideas in this environment. Enhancing the pharmaceutical care skills and training capacity of Ethiopia's pharmacy faculty members and students has the potential to improve the delivery of health care. Systems strengthening and training of new healthcare workers to meet the pressing challenges associated with delivering care to persons with HIV/AIDS and other conditions is a priority for both the US President's Emergency Plan for AIDS Relief and the Global Health Initiative.11 The importance of pharmaceutical services in saving lives and protecting public health is particularly relevant in resource-limited settings, where there is a high prevalence of major medicine-treatable diseases and systems-wide pharmaceutical care opportunities.6
There are numerous challenges to providing training of trainers through collaborative arrangements such as the one described here. One challenge was developing the training curriculum and agenda without prior knowledge about and experience dealing with the needs and realities of pharmacists in Ethiopia. Because pharmaceutical care is a broad topic that could span an extensive period of study, determining which aspects to address in a week-long training was also a challenge.
After arriving in Ethiopia and meeting their counterparts in person, the training team was better able to identify specifically what the training program should address as a result of touring health facilities, having discussions with pharmacists, and conducting a baseline needs assessment. The faculty members' flexibility in adapting and augmenting the agenda quickly was integral to the success of the training of trainers. Comments from the debriefing sessions at the end of each day helped the faculty members refine the curriculum for the next day in order to make it as relevant and applicable as possible. As pharmaceutical care is an attitude, feeling, and skill rather than didactic presentation or a one-time training, this training of trainers course was only a first step toward helping pharmacy faculty members understand how to better cultivate these skills in their students. This short intervention demonstrated a highly effective and economical method of transferring pharmaceutical care knowledge and skill. Subsequent steps could include clinical research projects, service implementation, and additional assessments of the need and impact on pharmaceutical care delivery in Ethiopia
SUMMARY
We describe the development, implementation, and initial outcomes of a pharmaceutical care training-of-trainers course offered in November 2009 to assist Ethiopian pharmacy faculty members and graduate students in the development of curriculum and provision of pharmaceutical care services of relevance to this low-income country and to facilitate faculty, curricular, and service development in pharmaceutical care. Assessments were conducted during the seminar, immediately following the seminar, at 3 months post-seminar, and at 1 year post-seminar. Pharmaceutical care training of Ethiopian faculty members was implemented successfully through master's thesis projects, with integration of related pharmaceutical care learning into curricula of the pharmacy training programs.
Acknowledgements
We acknowledge the support and assistance of Gabriel Daniel, MS, Jude Nwokike, MS, and Tina Brock, EdD, of Management Sciences for Health-Strengthening Pharmaceutical Systems and Dr. Hamza Addus, Training Director, I-TECH Ethiopia. We acknowledge the leadership of the other schools of pharmacy represented at the workshop: Woldeselassie Mequanent of Gondar University, Mussi Gezu of Mekele University, and Michael Awoke of Addis Ababa University and Sultan Suleman of Jimma University. We further acknowledge the assistance of Catherine Corbell, PhD, in preparing for the training of trainers, and we are grateful to all of the faculty members and students who participated in the training.
This project and report were supported by the Strengthening Pharmaceutical Systems Program, which receives funding from the US Agency for International Development.
Appendix 1. One-Minute Preceptor Unit Description10
Module Objective: Development of Advanced Pharmacy Practice Experience Precepting Skill
Methods: Didactic, active learning, debrief, and skill modeling.
Didactic: 30-minute didactic presentation which reviewed the andragogical basis for experiential learning and the key “microkills” of the One-Minute Preceptor model
Active Learning: Role play using clinical cases, defined roles, and participant pairings. Roles were distributed allowing participants 5-10 minutes to review their role and clarify questions with the session instructors. Participant pairs took turns playing the role of preceptor and student (15 minutes per role play) using two different clinical case scenarios.
Debrief: The role plays were immediately followed by a debrief which included listing the strengths and limitations of this technique, discussion of personal experience with precepting or the role plays, and identification of strategies for addressing perceived limitations of this instructional method.
Skill Modeling and Coaching: UW faculty members provided coaching and modeling of the One-Minute Preceptor technique during visits to health facility wards and health centers as part of the tours.
Sample Tools:
Role Play: Pharmacy Student Role
You were asked today to review the medication history and suggest treatment for Mrs. Jones, a 36 year old woman, seen in the health clinic this morning. Mrs. Jones has had a recent onset of urinary incontinence, frequency, urgency, and pain, and was diagnosed today with a urinary tract infection. She has not had UTIs previously and has no anatomical abnormalities that would increase her risk. She has also experienced anorexia, weight loss of 5 pounds, and insomnia over the past 3 months, although this has not been evaluated. Her medical history is significant for malnutrition and malaria (treated 10 years ago). You are meeting with your preceptor right now to discuss the patient. Your research has concluded that acceptable therapies include cotrimoxazole DS twice daily and ciprofloxacin 250 mg twice daily but you are uncertain about the duration of therapy. You do not understand how to determine if the patient's UTI is “complicated” or “uncomplicated” and this determination influences duration of therapy. You admit to your preceptor that you feel overwhelmed by all the case details and are not sure how to proceed with regard to identifying the patient's primary pharmaceutical care needs. She is still in clinic and you are to meet with her prior to her leaving to provide instruction on the use of her medications.
Role Play: Preceptor Role
You are precepting in the health clinic this morning. One of your pharmacy students is having difficulty with assessment of a patient's urinary tract infection and would like your input on the case.
Preceptor Background Case Content Resource
Mrs. Jones is a 36 year-old woman who presents to the clinic with complaints of urinary incontinence, painful urination (dysuria), frequent urination, and urgency to urinate. No back pains or fever complaints. No vaginal discharge.
Previous medical history: No previous diagnosis of UTI in last 8 months. Malaria treated 10 years ago. Not sure whether allergic to sulfa.
Social history: Married 23 years, non-smoker, does not drink alcohol
Laboratory profile: None
Meds: Long-acting insulin
Diagnosis: Uncomplicated urinary tract infection
Questions to consider for preceptor-student discussion:
What are the signs and symptoms that indicate the presence of a UTI?
➢ painful urination (dysuria), frequent urination and urgency to urinate.
What are the risk factors for UTI present in this patient?
➢ Female gender, unprotected sex
How would you verify whether or not Mrs. Jones is allergic to sulfa?
➢ Describe symptoms of Stevens-Johnson syndrome.
➢ Ask whether she has used and subsequently suffered any reactions to the antimalarial, sulphadoxine-pyrimethamine (“Fansidar™”)
What are the possible alternatives if Mrs. Jones is indeed allergic to sulfa?
➢ Nitrofurantoin, broad spectrum antibiotics
What information should be disseminated to Mrs. Jones to enhance treatment effectiveness?
➢ Must complete dose of cotrimoxazole
➢ Drink plenty of water.
➢ Avoid herbal medicines
➢ Report immediately to doctor if infection recurs.
Five Micro Skills: Preceptor Resource10
Ask for a commitment: “What do you think is going on?”
Probe for evidence: “What brought you to that conclusion?”
Teach general rules: “Typically, in a case like this…”
Provide positive feedback: “You did xyz really well…”
Correct mistakes: “Next time, you'll want to…”
Appendix 2. Training of Trainers Pharmaceutical Care Seminars Examination
In your own words, how does Pharmaceutical Care differ from traditional pharmacy practice?
-
Please complete a PC plan for the following case:
Jutta is a 24-year-old female admitted to the hospital with acute asthma. Aminophylline is initiated at 6 mg/kg and an infusion of 0.6 mg/kg is maintained. Her therapeutic drug monitoring level reported to the pharmacy PC service is 10 mcg/ml (desired range 5-15 mcg/ml). You are working the shift and asked to advise with regard to the continued aminophylline dose and other asthma PC needs. She is also taking erythromycin for bronchitis/pneumonia, salbutamol, and prednisione (1 mg/kg). You are concerned about the potential drug interactions (erythromycin and aminophylline), education on use of salbutamol, and needs for dose adjustment of her aminophylline. Please complete the PC plan attached to this examination.
List 4 drug-related problems and provide an example of each problem
List 3 symptoms of hyperglycemia
List 3 symptoms of hypoglycemia
-
Please match the appropriate advantage to the case-based educational technique below:
Technique Advantage-
a. lecture case _________
-
b. problem based learning case _________
-
c. guided case inquiry _________
Advantages-
a. students work independently to develop critical thinking
-
b. can provide to a large audience
-
c. reduces time students spend working on unrelated ideas
-
a.
- Schools of pharmacy in Ethiopia are significantly behind the rest of the world in developing PC services (circle the correct answer)
-
a. True
-
b.False
-
a.
- Refusal to provide a legal but controversial prescription would not be considered pharmaceutical care because (circle the correct answer)
-
a. The pharmacist in placing their concerns above the patient's needs
-
b. The denial of care may lead to patient harm
-
c. PC is defined, in part, as taking personal responsibility for beneficial patient outcomes
-
d. All of the above are correct
-
e. None of the above is correct
-
a.
- It is possible for someone to be coinfected with p.vivax and p.falciparum in Ethiopia (circle the correct answer)
-
a. True
-
b. False
-
a.
- Worldwide malaria is responsible for over 1 million deaths annually, especially among children in sub-Sarahan Africa (circle the correct answer)
-
a. True
-
b. False
-
a.
- Artemether-lumefantrine is commonly used for malaria case-management in Ethiopia. (circle the correct answer)
-
a. True
-
b. False
-
a.
- List two signs that diarrhea is due to bacterial infection.
-
a.
-
b.
-
a.
REFERENCES
- 1.Ethiopia. The World Fact Book. Central Intelligence Agency: USA. https://www.cia.gov/library/publications/the-world-factbook/geos/et.html Accessed June 13, 2011.
- 2.World Health Organization. WHO Country cooperation strategy: Ethiopia. http://www.who.int/countries/eth/eth/en/. Accessed June 13, 2011.
- 3.Karunamoorthi K, Rajalakshmi M, Babu SM, et al. HIV/AIDS patient's satisfactory and their expectations with pharmacy service at specialist antiretroviral therapy (ART) units. Eur Rev Med Pharmacol Sci. 2009;13(5):331–339. [PubMed] [Google Scholar]
- 4.Suleman S, Ketsela A, Mekonnen Z. Assessment of self-medication practices in Assendabo town, Jimma zone, southwestern Ethiopia. Res Social Adm Pharm. 2009;5(1):76–81. doi: 10.1016/j.sapharm.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 5.Abula T, Worku A, Thomas K. Assessment of the dispensing practices of drug retail outlets in selected towns, north west Ethiopia. Ethiop Med J. 2006;44(2):145–150. [PubMed] [Google Scholar]
- 6.Makonnen E, Yoseph M, Berhane Y. Quality of prescription at a tertiary care pharmacy in Addis Ababa. Ethiop Med J. 2002;40(3):233–239. [PubMed] [Google Scholar]
- 7.King RC, Fomundam HN. Remodeling PC in Sub-Saharan Africa (SSA) amidst human resources challenges and the HIV/AIDS pandemic. Int J Health Plann Manage. May 2009 doi: 10.1002/hpm.982. [DOI] [PubMed] [Google Scholar]
- 8.Babigumira J, Castelnuovo B, Lamorde M, et al. Economic Evaluation of Task Shifting in Follow-up of Patients on Antiretroviral Therapy in a Resource-Limited Setting. BMC Health Services Research. 2009;9:192. doi: 10.1186/1472-6963-9-192. doi:10.1186/1472-6963-9-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Addis Ababa University School of Pharmacy / Howard University Pharmacist and Continuing Education Center's HIV/AIDS Twinning Center website. Available at: http://www.twinningagainstaids.org/HIVAIDSTwinningCenter-EthiopiaAAUHoward.html. Accessed June 13, 2011.
- 10.Neher JO, Gordon KA, Meyer B, et al. A five-step “microskills” model of clinical teaching. J Am Board Fam Pract. 1992;5(4):419–424. [PubMed] [Google Scholar]
- 11.Global Health Initiative. http://www.pepfar.gov/ghi. Accessed June 13, 2011.