Abstract
Many studies have proven that the polymethylmethacrylate (PMMA) augmentation of the pedicle screw can significantly increase stiffness and strength of spinal fixation. Some major complications have also been reported. However, there are no reports discussing cement distribution and its morphology in the osteoporotic vertebral body, which is critical in the analysis of the biomechanical strength of the pedicle screw and the risk of cement leakage after pedicle screw augmentation. In this study, we used computed tomography (CT) to evaluate the cement distribution in the osteoporotic vertebral body after PMMA augmentation of a pedicle screw and to analyze the factors leading to cement leakage. Two groups of patients were studied. Group A consisted 25 osteoporotic patients (mean age of 73 years) with spinal instrumentation who had a total of 145 pedicle screws and cement augmentation with biopsy needles. Group B consisted of 23 osteoporotic patients (mean age of 74.6 years) with spinal instrumentation who had a total of 125 cannulated pedicle screws with cement augmentation. All patients had CT evaluation of the cement distribution in the vertebral body after the surgery. The cement distribution in the vertebrae was divided into four zones in the axial CT view: anterior one-third, middle third, and posterior third of vertebral body, and the pedicle. The morphology of the cement distribution around the pedicle screw was defined as scattered type or concentrate type. The leakage pattern was divided to anterior–lateral, posterior–lateral, and canal leakage. The correlations among bone mineral density (BMD), the cement leakage rate, and cement distribution morphology were also analyzed. The results showed that most augmented pedicle screws had cement extension into three of the four zones of the vertebral body (66.3%), followed by two zones (20%), all four zones (11.5%), and only one zone (2.2%). Overall, 123 screws (84.8%) in Group A and 108 screws (86.4%) in Group B had cement concentrate type distribution. The cement leakage rate in Group A is 18.3% and 13.6% in Group B. Patients with a BMD <0.6 g/cm2 had significantly higher rates of cement leakage and tended toward a scattered cement distribution. There was only one patient who had a symptomatic leakage (sciatica) in Group B. We concluded that the cement distribution after pedicle screw augmentation with biopsy needle or cannulated screw technique was mostly localized in three zones of the vertebral body, and patients with lower BMD had a higher risk of cement leakage and scattered cement distribution.
Keywords: Cannulated pedicle screw, Cement augmentation, Osteoporosis, Polymethylmethacrylate
Introduction
Osteoporosis has become a growing concern in the aged population. Many of these individuals experience spinal complications from osteoporosis, including vertebral fracture, deformity, and/or neural element compression. In some patients, surgical treatment is unavoidable. An osteoporotic spine presents a significant challenge for a spinal surgeon to manage [7, 14].
Pedicle screws can provide three-column fixation and are the most common implant used in spinal surgery. However, fixation failures have frequently been reported [10, 12]. Many studies have demonstrated a correlation between bone mineral density (BMD) and the strength of pedicle screw fixation [5, 7–9, 11, 17, 20, 22]. Furthermore, various techniques have been developed to increase the fixation strength in the osteoporotic spine, such as the use of supplemental laminar hooks, fixation with bi-cortical screws, improved screw geometry, and the augmentation of screw fixation with bone cement [1–3, 7, 13, 15, 16, 19, 20, 23–25]. Polymethylmethacrylate (PMMA) is most commonly utilized to strengthen the pedicle screws, and the results have proven to be quite effective in both in vitro and clinical reports [6, 18, 20–22, 26]. Risks involved in the use of PMMA for pedicle screw augmentation include nerve injury and vascular damage caused by cement leakage [25]. However, there are no studies describing the cement distribution within the vertebral body, the definitive cement leakage rates after pedicle screw augmentation, and the correlation between cement leakage and the technique utilized for cement injection. This study uses computed tomography (CT) in the evaluation of the morphology of cement distribution within the vertebral body, the pattern of cement leakage after PMMA augmentation of pedicle screws in the osteoporotic spine, and the analysis of factors leading to cement leakage.
Materials and methods
Study patients
Two groups of patients were studied. Group A contained 25 osteoporotic patients who underwent spinal instrumentation between March 2004 and January 2007 with PMMA augmented pedicle screws using a biopsy needle for cement injection. Information about twelve of these patients has been reported in a previous study [3]. Group B included 23 osteoporotic patients who underwent spinal instrumentation between January 2007 and June 2009 with PMMA augmented cannulated pedicle screws. The diagnoses and basic data of the patients are summarized in Table 1.
Table 1.
Basic data of patients
| Group A (25 cases) | Group B (23 cases) | |
|---|---|---|
| Female/male | 17/8 | 18/5 |
| Age (years) | 73 (57–85) | 74.6 (57–95) |
| BMD (g/cm2) | 0.579 (0.48–0.753) | 0.583 (0.435–0.798) |
| T-score | −2.8 (−1.8 to −4.3) | −2.7 (−1.5 to −3.6) |
| Diagnosis | ||
| Compression fracture/burst fracture | 17/25 (68%) | 14/23 (61%) |
| Spondylolisthesis with stenosis | 3/25 (12%) | 8/23 (35%) |
| Pathological fracture (metastasis) | 5/25 (20%) | 1/23 (4%) |
| Lesion level | ||
| T-spine | 2 | 1 |
| T–L junction | 8 | 6 |
| L-spine | 15 | 16 |
BMD bone mineral density
The indications for the insertion of pedicle screw with cement augmentation in these two groups were: first, spinal stabilization was necessary due to instability caused by degenerated listhesis, infection, tumor metastasis, and osteoporotic vertebral fracture; second, osteopenia or osteoporosis was found in pre-operative spinal plain X-ray; third, pre-operative DEXA also showed osteopenia or osteoporosis; mean T score: −2.8 (from −1.8 to −4.3) in group A and −2.7 (from −1.5 to −3.6) in group B. All patients, except those with tumor metastases, underwent posterior or posterior–lateral fusion. Data included the pre- and postoperative visual analog scale (VAS), Oswestry disability index (ODI), and complications such as extravasation of cement, nerve injury, and infection were recorded. For the evaluation of PMMA cement distribution in the vertebral body and cement leakage pattern, CT was performed on all of the patients.
Surgical technique
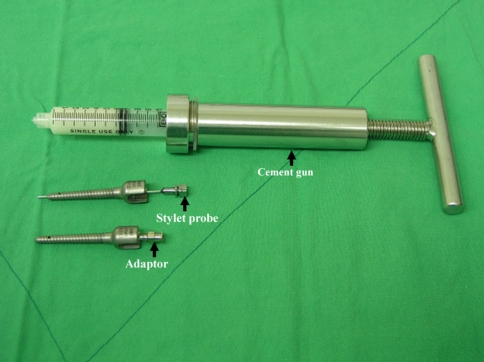
The surgical technique has been described in a previous study [3]. Group A underwent direct cement injection through a biopsy needle, followed by the removal of the biopsy needle and then insertion of pedicle screw. The PMMA (Surgical Simplex P, Stryker Corporation) was used in Group A. In Group B, bone cement was injected directly via a cannulated pedicle screw and its cement injection system (Wellong BMI Medical, Taiwan). The cannulated screw is a mono-axial top loading screw with a side hole at the distal third of the screw thread, and specifically designed for cement augmentation (Fig. 1). In patients with tumor metastasis or osteoporotic vertebral fracture, the augmented pedicle screws were applied on the non-lesion intact vertebral bodies. The commonly used screw diameter was 6.2–6.5 mm, and the length of the screw was 40–50 mm. The cement used in Group B (VERTEBROPLASTICTM, DePuy AcroMed, England) is designed specifically for vertebroplasty. The amounts of cement injected in each pedicle screw were 2 mL (T-spine) and 3 mL (L-spine). Cement was injected from the caudal screws to the cranial screws in Group B, and the sequence was recorded during each operation. The cement injection procedures in both groups were performed under the guidance of uniplane fluoroscopy.
Fig. 1.
The cannulated screw and cement injection set
Postoperative CT evaluation
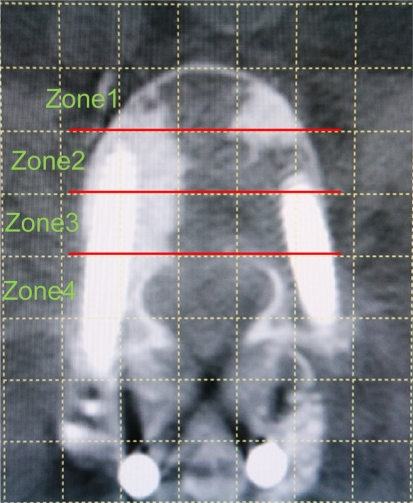
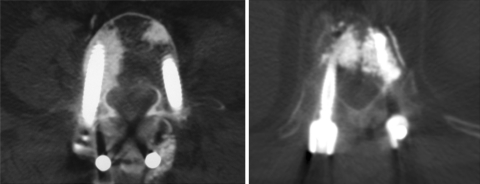
CT scan (Siemens SOMATOM PLUS 4, Germany) with 240 mA tube current, 120 KVP and Pitch 1 was used to evaluate the distribution of the cement within the spine. The image was cut every 3 mm, and the location and leakage direction of the cement, as well as the morphology of the leaked cement, were recorded. Using the computer software (Smart Iris, Medincom Cooperation, Taiwan), the axial view of the vertebral body which cut through the largest part of pedicle screws was latticed and evenly divided into three zones (Fig. 2). The extension of cement within the vertebral body was then categorized into four zones: zone 1 anterior third of the vertebral body; zone 2 middle third of the vertebral body; zone 3 posterior third of the vertebral body; and zone 4 pedicle area. Cement leakage was also divided into areas: anterior–lateral leak involved the anterior and/or anterior–lateral to anterior half of the vertebral body; posterior–lateral leak involved the posterior–lateral to posterior half of the vertebral body; and canal leak involved the spinal canal. The thickness of the canal leakage was measured and divided into <2, 2–4 and >4 mm. Furthermore, two types of cement morphology were identified: concentrated type had most of the injected cement concentrated around the pedicle screw without obvious radiolucent space between the cement; scattered type had most of the injected cement randomly scattered, spotted, or linearly distributed around the pedicle screw with obvious radiolucent space between the cement (Fig. 3).
Fig. 2.
CT axial view of cement distribution zones: zone 1 anterior third of the vertebral body; zone 2 middle third of the vertebral body; zone 3 posterior third of the vertebral body; and zone 4 pedicle area
Fig. 3.
The cement morphology in the vertebral body with axial view on CT scan. a concentrated type with 2 zone distribution (both screws). b scattered type with 2 zone distribution and anterior–lateral leak
Statistical analysis
The STATA software package (Texas, USA) was used for statistical analysis. Fisher’s exact test was applied for categorical variables, and the Mann–Whitney U test was used for continuous variables. The association between the cement injection sequence and the leakage rate was analyzed through simple linear regression. Statistical significance was assumed with p < 0.05.
Results
In Group A, a total of 155 pedicle screws were inserted, and 145 (93.5%) screws were augmented with PMMA cement (Table 2), the 10 screws were not augmented due to applying the screw on the vertebral body that had previous vertebroplasty (5 screws) and violation of the pedicle wall or anterior cortex of vertebral body during the preparation of the pedicle tract (5 screws). The mean amount of injected cement was 1.79 mL (1.3–2 mL) in the T-spine and 2.35 mL (1.5–3 mL) in the L-spine. In Group B, there were 140 cannulated pedicle screws inserted, and 125 (89.3%) were augmented with PMMA cement, the remaining 15 screws were not augmented due to the use of the bicortical purchase technique without cement augmentation for S1 lesions (8 screws), violation of the pedicle wall or anterior cortex of vertebral body during the preparation of the pedicle tract (3 screws), and application of the screw on vertebral body of an old compression fracture with solid union (4 screws). The mean amount of injected cement was 1.83 mL (1.5–2 mL) in the T-spine and 2.48 mL (1.8–3 mL) in the L-spine. The ODI and VAS pain score improved in both groups at final follow-up. The mean follow-up period was 16.5 months (from 6 to 26 months) in group A and 15.9 months (from 8 to 20 months) in Group B. The ODI score of Group A dropped from 76.5% before surgery to 40.2% after surgery, and the Group B score dropped from 71 to 28%. The VAS improved from 9.2 to 2.8 in Group A and 9.5 to 3.0 in Group B.
Table 2.
The level and number of augmented pedicle screws
| Level | Group A | Group B | ||||
|---|---|---|---|---|---|---|
| Total screw number | Cemented screw number | Cement leak number | Total screw number | Cemented screw number | Cement leak number | |
| T8 | 2 | 0 | 0 | 2 | 2 | 0 |
| T9 | 5 | 5 | 0 | 2 | 2 | 0 |
| T10 | 10 | 10 | 0 | 10 | 9 | 0 |
| T11 | 18 | 18 | 2 | 12 | 12 | 2 |
| T12 | 20 | 20 | 1 | 8 | 8 | 0 |
| L1 | 22 | 19 | 5 | 20 | 16 | 6 |
| L2 | 28 | 28 | 11 | 20 | 19 | 4 |
| L3 | 24 | 22 | 6 | 18 | 18 | 2 |
| L4 | 18 | 18 | 1 | 24 | 23 | 2 |
| L5 | 6 | 5 | 0 | 16 | 16 | 1 |
| S1 | 2 | 0 | 0 | 8 | 0 | 0 |
| Total | 155 | 145 | 26 | 140 | 125 | 17 |
CT evaluation of cement distribution
All patients in this study underwent post-operative CT scan evaluation. In Group A, there were 4 pedicle screws (2.7%) with cement located only in zone 1; 20 screws (13.8%) with cement located in zones 1 and 2; 11 screws (7.6%) with cement in zones 2 and 3; 91 screws (62.8%) in zones 1, 2, and 3; 5 screws (3.4%) in zones 2, 3, and 4; and 14 screws (9.7%) located in all 4 zones. In Group B, there were 2 pedicle screws with cement located only in zone 1 (1.6%); 19 screws (15.2%) in zones 1 and 2; 4 screws (3.2%) in zones 2 and 3; 80 screws (64%) in zones 1,2, and 3; 3 screws (2.4%) in zones 2, 3, and 4; and 17 screws (13.6%) in all 4 zones. Overall, the cement distribution in the vertebral body mostly involved three of the four zones (zones 1, 2, and 3; and zones 2, 3, and 4), which occurred in 66.2% of Group A and 66.4% of Group B (Table 3).
Table 3.
The extent of cement distribution within the vertebral body
| 1 zone | 2 zones | 3 zones | 4 zones | |
|---|---|---|---|---|
| Group A n = 145a | 4 (2.7%) | 31 (21.4%) | 96 (66.2%) | 14 (9.7%) |
| Group B n = 125a | 2 (1.6%) | 23 (18.4%) | 83 (66.4%) | 17 (13.6%) |
| Total n = 270a | 6 (2.2%) | 54 (20%) | 179 (66.3%) | 31 (11.5%) |
aData were presented as PMMA cement augmented screw numbers
Cement leakage occurred in 26 of 145 screws (17.9%) in Group A and 17 of 125 screws (13.6%) in Group B. Anterior–lateral cement leakage was evident in 11.7% (17 screws) in Group A and 8.8% (11 screws) in Group B. Posterior–lateral leakage occurred in 7.8% (11 screws) in Group A and 4% (5 screws) in Group B. Leakage into the spinal canal was observed in 11.7% (17 screws) in Group A and 8% (10 screws) in Group B (Table 4). No cement leakage into the vertebral disc was observed in both groups. Among these 17 screws with a spinal canal leak (involving 7 patients) in Group A, 13 (76%) were found to have leakage of <2 mm on CT axial view; 4 screws (24%) had a leakage between 2 and 4 mm. However, none of these seven patients had neurological symptoms. Among the 10 screws with a spinal canal leak (involving four patients) in Group B, 7 (70%) were found to have cement leakage <2 mm; 3 screws (30%) had leakage between 2 and 4 mm. Only one of these four patients with both spinal canal leakage and posterior–lateral leak experienced had mild post-operative sciatica.
Table 4.
Types of cement leak
| Leakage type | Group A (n = 145) | Group B (n = 125) | |
|---|---|---|---|
| Canal leak | 17 (11.7%)a | 10 (8%) | p = 0.21 |
| <2 mm | 13 | 7 | |
| 2–4 mm | 4 | 3 | |
| >4 mm | 0 | 0 | |
| Anterior–lateral leak | 17 (11.7%)b | 11 (8.8%)c | p = 0.28 |
| Posterior–lateral leak | 11 (7.6%)d | 5 (4%)e | p = 0.16 |
| Total screw leak no. | 26 (17.9%) | 17 (13.6%) | p = 0.21 |
aData were presented as screw no. and leakage rate (leakage screw no./total cemented screw no.)
bThere were 12 screws combined with canal leak, 5 screws combined with posterior–lateral leak
cThere were six screws combined with canal leak, one screw combined with posterior–lateral leak, one screw with 3-direction leak
dThere were two screws combined with canal leak, five screws combined with anterior–lateral leak
eThere was one screw combined with anterior–lateral leak, one screw combined with foramen leak
The BMD and cement leakage in each group was compared, and a significant difference was identified (p < 0.05) (Tables 5, 6). Patients with BMD <0.6 g/cm2 had a higher cement leakage rate (45% in Group A, 40% in Group B) compared to patients with BMD >0.6 g/cm2 (0% in both Group A and Group B).
Table 5.
Correlation between BMD and cement leak
| Group A | Group B | |||
|---|---|---|---|---|
| Patient no. | BMD (Mean ± SD) | Patient no. | BMD (Mean ± SD) | |
| Cement leak (−) | 16 | 0.61 ± 0.10 | 17 | 0.61 ± 0.06 |
| Cement leak (+) | 9 | 0.52 ± 0.05 | 6 | 0.51 ± 0.05 |
| p value | 0.015 | 0.006 | ||
Table 6.
Correlation between BMD and cement distribution
| Group A | Group B | |||
|---|---|---|---|---|
| Patient no. | BMD (Mean ± SD) | Patient no. | BMD (Mean ± SD) | |
| Concentrated type | 12 | 0.62 ± 0.12 | 18 | 0.60 ± 0.08 |
| Scattered type | 13 | 0.54 ± 0.05 | 5 | 0.54 ± 0.04 |
| p value | 0.045 | 0.048 | ||
The morphology of the cement distribution was categorized as concentrated type or scattered type. In Group A, 123 screws (84.8%) had the concentrated type cement, while 108 screws (86.4%) in Group B had the concentrated type cement distribution. The relationship between BMD and the cement distribution pattern in these two groups was compared, and a significant difference was identified (p < 0.05) (Table 5).
A correlation between the spinal canal leak and the zone of the cement distribution was also identified. Pedicle screws with the cement involving zone 4 had higher canal leakage rates. In Group A, 19 screws involved cement extension into zone 4 (zone 2, 3, and 4; and zones 1, 2, 3, and 4), and 15 screws involved cement extension into the spinal canal (15/19, 80%). In Group B, 20 screws involved cement extension into zone 4, and 8 screws involved cement extension into the spinal canal (8/20, 40%). The leakage rate was higher when cement extended into zone 4.
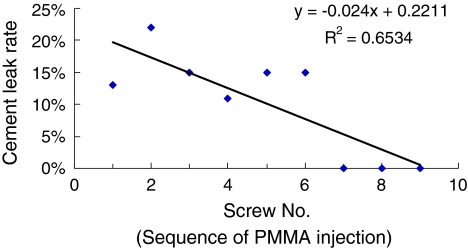
Every screw in Group B was numbered to identify the sequence of cement injection. Bone cement was injected from the L-spine to the T-spine (caudal to cranial). Seventeen screws developed cement leakage. The relationship between the cement sequence and the leakage rate was calculated by linear regression (Fig. 4).
Fig. 4.
Correlation between the sequence of cement injection and cement leak rate
Discussion
Most of the injected cement in the vertebral body after augmentation of pedicle screws with biopsy needle or cannulated screw was localized to a 3-zone distribution (66.3%), followed by a 2-zone (20%), 4-zone (11.5%), and 1-zone distribution (2.2%). There are several explanations for the different distributions. The injection of different cement volumes causes various cement distribution patterns. In this study, 2 mL of cement was injected for each T-spine screw, and 3 mL of cement was injected for each L-spine screw. However, the injection procedure was stopped when cement extended to the posterior vertebral line or extravasate to anterior lateral aspect of the vertebral body. Therefore, variations in cement volume occurred from screw to screw and patient to patient. Additionally, the cement viscosity may be responsible for the different cement distributions. When the viscosity was low, the cement distribution in the first two screws tended to be the scattered type. In contrast, when the viscosity was higher, the cement distribution for the last several screws tended to be the concentrated type. The distance between the screw tip and the anterior edge of the vertebral body may also effect the distribution of the cement. The morphology of the vertebral body varies in different levels of the spine, which affects the selection of screw size and length. When the screw tip approached the anterior edge of the vertebral body, the cement tended to distribute toward the anterior part (zones 1 and 2) of the vertebral body. On the other hand, when the screw tip was located in the middle of the vertebral body, the cement distributed to the middle and/or posterior part (zones 2 and 3) of the vertebral body.
According to the previous studies, the injection of PMMA along the entire length of the screw results in the highest pullout strength [14]. The pedicle area provides approximately 60% of the pullout strength [6], which means the more zones (especially the pedicle area) that involve PMMA, the stronger the pull-out strength of the pedicle screw. Thus, the ideal distribution of the cement involves all four zones of the vertebrae. However, the spinal canal leakage rate with cement extension to the pedicle zone (zone 4) in each group was up to 79% (15 screws with canal leak out of 19 screws which has cement extension to zone 4) in Group A and 40% in Group B (8/20), which is significantly higher than the screws without cement extension to the pedicle area: 3.2% in Group A (4 screws with canal leak out of 126 screws which has no cement extension to zone 4) and 2% in Group B (2/105), p < 0.05). The ideal cement distribution may be the screw with the anterior 3 zones (zone 1, 2, and 3) distribution, which may represent the perfect balance point between optimal biomechanical strength and risk of spinal canal leakage. We suggest that the tip of injection needle or the cannulated pedicle screw should be placed in zone 2 (mid-point of vertebral body.) in lateral view during cement injection, and the cement flow should be carefully monitored with fluoroscope not beyond the posterior vertebral body line (zone 3).
This study revealed that there were 26 screws (17.9%) in Group A with a cement leak, and 17 (11.7%) of those involved a spinal canal leak. In Group B, 17 screws (13.6%) had a cement leak, and 10 screws (8%) involved a spinal canal leak. One patient in Group B experienced a neurological complication. A posterior–lateral and foraminal leak in one of the screws (L1 vertebral body) caused sciatica of the left leg. Only conservative treatment was necessary. In present study, no screw with cement leakage into intervertebral disc was observed. This result is different from that of vertebroplasty treating osteoporotic compression fracture, in which fracture of endplate is common and cement leakage into the intervertebral disc through the broken endplate can occur. In contrast, the augmentation of pedicle screw is commonly performed on an intact vertebral body which has intact endplate, and cement leakage into the intervertebral disc is rare.
The cannulated screw used in this study is a mono-axial top loading screw with a side hole at the distal third of the screw thread. One study showed that a screw with multiple side holes from the proximal to the distal third of the screw thread had higher pullout strength than that of screw without or with only one side hole on the distal third [4]. However, the study also demonstrated that most injected cement tended to exude from the most proximal side hole of the screw. Therefore, a screw with a side hole or multiple side holes near the proximal third of screw thread may have a higher risk of cement leakage into the spinal canal or intervertebral foramen than that with only a distal side hole.
CT scan analysis demonstrated most cement leakage has a thin, linear and/or small spotted pattern. Most of those leakages were minor, occurring via the perispinal vessel network, and thus rarely cause nerve compression. There was no significant difference in the rates of cement leakage between Groups A and B; however, but the overall leakage rate was higher in Group A. There are two possible explanations for this difference. First of all, regular cement (Surgical Simplex P, Stryker Corporation) was used for pedicle screw augmentation in Group A. The cement, although clearly observed in CT scan, was hard to monitor under fluoroscopy, which may increase the risk of cement leakage. The second possibility involves the method of cement injection. In Group A, the cement was injected through a biopsy needle and the pedicle screw was inserted after the removal of the needle. The cement may extend or redistribute during pedicle screw insertion causing cement leakage. On the other hand, the technique of direct injection of PMMA cement through cannulated pedicle screws is easier and simpler than the biopsy needle cement injection technique. PMMA augmentation using cannulated pedicle screws has the advantage of simplicity with similar clinical outcome.
BMD may also play an important role in cement leakage. The cement leakage rate was higher in osteoporotic patients with lower BMD (p < 0.05). The overall leakage rate for patients with BMD <0.6 g/cm2 in each group was 45 and 40%, respectively, while patients in both groups with BMD >0.6 g/cm2 experienced a leakage rate of 0%. Patients with lower BMD have thinner trabeculae inside the vertebral body [6], which may have more inter-trabeculae space through which mobile cement can pass. This difference may create wide and unpredictable cement spread. The cement may extend more easily to vessels and spread via the vessel network. Care must be taken during cement injection in patients with BMD <0.6 g/cm2. The timing of PMMA cement injection was also very important because low viscosity cement carries a higher risk of extravasation. Therefore, in patients with severe osteoporosis extra caution should be taken during cement injection for augmentation of pedicle screws.
The relationship between BMD and bone cement distribution pattern in the vertebral body revealed a significant difference (p < 0.05). Patients with a lower BMD had a higher chance of experiencing scattered cement distribution. We think that the cement distribution morphology may affect the bone-cement-implant interface, which closely correlated with the stiffness of instrumentation. However, the ideal cement distribution morphology is unknown. Further investigation of cement pattern and biomechanical strength of the pedicle screw is needed.
Our study demonstrates that the timing of cement injection correlates with the risk of cement leakage. The pedicle screws with earlier cement injection tended to have a higher risk of cement leak, and screws with later injection have the opposite outcome. A possible explanation is that the viscosity of PMMA cement increased gradually with time which may have reduced the cement leak. The cement used in Group B is VERTEBROPLASTICTM, and its setting time under room temperature is approximately 15 to 20 min. Cement injection should not begin until the working phase starts. The duration of cement injection is less than 10 min. Furthermore, two or three fluoroscopy images were obtained for each screw augmentation, which increases further as the number of screws increases. According to our experience, a case with up to eight screws frequently experiences harder cement when inserting the last one or two cannulated pedicle screws. Two packs of cement may provide sufficient time for injection.
In conclusion, the PMMA distribution and morphology in the vertebral body after pedicle screw augmentation can be various due to many factors such bone mineral density, the sequence of injection etc. This phenomenon should be noticed during biomechanics test for analyzing the screw fixation strength after cement augmentation. Both the injection methods, biopsy needle or cannulated screw technique, had most cement localized in the vertebral body, and patients with lower BMD had higher risk of cement leakage and tended to have scattered cement distribution in morphology. It should be noted that the distribution of cement is least predictable and most likely to have canal penetration in those most likely to need the augmentation technique.
Conflict of interest
None.
Footnotes
The device/drug is FDA-approved or approved by corresponding national agency for this indication.
References
- 1.Becker S, Chavanne A, Spitaler R, et al. Assessment of different screw augmentation techniques and screw designs in osteoporotic spines. Eur Spine J. 2008;17:1462–1469. doi: 10.1007/s00586-008-0769-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Burval DJ, McLain RF, Milks R, et al. Primary pedicle screw augmentation in osteoporotic lumbar vertebrae: biomechanical analysis of pedicle fixation strength. Spine. 2007;32:1077–1083. doi: 10.1097/01.brs.0000261566.38422.40. [DOI] [PubMed] [Google Scholar]
- 3.Chang MC, Liu CL, Chen TH, et al. Polymethylmethacrylate augmentation of pedicle screw for osteoporotic spinal surgery: a novel technique. Spine. 2008;33:E317–E324. doi: 10.1097/BRS.0b013e31816f6c73. [DOI] [PubMed] [Google Scholar]
- 4.Chen LH, Tai CL, Lai PL, et al. Pullout strength for cannulated pedicle screws with bone cement augmentation in severely osteoporotic bone: influences of radial hole and pilot hole tapping. Clin Biomech (Bristol, Avon) 2009;24:613–618. doi: 10.1016/j.clinbiomech.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 5.Coe JD, Warden KE, Engr M, et al. Influence of bone mineral density on the fixation of thoracolumbar implants: a comparative study of transpedicular screws, laminar hooks, and spinous process wires. Spine. 1990;15:902–907. doi: 10.1097/00007632-199009000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Cook SD, Salkeld SL, Stanley T, et al. Biomechanical study of pedicle screw fixation in severely osteoporotic bone. Spine. 2004;4:402–408. doi: 10.1016/j.spinee.2003.11.010. [DOI] [PubMed] [Google Scholar]
- 7.Halvorson TL, Kelly LA, Thomas KA, et al. Effects of bone mineral density on pedicle screw fixation. Spine. 1994;19:2415–2420. doi: 10.1097/00007632-199411000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Hirano T, Hasegawa K, Takahashi HE, et al. Structural characteristics of the pedicle and its role in screw stability. Spine. 1997;22:2504–2509. doi: 10.1097/00007632-199711010-00007. [DOI] [PubMed] [Google Scholar]
- 9.Inceoglu S, Burghardt A, Akbay A, et al. Trabecular architecture of lumbar vertebral pedicle. Spine. 2005;30:1485–1490. doi: 10.1097/01.brs.0000168373.24644.9f. [DOI] [PubMed] [Google Scholar]
- 10.Kim YJ, Bridwell KH, Lenke LG, et al. Pseudarthrosis in long adult spinal deformity instrumentation and fusion to the sacrum: prevalence and risk factor analysis of 144 cases. Spine. 2006;31:2329–2336. doi: 10.1097/01.brs.0000238968.82799.d9. [DOI] [PubMed] [Google Scholar]
- 11.Kumano K, Hirabayashi S, Ogawa Y, et al. Pedicle screws and bone mineral density. Spine. 1994;19:1157–1161. doi: 10.1097/00007632-199405001-00012. [DOI] [PubMed] [Google Scholar]
- 12.Lebwohl NH, Cunningham BW, Dmitriev A, et al. Biomechanical comparison of lumbosacral fixation techniques in a calf spine model. Spine. 2002;27:2312–2320. doi: 10.1097/00007632-200211010-00003. [DOI] [PubMed] [Google Scholar]
- 13.Lotz JC, Hu SS, Chieu DF, et al. Carbonated apatite cement augmentation of pedicle screw fixation in the lumbar spine. Spine. 1997;22:2716–2723. doi: 10.1097/00007632-199712010-00003. [DOI] [PubMed] [Google Scholar]
- 14.McLain RF, McKinley TO, Yerby SA, et al. The effect of bone quality on pedicle screw loading in axial instability: a synthetic model. Spine. 1997;22:1454–1460. doi: 10.1097/00007632-199707010-00006. [DOI] [PubMed] [Google Scholar]
- 15.Moon BJ, Cho BY, Choi EY, et al. Polymethylmethacrylate-augmented screw fixation for stabilization of the osteoporotic spine: a three-year follow-up of 37 patients. J Korean Neurosurg Soc. 2009;46:305–311. doi: 10.3340/jkns.2009.46.4.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moore DC, Maitra RS, Farjo LA, et al. Restoration of pedicle screw fixation with an in situ setting calcium phosphate cement. Spine. 1997;22:1696–1705. doi: 10.1097/00007632-199708010-00003. [DOI] [PubMed] [Google Scholar]
- 17.Okuyama K, Sato K, Abe E, et al. Stability of transpedicle screwing for the osteoporotic spine: an in vitro study of mechanical stability. Spine. 1993;18:2240–2245. doi: 10.1097/00007632-199311000-00016. [DOI] [PubMed] [Google Scholar]
- 18.Pfeifer BA, Krag MH, Johnson C. Repair of failed transpedicle screw fixation: a biomechanical study comparing polymethylmethacrylate, milled bone, and matchstick bone reconstruction. Spine. 1994;19:350–353. doi: 10.1097/00007632-199402000-00017. [DOI] [PubMed] [Google Scholar]
- 19.Renner SM, Lim TH, Kim WJ, et al. Augmentation of pedicle screw fixation strength using an injectable calcium phosphate cement as a function of injection timing and method. Spine. 2004;29:E212–E216. doi: 10.1097/00007632-200406010-00020. [DOI] [PubMed] [Google Scholar]
- 20.Soshi S, Shiba R, Kondo H, et al. An experimental study on transpedicular screw fixation in relation to osteoporosis of the lumbar spine. Spine. 1991;16:1335–1341. doi: 10.1097/00007632-199111000-00015. [DOI] [PubMed] [Google Scholar]
- 21.Waits C, Burton D, McIff T. Cement augmentation of pedicle screw fixation using novel cannulated cement insertion device. Spine. 2009;34:E478–E483. doi: 10.1097/BRS.0b013e3181a8f663. [DOI] [PubMed] [Google Scholar]
- 22.Wittenberg RH, Shea M, Swartz DE, et al. Importance of bone mineral density in instrumented spine fusion. Spine. 1991;16:647–652. doi: 10.1097/00007632-199106000-00009. [DOI] [PubMed] [Google Scholar]
- 23.Yamagata M, Kitahara H, Minami S, et al. Mechanical stability of the pedicle screw fixation systems for the lumbar spine. Spine. 1992;17(suppl 3):S51–S54. doi: 10.1097/00007632-199203001-00011. [DOI] [PubMed] [Google Scholar]
- 24.Yerby SA, Toh E, McLain RF. Revision of failed pedicle screws using hydroxyapatite cement: a biomechanical analysis. Spine. 1998;23:1657–1661. doi: 10.1097/00007632-199808010-00008. [DOI] [PubMed] [Google Scholar]
- 25.Zhuang XM, Yu BS, Zheng ZM, et al (2010) Effect of the degree of osteoporosis on the biomechanical anchoring strength of the sacral pedicle screws: an in vitro comparison between unaugmented bicortical screws and polymethylmethacrylate augmented unicortical screws. Spine [Epub ahead of print] [DOI] [PubMed]
- 26.Zindrick MR, Wiltse LL, Widell EH, et al. A biomechanical study of intrapeduncular screw fixation in the lumbosacral spine. Clin Orthop Relat Res. 1986;203:99–112. [PubMed] [Google Scholar]