Abstract
Vertebral compression fractures represent a frequent pathology among elderly population, with potentially devastating consequences. More than 20 years have passed since percutaneous vertebroplasty was initially used in the treatment of angiomas, representing nowadays a widely used treatment for osteoporotic vertebral fractures. The authors present a retrospective review of 59 consecutive patients (in total 94 fractured levels) that underwent polymethylmethacrylate percutaneous vertebroplasty for vertebral compression fractures due to senile or secondary osteoporosis. All fractures were free from neurologic involvement and were classified as A1 type according to Magerl classification. All of patients were initially treated conservatively, by application of orthosis that allows immediate deambulation. At control, patients who complained of pain and limitation of daily activities underwent MRI. If presence of marrow signal changes, especially hypertense signal in T2-weighted images was confirmed, percutaneous vertebroplasty procedure was performed (we could call it “sub-acute” procedure). A limited group of patients that did not tolerate brace and had an insufficient pain control underwent vertebroplasty “in acute”, few days after fracture. Immediate post-operative pain reduction and follow-up clinical outcome (estimating quality of life and residual back pain) were evaluated by means of Visual Analogue Scale, SF-36 and Oswestry Disability Index. In the immediate post-operative course a significant pain relief was found in 39 patients (66.1%), moderate pain relief in 17 (28.8%), while 3 (5.1%) did not achieve relevant pain improvement. Pain intensity and life quality was maintained within satisfactory limits after a mean follow-up of 16 months. In conclusion, percutaneous vertebroplasty is an effective and safe procedure for treating vertebral compression fractures in the elderly. It provides immediate pain relief and allows early mobilization, thus avoiding potentially severe complications related to persistent back pain and prolonged bed rest. When performed by experienced surgeon complication rate is low, representing a safe procedure, able to provide a satisfactory outcome.
Keywords: Percutaneous vertebroplasty, Vertebral compression fractures, Osteoporosis, Pain, Quality of life
Introduction
Vertebral fractures are the most common complication of osteopenia [1, 2]. Almost 1 million vertebral fractures in the elderly occur each year in Europe, with health costs that amount at 337 million euro [3]. In the US, the annual incidence of osteoporotic fractures is estimated at 1.5 million: 700,000 of them are vertebral fractures, causing nearly 115,000 hospitalizations per year [4]. One-third of all over 65 year-old women experience at least one vertebral compression fracture (VCF), representing the most common fracture type in this population, outnumbering femoral neck and distal radius fractures [5]. Vertebral compression fractures occur in 20% of people over the age of 70 years, while 90% of over 75-year-old individuals are exposed to single or multi-level vertebral body compression, representing a potentially devastating pathological entity for the elderly population, that is destined to increase in the following years as population’s mean age and life expectation keeps increasing [6].
These fractures represent an important cause of disability and morbidity in elderly [7], and they have a negative effect on life quality, physical function, mental health and survival [8].
Vertebral fractures in osteoporotic patients may be of minimal degree and therefore go unnoticed, or they can cause acute and intense lumbar back pain, compromising quality of life [1]. In most cases, conservative treatment based on bed rest, bracing, physical therapy and pharmacological treatment may reduce pain intensity within a few weeks. Generally, this treatment allows a gradual recovery process within 2 or 3 months [9].
Although conservative treatment offers satisfactory clinical results in most of the cases, it is not riskless, especially in elderly people. A considerable number of patients do not respond successfully to conservative treatment and chronic pain may result from: (a) incomplete vertebral healing due to further bone collapse, (b) altered vertebral column kinematics subsequent to spinal deformity, (c) pseudoarthrosis of the fractured vertebral body [7]. Elderly patients frequently experience protraction of intense low back pain which leads to functional limitation, prolonged immobilization and life quality worsening. Thereby, bedsores may appear (often associated to infections), deep venous thrombosis, decrease of bone mineral density and muscle hypotonia. Other severe effects are mood impairment, depressive syndrome and, finally, higher mortality rate, as demonstrated by various studies [10–13]. Patients undergoing conservative treatment may also suffer serious consequences related to bracing incontinence [7, 14], represented by progressive kyphosis as a result of multiple vertebral collapses, that can potentially lead to thoracic and abdominal visceral compression with severe systemic pathological manifestations.
Percutaneous vertebroplasty (PVP) provides the possibility to stabilize vertebral fractures by injecting a small quantity of bone cement into the collapsed vertebral body. With the patient in prone position and under local or general anesthesia, the vertebral body is accessed through unilateral or bilateral transpedicular or parapedicular approach under imaging control, reaching the anterior aspect of the vertebral body, in order to guarantee a symmetrical filling. The quantity of polymethylmethacrylate (PMMA) that should be used for vertebral filling is established during the operating procedure and should be stopped, or even promptly converted in open surgery, if complications occur.
The aim of our study was to evaluate the immediate post-operative pain relief and the mid-long term (16 months) outcome in terms of pain, function and life quality.
Materials and methods
Fifty-nine consecutive patients underwent vertebroplasty procedure between January 2004 and December 2007.
Forty-seven (79.7%) females and 12 (20.3%) males had a total of 94 vertebral compression fractures caused by age-related or secondary osteoporosis (vertebral levels involved are resumed in Table 1).
Table 1.
Fractured vertebral levels
| T 7 | 2 |
| T 8 | 3 |
| T 9 | 2 |
| T 10 | 2 |
| T 11 | 5 |
| T 12 | 23 |
| L 1 | 20 |
| L 2 | 16 |
| L 3 | 11 |
| L 4 | 8 |
| L 5 | 2 |
| Total | 94 |
Densitometry exam showed low bone mineral density, the T-Score for BMD was less than −2.5 SD in all patients, confirming the diagnosis of osteoporosis. The age range of the study population was 53–90 years, with a mean age of 73 years.
Our protocol for treatment of vertebral compression fractures was aimed at early mobilization of patients, by means of bracing and pharmacological treatment to achieve a good pain control. Therefore, all the patients were initially treated conservatively by application of orthosis that allows immediate ambulation.
We examined all cases within 7 days after the fresh fracture. A group of patients that did not tolerate brace and had an insufficient pain control underwent PVP “in acute”, few days after fracture. On the contrary, if they can ambulate without pain, using occasional analgesic drugs and a brace we saw them again at 45 days, time that we consider enough to obtain an initial healing of the bone.
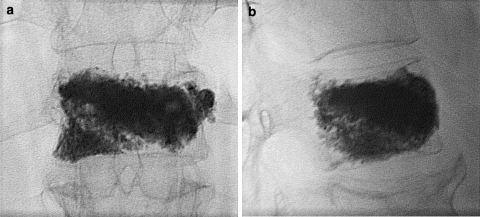
At 45 days consultation, if patients were pain free we eliminate the brace and sent them to medical practitioners. Whereas, if they complained of pain, intake of related analgesic drugs more than 2 times every day, limitation of daily activities and rest in bed many hours a day, we perform an MRI to evaluate the presence of the vertebral body edema (Fig. 1a, b).
Fig. 1.
G.S., 86 years. Osteoporotic fracture of T12: a T1-weighted images, b T2-weighted images
The correlation of local pain and the marrow signal changes in the vertebral body, especially hypertense signal in T2-weighted images, is the indication for PVP (“sub-acute” procedure). Exclusion criteria for PVP are resumed in Table 2.
Table 2.
Exclusion criteria
| Uncorrectable bleeding disorders |
| Infection of vertebral column |
| VCF due to causes other than osteoporosis |
| Compression of the spinal cord or stenosis of the vertebral canal by >30% of the local diameter |
| Neurological deficits |
Twenty-four patients (40.7%) received PVP immediately after acute trauma, while the remaining 35 patients (59.3%) underwent percutaneous procedure only after failure of conservative treatment.
Before the procedure all patients were studied by means of standard radiograms and MRI.
All cases were stable fractures without neurologic involvement, classified as A1 in all cases according to the Magerl classification [15]. Over 94 A1 fractures: 59 were A1.3, 21 A1.2, and 14 A1.1.
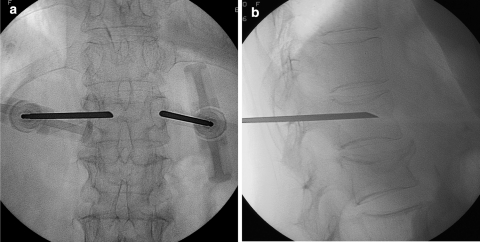
Single-level PVP (Fig. 2a, b) was performed in 29 patients (49.1%), two levels in 25 (42.4%) and three levels in five patients (8.5%). The approach was unipedicular in 67 vertebras (71.2%) and bipedicular (Fig. 3a, b) in 27 (28.7%). Confidence® cement (DePuy Spine) was used in all cases.
Fig. 2.
G.S., 86 years. Single-level PVP intraoperative view: a antero-posterior, b lateral
Fig. 3.
G.S., 86 years. Bipedicular PVP approach, intraoperative view: a antero-posterior, b lateral
All the patients were assessed before discharge with Tc scan (Fig. 4a, b) and at follow-ups (1, 3, 6, 12 months, and then yearly) by standing spinal radiographs in the two standard views.
Fig. 4.
G.S., 86 years. Tc scan performed before hospital discharge: a axial view, b sagittal view
In order to evaluate immediate post-operative pain improvement and long-term clinical outcome, for each patient pre and post-operative characteristics were obtained before the procedure, at the discharge from the hospital and at minimum follow-up of 6 months, including the Visual Analogue Scale (VAS) for pain evaluation, SF-36 health survey (SF36) and Oswestry Disability Index (ODI).
Results
All PVP procedures were performed in a fully equipped surgical environment, 44 patients (74.6%) under local anesthesia while the remaining fifteen (25.4%) underwent general anesthesia. Mean length of surgery was 30 min for single-level treatment, 45 min for two levels and 60 min for three-level procedure. Mean PMMA quantity introduced in each vertebral body was 4.4 cc (1–6).
A cement leakage outside the vertebral body through upper and lower endplates occurred in seven fractures (7.4%) before ideal vertebral filling was achieved. In 4 (4.3%) of these cases there was, moreover, cement flow inside the venous plexuses, yet no cement protrusion into the spinal canal or nerve root compression was found. In one case the procedure was interrupted because of needle breaking.
All patients were able to sustain rapid mobilization and discharge from hospital within 12–24 h after procedure, as mean hospitalization length after surgery was 1.2 days (range 1–3).
In the immediate post-operative course a significant pain relief was found in 39 patients (66.1%), moderate pain relief in 17 (28.8%), while 3 (5.1%) did not achieve relevant pain improvement. The mean pre and post-operative VAS score was 7.6 and 2.3, respectively (p < 0.001).
New non-traumatic vertebral fractures in adjacent levels occurred in eight patients (13.5%) and three of them had a double adjacent vertebral collapse; in five cases new adjacent vertebral fractures occurred within 45 days of treatment.
Mean follow-up was 16 months (3–34).
Just few of these old patients came to the clinical control after 1 year from the treatment, especially if they had remission of symptoms. Only one patient came back at 34 months.
At last follow-up the mean VAS score was 3.1 (0–8.6). Follow-up results of VAS score, SF-36 and ODI are summarized in Table 3.
Table 3.
Questionnaire results
| Pre-op | Follow-up | |
|---|---|---|
| SF-36 | ||
| Physical functioning | 19.6 | 51.2 (p = 0.001) |
| Role-physical | 45 | 47 |
| Bodily pain | 22.3 | 57.7 (p = 0.0008) |
| General health | 49 | 58 |
| Vitality | 45 | 60 |
| Social functioning | 49 | 60 |
| Role-emotional | 36 | 45 |
| Mental health | 46 | 55 |
| ODI | 61% | 25% |
| VAS | 7.6 | 3.1 |
Summarizing, there was a slight improvement of pain from the immediate post-operative to the last follow-up (2.3 vs. 3.31).
The comparison of clinical results (VAS, SF-36, ODI) between the early-treated (acute procedure) and the late-treated (sub-acute procedure) group of patients did not show any statistical difference, even if there was a trend toward a better outcome in the early-treated group.
Discussion and conclusions
Percutaneous vertebroplasty was introduced more than 20 years ago by Galibert et al. [16] to treat patients with painful vertebral hemangiomas. Since then, indications were extended to spinal column metastatic lesions, myelomas and acute vertebral fractures. During the past decades there has been adequate evidence in support of its safety, immediate pain reduction effectiveness exceeds 90% of cases and biomechanical stability [17–21]. Anyway, patient selection criteria and precise indications about timing of treatment for osteoporotic vertebral fractures have not been established yet.
The aim of our study was first to evaluate the mid-long term clinical outcome in patients that underwent PVP treatment, second we also seek to understand the relevance of immediate pain reduction in elderly people.
In our series, 35 patients underwent PVP secondary to conservative treatment failure, while 24 were treated within 2 weeks after acute fracture.
In this second group of patients early PVP was performed either because pain intensity was poorly controlled by pharmacological therapy, or because patient’s general health condition was such that a prolonged bed rest regimen would lead towards a worsening of concomitant pre-existing pathologies and/or the risk of onset of severe secondary pathological manifestations.
Our results showed that there was a significant decrease of VAS score after PVP so that all patients were able to sustain rapid mobilization and discharging.
We believe that prompt and significant decrease of back pain, as well as the effective stabilization of the fractured levels is essential in elderly patients: it provides faster return to daily-life activities and prevents the consequences of bed rest immobilization. Moreover, the low invasiveness of percutaneous treatment guarantees a rapid discharge from the hospital and therefore respects the necessities related to economical costs in modern healthcare.
Follow-up data revealed that pain intensity and life quality was maintained within satisfactory limits after a mean follow-up of 16 months. Different studies [21–23] have showed that patients who undergo PVP benefit from mid-term and long-term pain relief and good life quality. In our series we observed that pain and life quality indexes improve in patients that did not experience new vertebral compressions and in those who suffered from a minor number of pre-existing pathologies.
Cement leakage through upper and lower endplates, or throughout the posterior wall and towards the neural elements, as well as venous migration of solid fragments resulting in pulmonary cement embolism, represent possible complications of PVP but their rate is very low if performed by practiced surgeons. Nevertheless, PVP should always be undertaken in a fully equipped surgical environment that could promptly respond to the need of converting the percutaneous procedure into open surgery. In our series, we found only seven minor complications (7.4%) due to cement leakage outside the vertebral cortex without vascular or neurologic symptomatic consequences.
New non-traumatic vertebral fractures in adjacent levels occurred in eight patients (13.5%). It has been demonstrated that PMMA injection into the osteoporotic vertebral body increases its strength and stiffness [24, 25]. A study led by Alvarez et al. [1] found an increase in incidence of new fractures in the PVP group comparing with the conservative group, even if most of them were not adjacent to augmented vertebra, suggesting that it may represent the natural history of osteoporosis. Although new vertebral fractures subsequent to augmentation procedure has been described in different studies, it is still debated in literature if, and how much, PVP treatment increases the risk of adjacent vertebral fracture. In our opinion bone quality, number of treated levels, PMMA quality and quantity, spinal column and intervertebral discs biological and biomechanical features represent the main factors that establish the relationship between augmented and adjacent vertebras. Further studies should be carried out in order to assess the role that each of these factors play in determining the biomechanical outcome of PVP.
Recently two randomized, double-blind, placebo-controlled trials [26, 27] reported no significant difference between vertebroplasy for osteoporotic spinal fracture and a control group that underwent a “sham” procedure.
These results suggest that factors aside from the instillation of PMMA may have accounted for the clinical improvement after vertebroplasty including the effect of local anesthesia, as well as nonspecific effects, such as expectations of pain relief (the so-called placebo effect), the natural history of the fracture, and regression toward the mean [27].
The data of both trials were in contrast to our results and previous studies that compared series of patients treated using vertebroplasty with medical management (e.g., bed rest, bracing, and pain medications), concluded that vertebroplasty could provide good outcome regarding the pain and the functional restoration. In a recent literature review, meaningful unblended randomized controlled trials [28–30], have been showed that vertebroplasty and kyphoplasty achieved better results compared to conservative osteoporotic fractures treatment.
Commenting on the two studies [26, 27], James N. Weinstein remarked that these results could change vertebroplasty from a procedure that is mostly considered to be successful to one that is considered no better than a placebo.
Weinstein then criticizes some points of these two studies: there was a higher crossover rate in the control group than in the vertebroplasty group (43 vs. 12%) that probably underestimated the true treatment effect; moreover, placebo procedure was actually an active treatment, since it involved injection of a short-acting analgesic into the bony periosteum containing nociceptive fibers.
In summary, Weinstein argued that when faced with several treatment options for which the evidence is less than clear, rather than abandoning the procedure, informed patient choice is essential. Active involvement of informed patient in decision-making process leads to treatment that reflect the patients’ values, consistent with the best evidence. Therefore, he concludes that vertebroplasty should not be left, but cautiously used, informing patients about potential risks and benefits.
In conclusion, we believe that PVP is a safe and effective procedure for treatment of vertebral osteoporotic fractures; it can provide a significant decrease of pain intensity within a few hours after surgery and can guarantee a good quality of life. When executed by practiced surgeons it gives satisfactory results with a very low complication rate. PVP should be always considered in elderly patients with vertebral fractures that could risk severe secondary complications or worsening of pre-existing pathologies because of bed rest immobilization.
Conflict of interest
None declared.
References
- 1.Alvarez L, Alcaraz M, Perez-Higueras A, Granizo JJ, Miguel I, Rossi RE, Quinones D. Percutaneous vertebroplasty. Functional improvement in patients with osteoporotic compression fractures. Spine. 2006;31(10):1113–1118. doi: 10.1097/01.brs.0000216487.97965.38. [DOI] [PubMed] [Google Scholar]
- 2.Klift M, Laet CE, McCloskey EV, Hofman A, Pols HA. The incidence of vertebral fractures in men and women: the Rotterdam Study. J Bone Miner Res. 2002;17:1051–1056. doi: 10.1359/jbmr.2002.17.6.1051. [DOI] [PubMed] [Google Scholar]
- 3.Finnern HW, Sykes DP. The hospital costs of vertebral fractures in the EU. Osteoporos Int. 2003;14:429–436. doi: 10.1007/s00198-003-1395-2. [DOI] [PubMed] [Google Scholar]
- 4.Riggs BL, Melton LJ (1995) The worldwide problem of osteoporosis: insight afforded by epidemiology. Bone Suppl 5:S505–S511 [DOI] [PubMed]
- 5.Riggs BL, Melton LJ. Involutional osteoporosis. N Engl J Med. 1986;314(26):1676–1685. doi: 10.1056/NEJM198606263142605. [DOI] [PubMed] [Google Scholar]
- 6.Cohen LD. Fractures of the osteoporotic spine. Orthop Clin N Am. 1990;21(1):143–150. [PubMed] [Google Scholar]
- 7.Phillips FM. Minimally invasive treatments of osteoporotic vertebral compression fractures. Spine. 2003;28(15S):S45–S53. doi: 10.1097/00007632-200308011-00009. [DOI] [PubMed] [Google Scholar]
- 8.Silverman SL. The clinical consequences of vertebral compression fracture. Bone. 1992;13(Suppl 2):S27–S31. doi: 10.1016/8756-3282(92)90193-Z. [DOI] [PubMed] [Google Scholar]
- 9.Shen WJ, Shen YS. Nonsurgical treatment of three-column thoracolumbar junction burst fractures without neurologic deficit. Spine. 1999;24:412–415. doi: 10.1097/00007632-199902150-00024. [DOI] [PubMed] [Google Scholar]
- 10.Lau E, Ong K, Kurtz S, Schmier J, Edidin A. Mortality following the diagnosis of a vertebral compression fracture in the medicare population. J Bone Jt Surg Am. 2008;90:1479–1486. doi: 10.2106/JBJS.G.00675. [DOI] [PubMed] [Google Scholar]
- 11.Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cummings SR. Vertebral fractures and mortality in older women: a prospective study. Study of Osteoporotic Fractures Research Group. Arch Intern Med. 1999;159:1215–1220. doi: 10.1001/archinte.159.11.1215. [DOI] [PubMed] [Google Scholar]
- 12.Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA. Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet. 1999;353:878–882. doi: 10.1016/S0140-6736(98)09075-8. [DOI] [PubMed] [Google Scholar]
- 13.Johnell O, Kanis JA, Odén A, Sernbo I, Redlund-Johnell I, Petterson C, Laet C, Jönsson B. Mortality after osteoporotic fractures. Osteoporos Int. 2004;15:38–42. doi: 10.1007/s00198-003-1490-4. [DOI] [PubMed] [Google Scholar]
- 14.Been HD, Poolman RW, Ubags LH. Clinical outcome and radiographic results after surgical treatment of post/traumatic thoracolumbar kyphosis following simple type A fractures. Eur Spine J. 2004;13:101–107. doi: 10.1007/s00586-003-0576-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Magerl F et al (1994) A comprehensive classification of thoracic and lumbar injuries. Eur Spine J 3:184–201 [DOI] [PubMed]
- 16.Galibert P, Deramond H, Rosat P, Le Gars D. Note préliminaire sur le traitement des angiomes vertébraux par vertébroplastie percutanée. Neurochirurgie. 1987;33:166–168. [PubMed] [Google Scholar]
- 17.Diamond TH, Champion B, Clark WA. Management of acute osteoporotic vertebral fractures: a nonrandomized trial comparing percutaneous vertebroplasty with conservative therapy. Am J Med. 2003;114:257–265. doi: 10.1016/S0002-9343(02)01524-3. [DOI] [PubMed] [Google Scholar]
- 18.Heini PF, Walchli B, Berlemann U. Percutaneous transpedicular vertebroplasty with PMMA: operative technique and early results. A prospective study for the treatment of osteoporotic compression fractures. Eur Spine J. 2000;9:445–450. doi: 10.1007/s005860000182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kobayashi K, Shimoyama K, Nakamura K, Murata K. Percutaneous vertebroplasty immediately relieves pain of osteoporotic vertebral compression fractures and prevents prolonged immobilization of patients. Eur Radiol. 2005;15:360–367. doi: 10.1007/s00330-004-2549-0. [DOI] [PubMed] [Google Scholar]
- 20.Liliang PC, Su TM, Liang CL, Chen HJ, Tsai YD, Lu K. Percutaneous vertebroplasty improves pain and physical functioning in elderly osteoporotic vertebral compression fracture patients. Gerontology. 2005;51:34–39. doi: 10.1159/000081432. [DOI] [PubMed] [Google Scholar]
- 21.McKiernan F, Faciszewski T, Jensen R (2004) Quality of life following vertebroplasty. J Bone Jt Surg Am 86-A:2600–2606 [DOI] [PubMed]
- 22.Barr JD, Barr MS, Lemley TJ, McCann RM. Percutaneous vertebroplasty for pain relief and spinal stabilization. Spine. 2000;25:923–928. doi: 10.1097/00007632-200004150-00005. [DOI] [PubMed] [Google Scholar]
- 23.Perez-Higueras A, Alvarez L, Rossi R, Quinones D, Al-Assir I. Percutaneous vertebroplasty: long term clinical and radiological outcome. Neuroradiology. 2002;44:950–954. doi: 10.1007/s00234-002-0856-1. [DOI] [PubMed] [Google Scholar]
- 24.Tohmeh AG, Mathis JM, Fenton DC, Levine AM, Belkoff SM. Biomechanical efficacy of unipedicular versus bipedicular vertebroplasty for the management of vertebral osteoporotic fractures. Spine. 1999;24:1772–1776. doi: 10.1097/00007632-199909010-00004. [DOI] [PubMed] [Google Scholar]
- 25.Berlemann U, Ferguson SJ, Nolte LP, Heini PF. Adjacent vertebral failure after vertebroplasty. A biomechanical investigation. J Bone Jt Surg Br. 2002;84-B:748–752. doi: 10.1302/0301-620X.84B5.11841. [DOI] [PubMed] [Google Scholar]
- 26.Buchbinder R; Osborne RH, Ebeling PR, Wark JD, Mitchell P, Wriedt C, Graves S, Staples MP, Murphy B (2009) A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. New Engl J Med 361(6):557–568 [DOI] [PubMed]
- 27.Kallmes DF, Comstock BA, Heagerty PJ, Turner JA, Wilson DJ, Diamond TH, Edwards R, Gray LA, Stout L, Owen S, Hollingworth W, Ghdoke B, Annesley-Williams DJ, Ralston SH, Jarvik JG (2009) A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med 361(6):569–579 [DOI] [PMC free article] [PubMed]
- 28.Klazen CA, Verhaar HJ, Lampmann LE, Juttmann JR, Blonk MC, Jansen FH, Tielbeek AV, Schoemaker MC, Buskens E, van der Graaf Y, Janssens X, Fransen H, van Everdingen KJ, Muller AF, Mali WP, Lohle PN (2007) VERTOS II: percutaneous vertebroplasty versus conservative therapy in patients with painful osteoporotic vertebral compression fractures; rationale, objectives and design of a multicenter randomized controlled trial. Trials 8:33 [DOI] [PMC free article] [PubMed]
- 29.Jarvik JG, Hollingworth W. VERTOS: a step in the right direction. AJNR Am J Neuroradiol. 2007;28(3):561–562. [PMC free article] [PubMed] [Google Scholar]
- 30.Wardlaw D, Cummings SR, Meirhaeghe J, Bastian L, Tillman JB, Ranstam J, Eastell R, Shabe P, Talmadge K, Boonen S. Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a randomised controlled trial. Lancet. 2009;373(9668):1016–1024. doi: 10.1016/S0140-6736(09)60010-6. [DOI] [PubMed] [Google Scholar]