Abstract
Low back pain is regarded as the primary cause of occupational disability in many countries worldwide. However, there is a lack of valid assessment of kinematic spine and trunk parameters to provide further insight into occupational spine loads. A new 3-dimensional mobile measurement system (3D-SpineMoveGuard) was developed and evaluated by means of repeated dynamic and isometric trunk positions by 10 male and 10 female volunteers. The interclass correlation coefficient indicates high test–retest reliability (r = 0.975–0.999) of the 3D-SpineMoveGuard. Moreover, analysis of validity revealed almost identical results for the new measurement system. The evaluation study indicates a good scientific quality for the use in occupational task analyses. The objective assessment of indirectly measured spine and trunk kinematics will give further insight to predict and prevent job-related spine loads.
Keywords: 3D-SpineMoveGuard, Occupational medicine, Back pain, Ergonomics
Introduction
About 80% of the population in industrialized countries will suffer from back pain during their lifetime [1, 2]. Back pain is not only restricted to the elderly: highest injury rates are documented for mid-agers of the working population [3, 4]. Low back pain is estimated to be the number one disabling injury in Germany and many other countries [2, 5]. Moreover, once a person is affected by severe back pain it often reoccurs within the next years [6].
The primary occupational risk factors for low back pain are biomechanical stressors such as lifting, bending, twisting, awkward postures, isometric postures, high frequent actions, etc. Additionally, many “psycho-social stressors” are documented as co-factors; however, they are more likely to be involved in the recurrence of the initial biomechanical caused injury [7–9]. Low back pain is a multifactorial syndrome which makes the identification of work-related risk factors difficult.
Thus, the valid assessment of occupational risk factors is of paramount importance and has been part of recent scientific studies [10–12]. The focus of direct measurement systems was the analysis of spine loads resulting from load bearing occupational demands. However, only a few systems consider the kinematic demands of the job. As a result only occupational activities with high physical workloads have been adequately evaluated. In addition, epidemiological studies revealed that unspecific low back pain is not only linked to load bearing tasks. Awkward postures (bending, twisting, rotating) and kinematic specifications like repetitive movements or isometric postures are also highly correlated to low back pain [5, 9, 13–15]. Yet, for the overwhelming majority of job tasks or workplaces there is no way to derive occupational risk indicators for the spine from work-specific postures and movements of spine and trunk. Moreover, most existing measurement systems consist of relatively bulky sensors. These hardware requirements make it difficult to use the systems in occupational environments without encumbering the worker. Neither can they be used in differing situations (standing, sitting, walking, etc.). The use of the same system in different workplaces, however, would enable the comparison of spine-related risk indicators [16]. Furthermore, to extend the knowledge about work-related spine loads as a predictor of low back pain, a valid and reliable measurement system is necessary to quantify data of trunk and spine postures and movements [5, 17, 18].
The general aim of the study was the development of a lightweight, mobile measurement system for assessing postures and movements of trunk and spine. The sonoSens® Monitor (Friendly Sensor AG, Jena, Germany) was used to assess 3D movements and postures within the three spinal segments [cervical (CS), thoracic (TS) and lumbar (LS)] [19–21]. To record sagittal trunk inclination as an important parameter to predict occupation-related risk indicators for the spine an inclinometer was added to the system [10, 13]. Besides these hardware requirements, a new data analysing software was developed to standardize the evaluation of dynamic or isometric trunk action.
The present paper gives a concise description of the technical specifications of the new 3D-SpineMoveGuard (3D-SMG) and presents the results of the evaluation study. Additionally, the objectively calculated kinematic parameters will be discussed in order to assess spine-related risk indicators at the workplace.
Materials and methods
Components of the 3D-SpineMovementGuard (3D-SMG)
sonoSens® Monitor
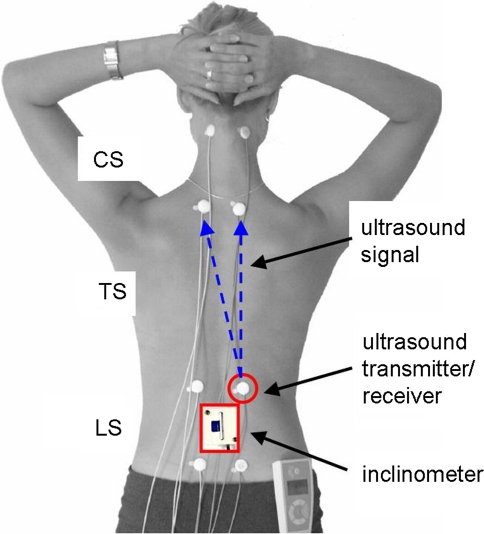
The sonoSens® Monitor is an ultrasound-based measurement device which is largely described elsewhere [19–21]. In brief: four pairs of ultrasound transmitters and receivers (diameter 20 mm, height 4 mm) were fixated on the skin (Fig. 1) with adhesive tape. For each channel the “skin distance” (shorter or longer traveling times of the ultrasound signal through the skin) between transmitter and receiver is determined at a sampling rate of 10 Hz. Transmitters and receivers are cable-connected to a small data logger. Variations in inter-transmitter skin distance represent changes in spine positions within the associated spine segment. The data points of the 12-channel system represent a 3D model (sagittal-, frontal- and horizontal plane) of the external spine curvature. Data can be recorded for up to 10 h.
Fig. 1.
Standardised positions of the ultrasound transmitters and receivers as well as inclinometer position. Each transmitter sends a vertical and diagonal coded signal to capture position differences between transmitter/receiver of CS, TS and LS. Changes in the sagittal and frontal body plane are captured by the vertical signal. Differences in the horizontal plane are recorded by the diagonal channel. CS cervical spine, TS thoracic spine, LS lumbar spine
To document the direction (“flexion”/“extension”, “right”/“left”) of movements or postures the signals were made comparable by software algorithms (“JSpinal” is described below) to the spine segment lengths in the reference position “upright body position” (see below). During this process, the dimension of data is changed from millimeters to percentage. With regard to the indices below (SLI, FLI, HLI) upright standing is set to the segment specific value “0” [21]. Positive values represent flexion (sagittal = SLI), right lateral flexion (frontal = FLI) or right rotation (horizontal = HLI), negative values vice versa.
 |
 |
 |
Inclinometer
Forward and backward bending of the trunk is an important factor to assess spine exposure [14, 22]. Recent studies have shown the advantages of sagittal posture measurements by inclinometer within the region of the lumbar spine [17, 23]. Because the sonoSens® Monitor cannot assess sagittal trunk inclination independent of spine movements, it was necessary to integrate a sagittal inclinometer. An one-dimensional capacitive dielectric liquid based inclinometer (NA4-70, Seika Mikrosystemtechnik GmbH, Kempten, Germany) was fit into a plastic box [50 mm × 50 mm × 32 mm (length × width × height) weight: 70 g]. The box was taped to the skin with the top edge at the middle of the spinous process of the second lumbar vertebra (Fig. 1). The inclinometer is connected via cable to a data logger. The range of measurement was adjusted between +110° and −30° (flexion/extension). Data was captured at a sampling rate of 10 Hz for durations of up to 10 h.
Data analysing software “JSpinal”
A new Java™ based data analysing software (JSpinal) was developed to:
merge and synchronize data of the different measurement devices (sonoSens® Monitor, inclinometer and heart rate monitor),
aggregate data and standardize documentation, data screening and pre-processing of the row data,
export the merged and pre-processed dataset to statistical software and/or database applications.
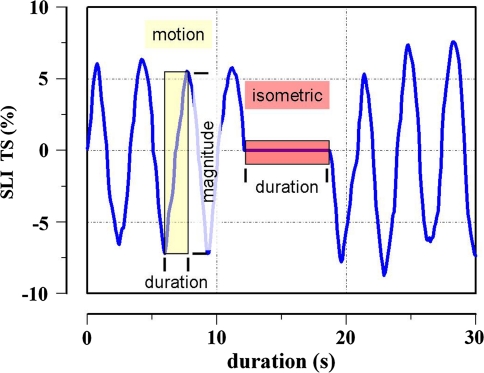
The most important step of this software project was the implementation of algorithms to derive and calculate magnitude, duration, direction and velocity of every single spine and trunk motion as well as to derive and calculate duration and position of every single isometric spine and trunk posture (Fig. 2).
Fig. 2.
Example of the relative 3D-SMG signal within the sagittal plane (SLI) of the thoracic spine. Automatically detected segments of motion (magnitude, direction, duration and velocity) and isometric (duration and position) are marked
Algorithm (1) motion analysis
Data segments were classified as “motion” if a continuous increase or decrease (from data point to data point) of intersegmental spine length exceeded a defined threshold. Furthermore, interruptions of spine movements were accepted within a time offset of 0.5 s (for example, to exclude artifacts of movement).
Algorithm (2) isometric analysis
Data segments were classified as “isometric” if the defined threshold were not exceeded by the consecutive data points (opposite situation of motion analysis). No interruptions were accepted to prolong isometric duration.
Both algorithms were continuously applied to all channels of the dataset.
Evaluation study
Purpose of the study was the scientific evaluation of the newly developed hardware and software components of the 3D-SMG by means of reference positions. Because the measurement technology is identical for different body planes and spine regions (cervical, thoracic and lumbar spine), only the data for sagittal postures and movements of spine and trunk will be shown to evaluate the system:
Test–retest reliability.
Validity.
Data of the frontal and horizontal plane are shown in the appendix (Table 4).
Table 4.
Mean values ( ), standard deviation (SD) and ICC values (r) of measurements during the final posture of “maximum lateral bending of the trunk to the left” and “maximum rotation of the trunk to the right” (n = 20)
), standard deviation (SD) and ICC values (r) of measurements during the final posture of “maximum lateral bending of the trunk to the left” and “maximum rotation of the trunk to the right” (n = 20)
| Measurements | Test repetitions of reference positions | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | ICC | ||||||
 |
SD |  |
SD |  |
SD |  |
SD |  |
SD | r | |
| “Maximum lateral bending of the trunk to the left” | |||||||||||
| FLI TS (%) | −12.4 | 2.4 | −12.5 | 2.4 | −12.5 | 2.7 | −12.4 | 2.6 | −12.5 | 2.7 | 0.988 |
| FLI LS (%) | −16.7 | 4.3 | −16.6 | 4.5 | −16.7 | 4.4 | −16.5 | 4.7 | −16.6 | 4.5 | 0.881 |
| “Maximum rotation of the trunk to the right” | |||||||||||
| HLI TS (%) | 6.1 | 3.3 | 6.0 | 3.2 | 6.2 | 3.1 | 6.0 | 3.0 | 6.3 | 3.0 | 0.995 |
| HLI LS (%) | 7.6 | 3.7 | 7.7 | 3.7 | 7.7 | 3.6 | 7.8 | 3.6 | 7.7 | 3.6 | 0.996 |
Data are shown for each test repetition
FLI frontal length index, HLI horizontal length index
Statistics (over all): repeated measures analysis of variance, inner subject factor p > 0.05; between subjects factor p ≤ 0.05. Inter-class-correlation (ICC), p ≤ 0.05
Subjects
20 young adult volunteers without any history of chronic or severe nor acute back pain participated in the study (Table 1). The majority of the participants were active or former physical education students. Before testing, all volunteers were informed about aim, scope and procedures of the study and gave their written consent. The study was evaluated and accepted by the ethics commission of the German Sport University.
Table 1.
Biometric characteristics of the 20 volunteers
| Variable | Men (n = 10) | Women (n = 10) | ||
|---|---|---|---|---|
| Mean ± SD | Range | Mean ± SD | Range | |
| Age, years | 29 ± 5 | 22–36 | 27 ± 4 | 22–36 |
| Body weight, kg | 75.4 ± 5.8 | 68.5–89.0 | 64.3 ± 5.7 | 57.0–75.0 |
| Body height, m | 1.80 ± 0.04 | 1.75–1.86 | 1.72 ± 0.08 | 1.56–1.81 |
| BMI, kg/m² | 23.2 ± 1.9 | 20.7–27.2 | 21.8 ± 1.6 | 19.0–23.4 |
Values are means ± SD
Reference positions
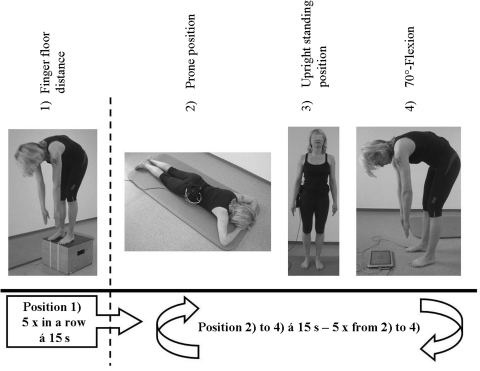
The following samples of static and dynamic reference positions were derived and used to evaluate the 3D-SMG (Fig. 3):
- Position 1: finger–floor distance (dynamic) was assessed by maximum flexion of the upper body. Subjects stood on top of a platform and kept their legs straight during the flexion.
- Test procedure Five repetitions of maximum finger–floor distance tests were performed. The maximum time of flexion was set to 15 s. Resting periods were also set to 15 s in an upright body position.
-
Measurements Distance from the fingertips to the platform-level was assessed with a tape measure. Same, positive or negative distances (0 or ±cm) for every repetition were recorded.“Schober’s measure” was assessed with a tape measure as the maximum prolongation of the signed skin markers from the upright body position to the fully flexed body position.The 3D-SMG was used to determine differences in LS curvature within the sagittal plane by relative (%) length changes compared to the upright body position. Moreover, trunk inclination was assessed by means of maximum degree in the flexed body position.
- Position 2: Prone position (static) was assessed on a gymnastic pad in a defined posture; the hands were placed on top of each other. The forehead rested on top of the crossed hands. The legs were kept straight while the feet were in an external rotation with the heels touching.
-
Test procedure The prone position was kept for 15 s and repeated five times. Between the trials one repetition of “upright standing position” and “70°-flexion” had to be performed.Measurements The 3D-SMG was used to assess relative changes in spine curvature within the sagittal plane of LS and TS. Moreover, trunk inclination was recorded to compare upper body position from trial to trial.
-
-
Position 3: Upright standing position (static) was assessed in a defined posture; feet were placed in a hip-wide position, knees straight, arms hanging relaxed at the side of the trunk and the head was held according to the Frankfurt horizontal [24].
Test procedure The standing position had to be kept for 15 s and repeated five times. Between the trials one repetition of “70°-flexion” and “prone position” had to be performed.
Measurements The 3D-SMG was used to assess relative changes in spine curvature within the sagittal plane of CS, TS and LS. Moreover, trunk inclination was recorded to compare upper body position from trial to trial.
-
Position 4: 70°-flexion (dynamic) was assessed in a defined movement procedure; feet were placed in a hip-wide position, knees straight and the arms being held relaxed in front of the body. Furthermore, a flat screen monitor was put in front of the feet that showed the degree position of the inclinometer.
Test procedure Starting from an upright position the volunteers were instructed to bend forward slowly until they could see “70°” on the monitor. This “70°-position” was to be kept for 15 s. The procedure was repeated five times. Between the trials one repetition of “prone position” and “upright standing position” had to be performed.
Measurements The 3D-SMG was used to assess relative spine curvature changes within the sagittal plane of LS and TS. Moreover, trunk inclination was recorded to compare upper body position from trial to trial.
Fig. 3.
Reference positions used: finger–floor distance was repeated 5 times in a row; positions 2–4 were performed consecutively and this sequence was repeated 5 times
The whole study followed a fixed protocol from the standardized instrumentation and placement of the sensors until the end of the repetition of each reference position. In addition to the described reference positions, postures and movements in the frontal and horizontal plane were also recorded (Appendix Table 4). However, due to the identical technical conditions and to preserve readability only the data within the sagittal plane are described in the “Results” section.
Data management and statistical analyses
Data from each test (3D-SMG, Schober’s sign or finger–floor distance) were extracted with the developed software “JSpinal” for every single trial.
Statistical analyses were performed using SPSS™ 17.0. Normal distribution was assessed by Kolmogorov–Smirnov test. Pearson correlation coefficient (r) was used to calculate bivariate relations. In addition, to assess the reliability of the data, the interclass correlation coefficient (ICC) was calculated for the five posture repetitions. Analysis of variance (ANOVA) for repeated measures was used to assess group differences. If the main factor revealed significant differences post hoc analyses (Newman–Keuls test) were used for multiple cell comparison. The significance level was chosen at p < 0.05.
According to statistical standards reliability was rated as “poor” for r < 0.8, “fair” for r = 0.8–0.9 and “good” for r > 0.9 [25]. Validity was assumed, if ANOVA for repeated measures yield consistent results within individual and different measurements.
Results
The Kolmogorov–Smirnov test confirmed normal distributions of the data for all variables.
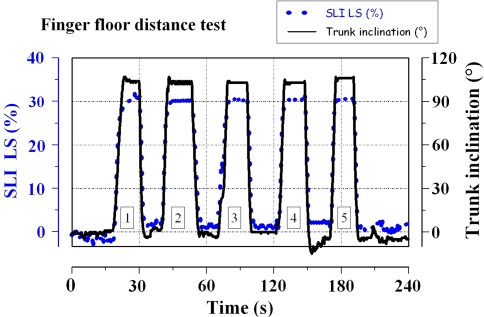
A generic time-course of 3D-SMG signals during the assessment of finger–floor distance is shown in Fig. 4. The corresponding data analysis revealed uniform results for all parameters: significant within- and between-subject effects were confirmed for the factor “test repetition” by ANOVA for repeated measures (p < 0.05). Table 2 shows a continuous decrease in finger–floor distance and a corresponding increase in Schober’s measure, sagittal spine curvature (SLI LS) and inclination of the trunk. To estimate reliability of the system, ICC was calculated for all measures. Significant correlation coefficients could be obtained for every investigated variable (Table 3).
Fig. 4.
Example of time-course data from sagittal movements of the lumbar spine (SLI LS) and corresponding trunk inclination during the finger–floor distance test. The value “0” represents the upright body position; positive values indicate spine flexion (SLI LS dotted line) or forward bending of the trunk (solid line). Data are presented as individual case example (n = 1) for the five test repetitions
Table 2.
Mean values  and standard deviations (SD) of measurements during each final posture in the reference positions (n = 20)
and standard deviations (SD) of measurements during each final posture in the reference positions (n = 20)
| Measurements | Test repetitions and reference positions | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | ||||||
 |
SD |  |
SD |  |
SD |  |
SD |  |
SD | |
| “Finger–floor distance” | ||||||||||
| finger–floor distance (cm) | −1.9 | 10.3 | −3.3 | 9.9 | −4.0 | 9.9 | −4.8 | 9.4 | −5.4 | 9.4 |
| Schober’s sign (cm) | 15.6 | 1.0 | 15.7 | 1.0 | 15.8 | 1.0 | 15.8 | 1.0 | 15.8 | 1.0 |
| SLI LS (%) | 35.7 | 9.2 | 36.0 | 9.4 | 36.3 | 9.4 | 36.6 | 9.5 | 36.7 | 9.6 |
| Trunk inclination (°) | 96.5 | 9.6 | 97.2 | 9.4 | 97.9 | 9.3 | 98.6 | 9.1 | 98.7 | 8.8 |
| “Prone position” | ||||||||||
| SLI TS (%) | 3.87 | 2.28 | 4.27 | 2.51 | 4.06 | 2.97 | 4.29 | 2.67 | 4.59 | 2.67 |
| SLI LS (%) | 1.19 | 4.24 | 0.19 | 4.38 | 0.86 | 4.87 | 1.37 | 4.10 | 1.51 | 4.61 |
| Trunk inclination (°) | 81.6 | 4.07 | 81.6 | 4.07 | 81.7 | 4.35 | 81.8 | 4.26 | 81.7 | 4.58 |
| “Upright standing” | ||||||||||
| SLI CS (%) | 0.20 | 1.81 | −0.20 | 1.42 | 0.00 | 0.00 | −0.34 | 1.91 | −0.11 | 1.95 |
| SLI TS (%) | 0.03 | 0.70 | 0.04 | 0.44 | 0.00 | 0.00 | 0.15 | 0.66 | 0.28 | 0.79 |
| SLI LS (%) | 0.60 | 2.57 | 0.37 | 1.13 | 0.00 | 0.00 | 0.45 | 1.21 | 0.01 | 1.40 |
| Trunk inclination (°) | 0.18 | 1.38 | 0.05 | 1.17 | 0.00 | 0.00 | 0.37 | 1.30 | 0.25 | 1.27 |
| “70°-flexion” | ||||||||||
| Schober’s sign (cm) | 15.3 | 0.9 | 15.3 | 0.9 | 15.3 | 0.9 | 15.3 | 0.9 | 15.3 | 0.9 |
| SLI LS (%) | 32.9 | 9.4 | 32.4 | 9.4 | 32.7 | 9.4 | 32.6 | 9.5 | 32.7 | 9.5 |
| Trunk inclination (°) | 70 | – | 70 | – | 70 | – | 70 | – | 70 | – |
Data are shown for test repetition 1–5
SLI sagittal length index
Table 3.
Bivariate data correlation as documented by Pearsons correlation coefficients for test repetition 1 versus 2, 2 versus 3, 3 versus 4, 4 versus 5 and 1 versus 5
| Measurements | Reference positions | |||||
|---|---|---|---|---|---|---|
| 1 vs. 2 (r) | 2 vs. 3 (r) | 3 vs. 4 (r) | 4 vs. 5 (r) | 1 vs. 5 (r) | ICC (R) | |
| “Finger–floor distance” | ||||||
| finger–floor distance (cm) | 0.993 | 0.993 | 0.997 | 0.994 | 0.971 | 0.997 |
| Schober’s sign (cm) | 0.983 | 0.994 | 0.987 | 0.992 | 0.966 | 0.996 |
| SLI LS (%) | 0.997 | 1.000 | 0.999 | 0.999 | 0.992 | 0.999 |
| Trunk inclination (°) | 0.992 | 0.990 | 0.990 | 0.994 | 0.943 | 0.995 |
| “Prone position” | ||||||
| SLI TS (%) | 0.809 | 0.772 | 0.950 | 0.964 | 0.921 | 0.975 |
| SLI LS (%) | 0.956 | 0.957 | 0.950 | 0.973 | 0.853 | 0.983 |
| Trunk inclination (°) | 0.876 | 0.961 | 0.961 | 0.964 | 0.811 | 0.981 |
| “Upright standing” | ||||||
| SLI CS (%) | 0.759 | 0.787 | 0.736 | 0.828 | 0.861 | 0.880 |
| SLI TS (%) | 0.910 | 0.845 | 0.839 | 0.869 | 0.897 | 0.975 |
| SLI LS (%) | 0.886 | 0.943 | 0.923 | 0.897 | 0.912 | 0.983 |
| Trunk inclination (°) | 0.943 | 0.967 | 0.966 | 0.985 | 0.918 | 0.981 |
| “70°-flexion” | ||||||
| Schober’s sign (cm) | 0.999 | 0.999 | 1.000 | 1.000 | 0.999 | 1.000 |
| SLI LS (%) | 0.965 | 0.999 | 1.000 | 1.000 | 0.965 | 0.994 |
| Trunk inclination (°) | – | – | – | – | – | – |
SLI sagittal length index
Every correlation coefficient yielded significant results (p < 0.05; n = 20). Test–retest reliability was rated by the interclass correlation coefficient (ICC). Each ICC yielded significant results (p < 0.05; n = 20)
Data analysis (ANOVA) of the prone position revealed significance in between-subject effects only (p < 0.05); within the subjects, prone positions were almost identical (p > 0.05; Table 2). Moreover, with regard to the standard values of reliability, ICCs indicate good and significant (p < 0.05) correlations (Table 3). The results of the second static reference position “upright standing” show neither between- nor within-subject differences for each parameter (p > 0.05; Table 2). Furthermore, ICCs of the upright standing positions reveal significant (p < 0.05) fair to good correlation coefficients (Table 3).
Data of the 3D-SMG device and Schober’s measure indicate almost identical characteristics for the dynamic reference position 70°-flexion: within the subjects, no difference in the means could be found from repetition to repetition (p > 0.05; Table 2). Values differ only between the participants (p < 0.05). In accordance with ANOVA, ICC revealed high and significant associations (p < 0.05; Table 3). Due to the test procedure the values of the inclinometer were excluded from analysis because no within- nor between-subject differences could be expected.
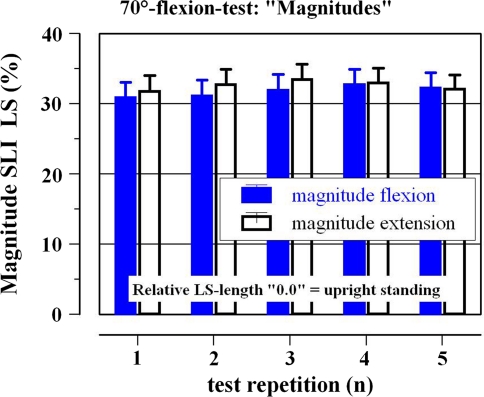
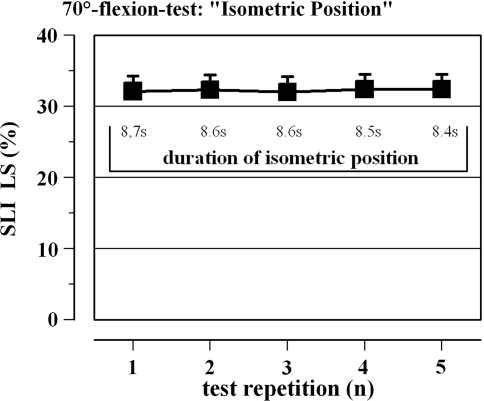
The generic analyses of dynamic and isometric parameters of the 3D-SMG were performed by extracting kinematic characteristics of the lumbar spine (LS) during the 70°-flexion test. Data analysis revealed that flexion and re-extension of the trunk was achieved by mean magnitudes of 31.8 ± 9.6% and 32.6 ± 9.3% (p ≥ 0.05; Fig. 5). The magnitudes were constant for each volunteer (p ≥ 0.05) but differed significantly between subjects (p < 0.05). Parameters of ICC indicate a strong and significant relation of the magnitudes from repetition to repetition for flexion and extension movements, respectively (r = 0.993 and r = 0.991; p < 0.05). Moreover, the isometric positions in a 70°-trunk flexion were kept for 8.6 ± 0.1 s. Figure 6 illustrates the duration and the LS position of the five isometric phases in 70°-trunk flexion. Statistics of isometric LS position can be taken from Tables 2 and 3 (part “70°-flexion”).
Fig. 5.
Magnitudes of sagittal lumbar spine (SLI LS) movements during the reference position 70°-flexion. Closed bars represent magnitudes of flexion, open bars magnitudes of extension. Data are presented for the five test repetitions (means ± standard error, n = 20)
Fig. 6.
Sagittal flexion of lumbar spine (SLI LS) and duration of the flexed posture during the isometric position in 70° trunk inclination. The value “0” represents the straight body position; positive values represent spine flexion (SLI LS). Data are presented for the five test repetitions (means ± standard error, n = 20)
Discussion
A simple and reproducible test procedure was chosen to evaluate the new measurement system. One-dimensional reference positions were defined to reduce possible bias of complex and hardly reproducible postures and movements [25]. Parameters of different sensors (ultrasound and inclinometer), manually taken measurements (finger–floor distance, Schober’s measure) as well as a biofeedback procedure (70°-flexion) were drawn upon to assess repeatability and validity of the 3D-SMG.
Data analysis revealed identical characteristics for all measures within the same reference positions: The data of the 3D-SMG were highly and significantly correlated (ICC 0.975–0.999) among themselves and in accordance with further manually obtained measures (ICC 0.996–1.000). With regard to the evaluation criteria validity, the equal results of the ANOVA for repeated measures document the accordance of 3D-SMG parameters and external measures. Thus, the results indicate a strong validity of the 3D-SMG for the assessment of trunk inclination and spine curvature in any given body posture. The results of the current study are consistent with the analyses of former studies with the basic ultrasound system (sonoSens® Monitor), whose reproducibility has already been rated as “good” or “very good” for short- and long-term test–retest reliability [19, 20]. However, theses evaluations were done without an inclinometer and the kinematic analysis of the new software “JSpinal”.
The present study is limited by the fact that there is no “gold standard” to assess spine movements. 3-D camera systems [26, 27] could have been an alternative to validate the 3D-SMG. However, they bear very high costs (inefficiency) and were not available for this study [28]. Nonetheless, the selected reference positions were chosen by a scientific expert committee. It cannot be excluded that there might be some better postures or movements to reduce methodical bias. Nevertheless, the present study used a standardized and efficient protocol, which yielded consistent results over different methods. In general, the indirect measures captured at the surface of the skin are limited by the fact that the assumed spine kinematics may not represent the real movements of the spine. The data could also be biased by the varying thickness of subcutaneous fat and the probably non-uniform distributed soft tissue. However, non-invasive methods provide sufficient validity and contribute to volunteer compliance [20, 29].
In addition to these methodical quality criteria, the new software package of the 3D-SMG is able to analyse the data for isometric and dynamic trunk and spine action. To the best of our knowledge the 3D-SMG is the first mobile measurement device to objectively assess kinematic criteria of spine and trunk in three dimensions. The current examples indicate the reproducibility of both dynamic (magnitude and direction of movements) and isometric (duration and position of static postures) parameters.
Kinematic trunk and spine parameters are of paramount importance to evaluate spine-related risk indicators at the workplace. As mentioned in the introduction, only weight-bearing tasks can be drawn upon to document occupation-specific strain on the lower back. In industrial workplaces, however, the overwhelming majority of employees are not primarily affected by load bearing tasks [30]. Monotonous, unilateral tasks with static or repetitive demands are common in industrial jobs [5, 23]. Moreover, epidemiological studies have frequently assessed occupation-specific body postures by questionnaire [5, 9, 13–15]. Multivariate data analysis of these studies revealed high risk ratios for awkward body postures or movements with regard to recurrence of low back pain, frequent pain episodes, etc. Although there is strong evidence of these kinematic stressors, a valid data base is missing to quantify occupation-specific characteristics of trunk and spine dynamics.
Occupation-specific analysis with the 3D-SMG will provide new insights in these yet unquantifiable parameters of movement and posture at the workplace. The detailed analyses of different spine segments, three dimensional movements or postures and the continuous, real-time data assessment will provide a valid database to rate occupation-specific risk indicators from the spine [31]. In addition, the data will derive further information on which specific preventive strategies can be based on to reduce spine loads at the workplace. For example: individual kinematic requirements of spine and trunk can be evaluated and used to specify vocational rehabilitation. Besides these individual possibilities the data of 3D-SMG analysis could be useful to evaluate ergonomic innovations. To quantify the impact of such innovations, pre and post analysis of the workplaces are necessary to assess the usefulness of the ergonomic measure.
Conclusion
The evaluation (reliability and validity) of the developed 3D-SMG hard- and software package revealed good to very good results. New kinematic parameters could be presented to rate dynamic and isometric trunk and spine action. It can be expected that further occupational analyses will provide new insights into these highly relevant data of spine loads at the workplace [30]. Furthermore, these data could be of paramount importance for prevention and rehabilitation and to appreciate ergonomic measures.
Conflict of interest
None of the authors has any potential conflict of interest.
Appendix
Position A1
Lateral flexion (static) was assessed in a defined posture: feet were placed in a hip-wide position, knees straight and the arms being held relaxed at the side of the body. The upper body was maximal flexed to the side within the frontal body plane (controlled by the investigator).
Test procedure
Starting from an upright position the volunteers were instructed to bend sideways as far as possible. The maximal lateral position was kept for 15 s. The procedure was repeated five times for the right and left side of the body. Between the trials one repetition of “prone position”, “upright standing, “70°-position” and “rotation” had to be performed.
Measurements
The 3D-SMG was used to assess relative spine curvature changes within the frontal plane of LS and TS.
Position A2
Rotation (static) was assessed in a defined posture: feet were kept together, knees straight and the arms being held relaxed at the side of the body. The upper body was maximal rotated to the side within the horizontal body plane (controlled by the investigator).
Test procedure
Starting from an upright position the volunteers were instructed to rotate as far as possible. The maximal rotated position was kept for 15 s. The procedure was repeated five times to the right and left side of the body. Between the trials one repetition of “prone position”, “upright standing, “70°-position” and “lateral bending” had to be performed.
Measurements
The 3D-SMG was used to assess relative spine curvature changes within the horizontal plane of LS and TS (see Table 4).
References
- 1.Hofmann F, Stössel U, Michaelis M, Nübling M, Siegel A. Low back pain and lumbago-sciatica in nurses and a reference group of clerks: results of a comparative prevalence study in Germany. Int Arch Occup Environ Health. 2002;75:484–490. doi: 10.1007/s00420-002-0332-6. [DOI] [PubMed] [Google Scholar]
- 2.Schmidt CO, Kohlmann T. What do we know about the symptoms of back pain? Epidemiological results on prevalence, incidence, progression and risk factors. Z Orthop. 2005;143:292–298. doi: 10.1055/s-2005-836631. [DOI] [PubMed] [Google Scholar]
- 3.Dimov M, Bhattacharya A, Lemasters G, Atterbury M, Greathouse L, Ollila-Glenn N. Exertion and body discomfort perceived symptoms associated with carpentry tasks: an on-site evaluation. AIHAJ. 2000;61:685–691. doi: 10.1202/0002-8894(2000)061<0685:EABDPS>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Guo HR, Chang YC, Yeh WY, Chen CW, Guo YL. Prevalence of musculoskeletal disorder among workers in Taiwan: a nationwide study. J Occup Health. 2004;46:26–36. doi: 10.1539/joh.46.26. [DOI] [PubMed] [Google Scholar]
- 5.Schneider S, Lipinski S, Schiltenwolf M. Occupations associated with a high risk of self-reported back pain: representative outcomes of a back pain prevalence study in the Federal Republic of Germany. Eur Spine J. 2006;15:821–833. doi: 10.1007/s00586-005-1015-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Waddell G, Burton AK. Occupational health guidelines for the management of low back pain at work: evidence review. Occup Med. 2001;51:124–135. doi: 10.1093/occmed/51.2.124. [DOI] [PubMed] [Google Scholar]
- 7.Hoogendoorn WE, Poppel MN, Bongers PM, Koes BW, Bouter LM. Systematic review of psychosocial factors at work and private life as risk factors for back pain. Spine. 2000;25:2115–2125. doi: 10.1097/00007632-200008150-00017. [DOI] [PubMed] [Google Scholar]
- 8.Nieuwenhuyse A, Fatkhutdinova L, Verbeke G. Risk factors for first-ever low back pain among workers in their first employment. Occup Med. 2004;54:513–519. doi: 10.1093/occmed/kqh091. [DOI] [PubMed] [Google Scholar]
- 9.Shelerud RA. Epidemiology of occupational low back pain. Clin Occup Environ Med. 2006;5:501–528. doi: 10.1016/j.coem.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 10.Derksen JC, Riel MP, Wingerden JP, Snijders CJ. A comparison of working postures of parcel sorters using three different working methods. Ergonomics. 1994;37:299–302. doi: 10.1080/00140139408963647. [DOI] [PubMed] [Google Scholar]
- 11.Juul-Kristensen B, Hansson GA, Fallentin N, Andersen JH, Ekdahl C. Assessment of work postures and movements using a video-based observation method and direct technical measurements. Appl Ergon. 2001;32:517–524. doi: 10.1016/S0003-6870(01)00017-5. [DOI] [PubMed] [Google Scholar]
- 12.Marras WS, Knapik GG, Ferguson S. Lumbar spine forces during manoeuvring of ceiling-based and floor-based patient transfer devices. Ergonomics. 2009;52:384–397. doi: 10.1080/00140130802376075. [DOI] [PubMed] [Google Scholar]
- 13.Chung MK, Lee I, Kee D. Quantitative postural load assessment for whole body manual tasks based on perceived discomfort. Ergonomics. 2005;48:492–505. doi: 10.1080/00140130400029217. [DOI] [PubMed] [Google Scholar]
- 14.Delleman NJ, Dul J. International standards on working postures and movements ISO 11226 and EN 1005-4. Ergonomics. 2007;50:1809–1819. doi: 10.1080/00140130701674430. [DOI] [PubMed] [Google Scholar]
- 15.Fallentin N, Juul-Kristensen B, Mikkelsen S, et al. Physical exposure assessment in monotonous repetitive work-the PRIM study. Scand J Work Environ Health. 2001;27:21–29. doi: 10.5271/sjweh.583. [DOI] [PubMed] [Google Scholar]
- 16.Beek AJ, Frings-Dresen MHW. Assessment of mechanical exposure in ergonomic epidemiology. Occup Environ Med. 1998;55:291–299. doi: 10.1136/oem.55.5.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vieira ER, Kumar S. Working postures: a literature review. J Occup Rehab. 2004;14:143–159. doi: 10.1023/B:JOOR.0000018330.46029.05. [DOI] [PubMed] [Google Scholar]
- 18.Wunderlich M, Rüther T, Eßfeld D, Rohde U, Eger T, Leyk D. Rückenschmerzen und Wirbelsäulenbelastungen–Befragung des zahnme-dizinischen Personals in der Bundeswehr. Wehrmed Mschr. 2009;53:230–234. [Google Scholar]
- 19.Baum K, Hoy S, Essfeld D. Continuous monitoring of spine geometry: a new approach to study back pain in space. Int J Sports Med. 1997;18:331–333. doi: 10.1055/s-2007-972748. [DOI] [PubMed] [Google Scholar]
- 20.Friedrich M. Measuring lumbar sagittal posture in sewage workers using an ultrasonic device. JMR. 2002;6:135–145. [Google Scholar]
- 21.Kopp S, Friedrich A, Pfaff G, Langbein U. Influence of occlusion frames on the functional movement area of cervical, thoracic and lumbar vertebrae A pilot study. Manuelle Medizin. 2003;41:39–51. doi: 10.1007/s00337-002-0200-1. [DOI] [Google Scholar]
- 22.McGill MS, Fenwick CMJ. Using a pneumatic support to correct sitting posture for prolonged periods: a study using airline seats. Ergonomics. 2009;32:1162–1168. doi: 10.1080/00140130902936067. [DOI] [PubMed] [Google Scholar]
- 23.Schneider S, Schmitt H, Zoller S, Schiltenwolf M. Workplace stress, lifestyle and social factors as correlates of back pain: a representative study of the German working population. Int Arch Occup Environ Health. 2005;78:253–269. doi: 10.1007/s00420-004-0576-4. [DOI] [PubMed] [Google Scholar]
- 24.International Organization of Standardization (2006) ISO 11226:2000 Evaluation of static working posture. Geneva, Switzerland
- 25.Bortz J, Döring N (2006) Forschungsmethoden und Evaluation für Human- und Sozialwissenschaftler, 4 edn. Springer, Heidelberg
- 26.Wong WY, Wong MS. Trunk posture monitoring with inertial sensors. Eur Spine J. 2008;17:743–753. doi: 10.1007/s00586-008-0586-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goodvin C, Park EJ, Huang K, Sakaki K. Development of a real-time three-dimensional spinal motion measurement system for clinical practice. Med Biol Eng Comput. 2006;44:1061–1075. doi: 10.1007/s11517-006-0132-3. [DOI] [PubMed] [Google Scholar]
- 28.Arnold J. APALYS—Eine Möglichkeit zur Berechnung der Wirbelsäulenbelastung beim Heben von Lasten. Die Säule. 2000;10:30–33. [Google Scholar]
- 29.Taylor WR, Consmüller T, Rohlmann A. A novel system for the dynamic assessment of back shape. Med Eng Phys. 2010;32:1080–1083. doi: 10.1016/j.medengphy.2010.07.011. [DOI] [PubMed] [Google Scholar]
- 30.Lis AM, Black KM, Korn H, Nordin M. Association between sitting and occupational LBP. Eur Spine J. 2007;16:283–298. doi: 10.1007/s00586-006-0143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wunderlich M, Jacob R, Rüther T, Leyk D (2010) Analysis of spinal stress during surgery in otolaryngology. HNO 58:791–798 [DOI] [PubMed]