Abstract
Even though a number of studies have evaluated postural adjustments based on kinematic changes in subjects with low back pain (LBP), kinematic stability has not been examined for abnormal postural responses during the one leg standing test. The purpose of this study was to evaluate the relative kinematic stability of the lower extremities and standing duration in subjects with and without chronic LBP. In total, 54 subjects enrolled in the study, including 28 subjects without LBP and 26 subjects with LBP. The average age of the subjects was 37.8 ± 12.6 years and ranged from 19 to 63 years. The outcome measures included normalized holding duration and relative kinematic stability. All participants were asked to maintain the test position without visual input (standing on one leg with his/her eyes closed and with the contra lateral hip flexed 90°) for 25 s. The age variable was used as a covariate to control confounding effects for the data analyses. The control group demonstrated significantly longer holding duration times (T = −2.78, p = 0.007) than the LBP group (24.6 ± 4.2 s vs. 20.5 ± 6.7 s). For the relative kinematic stability, there was a difference in dominance side (F = 9.91, p = 0.003). There was a group interaction between side and lower extremities (F = 11.79, p = 0.001) as well as an interaction between age and dominance side (F = 7.91, p = 0.007). The relative kinematic stability had a moderate negative relationship with age (r = −0.60, p = 0.007) in subjects without LBP. Clinicians need to understand the effects of age and relative stability, which decreased significantly in the single leg holding test, in subjects with LBP in order to develop effective rehabilitation strategies.
Keywords: Relative kinematic stability, Low back pain, Age, Postural stability, One leg standing test
Introduction
Poor postural alignment, dynamic standing balance, and postural strategies are often found in individuals with chronic low back pain (LBP) [1–3]. Control of postural balance is a complex function involving numerous neuromuscular processes which are dependent upon sensory input from the vestibular, visual, and somatosensory systems [4, 5]. Proprioception is a key component of the somatosensory system and is responsible for providing the central nervous system with afferent information used for neuromuscular control [6]. There are receptors responsible for this information which could be affected by dysfunction in the lumbar spine [7]. Accordingly, subjects with LBP may have altered postural control and balance deficits as well as reduced proprioception in the spine, which have been reported in several studies [2, 3, 7, 8].
Although there are several balance tests available [9–11], most examination tools are limited to measuring mechanical stability and cannot quantify functional mobility due to subjective judgment by the examiner. For example, one study investigated postural stability which was assessed and quantified by the Berg Balance test and vertical force measures [12]. There was a lack of objective and reliable methods for basic research regarding postural stability, which remains an important issue. Therefore, kinematic measurement with motion analysis could be utilized to observe comprehensive movement patterns in angular displacement and to specify three dimensional segmental differences in subjects with and without LBP.
There are several reports utilizing motion analysis for subjects with and without LBP with regard to interactions with the lower extremities [13–15]. As Bouisset initially proposed, stabilization of the pelvis and trunk is necessary for all movements of the upper and lower extremities [16]. It is evident that altered lumbopelvic control and stability could affect the lower extremities. The function of the spine should be considered in the context of the whole body [17]. Other studies also demonstrated a relationship between trunk muscle activity and lower extremity movement [14, 15]. Therefore, it is important to understand that a possible trunk dysfunction might present different lower extremity movement patterns in subjects with LBP compared with subjects without LBP.
Challenging tasks would be useful to examine when investigating stability control and aberrant motion resulting from compensatory mechanisms in subjects with LBP. Several studies also reported that LBP patients demonstrate reduced holding durations during the one leg standing test [3, 18]. Due to the importance in orthopedic physical assessment, there are several studies on kinematic patterns during one leg stance in healthy subjects [19–21]. The results suggest that at least two different forces, a large horizontal force and a restorative moment, are generated for balance maintenance during one leg standing. Another study investigated the movement of the ankle, knee, hip, and trunk of the supporting leg during one leg stance [21]. However, these studies were conducted in healthy subjects and focused on movement of the supporting leg.
Our study focused on three-dimensional angular displacement differences between subjects with and without LBP during the one leg standing test. Since movements of the lower extremities occur three dimensionally, we calculated the combined rotation angles (Rx, Ry, and Rz) to measure overall normalized balance stability. To our knowledge, no previous study has attempted to evaluate balance performance and identify the aberrant motion of the pelvis and lower extremity in subjects with LBP during the one leg standing test.
Therefore, the purpose of this study was to examine angular displacement of postural stability for the lower extremities (pelvis, thigh, shank, and foot) in subjects with and without LBP. It was hypothesized that, compared with subjects without LBP, the subjects with LBP would demonstrate shorter holding durations during the test. We expect that the differences in segmental movement of the lower extremities between subjects with and without LBP during the test may lead to improved understanding of postural stability and effective postural assessment.
Methods
Target population
Volunteers for this study were subjects who presented with LBP, met study inclusion criteria, and experienced a disturbing impairment or abnormality in the functioning of the low back for more than 2 months [22]. Subjects were eligible to participate if they (1) were 18 years of age or older, (2) had LBP for more than 2 months without pain referral into the lower extremities, and (3) had a current episode of recurrent LBP. Subjects were excluded from participation if they (1) had a diagnosed psychological illness that might interfere with the study protocol, (2) had overt neurological signs (sensory deficits or motor paralysis), and/or (3) were pregnant. Participants were withdrawn from the study if they requested to withdraw. The control group included age- and gender- matched subjects in order to eliminate the concurrent effects between groups.
Subjects were recruited from a health promotion society in Seoul, Korea. Subjects who expressed interest in the study became eligible for the study. Only subjects with and without LBP that had been enrolled in the society were contacted to minimize the risk of confounding effects over the study period as well as to increase the internal validity of the data. The dominant leg could be defined as the leg with which the largest horizontal hop distance was reached [23]. However, the dominant side had to be distinguished from the preferred leg. In our study, the dominant leg was defined as the leg that a subject automatically uses for a single leg jump [24]. All subjects were right leg dominant, and thus the right quadriceps and hamstring muscles were analyzed as the dominant side. The contra lateral side, or left lower extremity, was referred to as the non-dominant side.
Those subjects who met study inclusion criteria received information regarding the purpose and methods of the study and signed a copy of the Institutional Review Board approved consent form.
Outcome measures
Pain/disability was inferred from self-reported scores on the Oswestry low back pain disability index (ODI) [25]. The ODI is one of the most frequently used tools for measuring chronic disability [26]. A sum is calculated and presented as a percentage, where 0% represents no disability and 100% the worst possible disability.
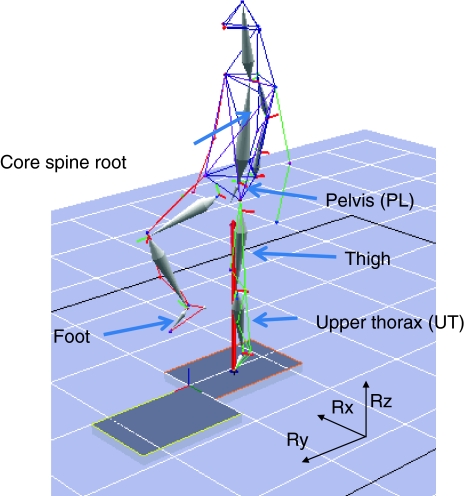
The one leg standing test (stork test) was conducted at the Motion Analysis Laboratory. Originally, this test was used to determine the mobility of the ligament in the sacroiliac joint [27]. Subjects performed two trials (right and left leg holding) in which they were instructed to stand quietly in the upright position with the tested foot parallel at hip width. The order of the tested lower limb was random. The subjects were given disposable hospital slipper socks with nonskid bottoms to wear during the test and had the Helen Hayes full body (with head) reflective marker set attached to specific sites on their bodies with adhesive tape rings. Each subject stood upright for 25 s on a force plate surface with his/her eyes closed and the contra lateral hip flexed 90° (Fig. 1). Balance stability is reflected by the subject’s ability to maintain the one-legged stance while the other foot is self supported. Subjects were given a 1-min rest between trials to avoid fatigue.
Fig. 1.
One leg standing balance test. A subject stands on one leg with the contra lateral hip flexed 90° for 25 s. During the test, the subject maintains stability while the reflective markers collect kinematic data from the three axes of the pelvis, thigh, shank, and foot
In Fig. 1, the core spine axis was calculated based on the coordinates between the pelvic plane and the shoulder girdle plane. The pelvic plane included both sides of the anterior superior iliac spine and the second sacrum level, while the shoulder plane included the glenohumeral joints and the seventh cervical spine level. Therefore, the core spine axis is the direct vertical line between the shoulder and pelvic planes.
The pelvis and lower extremities (foot, shank, and thigh) were included to compare kinematic changes during the test. Synchronized kinematic and force plate data were recorded and processed by six digital cameras capturing three-dimensional full body kinematic motion (Motion Analysis Corporation, Santa Rosa, CA, USA) using Advanced Mechanical Technology (AMTI, Inc., Newton, MA, USA). Synchronized kinematic data were recorded and processed by six digital cameras capturing three-dimensional full body kinematic motions sampling at 120 Hz. Marker position was acquired using a 6-camera motion analysis system and subsequently low-pass filtered with a low-pass cut-off frequency of 2 Hz.
Balance changes imposed during one leg standing were measured using a six-channel force platform, and the recordings lasted 25 s. Before the experiment, data were collected from the unloaded platform to determine the zero offset. All kinematic data were filtered and time synchronized within the test cycle. Digital video data were collected and tracked using EVA 5.20. Digital video and force plate data were then imported into Orthotrac 5.2 (Motion Analysis Corporation, Santa Rosa, CA, USA). The AMTI OR6-5 force plate was used to record the ground reaction forces (Fx, Fy, and Fz) and the force moments (Mx, My, and Mz) in orthogonal directions at a sampling frequency of 1,000 Hz. The signals were amplified (4,000 times), band-pass filtered (10–1,050 Hz), and recorded.
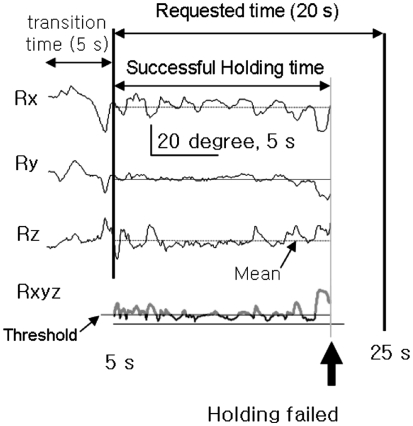
The successful holding time was measured as the total holding time until the subject failed to maintain stability during 20 s of the 25 s holding test protocol. During the initial 5 s, each subject was allowed to move his/her leg from the standing position. Therefore, the subsequent 20 s of the test was used as the requested holding time. The three-dimensional rotations included anterior-posterior (Rx), medio-lateral (Ry), and vertical (Rz). The combined rotation (Rxyz) was computed as a square sum of the three directional rotation angles of which the mean was subtracted to have zero-mean (Eq. 1). The relative stability represents the duration when the body segment is in a static position; therefore, this stability was quantified to normalize the capacity of motor control during the balance test.
The segments of standing tolerance time for Rxyz are drawn as solid thick lines in Fig. 2, which is based on the concept that limited motor control by damaged sensory feedback (ex. chronic back pain or tendon injury) could not maintain body segments within a certain tolerance during a motor task [28].
 |
1 |
Fig. 2.
Identification of successful relative stability for computing the stability index. The analysis time window was obtained from the total requested time, which excluded the initial transition time (5 s) from standing to leg holding. The relative stability was the ratio between successful holding time and total requested time (20 s after initial 5 s). The successful holding time was measured as the total duration until the subject failed to maintain stability (thick arrow). The relative stability time was the ratio between standstill time and successful holding time. The standstill time was the summation of temporal segments where the three dimensional rotation (Rxyz) of the tested axis was below the threshold until holding failed (Eq.1)
Statistical analysis
Statistical analyses were completed using SPSS 16 (SPSS, Chicago, IL, USA). Normality was assessed for each of the dependent variables (kinematic changes on foot, shank, thigh, and pelvis). An independent t test was used to analyze dependent variables based on group (subjects with and without LBP). A repeated measure analysis of variance (ANOVA) was used for each dependent variable to determine the main effects of group, and the age variable was used as a covariate to eliminate any confounding effects.
All continuous dependent variables were evaluated using the general linear model. Assumptions of repeated measures, including homogeneity of variance, normal distribution of data, and sphericity, were tested with Mauchly’s test [29]. For all statistical tests, type I error rate was set at 0.05.
Results
Description of samples
A summary of subject demographics and the relationship of groups are summarized in Table 1. In total, 54 subjects enrolled in the study, including 28 subjects without LBP and 26 subjects with LBP. The average age of the subjects was 37.8 ± 12.6 years and ranged from 19 to 63 years. The subjects without LBP were slightly younger (35.0 ± 10.0 years) than the subjects with LBP (46.7 ± 14.5 years), but there was no significant difference between groups (T = −1.67, p = 0.10). In addition, there was no gender difference between groups (χ2 = 0.12, p = 0.78).
Table 1.
Summary of subject demographics and bivariate relationship of groups with selected demographics
| Variable | Total | Control group | Pain group | Statistic | p |
|---|---|---|---|---|---|
| Number of subjects | 54 | 28 | 26 | ||
| Gender | |||||
| Female | 20 | 11 | 9 | χ2 = 0.12 | 0.78 |
| Male | 34 | 17 | 17 | ||
| Age (years) | |||||
| Range | 19–63 | 20–47 | 19–63 | t = −1.67 | 0.10 |
| Mean ± SD | 37.76 ± 12.61 | 35.04 ± 10.07 | 40.69 ± 14.50 | ||
| Height (cm) | |||||
| Range | 150–181 | 155–181 | 150–177 | t = 1.94 | 0.06 |
| Mean ± SD | 167.55 ± 7.89 | 169.17 ± 8.10 | 165.44 ± 7.30 | ||
| Weight (kg) | |||||
| Range | 43–94 | 49–82 | 43–94 | t = −1.22 | 0.23 |
| Mean ± SD | 65.54 ± 11.06 | 63.92 ± 8.74 | 65.63 ± 12.90 | ||
| Oswestry pain scale | |||||
| Range | N/A | N/A | 0.20–0.29 | N/A | N/A |
| Mean ± SD | 0.24 ± 0.13 | ||||
The subjects without LBP were slightly taller (169.1 ± 8.1 cm) than the subjects with LBP (165.4 ± 7.3 cm). The height variable was not significantly different between groups (T = 1.94, p = 0.06). Weight was also not significantly different between groups (T = −1.22, p = 0.23). The ODI pain scale for the subjects with LBP was 24%, which is the moderate disability level (20–40%).
Distribution of stability index
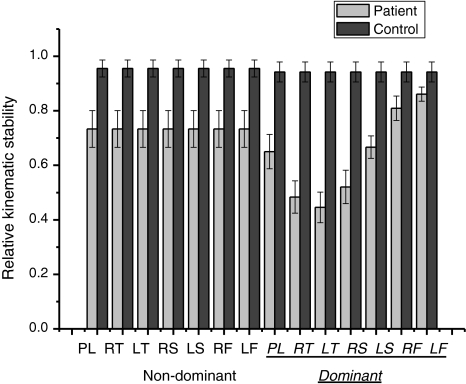
As shown in Fig. 3, the relative kinematic stability for the lower extremities was analyzed. There was a difference in dominance side (F = 9.91, p = 0.003), but no difference in part of the lower extremity (F = 1.04, p = 0.31). There was a group interaction between side and lower extremities (F = 11.79, p = 0.001).
Fig. 3.
The relative kinematic stability values obtained during the test. There was a difference in dominance side (F = 9.91, p = 0.003), but no differences in the lower extremities (F = 1.04, p = 0.31). There was a group interaction between side and lower extremities (F = 11.79, p = 0.001). (PL pelvis, RT right thigh, LT left thigh, RS right shank, LS left shank, RF right foot, LF left foot)
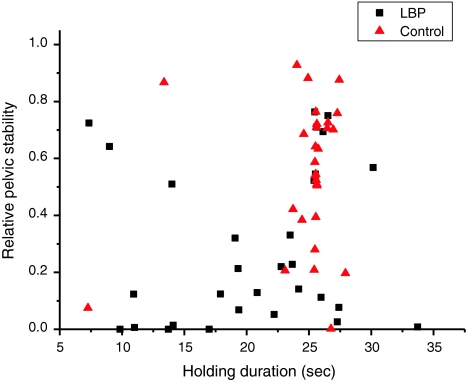
In Fig. 4, relative pelvic stability during the test was compared with holding duration. The subjects without LBP demonstrated longer hold times (24.6 ± 4.2 s) than the subjects with LBP (20.5 ± 6.7 s). There was also a difference in successful holding time during the test between groups (T = −2.78, p = 0.007).
Fig. 4.
The relationship between relative pelvic stability and holding duration during the one leg standing test. The control group demonstrated significantly longer holding duration times (T = −2.78, p = 0.007) than the LBP group (24.6 ± 4.2 s vs. 20.5 ± 6.7 s). There were no significant degrees of association for the control (r = 0.28, p = 0.14) or LBP (r = 0.12, p = 0.53) groups
The demographic variables were analyzed between groups. The aging factor was considered as a covariate, and there was an interaction with dominance side (F = 7.91, p = 0.007), but no interaction with lower extremity (F = 0.69, p = 0.40). The relative pelvic stability of the subjects without LBP was negatively correlated with age (r = −0.60, p = 0.007). There were no significant correlations with height (r = −0.14, p = 0.56), weight (r = −0.06, p = 0.81), foot length (r = −0.27, p = 0.26), or foot width (r = −0.14, p = 0.57).
The relative stability of the subjects with LBP indicated no significant correlations with age (r = −0.23, p = 0.24), weight (r = −0.09, p = 0.66), height (r = −0.11, p = 0.60), foot length (r = −0.13, p = 0.52), or foot width (r = −0.06, p = 0.75).
Discussion
The purpose of this study was to compare postural stability focusing on lower extremity kinematics during one leg standing in subjects with and without LBP. As we hypothesized, subjects with LBP demonstrated shorter holding duration times than the control subjects. This result is consistent with other studies which concluded that the control group demonstrated better stability than the patient group [2].
Regarding the segmental movement of the lower extremities during balance coordination, there was a group interaction between dominance side and lower extremities which indicated that the relative stability in the pelvis, thigh, and shank was significantly lower in subjects with LBP compared with subjects without LBP during the dominant leg holding test. Previously, one study on the lumbar spine found greater lumbopelvic motion in the transverse plane during lower limb movements of LBP patients [14]. The study suggested the need to understand the dynamic coordination of the lumbopelvic region during other functional activities.
Several studies have focused on the interaction between the lumbar spine and pelvis during diverse active movements such as stand-to-sit or gait and how it is altered in subjects with LBP [30, 31]. These results suggest that the pelvic segment demonstrates increased axial trunk rotation during the tasks, which is consistent with our results. Tropp and Odenrick recognized movement strategies for maintaining balance during one-legged standing. They reported that, during periods of disequilibrium, balance was maintained through movements at the hip joint which creates large restoring horizontal forces [32]. Increased movement in the pelvis segment during the holding test of the dominant side could be the reason.
One plausible explanation for these unstable segments is that altered direction of the pelvis led to rotation of the shank to the opposite direction to maintain stability. Further research with electromyography (EMG) is required to investigate this hypothesis. The use of EMG in the one leg standing test would also allow investigators to examine muscle activity of the steady supporting leg and its relationship with balance control.
As shown in Fig. 4, the control group demonstrated significantly higher relative pelvic stability as well as longer holding duration times than the subjects with LBP. Therefore, when relative pelvic stability during the test was compared with holding duration, the subjects with LBP were plotted in the left lower side of the graph.
One possible explanation for decreased balance performance in subjects with LBP is reduced proprioception in the spine. Although the knowledge surrounding proprioception is relatively limited because it is such a complex function, several studies have found that proprioceptive deficits in individuals with LBP might contribute to a lack of stability [8, 33, 34]. Another explanation for decreased balance performance in LBP subjects might be altered muscle function. As McGregor et al. [17] reported, there is a range of evidence that the hip joint of the lower limb should be considered in the context of the function of the spine as a whole body. This function is more important during one leg standing posture because of the holding leg.
The aging factor was considered as a covariate, and there was an interaction with dominance side. In addition, the relative pelvic stability of the subjects without LBP was negatively correlated with age. However, there was no significant correlation between relative stability and age in the subjects with LBP. In our study, the subjects without LBP were slightly younger (35.0 ± 10.0) than the subjects with LBP (46.7 ± 14.5), and the standard deviation was greater in the LBP group although there was no significant difference between groups.
One study reported that the initiation timing for triggering both voluntary and induced stepping was delayed substantially regardless of age [35]. The subjects with LBP demonstrated a decrease in spine range of motion and velocity [36]. Our study indicated the significant correlation between age and relative pelvic stability in subjects without LBP during one leg standing.
There were some limitations to the current study. One limitation was that it was not possible for every subject to flex his/her hip and knee exactly 90°. Visual inspection of the test starting posture might have resulted in little differences between subjects. However, we calculated the angular displacement changes from the starting posture which was 5 s later instead of the time of initiation of the test. A second limitation was that we did not identify the dominant directions of rotation for each segment. As we combined three rotational angles to determine instability, more research is needed to clarify the increased rotation, especially in the shank segment.
A third potential limitation is the design of the study. Because the study design is cross-sectional, it is unknown whether people in the LBP subgroup developed LBP as a result of early and increased lumbopelvic motion.
Despite these limitations, the quantification of balance deficits is valuable to a number of populations including subjects with LBP. The identification of individuals with balance deficits can lead to appropriate exercises not only for rehabilitation of LBP patients but also for the elderly population who demonstrate an increased risk for falls. Follow-up, randomized controlled trials are needed to investigate the characteristics of lumbar spine postural stability.
Conclusion
Relative stability decreased significantly in the lower extremities of subjects with LBP, especially in the pelvis and thigh, during the dominant leg holding test. It is important to understand relative stability based on dominance side and lower extremities while considering age between subjects with and without LBP. Clinicians need to understand the effects of age and relative stability in subjects with LBP in order to develop effective rehabilitation strategies.
Acknowledgments
This work was supported by the National Agenda Project (NAP) funded by the Korea Research Council of Fundamental Science & Technology (P-09-JC-LU63-C01). This research was also partially supported by Korea University and the Basic Science Research Program through the National Research Foundation of Korea funded by the Ministry of Education, Science and Technology (2010-0003015).
References
- 1.Nies N, Sinnott PL. Variations in balance and body sway in middle-aged adults. Subjects with healthy backs compared with subjects with low-back dysfunction. Spine. 1991;16:325–330. doi: 10.1097/00007632-199103000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Sung PS, Yoon B, Lee DC. Lumbar spine stability for subjects with and without low back pain during one-leg standing test. Spine (Phila Pa 1976) 2010;35:E753–E760. doi: 10.1097/BRS.0b013e3181d53b9c. [DOI] [PubMed] [Google Scholar]
- 3.Ham YW, Kim DM, Baek JY, Lee DC, Sung PS (2010) Kinematic analyses of trunk stability in one leg standing for individuals with recurrent low back pain. J Electromyogr Kinesiol 20:1134–1140 [DOI] [PubMed]
- 4.Shumway-Cook A, Horak FB. Assessing the influence of sensory interaction on balance: suggestion from the field. Phys Ther. 1986;66:1548–1550. doi: 10.1093/ptj/66.10.1548. [DOI] [PubMed] [Google Scholar]
- 5.Horak FB, Shupert CL, Mirka A. Components of postural dyscontrol in the elderly: a review. Neurobiol Aging. 1989;10:727–738. doi: 10.1016/0197-4580(89)90010-9. [DOI] [PubMed] [Google Scholar]
- 6.Lephart SM, Pincivero DM, Giraldo JL, Fu FH. The role of proprioception in the management and rehabilitation of athletic injuries. Am J Sports Med. 1997;25:130–137. doi: 10.1177/036354659702500126. [DOI] [PubMed] [Google Scholar]
- 7.Gill KP, Callaghan MJ. The measurement of lumbar proprioception in individuals with and without low back pain. Spine (Phila Pa 1976) 1998;23:371–377. doi: 10.1097/00007632-199802010-00017. [DOI] [PubMed] [Google Scholar]
- 8.Brumagne S, Cordo P, Verschueren S. Proprioceptive weighting changes in persons with low back pain and elderly persons during upright standing. Neurosci Lett. 2004;366:63–66. doi: 10.1016/j.neulet.2004.05.013. [DOI] [PubMed] [Google Scholar]
- 9.Brauer SG, Woollacott M, Shumway-Cook A. The interacting effects of cognitive demand and recovery of postural stability in balance-impaired elderly persons. J Gerontol A Biol Sci Med Sci. 2001;56:M489–M496. doi: 10.1093/gerona/56.8.M489. [DOI] [PubMed] [Google Scholar]
- 10.Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther. 2000;80:896–903. [PubMed] [Google Scholar]
- 11.Yelnik A, Bonan I. Clinical tools for assessing balance disorders. Neurophysiol Clin. 2008;38:439–445. doi: 10.1016/j.neucli.2008.09.008. [DOI] [PubMed] [Google Scholar]
- 12.Karlsson A, Frykberg G. Correlations between force plate measures for assessment of balance. Clin Biomech (Bristol, Avon) 2000;15:365–369. doi: 10.1016/S0268-0033(99)00096-0. [DOI] [PubMed] [Google Scholar]
- 13.Gombatto SP, Collins DR, Sahrmann SA, Engsberg JR, Dillen LR. Gender differences in pattern of hip and lumbopelvic rotation in people with low back pain. Clin Biomech (Bristol, Avon) 2006;21:263–271. doi: 10.1016/j.clinbiomech.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 14.Scholtes SA, Gombatto SP, Dillen LR. Differences in lumbopelvic motion between people with and people without low back pain during two lower limb movement tests. Clin Biomech (Bristol, Avon) 2009;24:7–12. doi: 10.1016/j.clinbiomech.2008.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Silfies SP, Bhattacharya A, Biely S, Smith SS, Giszter S. Trunk control during standing reach: a dynamical system analysis of movement strategies in patients with mechanical low back pain. Gait Posture. 2009;29:370–376. doi: 10.1016/j.gaitpost.2008.10.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bouisset S. Relationship between postural support and intentional movement: biomechanical approach. Arch Int Physiol Biochim Biophys. 1991;99:A77–A92. doi: 10.3109/13813459109145919. [DOI] [PubMed] [Google Scholar]
- 17.McGregor AH, Hukins DW. Lower limb involvement in spinal function and low back pain. J Back Musculoskelet Rehabil. 2009;22:219–222. doi: 10.3233/BMR-2009-0239. [DOI] [PubMed] [Google Scholar]
- 18.Nies N, Sinnott PL. Variations in balance and body sway in middle-aged adults. Subjects with healthy backs compared with subjects with low-back dysfunction. Spine (Phila Pa 1976) 1991;16:325–330. doi: 10.1097/00007632-199103000-00012. [DOI] [PubMed] [Google Scholar]
- 19.Gauffin H, Areblad M, Tropp H. Three-dimensional analysis of the talocrural and subtalar joints in single-limb stance. Clin Biomech. 1993;8:307–314. doi: 10.1016/0268-0033(93)90005-3. [DOI] [PubMed] [Google Scholar]
- 20.King DL, Zatsiorsky VM. Periods of extreme ankle displacement during one-legged standing. Gait Posture. 2002;15:172–179. doi: 10.1016/S0966-6362(01)00189-8. [DOI] [PubMed] [Google Scholar]
- 21.Riemann BL, Myers JB, Lephart SM. Comparison of the ankle, knee, hip, and trunk corrective action shown during single-leg stance on firm, foam, and multiaxial surfaces. Arch Phys Med Rehabil. 2003;84:90–95. doi: 10.1053/apmr.2003.50004. [DOI] [PubMed] [Google Scholar]
- 22.Klenerman L, Slade PD, Stanley IM, Pennie B, Reilly JP, Atchison LE, Troup JD, Rose MJ. The prediction of chronicity in patients with an acute attack of low back pain in a general practice setting. Spine. 1995;20:478–484. doi: 10.1097/00007632-199502001-00012. [DOI] [PubMed] [Google Scholar]
- 23.Harst JJ, Gokeler A, Hof AL. Leg kinematics and kinetics in landing from a single-leg hop for distance. A comparison between dominant and non-dominant leg. Clin Biomech (Bristol, Avon) 2007;22:674–680. doi: 10.1016/j.clinbiomech.2007.02.007. [DOI] [PubMed] [Google Scholar]
- 24.Malinzak RA, Colby SM, Kirkendall DT, Yu B, Garrett WE. A comparison of knee joint motion patterns between men and women in selected athletic tasks. Clin Biomech (Bristol, Avon) 2001;16:438–445. doi: 10.1016/S0268-0033(01)00019-5. [DOI] [PubMed] [Google Scholar]
- 25.Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66:271–273. [PubMed] [Google Scholar]
- 26.Ciccone DS, Just N, Bandilla EB. Non-organic symptom reporting in patients with chronic non-malignant pain. Pain. 1996;68:329–341. doi: 10.1016/S0304-3959(96)03216-2. [DOI] [PubMed] [Google Scholar]
- 27.Haneline MT, Cooperstein R, Young M, Birkeland K. Spinal motion palpation: a comparison of studies that assessed intersegmental end feel vs excursion. J Manipulative Physiol Ther. 2008;31:616–626. doi: 10.1016/j.jmpt.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 28.Learman KE, Myers JB, Lephart SM, Sell TC, Kerns GJ, Cook CE. Effects of spinal manipulation on trunk proprioception in subjects with chronic low back pain during symptom remission. J Manipulative Physiol Ther. 2009;32:118–126. doi: 10.1016/j.jmpt.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 29.Kleinbaum DG, Kupper LK, Muller KE. Applied regression analysis and other multivariable methods. Belmont: Duxbury Press; 1988. [Google Scholar]
- 30.Shum GL, Crosbie J, Lee RY. Three-dimensional kinetics of the lumbar spine and hips in low back pain patients during sit-to-stand and stand-to-sit. Spine (Phila Pa 1976) 2007;32:E211–E219. doi: 10.1097/01.brs.0000259204.05598.10. [DOI] [PubMed] [Google Scholar]
- 31.Whittle MW, Levine D. Three-dimensional relationships between the movements of the pelvis and lumbar spine during normal gait. Hum Mov Sci. 1999;18:681–692. doi: 10.1016/S0167-9457(99)00032-9. [DOI] [Google Scholar]
- 32.Tropp H, Odenrick P. Postural control in single-limb stance. J Orthop Res. 1988;6:833–839. doi: 10.1002/jor.1100060607. [DOI] [PubMed] [Google Scholar]
- 33.Brumagne S, Cordo P, Lysens R, Verschueren S, Swinnen S. The role of paraspinal muscle spindles in lumbosacral position sense in individuals with and without low back pain. Spine (Phila Pa 1976) 2000;25:989–994. doi: 10.1097/00007632-200004150-00015. [DOI] [PubMed] [Google Scholar]
- 34.Brumagne S, Janssens L, Knapen S, Claeys K, Suuden-Johanson E. Persons with recurrent low back pain exhibit a rigid postural control strategy. Eur Spine J. 2008;17:1177–1184. doi: 10.1007/s00586-008-0709-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rogers MW, Hedman LD, Johnson ME, Martinez KM, Mille ML. Triggering of protective stepping for the control of human balance: age and contextual dependence. Brain Res Cogn Brain Res. 2003;16:192–198. doi: 10.1016/S0926-6410(02)00273-2. [DOI] [PubMed] [Google Scholar]
- 36.Marras WS, Wongsam PE. Flexibility and velocity of the normal and impaired lumbar spine. Arch Phys Med Rehabil. 1986;67:213–217. [PubMed] [Google Scholar]