Abstract
We retrospectively reviewed plain radiographs from patients with four different diseases that can cause vertebral collapse: osteoporotic vertebral collapse, spinal infection, spinal metastasis, and multiple myeloma. The objective of the study was to find the percentages of intravertebral vacuum phenomena and vertebral collapse rates in the four groups. The vacuum phenomenon is often observed in osteoporotic compression fractures. However, these phenomena are rarely seen in spinal infection and malignant lesions. Whether the vacuum phenomenon is a benign indicator is not known. We retrospectively reviewed plain radiographs from four groups of patients, including 328 osteoporotic vertebral collapse patients, 317 spinal infection patients, 302 spinal metastasis patients, and 325 multiple myeloma patients. The pattern and occurrence rates of intravertebral vacuum phenomena and vertebral body collapse were analyzed. The occurrence rate of intravertebral vacuum phenomena in patients with osteoporotic vertebral collapse was approximately 18.9%. Only one case of intravertebral vacuum phenomena was observed in patients with spinal infection. Vacuum phenomena were not observed in patients with spinal metastasis. The occurrence rate of intravertebral vacuum phenomena in patients with multiple myeloma was 6.4%. The patterns of intravertebral vacuum phenomena were also analyzed. Intravertebral vacuum phenomena are common in patients with osteoporotic vertebral collapse. Most cases of intravertebral vacuum phenomena are of a benign nature. Moreover, intravertebral vacuum phenomena occur extremely rarely in patients with spinal infection. Such phenomena are also found in patients with multiple myeloma.
Keywords: Vacuum phenomenon, Compression fracture, Multiple myeloma, Metastatic tumor, Spinal infection
Introduction
Osteoporotic vertebral fractures are a common disease in clinical practice. Most fractures heal with conservative treatment, but some may develop into nonunion or pseudoarthrosis. In plain radiographs of vertebral body pseudoarthrosis, the fracture sites often present gas accumulation; this phenomenon is termed the vacuum phenomenon or the vacuum cleft sign [1–3]. Vacuum phenomena often appear as intravertebral radiolucent shadows that are typically band like or linear in shape and are often accompanied by peripheral sclerosis.
The vacuum phenomenon is a common finding in degenerative intervertebral disc [4, 5]. Many studies have demonstrated that intradiscal vacuum phenomena may also occur in pyogenic discitis, especially with gas-forming organisms [6–8]. Intravertebral vacuum phenomena may also be seen in benign vertebral compression fracture. However, whether intravertebral vacuum phenomena with vertebral collapse represent a benign lesion is controversial. Some studies have demonstrated that intravertebral vacuum phenomena are a benign sign [3, 9–13], and others have reported the occurrence of spinal malignancies (especially multiple myeloma) with vertebral collapse in patients with vacuum phenomena [14–16]. The exact frequencies with which intravertebral vacuum phenomena occur in patients with osteoporotic vertebral fracture, spinal infection, and malignant metastasis are still not well established. However, Lane et al. [17] have reported a rate of 11.4% of osteoporotic vertebral fractures with opacified clefts as seen on pre-operative radiographs of patients who underwent vertebroplasty, excluding those who had opted for other non-operative methods of treatment.
The main purpose of this study was to determine the following: (1) the frequency of intravertebral vacuum phenomena in patients with symptomatic osteoporotic vertebral fractures; (2) the percentage of intravertebral vacuum phenomena in patients with spinal infections and the pattern of these phenomena compared with those of patients with benign osteoporotic vertebral fractures; (3) whether vacuum phenomena exist in patients with spinal metastatic tumors with vertebral collapse; and (4) the incidence of vacuum phenomena in patients with multiple myeloma with vertebral collapse.
Materials and methods
We retrospectively and consecutively reviewed plain radiographs of four groups of patients with different diseases that can cause vertebral collapse. Two senior doctors, an orthopedic doctor (Chang) and a radiologist (Wu), reviewed all the radiographs independently. The presence of intravertebral vacuum phenomena was determined by consensus. Only if both reviewers agreed was the presence of intravertebral vacuum phenomena determined. Kappa reliability coefficients were used to assess interobserver reliability.
Group 1: patients with osteoporotic vertebral fractures. We reviewed the medical charts and plain radiographs of 328 consecutive patients (male 146, female 182, mean age 70.9 years) with 472 levels of osteoporotic vertebral fractures (mean 1.43 levels, range 1–6; Table 1), who suffered from back pain, and who had visited and were treated in the clinics of all the departments of our hospital between January and April of 2006. The average dual energy X-ray absorptiometry (DEXA) value of the patients was −2.81 (range −1.5 to −5.1). All patients had previously received medical treatment for their osteoporosis (calcium and vitamin D, and raloxifene, biphosphonate, calcitonin, or teriparatide). The patients had at least one level of vertebral collapse of the spine, which was observed upon analysis of their plain radiographs (anterior–posterior view and lateral view, taken in the supine position). Vertebral collapse was defined as a decrease in height of more than 20% of the anterior, middle, and/or posterior one-third of the vertebral body. Vertebral collapse was determined by measuring the difference in height of the diseased vertebral body as compared to the average height of the adjacent normal vertebral bodies. The incidence of vertebral collapse and vacuum phenomena (defined by the presence of intraosseous gas accumulation in the collapsed vertebral body, as seen in both the anterior and posterior view) was calculated. The patterns of intraosseous gas accumulation in the vertebral body were also analyzed. Interobserver reliability of agreement of the patterns was also evaluated.
Table 1.
Basic clinical data
| Group 1 | Group 2 | Group 3 | Group 4 | p value | |
|---|---|---|---|---|---|
| Number of patients | 328 | 317 | 302 | 325 | |
| Male versus female | 146:182 | 214:103 | 175:127 | 227:98 | |
| Age | 70.93 ± 7.51 | 63.03 ± 16.16 | 67.88 ± 14.2 | 69.45 ± 11.75 | <0.001 |
| Number of vertebral bodies involved | 472 | 647 | 810 | a | |
| Number of vertebral bodies with collapse | 472 | 167 | 141 | 125 | |
| Collapse rate | 100% | 25.8% | 17.4% | a | <0.001 |
| Number of vertebral bodies with intravertebral vacuum phenomena | 89 | 1 | 0 | 8 | |
| Rateb | 18.86% | 0.59% | 0% | 6.4% | <0.001 |
| Patterns | Linear: 44 | Unique Pattern (TB) | Linear: 4 | ||
| Band: 15 | Band: 1 | ||||
| Cloud: 15 | Cloud: 3 | ||||
| Triangular: 6 | |||||
| Multiple linear: 9 |
aThe correct level(s) of involvement could not be evaluated in group 4
bThe number of vertebral bodies with intravertebral vacuum phenomenon/number of vertebral bodies involved
Group 2: patients with spinal infection. We reviewed the medical charts and plain radiographs of 317 consecutive patients who had primary spinal infection and had been treated in our hospital (including the departments of orthopedics, neurosurgery, infectious disease, internal medicine, etc.) between January 2001 and December 2007. All patients had confirmed diagnoses of primary spinal infection upon admission or during hospitalization and included 281 cases of pyogenic spondylitis and 36 cases of tuberculous spondylitis. All patients in this group were confirmed by: (1) endplate destruction with disc space narrowing, with or without vertebral body collapse in plain radiographs; (2) signal change in the involved disc and adjacent vertebral body, with paraspinal abscess and post-contrast rim enhancement; (3) vertebral biopsy showing destruction of the disc or endplate, and proven infiltration of neutrophils or lymphocyte, or granulomatous change in TB cases; (4) biopsy culture or blood culture with positive results of bacteria or tuberculous infection. The incidence of vertebral collapse and vacuum phenomena was analyzed as described for patients with osteoporotic vertebral fractures.
Group 3: patients with spinal metastasis. Between January and December of 2006, medical charts and plain radiographs of 302 hospitalized patients (175 male, 127 female) with confirmed spinal metastasis were reviewed. The tumor type, the incidence of vertebral collapse, and occurrence rate of intravertebral vacuum phenomena among these patients were analyzed as described for patients with osteoporotic vertebral fractures. The number of levels involved was determined by whole body bone scan and/or MRI. The diagnosis was confirmed based on: (1) other organ malignancy with confirmed tissue diagnosis; (2) typical image findings of spinal metastasis such as multi-level and skip lesions in the vertebral bodies with/without cord compression, posterior element involvement, and paraspinal soft tissue mass without signs of spinal infection such as paraspinal abscess, and disc destruction in plain radiographs and MRI.
Group 4: patients with multiple myeloma. Between January 2002 and December 2006, the medical charts and plain radiographs of 325 consecutive hospitalized patients (including new onset and previously diagnosed patients, who were admitted to our hospital) with confirmed diagnoses of multiple myeloma were reviewed. The incidence of vertebral body collapse and the pattern and incidence of intravertebral vacuum phenomena among these patients were analyzed as described for patients with osteoporotic vertebral fractures. The diagnosis followed the criteria of the International Myeloma Working Group for symptomatic myeloma. The diagnoses were confirmed by a series of clinical examinations and investigations, including laboratory studies with findings of monoclonal protein in the urine or serum, plain radiographs or MRI images showing multiple lytic lesions in the skull, long bone and vertebra, and bone marrow biopsy showing clonal plasma cells and evidence of organ damage related to plasma cell disorder. In this group, the Tc 99m bone scan is usually silent, and MRI was not routinely used for screening these patients. As a result, precise evaluation of the number of levels of disorder involved and the collapse rate could not be done. We could only compare the frequency of intravertebral vacuum phenomena per fracture level to that of the other three groups.
Statistical analysis
The demographics of patients in each group were analyzed using the Chi-square method. Age was analyzed using the ANOVA test. The number of vertebral bodies and collapse rate in the first three groups were compared. The rate of presence of vacuum phenomena per fracture level was compared using chi-square method. Significance was defined as p < 0.05. Interobserver reliability in the presence and pattern of vacuum phenomena was evaluated using kappa coefficients (strength of agreement defined as <0 poor, 0.01–0.2 slight, 0.21–0.4 fair, 0.41–0.6 moderate, 0.61–0.8 substantial, and 0.81–1 almost perfect) [18].
Results
In the first group, 356 out of 472 fractures (75.5%) were at the thoracolumbar junction (T11 to L2). Among the 472 collapsed fractures, 89 levels (18.86%) presented with intravertebral vacuum phenomena. These 89 levels were observed in a total of 86 patients. A total of 76 (85.4%) vacuum phenomena occurred at the thoracolumbar junction (T11 to L2). Only three patients showed the presence of vacuum phenomena at two levels.
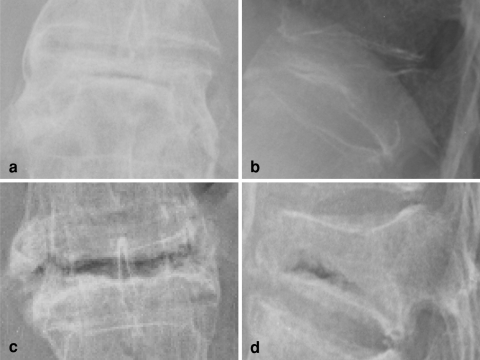
The vacuum phenomena observed were categorized into five patterns, according to the shape of their air distribution: linear type (dense gas accumulation was evenly and continuously distributed in the vertebral body with a thickness of less than 4 mm), band type (dense gas distribution similar to that of the linear type, but with a thickness of more than 4 mm), cloud type (linear or band like with an uneven distribution or irregular shape), triangular type (displayed gas accumulation in the anterior half of the vertebral body with a triangular distribution), and multiple linear type (several lines of gas accumulation but without continuous distribution) (Figs. 1, 2). Overall, 43 out of 89 vacuum phenomena were of the linear type, 15 were of the band type, 15 were of the cloud type, 9 were of the multiple linear type, and 6 were of the triangular type (Table 1). It is important to note, however, that most of the lesions found in this group presented sclerotic changes at the fracture site.
Fig. 1.
Intravertebral vacuum phenomena of the linear and band types. a, b Anterior–posterior (AP) and lateral views of linear type of vacuum phenomena. c, d AP and lateral views of band-type vacuum phenomena
Fig. 2.
Triangular, cloud, and multiple linear types of intravertebral vacuum phenomena. a, b AP and lateral views of triangular-type vacuum phenomena. c, d AP and lateral views of cloud-type vacuum phenomena. e, f AP and lateral views of multiple linear-type vacuum phenomena
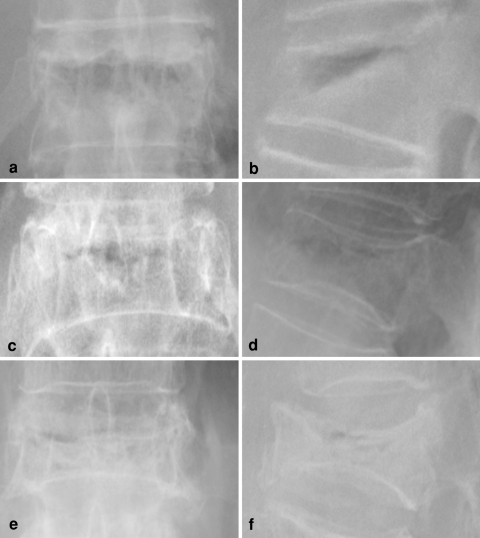
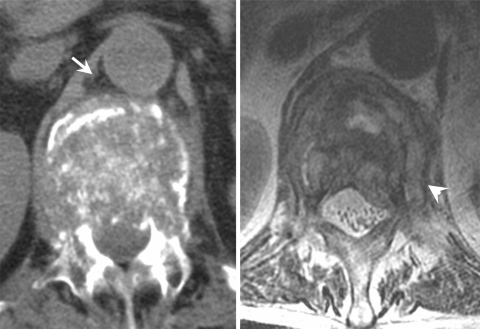
In the 317 patients of the second group, 647 vertebral bodies were identified. Among this group, 124 patients (93 with pyogenic spondylitis and 31 with tuberculous spondylitis) had 167 combined vertebral body collapses (patients with pyogenic spondylitis had 124 levels and those with tuberculous spondylitis had 43 levels). The collapse rate was 21% for patients with pyogenic spondylitis versus 58% for patients with tuberculous spondylitis. Only one patient with tuberculous spondylitis had an intravertebral vacuum phenomenon (Table 1). However, the patterns of the vacuum phenomenon in this patient were different from those seen in patients with osteoporotic vertebral fractures (Figs. 3, 4). The distribution of gas observed within the involved vertebral body was uneven and displayed a bubble-like pattern. Most distinctively, the gas extended into the paravertebral soft tissue, which was not observed in any of the patients with benign osteoporotic vertebral fractures.
Fig. 3.
An 84-year-old male with tuberculous infection. A unique pattern of intravertebral vacuum phenomena was found. Gas accumulation extends into the soft tissue (arrow)
Fig. 4.
Computed tomography of the same patient who showed gas accumulation in the prevertebral soft tissue, which was compatible with findings in plain radiographs (arrow). T2-weighted image of MRI shows paravertebral pus formation (arrowhead)
In the third group, 302 patients with spinal metastasis presented with 810 vertebral body involvements. The primary origins of the observed malignancies included 109 cases of lung cancer, 56 cases of prostate cancer, 48 cases of breast cancer, 14 cases of hepatocellular carcinoma, 12 cases of colon cancer, 6 cases of urothelial cancer, 6 cases of nasopharyngeal cancer, 8 cases of renal cell carcinoma, 7 cases of rectal cancer, 5 cases of cervical cancer, 4 cases of pancreatic cancer, 2 cases of gastric cancer, 1 case each of other kinds of cancer such as invasive schwannoma, fibrous histiocytoma, and synovial sarcoma, and finally 8 cases of unknown origin. A total of 54 vertebral bodies, found in 38 patients, showed vertebral body collapse. However, none of the collapsed bodies identified presented vacuum phenomena.
In the fourth group of 325 patients with confirmed multiple myeloma, 125 vertebral bodies in 73 patients were collapsed. Eight vertebral bodies in 8 patients (8/325 patients, 2.4%) and in 125 levels (8/125 levels, 6.4%) presented vacuum phenomena. The involved vertebral bodies were T11 (1 case), T12 (2 cases), L1 (4 cases), and L3 (1 case). The pattern of gas distribution was of the linear type in four lesions, the cloud type in three lesions, and of the band type in one lesion. All lesions presented sclerotic changes at the fracture sites. Among this group, four patients were initially diagnosed as having benign osteoporotic vertebral fractures and were treated with vertebroplasty. There were no postoperative complications from vertebroplasty in these patients. The pattern of vacuum phenomena observed in this group was very similar to that seen in patients with benign osteoporotic vertebral fractures and the pattern was impossible to differentiate between the two groups (Fig. 5).
Fig. 5.
A 75-year-old man with multiple myeloma. Band-type intravertebral vacuum phenomenon was present in the L3 vertebral body
The collapse rates of four groups were significantly different (p < 0.001). The rates of presence of intravertebral vacuum phenomena in the four groups were significantly different (p < 0.001). The kappa value of interobserver reliability was 0.967 for the presence of the intravertebral vacuum phenomena, and 0.753 for pattern classification.
Discussion
As seen from the results of the current study, vacuum phenomena may not be a definite indicator of benign lesions. However, most vacuum phenomena occur in benign osteoporotic vertebral fractures. Vacuum phenomena caused by spinal infection or metastasis are extremely rare, as we found only one lesion in one patient with infection and none in patients with metastasis. Although rare (2.4% per person, and 6.4% per fracture level), multiple myeloma can cause vacuum phenomena when vertebral collapse occurs.
In the present study, we evaluated intravertebral vacuum phenomena by the evaluation of plain radiographs only. CT scans may have a higher sensitivity for the differentiation of gas than do X-rays, as observed in the evaluation of degenerated discs by CT scan. However, the present study used only plain X-ray and MRI for lesion evaluation because plain X-ray is routinely used in clinical practice, while MRI is the modality of choice in the differential diagnosis among osteoporotic fracture, spinal infection, and other malignancy. On the other hand, all medical expenses are covered by government insurance in our country. It is impossible to routinely perform both CT scan and MRI for all those patients; also, it is difficult to appreciate the vacuum phenomena in MRI.
The differences in vacuum phenomena observed between patients with benign osteoporotic vertebral fractures and infection or metastasis may be due to several factors. First, vertebral collapse during infection or metastasis may actually represent bony destruction or erosion, but not a real fracture, which usually has two or more fracture fragments. Therefore, the opening–closing mechanism may not occur in a collapsed vertebral body, thereby preventing the formation of negative pressure. Second, tissue inflammation during an active infection may promote continuous and dynamic tissue expansion, which may induce fluid accumulation and tissue swelling. Positive, but not negative, pressure may occur at the lesion site. A similar situation may occur in rapidly growing tumor tissue. Hence, vacuum phenomena do not occur easily in collapsed vertebral bodies caused by infection or metastasis. In the present study, only one patient in the infection group presented with vacuum phenomena. This patient suffered from tuberculous spondylitis that involved the anterior and central aspects of the L1 vertebral body. Initially, however, this patient was diagnosed with a benign osteoporotic vertebral fracture, because the upper and lower end plates of the vertebral body appeared intact and an intraosseous vacuum was observed in the plain X-ray. However, paravertebral abscesses could be seen in an axial view by MRI. The mechanism that caused the appearance of vacuum phenomena in this case is unclear. It is thought that tuberculous spondylitis has a more chronic clinical course than does pyogenic infection [19]. When tuberculous infection primarily involves the central region (central-type tuberculous spine) and the intact upper and lower end plates of the vertebral body, a similar flexion–extension motion to that seen in benign vertebral fractures is observed. In such cases, gas accumulation may rarely occur. However, upon review of the plain X-rays, vacuum phenomena appear bubble-like and widely distributed in peripheral tissues (Fig. 3). The pattern of this particular vacuum phenomenon was different from that of the usual vacuum phenomena observed, which are commonly linear or band-like and are evenly distributed with peripheral sclerosis (Fig. 1).
Several case reports have demonstrated that intradiscal vacuum phenomena occur in the spine during infection [6–8]. The pattern of gas accumulation also appeared uneven, similar to the tuberculous spondylitis case we presented. Some groups have suggested that the gas observed in vacuum phenomena may be produced directly by gas-forming organisms [8]. Therefore, caution should be taken when abnormal patterns of vacuum phenomena are identified, by performing additional imaging studies and analyzing indicators of infection such as C-reactive protein (CRP) levels prior to surgical intervention for those lesions. Metastatic tumors of the spine are thought to be composed of solid soft tissue, which may have a rich arterial blood supply. The composition of such tumors makes it difficult to create negative pressure within the tissue, in spite of vertebral body collapse.
Few cases of vacuum phenomena have been identified in patients with multiple myeloma. It is uncertain whether fractures are caused directly by multiple myeloma or whether multiple myeloma creates a situation of osteoporosis resulting in collapse of the vertebral body, as observed in benign osteoporotic fractures. Another possibility is that patients with multiple myeloma coincidentally present with osteoporosis, which may cause vertebral fractures. No matter which possibility is correct, the vacuum phenomena observed in multiple myeloma were similar to those observed in osteoporotic vertebral fractures, making it difficult to differentiate between these two types of vacuum phenomena. This similarity caused the initial misdiagnosis or delayed diagnosis of four patients with multiple myeloma, who were treated with vertebroplasty prior to confirming a diagnosis of multiple myeloma.
Even though vertebral body collapse caused by multiple myeloma can often be misdiagnosed as osteoporotic vertebral fracture, many reports have shown that the pain caused by vertebral body collapse in multiple myeloma can still be managed safely and effectively with vertebroplasty [20, 21].
In summary, intravertebral vacuum phenomena are commonly observed in patients with osteoporotic vertebral fracture, in some patients with multiple myeloma and rarely in spinal infection. However, the pattern of vacuum phenomena in spinal infection is different from that in other diseases. Caution should be taken when an unusual pattern of intravertebral vacuum phenomena is observed, and further studies, such as MRI or CT-guided biopsy, may be necessary before planning further treatment.
Acknowledgments
No funds were received in support of this work.
Conflict of interest No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
References
- 1.Resnick D, Niwayama G, Guerra J, Jr, Vint V, Usselman J. Spinal vacuum phenomena: anatomical study and review. Radiology. 1981;139:341–348. doi: 10.1148/radiology.139.2.7220878. [DOI] [PubMed] [Google Scholar]
- 2.Hasegawa K, Homma T, Uchiyama S, Takahashi H. Vertebral pseudarthrosis in the osteoporotic spine. Spine. 1998;23:2201–2206. doi: 10.1097/00007632-199810150-00011. [DOI] [PubMed] [Google Scholar]
- 3.Sarli M, Perez Manghi FC, Gallo R, Zanchetta JR. The vacuum cleft sign: an uncommon radiological sign. Osteoporos Int. 2005;16:1210–1214. doi: 10.1007/s00198-005-1833-4. [DOI] [PubMed] [Google Scholar]
- 4.Samuel E. Vacuum intervertebral discs. Br J Radiol. 1948;21:337–339. doi: 10.1259/0007-1285-21-247-337. [DOI] [PubMed] [Google Scholar]
- 5.Morishita K, Kasai Y, Uchida A. Clinical symptoms of patients with intervertebral vacuum phenomenon. Neurologist. 2008;14:37–39. doi: 10.1097/NRL.0b013e3180dc9992. [DOI] [PubMed] [Google Scholar]
- 6.Pate D, Katz A. Clostridia discitis: a case report. Arthritis Rheum. 1979;22:1039–1040. doi: 10.1002/art.1780220916. [DOI] [PubMed] [Google Scholar]
- 7.Beguiristain JL, Pablos J, Llombart R, Gomez A. Discitis due to Clostridium perfringens. Spine. 1986;11:170–172. doi: 10.1097/00007632-198603000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Bielecki DK, Sartoris D, Resnick D, Lom K, Fierer J, Haghighi P. Intraosseous and intradiscal gas in association with spinal infection: report of three cases. AJR Am J Roentgenol. 1986;147:83–86. doi: 10.2214/ajr.147.1.83. [DOI] [PubMed] [Google Scholar]
- 9.Bhalla S, Reinus WR. The linear intravertebral vacuum: a sign of benign vertebral collapse. AJR Am J Roentgenol. 1998;170:1563–1569. doi: 10.2214/ajr.170.6.9609175. [DOI] [PubMed] [Google Scholar]
- 10.Uetani M, Hashmi R, Hayashi K. Malignant and benign compression fractures: differentiation and diagnostic pitfalls on MRI. Clin Radiol. 2004;59:124–131. doi: 10.1016/j.crad.2003.07.005. [DOI] [PubMed] [Google Scholar]
- 11.Libicher M, Appelt A, Berger I, Baier M, Meeder PJ, Grafe I, Dafonseca K, Noldge G, Kasperk C. The intravertebral vacuum phenomenon as specific sign of osteonecrosis in vertebral compression fractures: results from a radiological and histological study. Eur Radiol. 2007;17:2248–2252. doi: 10.1007/s00330-007-0684-0. [DOI] [PubMed] [Google Scholar]
- 12.Maldague BE, Noel HM, Malghem JJ. The intravertebral vacuum cleft: a sign of ischemic vertebral collapse. Radiology. 1978;129:23–29. doi: 10.1148/129.1.23. [DOI] [PubMed] [Google Scholar]
- 13.Pappou IP, Papadopoulos EC, Swanson AN, Cammisa FP, Jr, Girardi FP. Osteoporotic vertebral fractures and collapse with intravertebral vacuum sign (Kummel’s disease) Orthopedics. 2008;31:61–66. doi: 10.3928/01477447-20080101-35. [DOI] [PubMed] [Google Scholar]
- 14.Kumpan W, Salomonowitz E, Seidl G, Wittich GR. The intravertebral vacuum phenomenon. Skeletal Radiol. 1986;15:444–447. doi: 10.1007/BF00355102. [DOI] [PubMed] [Google Scholar]
- 15.Gagnerie F, Taillan B, Euller-Ziegler L, Ziegler G. Intravertebral vacuum phenomenon in multiple myeloma. Clin Rheumatol. 1987;6:597–599. doi: 10.1007/BF02330600. [DOI] [PubMed] [Google Scholar]
- 16.Schabel SI, Moore TE, Rittenberg GM (1979) Vertebral vacuum phenomenon: a radiographic manifestation of metastatic malignancy. Skeletal Radiol 4:154–156
- 17.Lane JI, Maus TP, Wald JT, Thielen KR, Bobra S, Luetmer PH. Intravertebral clefts opacified during vertebroplasty: pathogenesis, technical implications, and prognostic significance. AJNR Am J Neuroradiol. 2002;23:1642–1646. [PMC free article] [PubMed] [Google Scholar]
- 18.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 19.Chang MC, Wu HT, Lee CH, Liu CL, Chen TH. Tuberculous spondylitis and pyogenic spondylitis: comparative magnetic resonance imaging features. Spine. 2006;31:782–788. doi: 10.1097/01.brs.0000206385.11684.d5. [DOI] [PubMed] [Google Scholar]
- 20.McDonald RJ, Trout AT, Gray LA, Dispenzieri A, Thielen KR, Kallmes DF. Vertebroplasty in multiple myeloma: outcomes in a large patient series. AJNR Am J Neuroradiol. 2008;29:642–648. doi: 10.3174/ajnr.A0918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee B, Franklin I, Lewis JS, Coombes RC, Leonard R, Gishen P, Stebbing J. The efficacy of percutaneous vertebroplasty for vertebral metastases associated with solid malignancies. Eur J Cancer. 2009;45:1597–1602. doi: 10.1016/j.ejca.2009.01.021. [DOI] [PubMed] [Google Scholar]