Abstract
Relationship between lumbar disc degeneration and segmental instability has remained controversial. Using instability factors that found close relations with symptoms in flexion–extension radiographic study, their relationship with degenerative findings was examined. More than (≥) 3 mm slip in neutral position (SN), ≥3 mm translation (ST), and ≥10° angulation (SA) at L4/5 segment were defined as instability factors and were applied on 447 patients who had low back and/or leg pain and satisfied inclusion criteria for accurate measurements. Radiologic findings for degeneration were disc height including three groups with different disc heights divided by mean ± 1 standard deviation, length of the anterior spur formation, presence of vacuum phenomenon, and endplate sclerosis. As results, group with SN factor was the oldest in age and the lowest in disc height; in contrast, group with SA was the youngest in age and the highest in disc height. The group with ST showed a mid-standing position in both age and disc height. These findings indicate that instability factors are intimately related to age and disc height. The three different disc height groups showed more anterior slip according to the progression of the disc height diminution. Presence of the apparent spur formation and/or vacuum phenomenon had an intimate relationship with the ST factor. Disc height was the most important in the examined parameters and showed an intimate relationship with age and instability factors. Although the etiology is still unknown, clinical common knowledge, that a diminution of disc height with progressive degeneration had a close relation with anterior vertebral slippage, was firstly confirmed. This study allows comprehensive understanding of segmental instability and is useful for considering surgical indications.
Keywords: Lumbar spine, Disc degeneration, Instability, Radiologic sign, MRI
Introduction
A high incidence of degenerative findings in the lumbar disc is observed when patients with low back pain (LBP) and/or sciatica are examined by MRI. Moreover, disc degenerations are largely observed in elderly patients and often does not relate to neurological signs and symptoms. These findings have led to a general belief that there are no specific signs related to LBP [1, 13, 16].
Another important factor related to LBP is instability indicating excessive motion around the disc segment. Previously several authors have studied the relationship between instability and LBP using various types of equipments [11], measurement methods [24], and clinical and experimental studies [5]. In their results, some authors reported a strong relationship [7, 22, 24], but the others did not [1, 13, 16] or weak relationship [18], showing that the definition of instability to suggest a treatment decision had not been determined. Because large numbers of lumbar fusion surgery were indicated by using X-ray, CT, and MRI examinations, thus the radiology and MRI are still important measures to judge lumbar instability [8].
MRI evaluation of disc degeneration is usually performed in a static supine condition. Previously, the current authors reported the relationship between instability and clinical symptoms by using flexion–extension radiography in standing condition [7, 8]. In this research, we investigated the controversial topic of whether spinal degeneration at the motion segment has an intimate relationship with instability. Some authors have insisted there is a close correlation between disc degeneration and instability [11, 15], while several others have disputed this [14, 21]. In this study, we examined radiologic and MRI findings around L4/5 segment of patients with LBP and/or sciatica. There is general agreement that the presence of degenerative changes in the disc itself is not a reliable sign of LBP, therefore the purpose of this study is to establish what types of segmental degeneration have a relationship with instability using a measuring method we developed.
Materials and methods
In recent 3 years, 637 outpatients with LBP and/or leg pain underwent radiologic and MRI examinations simultaneously within a 2-month interval. The radiologic examinations were performed in standing position. MRI scans were obtained using a 1.5 Tesla clinical magnet (Magnetron Vision, Siemens, Germany) with sagittal T2-weighted imaging sequence (TR: 3400 ms, TE: 120 ms, FOV: 280 mm, sliced with 5 mm). Patients were scanned in supine position with knee flexion.
In order to obtain a more precise segmental instability rating, 190 patients with conditions which might impede accurate measurement of instability were excluded from the study. The exclusion criteria were infection, tumors, trauma, previous surgery, spondylolysis, spondylolisthesis at other segments, scoliosis with ≥10°, osteoporosis with compression fracture, and unsuitable radiographs to measure. The remaining 447 patients, 268 men and 179 women, were included in this study and their age range varied from 10 to 86 years (mean ± SD: 53.0 ± 19.8).
Evaluation of instability
Sagittal segmental instability at L4/5 disc measured using three lateral radiographs at neutral, extension, and flexion position, was assessed by three variables: L4 anterior slip on L5 in neutral position (SN), sagittal translation (ST), and segmental angulation (SA) [6–8]. Measurement of each slip was performed using the method basically described by White and Panjabi [25], which has only three landmarks for the measurement: the anterior edge and the posterior edge of upper endplate of L5, and the inferior posterior edge of L4. It was considered that a less variable result could be obtained with this system compared with other methods using more than three landmarks [20]. The amount of sagittal translation was obtained as the difference of the displacement between flexion and extension. Segmental angulation was also measured as the difference of intervertebral angles from extension to flexion. Detailed measurement methods were described previously elsewhere [6–8]. Then, ≥3 mm slip in neural position (SN), ≥3 mm translation (ST), and ≥10° angulation (SA) were provisionally defined as excessive motion (instability) factors in this study.
Evaluation of degeneration
Radiologic degenerative evaluation was performed by examinations of disc height, spur formation of the anterior vertebral edges, vacuum phenomenon observed in flexion–extension films, and endplate sclerosis [14, 18]. Disc height ratio was obtained as a quotient of mean of anterior and posterior disc heights divided by inferior AP diameter of L4 vertebra to correct body size [5]. Mean disc height ratio of all patients was 0.232, and they were classified into three height groups divided by ±1 standard deviation. Disc height ≥0.291 was defined as the high disc height (HDH) group (68 patients), ≥0.173 and <0.291 was the medium disc height (MDH) group (312 patients), and <0.173 was the low disc height (LDH) group (67 patients). Bony spur formation was measured as the sum length of the upper and lower anterior spur at the segment. The presence of vacuum phenomenon and endplate sclerosis were judged as present or not present. Evaluation of the disc degeneration by MRI was performed according to a criterion proposed by Pfirrmann et al. [19]; grade 1 to 5 from normal to severe degeneration. Radiologic and MRI examinations were performed by three examiners unaware of the patient’s conditions. Difference in the measurement values of the observers was determined by discussion.
Group definition
Patients were divided into 8 groups based on their instability factors [8]. Group A, whom had all factors (SN+ST+SA), was composed of 20 patients with mean age of 72.2 years. Group B had 21 patients (SN+ST; 72.7 years); group C, only one patient (SN+SA; 66 years); group D, 17 patients (SN alone, 63.8 years); group E, 32 patients (ST+SA, 45.1 years); group F, 30 patients (ST alone, 59.7 years); group G, 46 patients (SA alone, 40.1 years); and group H, 280 patients, had none of above factors (51.4 years). The relationship of disc height, spur length, vacuum phenomenon, endplate sclerosis, and disc degeneration by MRI findings with various types of instability were examined except for the group C because there was only one patient in that group.
Statistical analysis
Statistical examination was performed using one way ANOVA (Fisher’s PLSD) and p value less than 0.05 was defined as significant.
Results
Disc height and instability factors
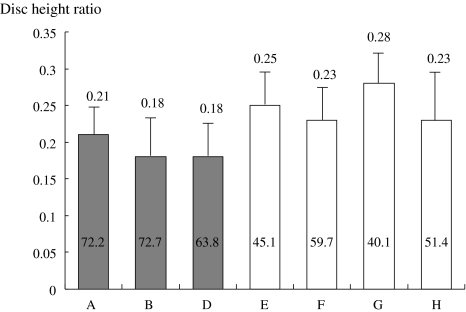
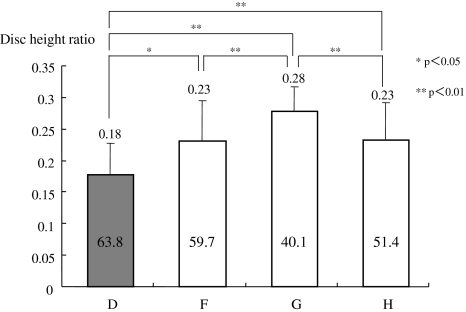
Among the groups, group G with SA factor alone was characterized by the young age (mean, 40.1 years) and the highest disc height. In contrast, groups A, B, and D with SN factors (closed bars) demonstrated higher age and lower disc height (Fig. 1). To simplify the effect of instability factors, the three groups having only one factor alone and group H, without any factors, were compared (Fig. 2). Groups D, F, and G were ordered in age, with D being the oldest, group F in the mid-range, and group G the youngest. Disc heights were also ordered from the oldest age group with the lowest height, the mid-age group with a mid range height, and the youngest age with the highest disc. These findings indicate instability factors are intimately related with age and disc height. Group H without factors was positioned in the middle of the groups both in age and in disc height comparisons (Fig. 2).
Fig. 1.
Disc height ratio of the groups with various instability factors. Group A had all 3 instability factors (SN+ST+SA; SN: ≥3 mm slip, ST: ≥3 mm translation, and SA: ≥10° angulation), Group B: SN+SA, Group D: SN alone, Group E: ST+SA, Group F: ST alone, Group G: SA alone, Group H: none of the 3 factors. The numbers in each bar indicates the mean age of the group. Closed bars showed the groups which had the SN factor
Fig. 2.
Disc height ratio of the groups with/without a typical instability factor. Groups D, F, G, and H represent the same groups as in Fig. 1. Age and disc height differences were more distinctive. The closed bar indicates the disc height ratio of the group which had SN factor alone
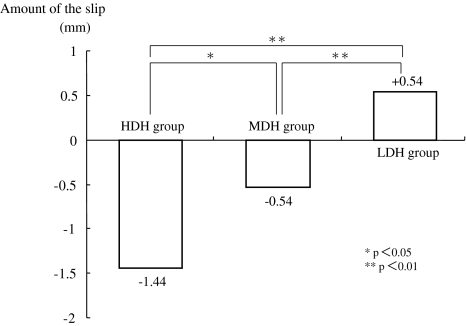
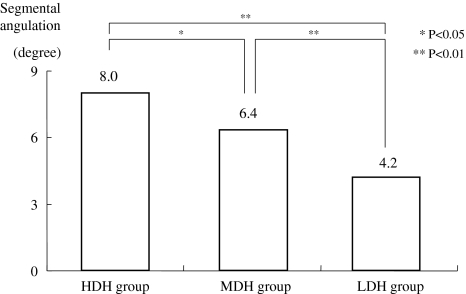
The above findings were confirmed by another study. The three disc height groups divided by ±1 SD showed that the L4 vertebra of the LDH group slipped most anteriorly among the groups, followed by the MDH and then HDH group (Fig. 3). The difference of mean slip between the HDH group and LDH group reached 2 mm, and statistically significant differences were observed between them. The degrees of segmental angulation among the groups were also statistically different, demonstrating that the HDH group had the largest angulation and the LDH group the least angulation (Fig. 4).
Fig. 3.
Amount and direction of the slip in three different disc height groups. Amount of slip was measured using the lateral radiograph in neutral standing position. Positive and negative signs indicate the relative position of the L4 landmark to the L5 landmark in the sagittal plane, therefore a positive value means anterior slip of the L4, and a negative means posterior slip. According to the decreased disc height, more anterior slip was observed. HDH high disc height, MDH medium disc height, LDH low disc height
Fig. 4.
Relationship between disc height and segmental angulation. According to the decrease in disc height, less angulation was observed. HDH high disc height, MDH medium disc height, LDH low disc height
Spur length and vacuum phenomenon
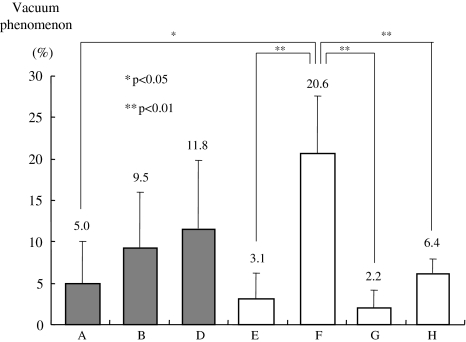
Spur length around the L4/5 segment was the longest (≥5 mm) in group F with ST alone factor and group H with no instability factors compared to the other groups with 2–3 mm length (Data not shown). The incidence of vacuum phenomenon was the highest (20.6%) in group F with ST alone, followed by group D (11.8%) with SN alone. In contrast, group G with SA alone and the group E with ST and SA factors showed low incidences of 2.2 and 3.1%, respectively (Fig. 5).
Fig. 5.
Incidence of vacuum phenomenon. Vacuum phenomenon was observed the most frequently in group F with ST factor alone, and was significantly higher than in groups G, E, A, and H. Closed bars shows the group which had SN factor
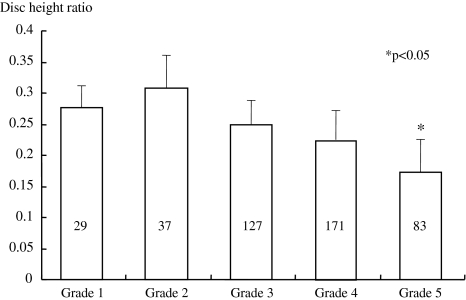
Disc height and grade of degeneration
The number of patient who had each degeneration grade on the L4/5 disc were classified as 29 cases in grade 1, 37 cases in grade 2, 127 cases in grade 3, 171 cases in grade 4, and 83 cases in grade 5 (Fig. 6). More than 85% of the patients showed grade 3 (inhomogeneous, gray) or more disc degeneration in this series. The disc height of grade 2 was the highest followed by grade 1, grade 3, grade 4, and finally grade 5. The disc height of the grade 5 group had statistically significant shortening than the other grades (Fig. 6).
Fig. 6.
Disc height and classified grades of disc degeneration. Disc height of grade 2 degeneration group was the highest and gradually decreased heights were observed in the order grade 1, 3, 4, and 5 degeneration groups. The height of grade 5 was the lowest and the difference was statistically significant compared to the others (p < 0.05). The numbers in the bar indicate the number of patients in each group
Vacuum phenomenon and endplate sclerosis
The appearance rate of vacuum phenomenon was zero in grade 1 and 2, and low in grade 3 (3.6%) and grade 4 (4.8%), however, it remarkably increased to 30.0% in the grade 5 degeneration group. Similarly, the incidence of endplate sclerosis was zero in grade 1, 3.1% in grade 2, and 11.6% in grade 4, and finally 36.2% in grade 5 degeneration showing that these vacuum phenomenon and endplate sclerosis start to appear at the middle stage of degeneration and became the most frequent in the end stage of disc degeneration (Table 1).
Table 1.
Appearance rate of vacuum phenomenon and endplate sclerosis in graded disc degeneration
| Classification of disc degenerationa | |||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |
| Number of disc | 29 | 37 | 127 | 171 | 83 |
| Vacuum phenomenon (%) | 0 | 0 | 3.6 | 4.8 | 30.0 |
| Endplate sclerosis (%) | 0 | 3.1 | 2.7 | 11.6 | 36.2 |
aPfirrmann’s criterion
Discussion
Information about disc degeneration and segmental instability in the lumbar spine is obscure. Previously, the authors reported relationships between the instability factors used in this study and the severity of symptoms using flexion–extension radiography with special attention to the minimization of variance [7, 8]. It was revealed that ≥3 mm slip had a higher influence on severity of symptoms than a factor of ≥3 mm translation, and ≥10° angulation had the least effect on symptoms, however, there was a greater effect on severity and longevity of symptoms when this factor was combined with other factors [7]. Considering that disc degeneration and LBP increase with age and are common among the elderly generation, a relationship between lumbar disc degeneration and instability is strongly suspected. The current study, therefore, represents a second stage of that study and thus evaluates the relationship between the segmental instability and degenerative findings detected by radiography and MRI.
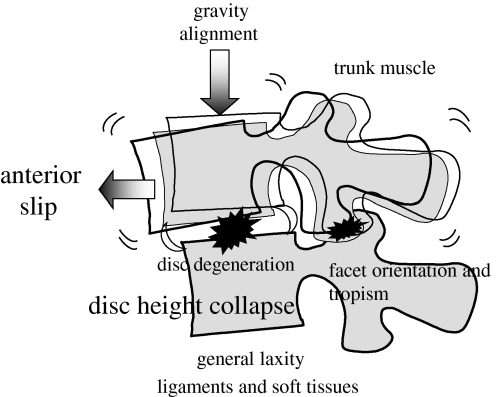
In the degenerative findings, disc height showed an apparent relationship with age and instability. A lower disc height was closely related with older age and ≥3 mm slippage. In contrast, a higher disc height was related to a younger age and larger segmental angulation. Murata et al. [15] examined lower lumbar segments in 109 patients using radiograph and MRI and pointed out that the severity of disc degeneration had a correlation with an older age, lower disc height, and less segmental angulation. However, they found no relationship between degeneration and translation, probably due to the use of different measuring methods providing more than four landmarks [2]. Increased anterior slippage, degenerative spondylolisthesis at L4/5 segment, with diminution of the disc height was frequently observed among the elderly, however, this finding was firstly confirmed and described in our study. The etiology of the anterior slippage is still not clear. In addition to degeneration of the disc and facet joint, many factors such as gravity, spinal alignment, weakness of trunk muscles, damage of ligaments and soft tissues related to genetic abnormality were reported previously (Fig. 7) [9, 12, 17]. The increased segmental motion in flexion and lateral bending position compared to extension position in a previous cadaveric experiment may explain this phenomenon [26].
Fig. 7.
Scheme showing considerable mechanism of the anterior slip with progressive disc degeneration. According to the diminishing disc height with progressive degeneration, increased anterior slip was observed. Factors such as spinal alignment, trunk muscle, ligament and soft tissues, and facet orientation and tropism, are thought to be promoting factors in addition to the degeneration of discs and facet joints
Spur formation at the motion segment often occurs at the edge of the endplate and/or facet joints. Eubanks et al. [3] found that osteophytes of the facet joint occurs in the population younger than 30 years at the upper lumbar segments, but is observed as more vertebral rim osteophytes in the lower lumbar segments at all levels except for L4/5 and L5/S1 in the population older than 40 years. The spur formation around the motion segments, therefore, may not be a good indicator of segmental instability at the lower lumbar segments. Other degenerative findings, vacuum phenomenon and endplate sclerosis, were observed in the end stage of the disc degeneration. The lower disc height with less segmental motion was thought to be stable and clinically not harmful [4, 10]. However, prominent anterior spur formation and/or vacuum phenomenon showed a close relationship to sagittal translation which was an important factor for instability [8, 23].
There are several limitations in this study. Even though less variance has been reported using this measuring method [20], selections of films were variable and the accuracy of the measurement was limited by sight. Secondly, although we attempted to enroll a large number of patients and examine them both with radiology and MRI simultaneously, after exclusion criteria were met rather small patients groups were available. Finally, this is a restricted study examining only the L4/5 segment. No further information from the neighboring segments was obtained.
In conclusion, the disc height showed an intimate relationship with age and instability, and furthermore the principal part of the instability factors changed across age decades: ≥10° angulation, ≥3 mm translation, and finally ≥3 mm slip. According to the progression of disc degeneration, disc height decreased and anterior slippage occurred. Spur formation, vacuum phenomenon, and endplate sclerosis were not the primary indicators for segmental instability, but the presence of apparent anterior spur formation and/or vacuum phenomenon should be considered as evidence of segmental instability of translation. Combination of the ≥3 mm slip and the ≥3 mm translation were closely related to severe symptoms and considered to be critical for surgical indication previously [8]. This study revealed comprehensive information about lumbar segmental instability related to LBP. Due to the aforementioned limitations, more detailed study examining all segments separately is necessary to confirm the results.
Acknowledgments
No funds were received in support of this study. The authors thank Ms. Janina Tubby for her help in preparing the manuscript.
Conflict of interest None.
References
- 1.Boos N, Semmer N, Elfering A, et al. Natural history of individuals with asymptomatic disc abnormalities in magnetic resonance imaging. Spine. 2000;25:1484–1492. doi: 10.1097/00007632-200006150-00006. [DOI] [PubMed] [Google Scholar]
- 2.Dupuis PR, Yong-Hing K, Cassidy JD, Kirkaldy-Willis WH. Radiologic diagnosis of degenerative lumbar spinal instability. Spine. 1985;10:262–276. doi: 10.1097/00007632-198504000-00015. [DOI] [PubMed] [Google Scholar]
- 3.Eubanks JD, Lee MJ, Cassinelli E, Ahn NU. Does lumbar facet arthrosis precede disc degeneration? Clin Orthop. 2007;464:184–189. doi: 10.1097/BLO.0b013e3181583d4e. [DOI] [PubMed] [Google Scholar]
- 4.Fujiwara A, Lim TH, An HS, et al. The effect of disc degeneration and facet joint osteoarthritis on the segmental flexibility of the lumbar spine. Spine. 2000;25:3036–3044. doi: 10.1097/00007632-200012010-00011. [DOI] [PubMed] [Google Scholar]
- 5.Hasegawa K, Kitahara K, Hara T, et al. Evaluation of lumbar segmental instability in degenerative diseases by using a new intraoperative measurement system. J Neurosurg Spine. 2008;8:255–262. doi: 10.3171/SPI/2008/8/3/255. [DOI] [PubMed] [Google Scholar]
- 6.Iguchi T, Kanemura A, Kasahara K, et al. Age distribution of three radiological factors for lumbar instability: probable aging process of the instability with disc degeneration. Spine. 2003;28:2628–2633. doi: 10.1097/01.BRS.0000097162.80495.66. [DOI] [PubMed] [Google Scholar]
- 7.Iguchi T, Kanemura A, Kasahara K, et al. Lumbar instability and clinical symptoms: which is the more critical factor for symptoms, sagittal translation or segmental angulation? J Spinal Disord Tech. 2004;17:284–290. doi: 10.1097/01.bsd.0000102473.95064.9d. [DOI] [PubMed] [Google Scholar]
- 8.Kanemura A, Doita M, Kasahara K, et al. The influence of sagittal instability factors on clinical lumbar spinal symptoms. J Spinal Disord Tech. 2009;22:479–485. doi: 10.1097/BSD.0b013e31818d1b18. [DOI] [PubMed] [Google Scholar]
- 9.Kim NH, Lee JW. The relationship between isthmic and degenerative spondylolisthesis and the configuration of the lamina and facet joints. Eur Spine J. 1995;4:139–144. doi: 10.1007/BF00298237. [DOI] [PubMed] [Google Scholar]
- 10.Kirkaldy-Willis WH, Farfan HF. Instability of the lumbar spine. Clin Orthop. 1982;165:110–123. [PubMed] [Google Scholar]
- 11.Kong MH, Hymanson HJ, Song KY, et al. Kinetic magnetic resonance imaging analysis of abnormal segmental motion of the functional spine unit. J Neurosurg Spine. 2009;10:357–365. doi: 10.3171/2008.12.SPINE08321. [DOI] [PubMed] [Google Scholar]
- 12.Leone A, Guglielmi G, Cassar-Pullicino VN, Bonomo L. Lumbar intervertebral instability: a review. Radiology. 2007;245:62–77. doi: 10.1148/radiol.2451051359. [DOI] [PubMed] [Google Scholar]
- 13.Luoma K, Riihimäki H, Luukkonen R, et al. Low back pain in relation to lumbar disc degeneration. Spine. 2000;25:487–492. doi: 10.1097/00007632-200002150-00016. [DOI] [PubMed] [Google Scholar]
- 14.McGregor AH, Cattermole HR, Hughes SPF (1998) Spinal motion in lumbar degenerative disc disease. J Bone Joint Surg 80-B:1009–1013 [DOI] [PubMed]
- 15.Murata M, Morio Y, Kuranobu K. Lumbar disc degeneration and segmental instability: a comparison of magnetic resonance images and plain radiographs of patients with low back pain. Arch Orthop Trauma Surg. 1994;113:297–301. doi: 10.1007/BF00426175. [DOI] [PubMed] [Google Scholar]
- 16.Ochia RS, Inoue N, Takatori R, et al. In vivo measurements of lumbar segmental motion during axial rotation in asymptomatic and chronic low back pain male subjects. Spine. 2007;32:1394–1399. doi: 10.1097/BRS.0b013e318060122b. [DOI] [PubMed] [Google Scholar]
- 17.Oishi Y, Murase M, Hayashi Y, et al. Smaller facet effusion in association with restabilization at the time of operation in Japanese patients with lumbar degenerative spondylolisthesis. J Neurosurg Spine. 2010;12:88–95. doi: 10.3171/2009.7.SPINE08908. [DOI] [PubMed] [Google Scholar]
- 18.Peterson CK, Bolton JE, Wood AR. A cross-sectional study correlating lumbar spine degeneration with disability and pain. Spine. 2000;25:218–223. doi: 10.1097/00007632-200001150-00013. [DOI] [PubMed] [Google Scholar]
- 19.Pfirrmann CWA, Metzdorf A, Zanetti M, et al. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine. 2001;26:1873–1878. doi: 10.1097/00007632-200109010-00011. [DOI] [PubMed] [Google Scholar]
- 20.Shaffer WO, Spratt KF, Weinstein J, et al. The consistency and accuracy of roentgenograms for measuring sagittal translation in the lumbar vertebral motion segment: an experimental model. Spine. 1990;15:741–750. [PubMed] [Google Scholar]
- 21.Soini J, Antti-Poika I, Tallroth K, et al. Disc degeneration and angular movement of the lumbar spine: comparative study using plain and flexion-extension radiography and discography. J Spinal Disord Tec. 1991;4:183–187. doi: 10.1097/00002517-199106000-00008. [DOI] [PubMed] [Google Scholar]
- 22.Torgerson WR, Dotter WE (1976) Comparative roentgenographic study of the asymptomatic and symptomatic lumbar spine. J Bone Joint Surg 58-A: 850–853 [PubMed]
- 23.Vernon-Roberts B, Moore RJ, Fraser RD. The natural history of age-related disc degeneration. Spine. 2007;32:2797–2804. doi: 10.1097/BRS.0b013e31815b64d2. [DOI] [PubMed] [Google Scholar]
- 24.Weiler PJ, King GJ, Gertzbein SD. Analysis of sagittal plane instability of the lumbar spine in vivo. Spine. 1990;15:1300–1306. doi: 10.1097/00007632-199012000-00012. [DOI] [PubMed] [Google Scholar]
- 25.White AA, III, Panjabi MM. Clinical biomechanics of the spine. 2. Philadelphia: Lippincott; 1990. [Google Scholar]
- 26.Zhao F, Pollintine P, Hole BD, et al. Discogenic origins of spinal instability. Spine. 2005;30:2621–2630. doi: 10.1097/01.brs.0000188203.71182.c0. [DOI] [PubMed] [Google Scholar]