Abstract
In the elderly population, reported union rates with anterior odontoid screw fixation (AOSF) for odontoid fracture (OF) treatment vary between 23 and 93% when using plain radiographs. However, recent research revealed poor interobserver reliability for fusion assessment using plain radiographs compared to CT scans. Therefore, union rates in patients aged ≥60 years treated with AOSF have to be revisited using CT scans and factors for non-union to be analysed. Prospectively gathered consecutively treated patients using AOSF for odontoid fracture with age ≥60 years were reviewed. Medical charts were assessed for demographics, clinical outcomes and complications. Patients’ preoperative radiographs and CT scans were analysed to characterize fracture morphology and type, fracture displacement, presence of atlanto-dental osteoarthritis as well as a detailed morphometric assessment of fracture surfaces (in mm2). CT scans performed after a minimum of 3 months postoperatively were analysed for fracture union. Those patients not showing CT-based evidence of completely fused odontoid fracture were invited for radiographic follow-up at a minimum of 6 months follow-up. Follow-up CT-scan were studied for odontoid union as well as the number of screws used and the square surface of screws used for AOSF and the related corticocancellous osseous healing surface of the odontoid fragment (in %) were calculated. Patients were stratified whether they achieved osseous union or fibrous non-union. Patients with a non-union were subjected to flexion–extension lateral radiographs and the non-union defined as stable if no motion was detected. The sample included 13 male (72%) and 5 female (18%) patients. The interval from injury to AOSF was 4.1 ± 5.3 days (0–16 days). Age at injury was 78.1 ± 7.6 years (60–87 years) and follow-up was 75.7 ± 50.8 months (4.2–150.2 months). 10 patients had dislocated fractures, 14 had Type II and 4 “shallow” Type III fractures according to the Anderson classification, 2 had stable C1-ring fractures, 8 had displayed atlanto-dental osteoarthritis. Fracture square surface was 127.1 ± 50.9 mm2 (56.3–215.9 mm2) and osseous healing surface was 84.0 ± 6.8% (67.6–91.1%). CT-based analysis revealed osseous union in 9 (50%) and non-union in 9 patients (50%). Union rates correlated with increased fracture surface (P = 0.02). Statistical analysis revealed a trend that the usage of two screws with AOSF correlates with increased fusion rates (P = 0.06). Stability at C1–2 was achieved in 89% of patients. CT scans are accepted as the standard of reference to assess osseous union. The current study offers an objective insight into the union rates of odontoid fractures treated with AOSF using CT scans in consecutive series of 18 patients ≥60 years. Literature serves evidence that elderly patients with unstable OF benefit from early surgical stabilization. However, although using AOSF for unstable OF yields segmental stability at C1–2 in a high number of patients as echoed in the current study, our analysis stressed that using follow-up CT scans in comparison to biplanar radiographs dramatically reduces osseous union rates compared to those previously reported for AOSF.
Keywords: Odontoid fracture, Elderly patient, Anterior odontoid screw fixation, CT scan, Osseous fusion
Introduction
Odontoid fractures (OF) are the most common cervical spine fracture in patients aged older than 70 years and even the most common spinal fracture of patients aged older than 80 years [1–5]. Treatment of OF yields for stable osseous fusion to avoid the risk of late neurologic deterioration due to instability at C1–C2.
Previous studies served evidence for increased risk of pseudoarthrosis with OF treatment in the elderly [6–11] correlating with the different techniques available and their related morbidity [12]. Accordingly, the decision making process regarding the ideal method remains challenging.
Anterior odontoid screw fixation (AOSF) has been proven to be a valuable method in the elderly population. First described by Bohler [13], several studies also reported on technical details, surgical outcomes and complications [2, 6, 14–25]. AOSF allows osteosynthesis of reduced OF through a non-traumatic standardized surgical approach if compared to the posterior approach [26] and can preserve atlantoaxial motion. Contraindications such as remote or compound fractures have to be respected for successful surgery [6, 27]. Using AOSF, overall fusion rates were reported with up to 84–96% [14–25] and 23–93% in the elderly population [6–11, 28, 29]. The impact of patients’ age at index surgery on outcome was discussed controversially. While it was shown to have significant impact on union rates in several studies [6–10, 30], other authors did not find a significant correlation between age and union rates [15, 18, 20, 31]. Besides age, the number of screws used for AOSF might have significant impact on union rates, too. However, while biomechanical studies supported the use of AOSF using single screws only based on axial torque stiffness measurements [22, 32, 33] and most clinical studies so far have shown no significant advantage by placing two screws [18, 20, 34], a recent clinical study indicated that usage of two screws in the elderly patient might be beneficial [28].
Notably, assessment of union in previous outcome studies on AOSF in the elderly [6–11, 28] was based on radiographs only, while a recently published study demonstrated that reliability of OF union assessment is moderate using radiographs only if compared to CT scans as the standard of reference [35].
Because osseous union is an important outcome anchor in benchmark studies concerning the ideal treatment of OF in the elderly, aim of this study was to evaluate the union rate of odontoid fractures treated with AOSF in patients aged ≥60 years using CT scans for fusion assessment and the identification of biometrical and technical risk factors for non-union.
Methods
The institutional database of prospectively gathered patients treated for cervical spine injuries was reviewed. Patients treated with AOSF for OF were included into the study if they fulfilled the following criteria: age 60 years or greater at time of index surgery, preoperative biplanar radiographs and reformatted CT scans, CT scans available as digital DICOM data sets, AOSF performed within 10 days after trauma, patients with or without a stable non-displaced C1-ring fracture without transverse ligament incompetence, no evidence of subaxial spinal injury, no second or third grade skull and brain injury, no history of failed non-surgical OF treatment, and patients that had complete radiographic follow-up which was defined as having a follow-up CT scan at least 3 months after the index surgery showing a solid fusion of the OF or a CT scan of at least 6 months postoperatively showing a non-union on CT-scans. In the presence of a non-union with CT scans, flexion–extension films had to be performed for stability assessment of the non-union.
The database analysis revealed 32 patients older than 60 years of age who were treated with AOSF for OF. During the follow-up period, 10 patients died due to reasons not related to the OF and index treatment. 13 patients had complete clinical and radiographic follow-up. 5 patients were invited to complete radiographic follow-up in terms of CT scanning. Four patients who lived abroad could not be tracked successfully and invited for follow-up. Hence, 18 patients had complete radiographic follow-up, full-filled eligibility criteria and were included in the final analysis.
Patients’ charts were reviewed for demographics, injury characteristics, number and diameter of screws used at index surgery and any perioperative complication or revision surgery. We documented the time period a semi-rigid cervical collar was applied postoperatively.
Radiographic assessment using biplanar radiographs and reformatted injury CT scans before index surgery were analysed for fracture displacement greater than 2 mm, presence and classification of associated C1-ring injury and classification of the fracture type according to Anderson and D’ Alonzo [36]. Furthermore, CT scans were analysed regarding atlanto-dental osteoarthritis which was defined as narrowed atlanto-dental joint space with osteophytosis [37].
In the current study, the biometrical characteristics of odontoid fractures at the time of injury were analysed for the first time. For that purpose, injury CT scans were revised and three parameters evaluated:
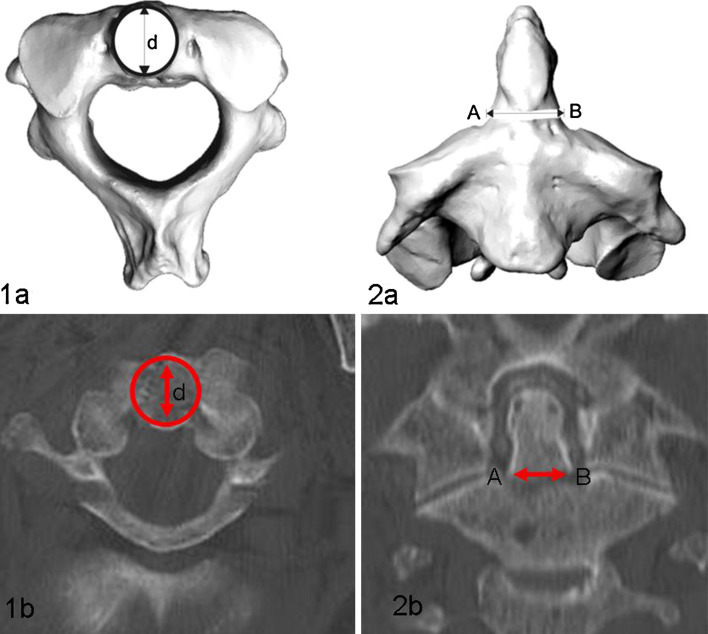
Square fracture surface (in mm2): Axial images of the preoperative CT scans were analysed for the diameter of the proximal fragment and the square fracture surface (Fig. 1, 1a, 1b) was calculated using the following formula: A = r 2 π.
Fracture length (in mm): Horizontal fracture surface was measured on coronary plane of CT scans at its widest expansion from point A to B (Fig. 1, 2a, 2b).
Osseous healing surface (in %): The ratio between the square surface of the fracture (a) and the square surface of screws used (A = π/4 × screw diameter d) was calculated and expressed as a percentage.
Fig. 1.
Description of measurement reference points: Square fracture surface (1a, 1b) was calculated at the base of fracture on an axial CT-slice with the formula A = r 2 π. Horizontal fracture surface was measured on coronary CT scans at its widest expansion from point A to B (2a, 2b)
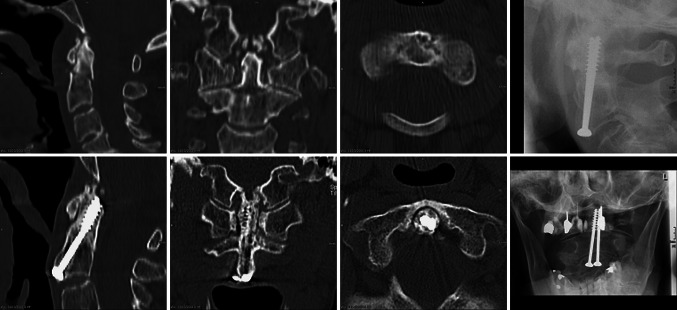
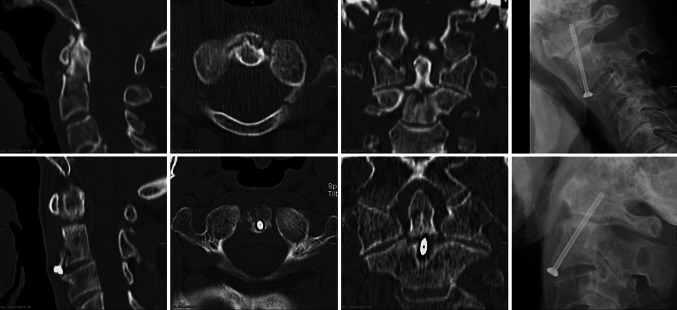
On follow-up CT scans we defined odontoid union and non-union. Osseous union was defined with bone- and trabecular bridging on at least three CT slides in the coronary and sagittal planes (Fig. 2). In the absence of osseous healing and solid fusion, the overall segmental stability at C1–C2 was assessed through flexion–extensions films with angulations greater than 4° [12] delineating an unstable non-union (Figs. 2, 3).
Fig. 2.
Illustrative case 1, union: 87-year-old female patient after fall from stairs, non-displaced OF treated with anterior double-screw fixation. CT scan at 12 months follow-up revealed osseous union
Fig. 3.
Illustrative case 2, non-union. 78-year-old male patient after a motor vehicle accident, displaced OF treated with single anterior screw fixation. CT scan at 14 months follow-up displayed odontoid non-union
Reformatted follow-up CT scans were assessed for technical failures, e.g., threads of lag screws within the fracture trace, incomplete reduction, lack of fracture gap compression, and others, as well as the presence of osseous odontoid union and the number of screws used.
All radiographs were taken on a digital X-ray system (Vertix 3D-III unit, Siemens, Germany) and radiographs were stored digitally (PACS Magic View VC 42, Rel A, Siemens, Germany). All cervical spine CT scans were performed on a four-row helical CT scanner (SOMATOM Volume Zoom, Germany) using a 14–18 cm field of view with 4 × 1 mm collimation and overlapping axial slice thickness of 1 mm.
With regards to the surgical technique, all AOSF were performed using an anterior retropharyngeal approach, fluoroscopy controlled drilling and placement of one or two 3.5 or 4.0 mm diameter lag screws according to the surgeons discretion. Further details of the technique used were published elsewhere [13].
Statistical analysis included descriptive statistics such as mean values, standard deviations, correlations and cross-tabulation tables as well as independent two-sided Student’s t test and tests for Pearson’s correlation coefficient. A P value less than 5% was considered to indicate a statistically significant effect. All analyses were done using Statistica 6.1 (StatSoft, Tulsa) and SPSS 11.0 (SPSS Inc, Chicago).
Results
18 patients with complete sets of preoperative and follow-up CT scans were included in the study. The sample comprised 13 male (72.2%) and 5 female (17.8%) patients with a mean age of 78.1 ± 7.6 years (60–87 years) at injury. Mean radiological follow-up with CT scans as outcome anchor was 75.7 ± 50.8 months (6.2–150.2 months). The interval from injury to AOSF was 4.1 ± 5.3 days (0–10 days). 10 patients (55.6%) revealed a fracture dislocation greater than 2 mm. According to the Anderson classification, 14 (77.8%) patients had Type II and 4 (22.2%) had high Type III fractures (“shallow” Type III). In 2 cases an associated stable C1-ring fracture was found and 8 patients (44.4%) displayed atlanto-dental osteoarthritis.
We identified 4 cases (22.2%) with evidence of a technical failure. In all of these cases, the threads of lag screws were within the fracture trace. These patients had a non-union. Average duration of external orthosis application was 6.3 weeks (4–10 weeks). 15 patients (83.3%) were treated with a double-screw fixation, while in 3 cases (16.7%) 1 screw was used.
The square surface of fractures at time of injury averaged 127.1 ± 50.9 mm2 (56.3–215.9 mm2) and, if put into perspective of diameter of screws inserted, the osseous healing surface averaged 84.0 ± 6.8% (67.6–91.1%). Mean fracture length in the coronary plane was 12.25 mm, ranging from 7.9 to 17.62 mm.
Analysis of follow-up CT scans revealed solid osseous union in 50% (n = 9) while the remaining 50% (n = 9) had a non-union. 2 (11%) showed symptomatic, unstable odontoid non-union indicating instrumented posterior fusion of C1–C2, while in 7 cases (39%) no signs of fracture instability in flexion–extension films were detected and, thus indicated stable fibrous union without radiographic signs of osseous union.
Osseous healing was observed in all 4 Type III fractures (100%), osseous union rate among patients with Type II fractures was 36.6% (n = 5). Overall, segmental stability at the fracture site and at C1–2 either through osseous fusion or through fibrous union was achieved in 89% (n = 16)
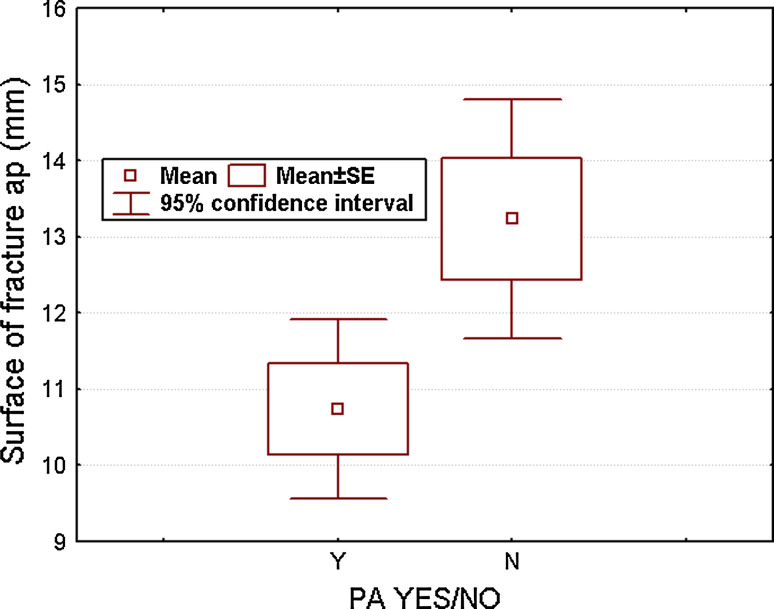
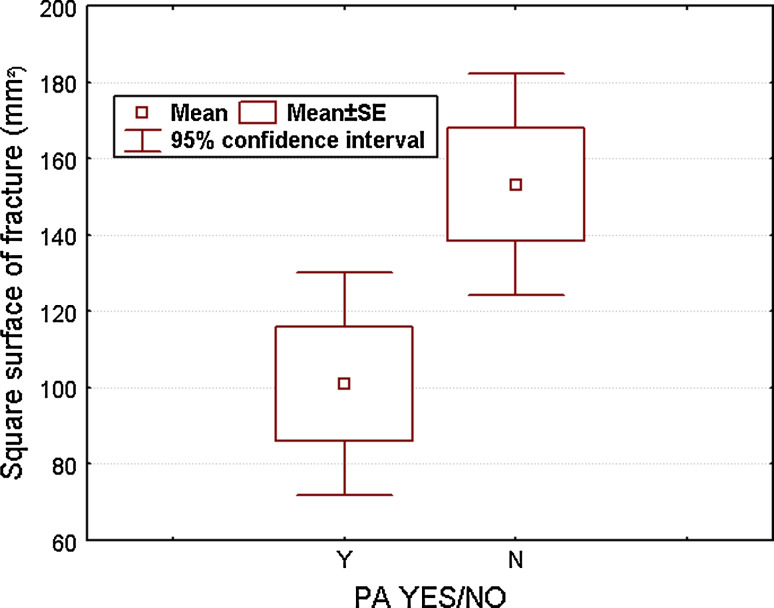
Statistical analysis showed that the union rate significantly correlated with increased square fracture surface (in mm2) as with fracture length (in mm). Patients with osseous union had a square fracture surface of 153.2 mm2 (107.9–215.9 mm2) and a mean fracture length of 13.2 mm (10.25–17.62 mm) while those with non-union averaged 100.9 mm2 (56.3–196.4 mm2) and 11.1 mm (7.9–13.94 mm), respectively. The difference yielded significance for both measurements (P = 0.02; Figs. 4, 5).
Fig. 4.
In patients with osseous union we found a mean horizontal fracture length in the ap-view of 13.2 mm (10.25–17.62 mm) while those with non-union averaged 11.1 mm (7.9–13.94 mm), the difference was significant at P = 0.02
Fig. 5.
Patients with osseous union had a square fracture surface of 153.2 mm2 (107.9–215.9 mm2), those with non-union averaged 100.9 mm2 (56.3–196.4 mm2), P = 0.02
The square surface of screws with double AOSF compared to single AOSF was significantly greater (P > 0.0001). Evaluated osseous healing surface, calculated as the ratio between screw diameter and square fracture surface, had no statistically significant impact on union rate. Although usage of two screws reduced the osseous healing surface, trend was towards increased union rates with usage of two screws, although analysis failed to yield statistical significance (P = 0.06). No patient treated with single AOSF (n = 3) showed CT scan-verified osseous union.
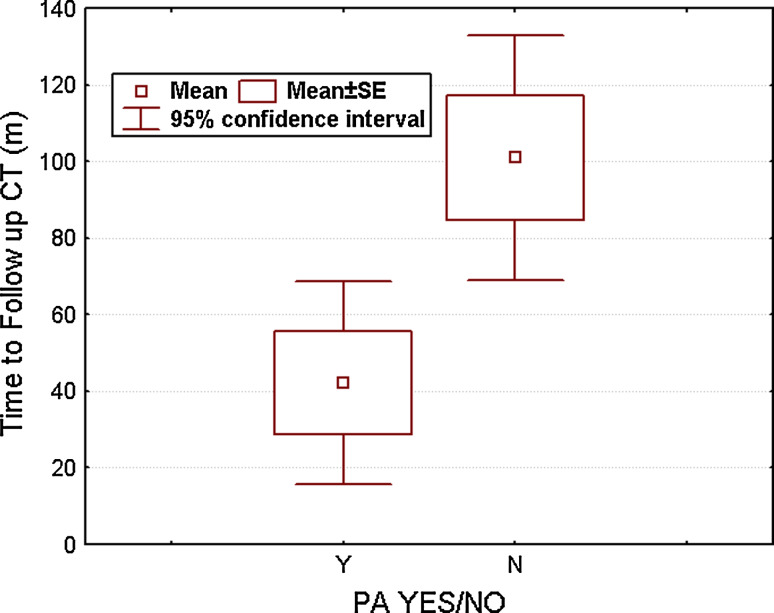
In addition, patients with longer interval from injury to postoperative CT scans were found more likely to succeed to osseous union. Patients with osseous union had mean of 101 months (ranging from 12 to 150.2 months) interval, while those with non-union had 42.4 months interval (ranging from 6 to 136 months; P = 0.01, see also Fig. 6).
Fig. 6.
Statistical analysis of differences in fusion rates regarding the interval from trauma to follow-up CT scan yielded significance at a P = 0.01
Statistically, the development of osseous union was not influenced by age or sex of the patient, the interval from injury to index treatment, the presence of fracture dislocation ≥2 mm or concomitant C1 fracture, the presence of atlanto-dental osteoarthritis, or by the amount of osseous healing surface, the diameter of screws used (3.5 or 4.0 mm) and presence of a technical failure.
Analysis of perioperative complications identified one patient (5.5%) that had a gastrointestinal haemorrhage after intubation and subsequent gastric tube application. No patient in the current series suffered from neurovascular injury (Table 1).
Table 1.
Results after AOSF in elderly patients
| Osseous fusion | Non-union | LoS | |
|---|---|---|---|
| Fracture type (n = 18) | n.s. | ||
| Type II | 5 | 9 | |
| Type III | 4 | 0 | |
| No. of screws (n = 18) | P = 0.06 | ||
| Single | 0 | 3 | |
| Dual | 9 | 6 | |
| Fracture surface (mm, coronary) | 13.2 (10.25–17.62) | 11.1 (7.9–13.94) | P = 0.02 |
| Fracture surface (mm2, axial) | 153.2 (107.9–215.9) | 100.9 (56.3–196.4) | P = 0.02 |
| Time to FU-CT (months) | 101 (12–150.2) | 42.4 (6–136) | P = 0.01 |
| Osseous healing surface (%) | 86.5 (82.2–91.1%) | 81.4 (67.6–90.7%) | n.s. |
| ADOA (n = 18) | n.s. | ||
| Yes | 1 | 5 | |
| No | 8 | 4 | |
| Technical failure | n.s. | ||
| Yes | 0 | 4 | |
| No | 9 | 5 | |
| Dislocation >2 mm | n.s. | ||
| Yes | 6 | 4 | |
| No | 5 | 3 |
LoS level of significance, ADOA atlantodental osteoarthritis, n.s. not significant
Discussion
Treatment options for OF include external orthosis fixation or surgical stabilization. Regardless of the increasing prevalence of OF among senior patients, the ideal treatment remains controversial. Since several authors reported on a morbidity and mortality of geriatric patients following external cervicothoracic immobilization of OF equalling that of surgical treatment [38–40], we also prefer surgical treatment of unstable and/or dislocated Type II and III OF for the purpose of faster recuperation and better clinical results. In the light of significant non-union rates of up to 93% [2, 4, 7, 10, 11, 41–51] and a fourfold higher risk to suffer from pulmonary or cardiac complications for an elderly patient immobilized in a Halo Thoracic Vest (HTV) for OF treatment [39], a semi-rigid cervical collar is recommended as non-surgical treatment of stable and non-displaced OF or if surgical treatment is not contrivable due to the general state of health. Recently, usage of the semi-rigid cervical collar was shown to confer a comparable capacity in limiting motion at C1–2 if compared to the HTV [12].
In view of distinct surgical and medical aspects, literature serves sufficient evidence that surgical treatment of displaced OF is beneficial [3, 39, 40, 45, 52, 53]. The current rigid techniques for the treatment of OF include an instrumented posterior fusion of C1–2 or AOSF. While posterior fusion was so far considered to have higher rates of osseous union of C1–2 in elderly patients of up to 100% [54], rather discouraging outcome reports after AOSF among elderly patients with non-union rates of as much as 77% [10] were published. Reason for high non-union rates is thought to be, e.g., a consequence of extensive posterior dislocation in Type II fractures (here 88% [10]) [7–9, 11, 41–43, 55]. Julien et al. [14] reviewed a mean overall union rate of 85.5% with posterior instrumented fusion of C1–2, while the fusion rates after AOSF were reported with 95, 90% for Type II and 100% for Type III. The results were echoed in several other studies with fusion rates ranging 84–96% [14–25].
In the current study, we obtained an osseous union rate of 50% while fractures succeeded to a stable union either through osseous fusion or through fibrous union in 89% of cases.
The meaningful variety of reported union rates following treatment of OF in the literature and compared to our study result from our follow-up protocol. Previous studies used dynamic and/or biplanar radiographs as outcome anchor only.
Osseous union in the current study was confirmed using CT scans as an outcome tool and only 50% of patients showed solid union; therefore, lower than in most preceding series. However, we found stability of the fracture site through either osseous or stable fibrous union in 89% of cases. This number is comparable to other studies where distinction between osseous union and stable fibrous union was limited by the use of radiographs only at follow up [35].
Unquestioned remains the loss of 50% of normal C1–2 rotatory motion and 10% of flexion–extension capacity associated with posterior fusion as compared to AOSF although normal axial rotation is not gained after AOSF [56, 57]. Posterior cervical fusion is furthermore associated with increased approach-related morbidity than AOSF [26]. Platzer et al. [54] found even significant better functional outcome after AOSF with excellent-to-good results compared to patients after posterior fusion with an average outcome of good-to-fair results in the Smiley-Webster scale and clearly better clinical results regarding daily life activities and pain after AOSF.
Rates of major perioperative complications after AOSF in the recent literature ranged from 1 to 9% [15–18, 20, 28, 58, 59] which is comparable with our rate of 5.5%.
In light of the existing literature without clear evidence for a preferable technique [18, 22, 25, 28, 34, 43, 60–62], the decision regarding the number of screws in our cohort was taken by the surgeon depending on individual preference. Bohler [13] advocated a two screw fixation, thus theoretically increasing rotational stability and construct strength. While this opinion was supported by several authors [4, 13, 19, 60, 63], in the cadaveric model [33] this effect of increased stability through a dual screw system was not confirmed. However, this study did not address the BMD of the specimen and thus, the relevance of this study for elderly patients with poor bone quality remains questionable. Dailey et al. [28] recently found significantly increased union rates in elderly patients using a two-screw construct and also our results, though not significant (P = 0.06) indicated similar. A remarkable finding of our study was a significant higher union rate through an increased fracture footprint, explainable through the endostal healing process of the odontoid, and explaining higher healing rates of Type III OF. Considering this, it was surprising that diminishing the osseous healing surface significantly using two instead of one screw did not lead to lower union rates in patients treated with a two-screw construct. This finding might be explainable through the observed prolonged osseous healing process of the OF in the elderly patient [28], with a second screw adding rotational stability in the osteoporotic bone until fusion matures, thus increasing the overall chance of fusion. Finally, our study with CT scans at follow-up stressed that technical details during AOSF can have an impact non-union rate. Meticulous care has to be taken with screw threads engaging only the distant odontoid fragment.
Limitations
Sample number of this present study was limited to 18 patients with OF. Further prospective comparative studies assessing the outcome following AOSF in the light of the presented results with larger sample number and specific questions regarding the outcome especially among older patients are required to confirm these findings. The results and data are reported in detail and suitable for data pooling for meta-analysis research. However, CT-based comparison will be decisive for future study on OF.
Conclusion
This is the first CT-based biometrical analysis of odontoid fracture characteristics. In contrast to previous studies dealing with this clinically relevant topic [1, 6, 9, 10, 15, 31, 64], all patients included in this study were subject to not only pre- but also postoperative CT-scans, providing valuable data regarding fracture properties and factors influencing osseous union rates. Our findings confirmed that AOSF in the recent reducible OF represents a safe alternative to posterior fusion in the appropriately selected elderly patient and fracture.
Even though osseous healing is supposed to happen within the first 6 months after surgical stabilization, we showed that through prolonged follow-up osseous fusion rates significantly increased over time, indicating prolonged healing process in the elderly patient due to poor bone quality. In the absence of pathologic motion pattern in dynamic radiographs, we therefore recommend prolonged follow-up without the need of intervention since this process usually reflects a stable fibrous union with potential for secondary osseous healing.
Though not statistically significant, we observed increased fusion rates by the use of two screws which might add stability especially in the setting of poor bone quality with prolonged healing process. We therefore recommend the use of a double-screw construct whenever technically possible especially since no adverse factors negatively influencing osseous healing were observed.
Although using AOSF for unstable OF yields stability at the C1–2 junction in a high number of patients, our study stressed that using follow-up CT scans dramatically reduces radiological osseous union rates after AOSF compared to previous, rather enthusiastic, reports on AOSF. For comparative analysis, e.g. posterior fusion versus AOSF, the current study emphasizes the need for follow-up CT scans in future studies using fusion status as endpoint anchor in outcome analysis of OF.
This study has been approved by the Institutional Review Board and all human subjects gave informed consent to participate in the study.
Acknowledgments
No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Conflict of interest
None.
References
- 1.Bednar DA, Parikh J, Hummel J. Management of type II odontoid process fractures in geriatric patients; a prospective study of sequential cohorts with attention to survivorship. J Spinal Disord. 1995;8(2):166–169. doi: 10.1097/00002517-199504000-00013. [DOI] [PubMed] [Google Scholar]
- 2.Maak TG, Grauer JN. The contemporary treatment of odontoid injuries. Spine (Phila Pa 1976) 2006;31(11 Suppl):S53–S60. doi: 10.1097/01.brs.0000217941.55817.52. [DOI] [PubMed] [Google Scholar]
- 3.Muller EJ, Wick M, Russe O, Muhr G. Management of odontoid fractures in the elderly. Eur Spine J. 1999;8(5):360–365. doi: 10.1007/s005860050188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pepin JW, Bourne RB, Hawkins RJ. Odontoid fractures, with special reference to the elderly patient. Clin Orthop Relat Res. 1985;193:178–183. [PubMed] [Google Scholar]
- 5.Ryan MD, Henderson JJ. The epidemiology of fractures and fracture-dislocations of the cervical spine. Injury. 1992;23(1):38–40. doi: 10.1016/0020-1383(92)90123-A. [DOI] [PubMed] [Google Scholar]
- 6.Platzer P, Thalhammer G, Ostermann R, et al. Anterior screw fixation of odontoid fractures comparing younger and elderly patients. Spine (Phila Pa 1976) 2007;32(16):1714–1720. doi: 10.1097/BRS.0b013e3180dc9758. [DOI] [PubMed] [Google Scholar]
- 7.Dunn ME, Seljeskog EL. Experience in the management of odontoid process injuries: an analysis of 128 cases. Neurosurgery. 1986;18(3):306–310. doi: 10.1227/00006123-198603000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Ekong CE, Schwartz ML, Tator CH, Rowed DW, Edmonds VE. Odontoid fracture: management with early mobilization using the halo device. Neurosurgery. 1981;9(6):631–637. doi: 10.1227/00006123-198112000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Hanigan WC, Powell FC, Elwood PW, Henderson JP. Odontoid fractures in elderly patients. J Neurosurg. 1993;78(1):32–35. doi: 10.3171/jns.1993.78.1.0032. [DOI] [PubMed] [Google Scholar]
- 10.Ryan MD, Taylor TK. Odontoid fractures in the elderly. J Spinal Disord. 1993;6(5):397–401. doi: 10.1097/00002517-199306050-00005. [DOI] [PubMed] [Google Scholar]
- 11.Schatzker J, Rorabeck CH, Waddell JP. Fractures of the dens (odontoid process). An analysis of thirty-seven cases. J Bone Joint Surg Br. 1971;53(3):392–405. [PubMed] [Google Scholar]
- 12.Koller H, Zenner J, Hitzl W, et al. In vivo analysis of atlantoaxial motion in individuals immobilized with the halo thoracic vest or Philadelphia collar. Spine (Phila Pa 1976) 2009;34(7):670–679. doi: 10.1097/BRS.0b013e31819c40f5. [DOI] [PubMed] [Google Scholar]
- 13.Bohler J. Anterior stabilization for acute fractures and non-unions of the dens. J Bone Joint Surg Am. 1982;64(1):18–27. [PubMed] [Google Scholar]
- 14.Julien TD, Frankel B, Traynelis VC, Ryken TC. Evidence-based analysis of odontoid fracture management. Neurosurg Focus. 2000;8(6):e1. doi: 10.3171/foc.2000.8.6.2. [DOI] [PubMed] [Google Scholar]
- 15.Berlemann U, Schwarzenbach O. Dens fractures in the elderly. Results of anterior screw fixation in 19 elderly patients. Acta Orthop Scand. 1997;68(4):319–324. doi: 10.3109/17453679708996169. [DOI] [PubMed] [Google Scholar]
- 16.Etter C, Coscia M, Jaberg H, Aebi M. Direct anterior fixation of dens fractures with a cannulated screw system. Spine (Phila Pa 1976) 1991;16(3 Suppl):S25–S32. doi: 10.1097/00007632-199103001-00006. [DOI] [PubMed] [Google Scholar]
- 17.Marchesi DG. Management of odontoid fractures. Orthopedics. 1997;20(10):911–916. doi: 10.3928/0147-7447-19971001-06. [DOI] [PubMed] [Google Scholar]
- 18.Fountas KN, Kapsalaki EZ, Karampelas I, et al. Results of long-term follow-up in patients undergoing anterior screw fixation for type II and rostral type III odontoid fractures. Spine (Phila Pa 1976) 2005;30(6):661–669. doi: 10.1097/01.brs.0000155415.89974.d3. [DOI] [PubMed] [Google Scholar]
- 19.Aebi M, Etter C, Coscia M. Fractures of the odontoid process. Treatment with anterior screw fixation. Spine (Phila Pa 1976) 1989;14(10):1065–1070. doi: 10.1097/00007632-198910000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Apfelbaum RI, Lonser RR, Veres R, Casey A. Direct anterior screw fixation for recent and remote odontoid fractures. J Neurosurg. 2000;93(2 Suppl):227–236. doi: 10.3171/spi.2000.93.2.0227. [DOI] [PubMed] [Google Scholar]
- 21.Borne GM, Bedou GL, Pinaudeau M, Cristino G, Hussein A. Odontoid process fracture osteosynthesis with a direct screw fixation technique in nine consecutive cases. J Neurosurg. 1988;68(2):223–226. doi: 10.3171/jns.1988.68.2.0223. [DOI] [PubMed] [Google Scholar]
- 22.Chang KW, Liu YW, Cheng PG, et al. One Herbert double-threaded compression screw fixation of displaced type II odontoid fractures. J Spinal Disord. 1994;7(1):62–69. doi: 10.1097/00002517-199407010-00009. [DOI] [PubMed] [Google Scholar]
- 23.Henry AD, Bohly J, Grosse A. Fixation of odontoid fractures by an anterior screw. J Bone Joint Surg Br. 1999;81(3):472–477. doi: 10.1302/0301-620X.81B3.9109. [DOI] [PubMed] [Google Scholar]
- 24.Montesano PX, Anderson PA, Schlehr F, Thalgott JS, Lowrey G. Odontoid fractures treated by anterior odontoid screw fixation. Spine (Phila Pa 1976) 1991;16(3 Suppl):S33–S37. doi: 10.1097/00007632-199103001-00007. [DOI] [PubMed] [Google Scholar]
- 25.Subach BR, Morone MA, Haid RW, Jr, et al. Management of acute odontoid fractures with single-screw anterior fixation. Neurosurgery. 1999;45(4):812–819. doi: 10.1097/00006123-199910000-00015. [DOI] [PubMed] [Google Scholar]
- 26.Shamji MF, Cook C, Pietrobon R, et al. Impact of surgical approach on complications and resource utilization of cervical spine fusion: a nationwide perspective to the surgical treatment of diffuse cervical spondylosis. Spine J. 2009;9(1):31–38. doi: 10.1016/j.spinee.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 27.Grauer JN, Vaccaro AR, Beiner JM, et al. Similarities and differences in the treatment of spine trauma between surgical specialties and location of practice. Spine (Phila Pa 1976) 2004;29(6):685–696. doi: 10.1097/01.BRS.0000115137.11276.0E. [DOI] [PubMed] [Google Scholar]
- 28.Dailey AT, Hart D, Finn MA, Schmidt MH, Apfelbaum RI. Anterior fixation of odontoid fractures in an elderly population. J Neurosurg Spine. 2010;12(1):1–8. doi: 10.3171/2009.7.SPINE08589. [DOI] [PubMed] [Google Scholar]
- 29.Harrop JS, Przybylski GJ, Vaccaro AR, Yalamanchili K. Efficacy of anterior odontoid screw fixation in elderly patients with Type II odontoid fractures. Neurosurg Focus. 2000;8(6):e6. [PubMed] [Google Scholar]
- 30.Andersson S, Rodrigues M, Olerud C. Odontoid fractures: high complication rate associated with anterior screw fixation in the elderly. Eur Spine J. 2000;9(1):56–59. doi: 10.1007/s005860050009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Borm W, Kast E, Richter HP, Mohr K. Anterior screw fixation in type II odontoid fractures: is there a difference in outcome between age groups? Neurosurgery. 2003;52(5):1089–1092. doi: 10.1227/01.NEU.0000057697.62046.16. [DOI] [PubMed] [Google Scholar]
- 32.Graziano G, Jaggers C, Lee M, Lynch W. A comparative study of fixation techniques for type II fractures of the odontoid process. Spine (Phila Pa 1976) 1993;18(16):2383–2387. doi: 10.1097/00007632-199312000-00003. [DOI] [PubMed] [Google Scholar]
- 33.Sasso R, Doherty BJ, Crawford MJ, Heggeness MH. Biomechanics of odontoid fracture fixation. Comparison of the one- and two-screw technique. Spine (Phila Pa 1976) 1993;18(14):1950–1953. doi: 10.1097/00007632-199310001-00004. [DOI] [PubMed] [Google Scholar]
- 34.Jenkins JD, Coric D, Branch CL., Jr A clinical comparison of one- and two-screw odontoid fixation. J Neurosurg. 1998;89(3):366–370. doi: 10.3171/jns.1998.89.3.0366. [DOI] [PubMed] [Google Scholar]
- 35.Koller H, Kolb K, Zenner J, et al. Study on accuracy and interobserver reliability of the assessment of odontoid fracture union using plain radiographs or CT scans. Eur Spine J. 2009;18(11):1659–1668. doi: 10.1007/s00586-009-1134-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. 1974. J Bone Joint Surg Am A. 2004;86(9):2081. [PubMed] [Google Scholar]
- 37.Lakshmanan P, Jones A, Howes J, Lyons K. CT evaluation of the pattern of odontoid fractures in the elderly-relationship to upper cervical spine osteoarthritis. Eur Spine J. 2005;14(1):78–83. doi: 10.1007/s00586-004-0743-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Majercik S, Tashjian RZ, Biffl WL, Harrington DT, Cioffi WG. Halo vest immobilization in the elderly: a death sentence? J Trauma. 2005;59(2):350–356. doi: 10.1097/01.ta.0000174671.07664.7c. [DOI] [PubMed] [Google Scholar]
- 39.Tashjian RZ, Majercik S, Biffl WL, Palumbo MA, Cioffi WG. Halo-vest immobilization increases early morbidity and mortality in elderly odontoid fractures. J Trauma. 2006;60(1):199–203. doi: 10.1097/01.ta.0000197426.72261.17. [DOI] [PubMed] [Google Scholar]
- 40.Garfin SR, Botte MJ, Waters RL, Nickel VL. Complications in the use of the halo fixation device. J Bone Joint Surg Am. 1986;68(3):320–325. [PubMed] [Google Scholar]
- 41.Apuzzo ML, Heiden JS, Weiss MH, et al. Acute fractures of the odontoid process. An analysis of 45 cases. J Neurosurg. 1978;48(1):85–91. doi: 10.3171/jns.1978.48.1.0085. [DOI] [PubMed] [Google Scholar]
- 42.Clark CR, White AA,, III Fractures of the dens. A multicenter study. J Bone Joint Surg Am. 1985;67(9):1340–1348. [PubMed] [Google Scholar]
- 43.Hadley MN, Dickman CA, Browner CM, Sonntag VK. Acute axis fractures: a review of 229 cases. J Neurosurg. 1989;71(5 Pt 1):642–647. doi: 10.3171/jns.1989.71.5.0642. [DOI] [PubMed] [Google Scholar]
- 44.Lennarson PJ, Mostafavi H, Traynelis VC, Walters BC. Management of type II dens fractures: a case–control study. Spine (Phila Pa 1976) 2000;25(10):1234–1237. doi: 10.1097/00007632-200005150-00006. [DOI] [PubMed] [Google Scholar]
- 45.Lind B, Nordwall A, Sihlbom H. Odontoid fractures treated with halo-vest. Spine (Phila Pa 1976) 1987;12(2):173–177. doi: 10.1097/00007632-198703000-00014. [DOI] [PubMed] [Google Scholar]
- 46.Althoff B. Fracture of the odontoid process. An experimental and clinical study. Acta Orthop Scand Suppl. 1979;177:1–95. doi: 10.3109/ort.1979.50.suppl-177.01. [DOI] [PubMed] [Google Scholar]
- 47.Blockey NJ, Purser DW. Fractures of the odontoid process of the axis. J Bone Joint Surg Br. 1956;38-B(4):794–817. doi: 10.1302/0301-620X.38B4.794. [DOI] [PubMed] [Google Scholar]
- 48.Dickson H, Engel S, Blum P, Jones RF. Odontoid fractures, systemic disease and conservative care. Aust N Z J Surg. 1984;54(3):243–247. doi: 10.1111/j.1445-2197.1984.tb05311.x. [DOI] [PubMed] [Google Scholar]
- 49.Fujii E, Kobayashi K, Hirabayashi K. Treatment in fractures of the odontoid process. Spine (Phila Pa 1976) 1988;13(6):604–609. [PubMed] [Google Scholar]
- 50.Hentzer L, Schalimtzek M. Fractures and subluxations of the atlas and axis. A follow-up study of 20 patients. Acta Orthop Scand. 1971;42(3):251–258. doi: 10.3109/17453677108989044. [DOI] [PubMed] [Google Scholar]
- 51.Wang GJ, Mabie KN, Whitehill R, Stamp WG. The nonsurgical management of odontoid fractures in adults. Spine (Phila Pa 1976) 1984;9(3):229–230. doi: 10.1097/00007632-198404000-00001. [DOI] [PubMed] [Google Scholar]
- 52.(2002) Isolated fractures of the axis in adults. Neurosurgery 50(3 Suppl):S125–S139 [DOI] [PubMed]
- 53.Ziai WC, Hurlbert RJ. A six year review of odontoid fractures: the emerging role of surgical intervention. Can J Neurol Sci. 2000;27(4):297–301. doi: 10.1017/s0317167100001037. [DOI] [PubMed] [Google Scholar]
- 54.Platzer P, Thalhammer G, Oberleitner G, et al. Surgical treatment of dens fractures in elderly patients. J Bone Joint Surg Am. 2007;89(8):1716–1722. doi: 10.2106/JBJS.F.00968. [DOI] [PubMed] [Google Scholar]
- 55.Greene KA, Dickman CA, Marciano FF, et al. Acute axis fractures. Analysis of management and outcome in 340 consecutive cases. Spine (Phila Pa 1976) 1997;22(16):1843–1852. doi: 10.1097/00007632-199708150-00009. [DOI] [PubMed] [Google Scholar]
- 56.Koller H, Resch H, Acosta F, et al. Assessment of two measurement techniques of cervical spine and C1–C2 rotation in the outcome research of axis fractures: a morphometrical analysis using dynamic computed tomography scanning. Spine (Phila Pa 1976) 2010;35(3):286–290. doi: 10.1097/BRS.0b013e3181c911a0. [DOI] [PubMed] [Google Scholar]
- 57.White AA, III, Panjabi MM. Clinical biomechanics of the spine. Clinical biomechanics of the spine. 2. Baltimore: Lippincott Williams & Wilkins; 1990. pp. 610–611. [Google Scholar]
- 58.Bhanot A, Sawhney G, Kaushal R, Aggarwal AK, Bahadur R. Management of odontoid fractures with anterior screw fixation. J Surg Orthop Adv. 2006;15(1):38–42. [PubMed] [Google Scholar]
- 59.Fountas KN, Machinis TG, Kapsalaki EZ, et al. Surgical treatment of acute type II and rostral type III odontoid fractures managed by anterior screw fixation. South Med J. 2005;98(9):896–901. doi: 10.1097/01.smj.0000177342.81752.74. [DOI] [PubMed] [Google Scholar]
- 60.ElSaghir H, Bohm H. Anderson type II fracture of the odontoid process: results of anterior screw fixation. J Spinal Disord. 2000;13(6):527–530. doi: 10.1097/00002517-200012000-00011. [DOI] [PubMed] [Google Scholar]
- 61.Lee SH, Sung JK. Anterior odontoid fixation using a 4.5-mm Herbert screw: the first report of 20 consecutive cases with odontoid fracture. Surg Neurol. 2006;66(4):361–366. doi: 10.1016/j.surneu.2006.04.018. [DOI] [PubMed] [Google Scholar]
- 62.Shilpakar S, McLaughlin MR, Haid RW, Jr, Rodts GE, Jr, Subach BR. Management of acute odontoid fractures: operative techniques and complication avoidance. Neurosurg Focus. 2000;8(6):e3. [PubMed] [Google Scholar]
- 63.Geisler FH, Cheng C, Poka A, Brumback RJ. Anterior screw fixation of posteriorly displaced type II odontoid fractures. Neurosurgery. 1989;25(1):30–37. doi: 10.1227/00006123-198907000-00006. [DOI] [PubMed] [Google Scholar]
- 64.Collins I, Min WK. Anterior screw fixation of type II odontoid fractures in the elderly. J Trauma. 2008;65(5):1083–1087. doi: 10.1097/TA.0b013e3181848cbc. [DOI] [PubMed] [Google Scholar]