Abstract
Kyphosis is a common sequel of inadequately managed thoracolumbar fractures. This study compares between pedicle subtraction osteotomy (PSO) and anterior corpectomy and plating (ACP) for correcting post-traumatic kyphosis. Forty-three patients with symptomatic post-traumatic kyphosis of the thoracolumbar spine were treated with PSO and prospectively followed for a minimum of 2 years. Visual Analogue Scale (VAS) and Oswestry Disability Index (ODI) were used to assess clinical improvement and radiographs were obtained at 2, 6, 12 and 24 months. The recorded clinical and radiological outcomes were compared to a control group of 37 patients, who were treated earlier by the same authors with ACP. The mean correction of the kyphotic angle was 29.8° for the PSO group and 22° for the ACP group (P = 0.001). PSO group showed significantly better improvement in the VAS score and the ODI. At final follow-up, patients reported very good satisfaction (93% in PSO vs. 81% in ACP) and good function (90% in PSO vs. 73% in ACP). Complications in the PSO group included pulling out of screws and recurrence of deformity requiring revision and longer fixation (1 patient), and transient lower limb paraesthesia (2 patients). Recorded complications in the ACP group included an aortic injury (1 patient) that was successfully repaired, pseudarthrosis (1 patient), persistent graft donor site morbidity (3 patients), and incisional hernia (1 patient). PSO and ACP are demanding procedures. PSO seems to be equally safe but more effective than ACP for correcting post-traumatic kyphosis.
Keywords: Post-traumatic, Kyphosis, Dorsolumbar fractures, PSO, Anterior corpectomy
Introduction
Kyphosis is a common sequel of neglected or inadequately managed thoracolumbar fractures. Post-traumatic kyphosis may become progressive as the line of gravity shifts forward and as posterior erector muscles weaken [1]. Patients with kyphotic deformity of >30° are at increased risk for having chronic pain in their kyphotic region [2–4] and may occasionally develop progressive neurologic deficit [3, 4]. Furthermore, compensatory hyperextension of the lower lumbar spine has been linked to a higher incidence of low-back pain, degenerative facet arthritis and painful spondylolysis [5, 6].
Kostuik [4, 7] advocated the anterior approach for treating post-traumatic kyphosis. Posterior instrumentation following anterior intervention to protect anteriorly placed strut grafts and to correct vertebral instability is the most commonly used method since then [8–10]. Several more recent studies reported successful outcome after anterior corpectomy and only anterior instrumentation using various types of implants [11–14].
Pedicle subtraction osteotomy (PSO) was introduced several years ago to correct sagittal imbalance as an alternative method with favorable outcome [2, 15–20]. Buchowski et al. [21] recently reviewed the literature concerning post-traumatic kyphosis and recommended the use of PSO in cases associated with normal sagittal balance and sharp angular deformity. However, to date, very few reports have focused on the use of PSO in post-traumatic kyphosis [22, 23] and, to the best of our knowledge, none has compared between PSO and anterior corpectomy and plating (ACP) for this surgical indication.
The aim of this study is to compare the clinical and radiological outcomes of PSO and ACP for correcting post-traumatic kyphosis of the thoracolumbar spine.
Methods
Forty-three consecutive patients with symptomatic post-traumatic kyphosis of the thoracolumbar spine were treated with PSO and were prospectively followed for a minimum of 2 years. Four spine surgeons were involved in these surgeries and cases were collected from three tertiary care centers. There were 15 females and 28 males with a mean age at time of surgery of 34.2 years (range 19–66 years). The mean time from trauma to surgery was 15.3 months (range 3–39 months). Most fractures/deformity apex occurred at L1 (39.5%) followed in incidence by D12 levels (Table 1).
Table 1.
Demographic data of the patients
| Operative technique | PSO | ACP | P |
|---|---|---|---|
| Number of patients | 43 | 37 | |
| Gender (M/F) | 28/15 | 22/15 | |
| Mean Age in years | 34.2 ± 9.9 | 35.6 ± 9.4 | 0.518 |
| Fracture/deformity level: number of patients | D10: 2 (4.7%) | D10: 1 (2.7%) | |
| D11: 3 (7%) | D11: 2 (5.4%) | ||
| D12: 11 (25.6%) | D12 :9 (24.3%) | ||
| L1: 17 (39.5%) | L1: 13 (35.1%) | ||
| L2:7 (16.2%) | L2: 7 (19%) | ||
| L3: 3 (7%) | L3: 5 (13.5%) | ||
| Time interval between trauma and surgery in months | 19.1 ± 10.6 | 15.7 ± 9.7 | 0.133 |
| Preop. VAS | 8.7 ± 1 | 8.7 ± 1 | 0.725 |
| Preop. ODI score | 38.1 ± 3.5 | 37.5 ± 3.7 | 0.463 |
| Preop. kyphosis angle | 33.7° ± 4.5° | 31.7° ± 5.2° | 0.075 |
| Follow-up duration | 29.3 ± 3.7 | 40.1 ± 6.8 | 0.001 |
Detailed history was obtained; particular attention was given to symptoms suggesting neurologic claudication or sphincteric disturbance. The Visual Analogue Scale (VAS) and Oswestry Disability Index (ODI) were used for pain and functional assessment. Physical examination along with a detailed neurologic examination was done. All patients were neurologically intact and had persistent pain localized to the apex of the kyphotic deformity. Seven patients (16%) had also persistent low back pain and eighteen patients (42%) indicated that the cosmetic appearance of their back was also a major concern.
Radiographic evaluation included standing lateral and posteroanterior radiographs. The local kyphotic angle was measured independently by the four surgeons on standing lateral radiographs between lines drawn along the upper and lower endplates of the fractured vertebra and the average of the 4 readings was recorded. MR images were obtained to exclude any neural compression or post-traumatic syringomyelia.
The operative technique used is the same as described by Bridwell et al. [16, 18]. In young patients and in patients with good bone stock, pedicle screws were inserted in only one level above and below the deformity level (29 patients). In older patients and in osteoporotic patients, pedicle screws were inserted in two levels above and below the osteotomy level. Only fourteen patients (32.5%) had instrumentation extended to 2 levels above and below the osteotomy. Correction of the deformity without inducing any anterior column lengthening or defect was ascertained by intra-operative imaging in all patients. A wake-up test was routinely used for neurologic monitoring. The operative time and the amount of blood loss were recorded. All patients were allowed out of bed on the first postoperative day. No cast or brace was used after surgery.
At each follow-up visit, patients were evaluated both clinically and radiographically. Radiographs were obtained at 2, 6, 12 months and every 6 months thereafter. Only patients who have completed a minimum follow-up period of 2 years were included in this study. The recorded clinical and radiological outcomes were compared to a historical group of patients, who were treated earlier with ACP by the same surgeons from the three institutes. Thirty-seven patients out of 45 ACP patients (82%) responded to the invitation for follow-up and constituted the control group. The study protocol was approved by the institutional ethics committee and all patients gave an informed consent. Table 1 summarizes the clinical data of the patients.
Statistical analysis of the data was performed using SPSS 17.0 software (SPSS Inc., Chicago, IL). Continuous variables (such as age, time interval between trauma and surgery, VAS, ODI, kyphosis angle, blood loss, operative time, and follow-up time) were compared using a two-sample t test. Probability values of <0.05 were considered to be significant. Grouped variables (such as gender, and deformity level) were evaluated using a Pearson Chi-square test; values of <0.05 were considered significant. Statistical evaluation of all the demographic data of patients was performed and showed no statistical difference between the two groups except for the duration of follow-up (P = 0.001), which was longer for the historical ACP group (mean 40.1 ± 6.8 months, range 30–60 months) when compared to the PSO group (mean 29.3 ± 3.7 months, range 24–36 months).
Results
No patient in the PSO group was lost to follow-up. The mean estimated blood loss was 1,107.4 ± 366.2 ml (range 370–1,750 ml) in the PSO group and 1,071.6 ± 544.7 ml (range 450–3,100 ml) in the ACP group with no statistical difference. The mean operative time was 149.2 ± 30.2 min (range 90–210 min) in the PSO group and 165.3 ± 46.7 min (range 150–325 min) in the ACP group, again with no statistical difference.
There was significant improvement of the VAS and ODI scores in both groups following surgery. The mean VAS for pain dropped down from 8.7 ± 1 to 0.95 ± 1 in the PSO group (P = 0.001), and from 8.7 ± 1 to 1.8 ± 1.3 in the ACP group (P = 0.001). The mean VAS difference was statistically significant (P = 0.013) in favor of the PSO group. Likewise, the mean ODI score showed significant decrease from 38.1 ± 3.5 to 6.2 ± 1.9 in the PSO group (P = 0.001), and from 37.5 ± 3.7 to 9.7 ± 2.8 in the ACP group (P = 0.001). The mean ODI score difference was also statistically significant (P = 0.001) in favor of the PSO group.
In answer to the question “If you could go back in time and make decisions again, would you choose the same treatment for your musculoskeletal condition or problem?”, 40 patients (93%) of the PSO group replied definitely yes, and 3 (7%) were not sure. In the ACP group, 30 patients (81.1%) replied by definitely yes, 2 (5.4%) were not sure, and 5 patient (13.5%) replied by definitely not (P = 0.045). In the PSO group, 39 patients (90.7%) returned to their previous work or activity level and 4 (9.3%) to a lighter work, whereas in the ACP group, 27 patients (73%) returned to their previous work or activity level, 6 (16.2%) to a lighter work and 4 (10.8%) retired (P = 0.046).
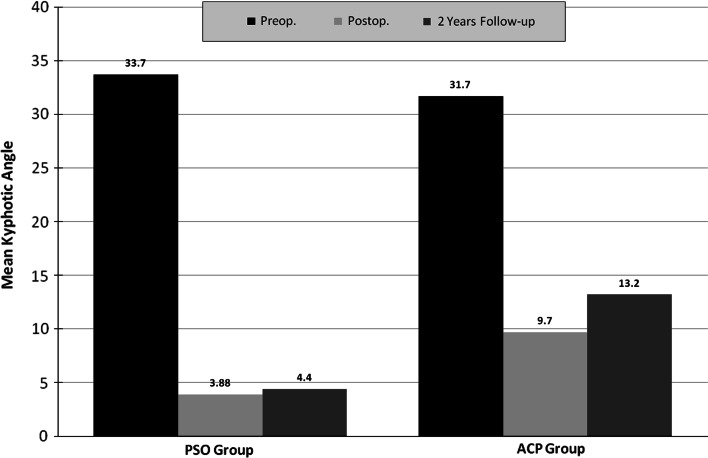
The mean preoperative kyphotic angle (Figs. 1, 2, 3, 4, 5) was 33.7° ± 4.5° in the PSO group and 31.7° ± 5.2° in the ACP group. Postoperatively, this has improved to 3.8° ± 3.4° in the PSO group and to 9.7° ± 6.4° in the ACP group (P = 0.001). The mean amount of correction of the kyphotic angle was 29.8° ± 3.4° for the PSO group and 22° ± 3.7° for the ACP group (P = 0.001). At the latest follow-up, the mean angle was 4.4° ± 3.5° in the PSO group and 13.2° ± 6.2° in the ACP group with a mean loss of correction of 0.5° ± 0.7° in the PSO group compared to 3.4° ± 1.2° in the ACP group (P = 0.001).
Fig. 1.
Changes in mean kyphotic angle in the PSO and ACP groups
Fig. 2.
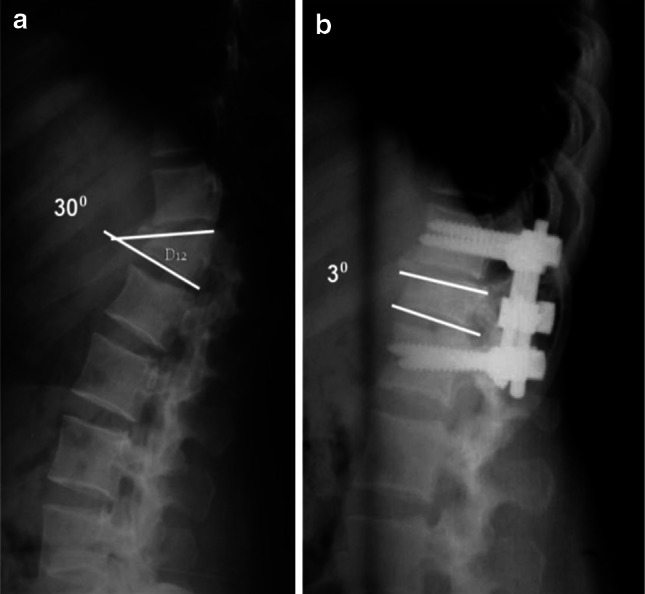
a Lateral X-ray of a 41-year-old manual worker who is suffering from severe back pain and inability to work for 1 year due to post-traumatic kyphosis of D12 of 30°. b Two years follow-up lateral X-ray after PSO shows excellent correction of the deformity to 3°. This patient returned to his previous work 9 months postoperatively
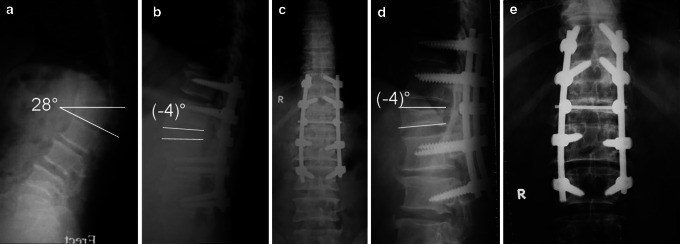
Fig. 3.

A 27-year-old accountant presented with severe back pain and deformity and inability to work. Five months earlier, he had percutaneous fixation of his L1 fracture in another hospital. a Lateral X-ray shows post-traumatic kyphosis of L1 of 28°. b Two years follow-up X-ray after PSO shows excellent correction of the deformity to (−4)°. He resumed his previous work 6 months postoperatively
Fig. 4.
a Lateral X-ray of a 58-year-old worker who is suffering from severe back pain and inability to work for 15 months due to post-traumatic kyphosis of L1 of 28°. b, c Postoperative X-rays show excellent correction of the deformity to (−4°). d, e Two years follow-up X-rays after PSO show maintenance of deformity correction and solid fusion. He resumed his previous work 6 months postoperatively. Although the distal screws seem to have pulled out partially, this was asymptomatic and did not affect the degree of local kyphosis correction. This backing out of the very distal screws was observed in the 2-month radiographs and was attributed to overcontouring of the rods
Fig. 5.
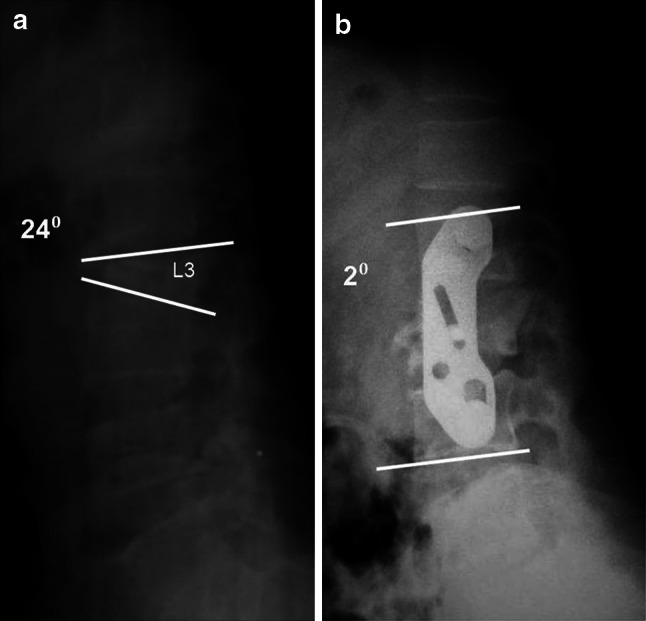
a Lateral X-ray of a 33-year-old housewife who is suffering from severe back pain for the last 7 months due to post-traumatic kyphosis of L3 of 24°. b Two years follow-up lateral X-ray following ACP shows significant correction of her deformity to 2°. She fully resumed her activities of daily living 4 months postoperatively, despite the suboptimal correction of her deformity
No neurological deterioration was observed in either group. One patient in the PSO group was noted during the wake-up test to have sluggish movement in his right leg. This improved immediately following further central decompression. Complications in the PSO group included transient lower limb paraesthesia occurring in two patients that resolved spontaneously within 2 days. Pulling out of distal screws associated with severe pain and recurrence of the deformity was detected in the second postoperative day in an old osteoporotic patient, who was successfully revised with longer fixation segments. His kyphosis correction was maintained and confirmed in his follow-up X-rays. Recorded complications in the ACP group included an accidental aortic injury in a young patient from a slipped instrument that was successfully repaired. Painful pseudarthrosis was detected in another patient, who refused any further surgical management. Persistent graft donor site pain was recorded in three patients, and one patient suffered incisional hernia that was surgically treated.
Discussion
Kyphosis is a common sequel of neglected or inadequately managed thoracolumbar fractures. Post-traumatic kyphosis may become progressive [1], may cause severe pain at its apex [2–4] and/or in the low-back [5, 6] and may occasionally develop progressive neurologic deficit [3, 4].
The choice of surgical technique for the correction of sagittal plane deformity may involve an anterior-only surgery, a posterior-only surgery, or a combined anterior–posterior surgery. Successful clinical and radiological outcomes were reported after anterior corpectomy and anterior instrumentation [11–14] as well as following pedicle subtraction osteotomy [15–20]. Combined anterior–posterior surgery is associated with a high (32%) perioperative complication rate and therefore its use should be limited to revisions and pseudarthrosis cases and fusions across the lumbosacral junction [24].
The aim of this study is to compare the two commonly used procedures to correct post-traumatic kyphosis, namely, the PSO and the ACP. To our knowledge, such comparison has never been published in the English literature. ACP has long been used to correct post-traumatic kyphosis with favorable outcome [4, 7, 12–14]. However, high incidence of complications has been reported, including major vascular injuries, neurological injuries, pseudarthrosis, significant graft donor site morbidity as well as prolonged recovery, delayed rehabilitation and patients’ dissatisfaction [11–13, 25, 26].
PSO has many theoretical advantages. PSO achieves correction through all three columns from a posterior approach without lengthening the anterior column, thereby maximizing the healing potential while avoiding stretch on the major vessels and viscera anterior to the spine. Furthermore, PSO is performed through a more familiar approach to all spine surgeons with no need for an access surgeon, no need to harvest bone graft, less operative time and blood loss in experienced hands, and faster mobilization and rehabilitation. Two major concerns, however, are always linked to PSO; safety and efficacy.
Most published reports on PSO include a heterogeneous group of type I and type II sagittal imbalance [16–20]. Post-traumatic kyphosis represents the commonest form of type I (focal) sagittal imbalance, which is associated with normal global alignment and its treatment strategy should be identified in distinction from that of type II (global) sagittal imbalance. The choice of osteotomy level is dictated in type I sagittal imbalance by the site of the deformity, frequently at the cord level. Bridwell et al. [17] included only 8 cases of post-traumatic kyphosis in his series of 66 patients. Other reported series included also a small number of patients with post-traumatic kyphosis [2, 22, 23], and none has previously compared between PSO and ACP for this specific indication. To the best of our knowledge, this is the largest series in the English literature focusing on post-traumatic kyphosis and comparing between PSO and ACP with a minimum of 2 years follow-up. No single incidence of neurological deterioration could be detected in the PSO group in our series, despite the fact that 33 PSOs (76.7%) were performed at the cord level (D10–L1), which proves the safety of the technique.
The efficacy of PSO for correcting post-traumatic kyphosis has also been proved in many previous studies [15–20, 22, 23]. However, our study has also proved its superiority over ACP with significantly better clinical outcome as reflected by the significant improvement of the mean pain VAS, mean ODI, patients’ satisfaction and ability to resume their previous work. From the radiological point of view, the mean amount of kyphosis correction achieved in our study in the ACP group (22°) was comparable or even better than many published reports. Yet, the mean amount of kyphosis correction achieved in the PSO group (30°) was significantly higher (P = 0.001).
Several factors were proposed to influence the results of surgery in post-traumatic kyphosis. These include patient age, general health status, type of trauma, time from trauma to operation, and surgical experience [15, 27]. It is our belief that the most important factor limiting the ability of anterior correction of post-traumatic kyphosis is the duration between the trauma and operation. We frequently observed, during posterior surgery, spontaneous fusion or at least marked ankylosis and stiffness of the facet joints, which is expected to limit the ability of the anterior surgery alone to correct post-traumatic deformity. Osteoporosis is another important limiting factor against anterior correction; the distraction force applied on the main bolts may lead to their loosening and contribute to loss of correction. In PSO, on the other hand, any spontaneously fused facets are excised, which significantly mobilizes the spine and allows better correction without the use of any forceful maneuvers. Furthermore, in osteoporotic patients, one can easily add more pedicle screws over a longer segment to achieve adequate fixation and consequently prevent implant loosening or loss of correction.
Significant loss of correction has been frequently reported after anterior surgery [13, 24, 26], which coincides with the finding in our series, where a mean loss of kyphosis correction of 3.4° was observed in the ACP group. On the other hand, there was no significant loss of correction in our PSO group, which also coincides with all published reports on PSO [15–23, 27]. Loss of correction in either case is usually observed in the early follow-up period. Kim et al. [20] found no significant radiographic changes between 2 and 5 years follow-up after PSO for various etiologies and therefore the difference observed between the two groups in the current study cannot be related to a shorter follow-up period in the PSO group.
This study could be criticized for not assessing the flexibility of the kyphosis deformity and for using a less accurate method of kyphosis angle measurement especially in the presence of post fracture deformation of the endplate(s) rather than the use of one level above/one level below measurement. In fact, flexibility analysis of the kyphosis deformity was not available for most of the historical ACP group, and to avoid possible flaws and confusion, the authors decided to rely on the endplates of the deformed vertebra to be able to compare both groups. To face the occasional problem of endplate deformation, the angle was independently measured by the four authors and an average value was recorded for all cases.
Management of post-traumatic thoracolumbar kyphosis remains controversial: anterior, posterior or combined anterior and posterior procedures have been advocated by different authors and have shown various degrees of success. We believe that PSO provides better clinical and radiographic outcomes for patients with post-traumatic kyphosis.
Conflict of interest
None.
References
- 1.Roberson JR, Whitesides TE. Surgical reconstruction of late post-traumatic thoracolumbar kyphosis. Spine. 1985;10:307–312. doi: 10.1097/00007632-198505000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Gertzbein SD, Harris MB. Wedge osteotomy for the correction of posttraumatic kyphosis: a new technique and a report of three cases. Spine. 1992;17:374–379. doi: 10.1097/00007632-199203000-00025. [DOI] [PubMed] [Google Scholar]
- 3.Malcolm BW, Bradford DS, Winter RB, Chou SN. Post-traumatic kyphosis: a review of forty-eight surgically treated patients. J Bone Joint Surg Am. 1981;63:891–899. [PubMed] [Google Scholar]
- 4.Kostuik JP, Matsusaki H. Anterior stabilization instrumentation, and decompression for post-traumatic kyphosis. Spine. 1989;14:379–386. doi: 10.1097/00007632-198904000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Oda I, Cunningham BW, Buckley RA, Goebel MJ, Haggerty CJ, Orbegoso CM, McAfee PC. Does spinal kyphotic deformity influence the biomechanical characteristics of the adjacent motion segments? An in vivo animal model. Spine. 1999;24:2139–2146. doi: 10.1097/00007632-199910150-00014. [DOI] [PubMed] [Google Scholar]
- 6.Dietrich M, Kurowski P. The importance of mechanical factors in the etiology of spondylolysis: a model analysis of loads and stresses in human lumbar spine. Spine. 1985;10:532–542. doi: 10.1097/00007632-198507000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Kostuik JP. Anterior Kostuik–Harrington distraction system for the treatment of kyphotic deformities. Spine. 1990;15:169–180. doi: 10.1097/00007632-199003000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Illes T, de Jonge T, Doman I, Doczi T. Surgical correction of the late consequences of post-traumatic spinal disorders. J Spinal Disord Tech. 2002;15:127–132. doi: 10.1097/00024720-200204000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Stoltze D, Harms J. Correction of post-traumatic deformities: principles and methods. Orthopäde. 1999;28:731–745. doi: 10.1007/PL00003661. [DOI] [PubMed] [Google Scholar]
- 10.Suk SI, Kim JH, Lee SM, Chung ER, Lee JH. Anterior–posterior surgery versus posterior closing wedge osteotomy in posttraumatic kyphosis with neurologic compromised osteoporotic fracture. Spine. 2003;28:2170–2175. doi: 10.1097/01.BRS.0000090889.45158.5A. [DOI] [PubMed] [Google Scholar]
- 11.Eysel P, Hopf C, Furderer S. Kyphotic deformation in fractures of the thoracic and lumbar spine. Orthopäde. 2001;30:355–364. doi: 10.1007/s001320170009. [DOI] [PubMed] [Google Scholar]
- 12.Kaneda K. Anterior approach and Kaneda instrumentation for lesions of the thoracic and lumbar spine. In: Bridwell KH, DeWald RL, editors. The textbook of spinal surgery. Philadelphia: Lippincott; 1991. pp. 959–990. [Google Scholar]
- 13.Benli T, Kaya A, Uruc V, Akalin S. Minimum 5-year follow-up surgical results of post-traumatic thoracic and lumbar kyphosis treated with anterior instrumentation comparison of anterior plate and dual rod systems. Spine. 2007;9:986–994. doi: 10.1097/01.brs.0000260796.77990.f7. [DOI] [PubMed] [Google Scholar]
- 14.Been HD, Poolman RW, Ubags LH. Clinical outcome and radiographic results after surgical treatment of post-traumatic thoracolumbar kyphosis. Eur Spine J. 2004;13:101–107. doi: 10.1007/s00586-003-0576-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berven SH, Deviren V, Smith JA, Emami A, Hu SS, Bradford DS. Management of fixed sagittal plane deformity: results of the transpedicular wedge resection osteotomy. Spine. 2001;26:2036–2043. doi: 10.1097/00007632-200109150-00020. [DOI] [PubMed] [Google Scholar]
- 16.Bridwell KH, Lewis SJ, Lenke LG, Baldus C, Blanke K. Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. J Bone Joint Surg Am. 2003;85:454–463. doi: 10.2106/00004623-200303000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Bridwell KH, Lewis SJ, Edwards C, Lenke LG, Iffrig TM, Berra A, Baldus C, Blanke K. Complications and outcomes of pedicle subtraction osteotomies for fixed sagittal imbalance. Spine. 2003;28:2093–2101. doi: 10.1097/01.BRS.0000090891.60232.70. [DOI] [PubMed] [Google Scholar]
- 18.Bridwell KH, Lewis SJ, Rinella A, Lenke LG, Baldus C, Blanke K. Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. Surgical technique. J Bone Joint Surg Am. 2004;86(Suppl 1):44–50. doi: 10.2106/00004623-200403001-00007. [DOI] [PubMed] [Google Scholar]
- 19.Yang BP, Ondra SL, Chen LA, Jung HS, Koski TR, Salehi SA. Clinical and radiographic outcomes of thoracic and lumbar pedicle subtraction osteotomy for fixed sagittal imbalance. J Neurosurg Spine. 2006;5:9–17. doi: 10.3171/spi.2006.5.1.9. [DOI] [PubMed] [Google Scholar]
- 20.Kim YJ, Bridwell KH, Lenke LG, Cheh G, Baldus C. Results of lumbar pedicle subtraction osteotomies for fixed sagittal imbalance: a minimum 5-year follow-up study. Spine. 2007;32:2189–2197. doi: 10.1097/BRS.0b013e31814b8371. [DOI] [PubMed] [Google Scholar]
- 21.Buchowski JM, Kuhns CA, Bridwell KH, Lenke LG. Surgical management of posttraumatic thoracolumbar kyphosis. Spine J. 2008;8:666–677. doi: 10.1016/j.spinee.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 22.Wu SS, Hwa SY, Lin LC, Pai WM, Chen PQ, Au MK. Management of rigid post-traumatic kyphosis. Spine. 1996;19:2260–2266. doi: 10.1097/00007632-199610010-00016. [DOI] [PubMed] [Google Scholar]
- 23.Lazennec JY, Neves N, Rousseau MA, Boyer P, Mousselard HP, Saillant G. Wedge osteotomy for treating post-traumatic kyphosis at thoracolumbar and lumbar levels. J Spinal Disord Tech. 2006;19:487–494. doi: 10.1097/01.bsd.0000211296.52260.9c. [DOI] [PubMed] [Google Scholar]
- 24.Berven S, Deviren V, Smith J, Hu S, Bradford D. Management of fixed sagittal plane deformity: outcome of combined anterior and posterior surgery. Spine. 2003;15:1710–1716. doi: 10.1097/01.BRS.0000083181.25260.D6. [DOI] [PubMed] [Google Scholar]
- 25.Oskouian RJ, Jr, Johnson JP. Vascular complications in anterior thoracolumbar spinal reconstruction. J Neurosurg. 2002;96(1 Suppl):1–5. doi: 10.3171/jns.2002.96.1.0001. [DOI] [PubMed] [Google Scholar]
- 26.Kim YB, Lenke LG, Kim YJ, Kim YW, Blanke K, Stobbs G, Bridwell KH. The morbidity of an anterior thoracolumbar approach: adult spinal deformity patients with greater than five-year follow-up. Spine. 2009;34:822–826. doi: 10.1097/BRS.0b013e31818e3157. [DOI] [PubMed] [Google Scholar]
- 27.Munting E. Surgical treatment of post-traumatic kyphosis in the thoracolumbar spine: indications and technical aspects. Eur Spine J. 2010;19(Suppl 1):S69–S73. doi: 10.1007/s00586-009-1117-3. [DOI] [PMC free article] [PubMed] [Google Scholar]