Abstract
Introduction
Standing in an erect position is a human property. The pelvis anatomy and position, defined by the pelvis incidence, interact with the spinal organization in shape and position to regulate the sagittal balance between both the spine and pelvis. Sagittal balance of the human body may be defined by a setting of different parameters such as (a) pelvic parameters: pelvic incidence (PI), pelvic tilt (PT) and sacral slope (SS); (b) C7 positioning: spino-pelvic angle (SSA) and C7 plumb line; (c) shape of the spine: lumbar lordosis.
Biomechanical adaptation of the spine in pathology
In case of pathological kyphosis, different mechanical compensations may be activated. When the spine remains flexible, the hyperextension of the spine below or above compensates the kyphosis. When the spine is rigid, the only way is rotating backward the pelvis (retroversion). This mechanism is limited by the value of PI. Hip extension is a limitation factor of big retroversion when PI is high. Flexion of the knees may occur when hip extension is overpassed. The quantity of global kyphosis may be calculated by the SSA. The more SSA decreases, the more the severity of kyphosis increases. We used Roussouly’s classification of lumbar lordosis into four types to define the shape of the spine. The forces acting on a spinal unit are combined in a contact force (CF). CF is the addition of gravity and muscle forces. In case of unbalance, CF is tremendously increased. Distribution of CF depends on the vertebral plate orientation. In an average tilt (45°), the two resultants, parallel to the plate (sliding force) or perpendicular (pressure), are equivalent. If the tilt increases, the sliding force is predominant. On the contrary, with a horizontal plate, the pressure increases. Importance of curvature is another factor of CF distribution. In a flat or kyphosis spine, CF acts more on the vertebral bodies and disc. In the case of important extension curvature, it is on the posterior elements that CF acts more. According to the shape of the spine, we may expect different degenerative evolution: (a) Type 1 is a long thoraco-lumbar kyphosis and a short hyperlordosis: discopathies in the TL area and arthritis of the posterior facets in the distal lumbar spine. In younger patients, L4 S1 hyperextension may induce a nutcracker L5 spondylolysis. (b) Type 2 is a flat lordosis: Stress is at its maximum on the discs with a high risk of early disc herniation than later with multilevel discopathies. (c) Type 3 has an average shape without characteristics for a specific degeneration of the spine. (d) Type 4 is a long and curved lumbar spine: this is the spine for L5 isthmic lysis by shear forces. When the patient keeps the lordosis curvature, a posterior arthritis may occur and later a degenerative L4 L5 spondylolisthesis. Older patients may lose the lordosis curvature, SSA decreases and pelvis tilt increases. A widely retroverted pelvis with a high pelvic incidence is certainly a previous Type 4 and a restoration of a big lordosis is needed in case of arthrodesis.
Conclusion
The genuine shape of the spine is probably one of the main mechanical factors of degenerative evolution. This shape is oriented by a shape pelvis parameter, the pelvis incidence. In case of pathology, this constant parameter is the only signature to determine the original spine shape we have to restore the balance of the patient.
Keywords: Lumbar lordosis, Spino-sacral angle, Thoracic kyphosis, Pelvic incidence, Pelvic tilt, Sacral slope, Sagittal balance, Pathological balance
Introduction
The acquisition of a vertical posture, i.e., the ability Man acquired to extend simultaneously the trunk, hips, thigh and legs—and the resulting bipedal locomotion represented definitively the main transformation in the history of the Hominidae, the one that induced slowly the others, the evolution of the hand and the brain, which consequently gave rise to the tools, conscience, culture and the society [1].
Human beings are the only vertebrates to maintain an upright, totally vertical, bipedal position. In addition to diverse other morphological transformations, as the relations between the foramen magnum orientation and the cervical spine, the spino-pelvic complex played a relevant role in the acquisition of bipedalism. Unlike other vertebrates, the human spine comprises successive, opposing curves that allow the trunk to assume an erect position. The lumbar lordosis is found in no other species. The great apes can achieve an upright position, but only with a semi-erect trunk. Their whole spine looks like a big “C”, a long kyphosis that is incompatible with a constant stable erect posture and walking. Bipedal locomotion in non-human primates is awfully limited. They often use their long forelimbs in pronation for balance when trying to perform a bipedal displacement. Studies have shown that the orangutans are frequently biped, with knees in extension (a characteristic usually associated with human bipedalism [2]. The kangaroo, as well as the extinct Tyrannosaurus rex, walks (or walked) with two legs; however, they have (or had) a stabilizing tail [3]. The biomechanics of birds’ bipedalism also has nothing to do with ours [2].
The human pelvis has equally a tremendous importance in the development of verticality. Its intrinsic anatomical relationship with the spine created mechanisms to modulate posture. The pelvis attempts to couple lumbar lordosis with hip extension in the erect position with minimal expense of energy. However, some pelvis can accomplish this task better than others. Progressive knowledge has demonstrated that the shape of the pelvis and its relation to the sacral slope (SS) influence dramatically the type of lumbar lordosis in a single individual [4].
Thanks to the pelvic parameters described by Duval-Beaupère et al. [5–7], it became possible to define the pelvic geometry and the relation of this geometry with the position of the pelvis. In other words, for the first time, it was possible to relate the form and function of the pelvis. Recently, some authors have highlighted the correlation between the spino-pelvic organization and an eventual specific degenerative evolution derived from the original organization [8]. The key for it is the pelvic incidence (PI) angle. It is now crystal clear that the PI and the SS are important in determining the type of lumbar lordosis in a specific individual. According to the SS value, Roussouly et al. [8] described four types of lumbar lordosis. Each type represents a distinct spino-pelvic morphological complex. Each type of spino-pelvic geometry, with respective functional spinal units, will endure, obviously, mechanical stresses, according to the geometry of the lordosis and to the global spinal balance. A better understanding of the local stress on a vertebral unit allows understanding the relations between the geometry of discs and vertebrae, the combination of gravity and muscles forces and the resulting pathological consequences.
Any pattern of degenerative spine is not a static entity. It resulted from an evolution, a transformation. This evolution had certainly, among its causes, mechanical stresses. Both physicians and patients are not satisfied with terms such as non-specific lumbar degenerative disc disease or non-specific low back pain. It is imperative to understand the process to better target treatments. The opening of new horizons of knowledge will help understand the complex challenge that is degenerative disc disease. The comprehension of spinal sagittal balance and the identification of different morphotypes, which may undergo straight degenerative conditions, may imply earlier treatment possibilities, perhaps easier therapies or even prevention measures for specific situations according to each morphotype.
A thorough understanding of how different types of spino-pelvic complexes can lead to different patterns of degenerative spine disease may help the surgeon to tailor more appropriately the treatment strategy for his/her patient.
Biomechanics review
Pelvic parameters
Several authors [5, 9] have employed pelvic parameters to characterize morphologically and functionally the pelvis. Duval-Beaupère et al. defined the PI as the angle created by the intersection of the line drawn from the center of the femoral heads to the middle of the sacral plate and the line running perpendicular to the middle of the sacral plate. The PI is the angle that describes the relation between the sacral plate and the femoral heads. It is a constant morphological parameter for one person.
The result of PI on pelvis morphology
The pelvic incidence angle provides substantial information regarding the possibilities of pelvic compensation such as ability of pelvic retroversion. The PI determines the relative position of the sacral plate in relation to the femoral heads. In a recent study, we demonstrated that, in an asymptomatic population, the lower value is approximately 35° and the higher around 85°, the average being 51.9° [10]. IP values inferior to 35° are seen in Scheuermann disease and IP higher than 85° are seen in patients with isthmic spondylolisthesis as reported by Labelle et al. [11]. We assume that values outside these bounders are representative of pathological conditions.
Patients with a very low PI present a pelvis with a very short pelvic ring on the anterior–posterior (AP) diameter. The femoral heads are just below the sacral plate. Inversely, a pelvis with a high-grade PI has a large AP axis; it is a large horizontal pelvis. In the sagittal plane, the femoral heads are placed ahead the midpoint of the sacral plate (Fig. 1). As aforementioned, the vertical shape is less adapted to the verticality and has a low SS and, therefore, a low ability of pelvic tilting; conversely, a horizontal pelvis has a high SS and a higher possibilities of retroversion.
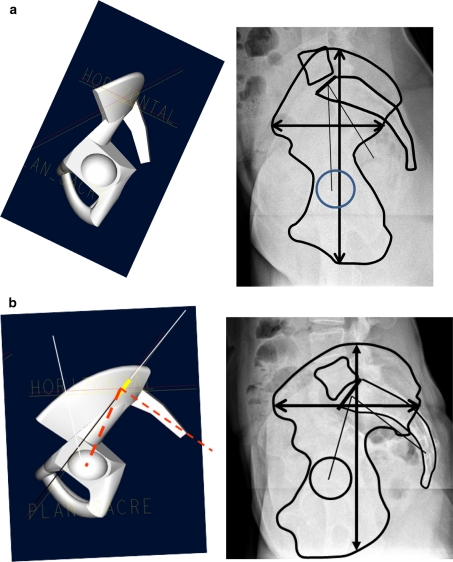
Fig. 1.
a Model and lateral X-ray of a low-grade pelvic incidence pelvis (vertical pelvis). Note the high position of L5 S1 disc with respect to the top of the iliac crest. b High-grade pelvic incidence pelvis (horizontal pelvis). L5 S1 disc and L5 are totally below the top of the iliac crest
The influence of PI on positioning the pelvis
The pelvis can rotate around the femoral heads, following the bicoxo-femoral axis. The pelvic tilt (PT) is the angle between the vertical line and the line drawn from the center of the femoral heads to the center of the upper sacral endplate. When the pelvis rotates backward (retroversion), PT increases; when the pelvis rotates forward (anteversion), PT decreases. PT is a positional parameter, as well as the SS. The SS refers to the orientation of the sacral plate in relation to a horizontal line.
There is a geometrical relation between the PI (morphological parameter) and the two positional (functional) parameters, PT and SS, according to the equation: PI = PT + SS [8]. The possibility of rotation of the pelvis around the femoral head’s axis is one of the best mechanisms of regulation of sagittal balance. Due to the relation among PI, PT and SS, PI induces directly the potential respective values of PT and SS, permitting major or minor compensation of a sagittal imbalance. Mac-Thiong et al. [12] suggested that the non-pathological upper limit of PT would ideally be <50% of PI. Likewise, the ideal values for SS should exceed 50% of PI. In pathology, SS never reaches a negative position, <0°. The minimal value of SS is 0°, which is the horizontal sacral plate. This situation corresponds to the maximal retroversion possible. A negative SS is not possible in erect persons. This hypothetical condition could be reached, however, if one sits backward in an office chair. We may assume that the theoretical maximum value of PT is equal to PI (Fig. 2).
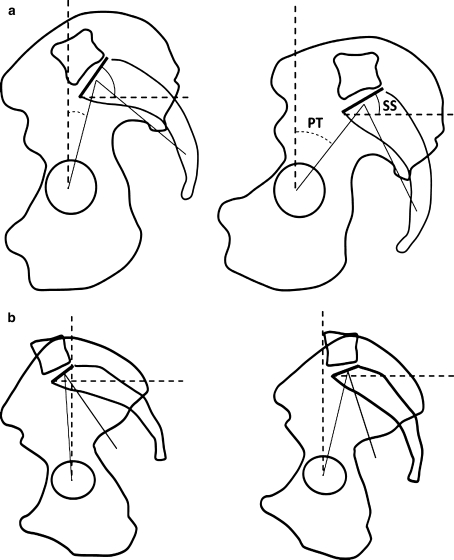
Fig. 2.
a For the same pelvis with the same PI, when PT increases (retroverted pelvis), SS increases. A high-grade PI allows a bigger angle of PT, but PT may be limited by hip extension. b A smaller PI permits less retroversion, but PT may reach a greater value for SS = 0 (PT = PI) because of less hip extension
For a person, the ability of retroversion is limited by the value of its own PI. Patients with a small PI have a small capacity to compensate for their sagittal imbalance through pelvis retroversion. The limited posterior offset of the sacrum regarding the femoral heads can be observed in lateral radiographs. The same poor ability of compensation seems theoretically to occur in different pathologies when there is a low PI. This is the case of severe kyphosis and of ankylosing spondylitis with low-grade PI. Debarge et al. [13] showed that, in ankylosing spondylitis, when there is low-grade PI, the extension of the hips does not limit the pelvis retroversion and the 0° of SS may be easily reached.
Inversely, an individual with a high value of PI, when in sagittal imbalance, has higher possibilities of retroversion and is able to increase widely the posterior offset between the sacrum and the femoral heads in the sagittal plane. This mechanism may help to restore the position of C7 plumb line behind the femoral heads, as in cases of progressive kyphosis. However, this large retroverted pelvis is limited by hip joint extension, which forbids reaching the maximum allowed PT, with SS equal to 0°. This is the reason why, after reaching maximal retroversion, the spino-pelvic complex performs the next method of balance correction, which is flexing the knees to tilt the femoral shaft. Le Huec et al. [14] reported the importance of the axis of the femoral shaft and the vertical line when imbalance is evaluated before surgical correction. In this situation, PT is equal to the femur angulation angle plus hip extension reserve (4°–6°) (Fig. 3). This position with hip in maximal extension and knees flexed is well known in severe kyphosis, but remains very uncomfortable and non-economical.
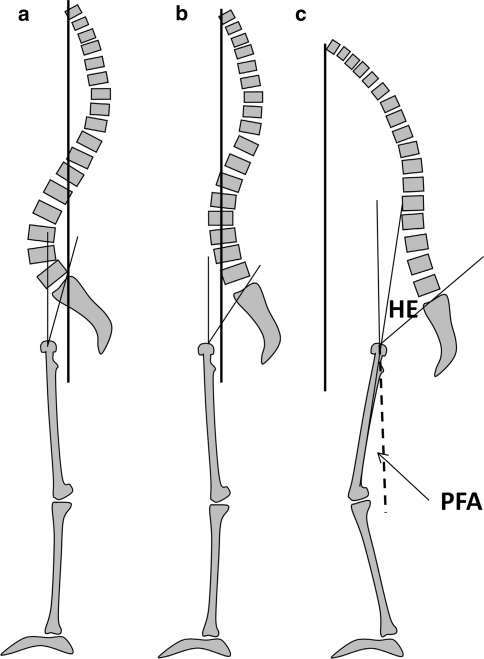
Fig. 3.
Mechanism of compensation of a progressive kyphosis. a Normal situation with a slight pelvis retroversion and C7 PL over the sacral endplate. b With a progressive loss of lordosis, pelvis retroversion permits maintaining C7 PL behind the femoral heads. c In case of severe kyphosis, hip extension (HE) limits the pelvis retroversion. It is compensated by flexion of the knees. C7 PL passes forward to the femoral heads. Due to the tilt of the femoral shaft, PT = PFA + HE
Effect of PI on the shape of lumbar lordosis
The relation between lumbar lordosis and sacral slope was originally demonstrated by Stagnara et al. [4]. The more SS was tilted, the more the lumbar curvature was high (“dynamic back”); contrarily, when SS was rather horizontal, lumbar curvature was flat (“static back”). Several studies presented this strong correlation between SS and the global angle of lordosis [15–17].
Another important observation is that lordosis can be reconstructed into two tangent arcs of circle, with a superior (proximal) one and an inferior (distal) one [18]. The purpose of this division is to better understand the geometry of lordosis. Lumbar lordosis must not be studied as a single curve.
The superior arc of lumbar lordosis is equal to the inferior arc of the thoracic kyphosis, i.e., in the degenerative spine one angle is dependent on the other. Then, for slowly progressive degenerative spine disease, thoracic and lumbar spine geometries are interrelated and must be globally analyzed. For a balanced spine, thoracic kyphosis and lumbar lordosis are intrinsically related and one will depend and “react” according to the other degenerative evolution. Finally, the second and inferior (distal) arc of the lordosis corresponds to the SS, which means that it has substantial importance on the determination of global lordosis. In this way, according to the orientation of SS, we described four types of lumbar lordosis in a population of asymptomatic adult volunteers [8] (Fig. 4):
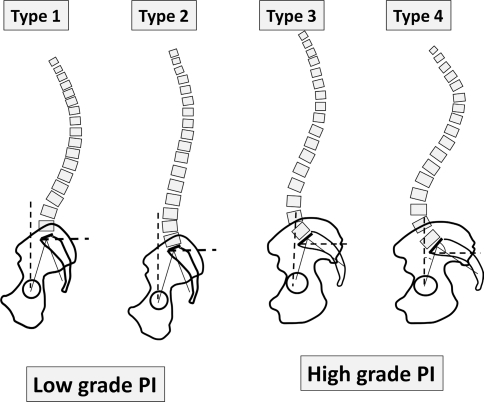
Fig. 4.
The shape of lumbar lordosis depends on SS orientation. Type 1 and 2 have SS < 35°; Type 3 has 35° < SS < 45°; Type 4 has SS > 45°. Generally Type 1 and 2 have a low PI and Type 3 and 4 have a high PI
Low sacral slope (<35°)
Regarding the shape of the distal arch, two constructions are possible:
Type 1 the distal arch is almost absent, the apex is very low, close to L5 and LL is quite constructed by only the proximal arch. LL is short and, therefore, the kyphosis is long, with an extension on the thoraco-lumbar area. In summary, it is a non-harmonious back with thoraco-lumbar kyphosis and short hyperlordosis.
Type 2 the distal arch is low; it is longer but flat, close to a straight line. It is a harmonious flat back.
Mean sacral slope (35° < SS < 45°)
Type 3 LL is well balanced between its two arches. It is a harmonious regular back.
High sacral slope (SS > 45°)
Type 4 the distal arch is highly increased in angle and number of vertebrae; length and curvature of LL increase. It is a harmonious hypercurved back.
Due to the correlation between SS and PI (when PI values are higher, SS also is higher), Type 1 and 2 have generally a low-grade PI; Type 3 and 4 have generally a higher grade of PI.
Assessment of the global spinal balance: C7 positioning
The center of the C7 vertebral body was preferred to T1 as a reference point of the top of the thoraco-lumbar spine because of the readability of C7 on lateral X-rays. The C7 vertebra is employed as a reference in two ways: the C7 plumb line (C7 PL) or the spino-sacral angle (SSA), defined by the angle between the line drawn from C7 to the middle of the sacral plate and the SS line [19] (Fig. 5).
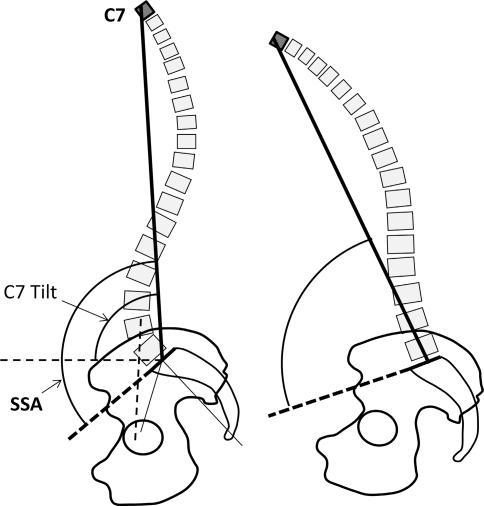
Fig. 5.
Positioning angles of C7; in case of severe kyphosis (right), SSA decreases strongly
The C7 PL is the reflection of the global balance of the spine. Its position in the sagittal plane is analyzed in relation to two anatomical landmarks: the femoral head axis (HA) and the posterior edge of the sacral plate. In a population with a balanced spine, the C7 PL is generally located behind or at the level of the posterior edge of the sacral endplate [19]. If C7 PL locates between HA and the posterior edge of the sacral plate, the system may be considered as slightly unbalanced. When it is forward HA, the system is probably severely unbalanced. Later in this article, it will be presented that the positioning of C7 must be correlated to PT, which is another indicator of balance failure.
The second method of employing C7 vertebra as an indicator of sagittal balance is through SSA, an angle that quantifies the global kyphosis of the whole spine. In a well-balanced spine, SSA remains proportional to SS. In case of kyphosis, or loss of lumbar lordosis, SSA decreases (Fig. 5). In severe kyphosis, SSA decreases strongly. These relations may provide a guide to evaluate the need of correction for the kyphosis.
Orientation of the spine and local stress: the contact force
The lumbar spine may be imagined as the pylon of a crane: in the forward position, the arrow has to support the corresponding body weight, passing by the gravity line. This force may be decreased by the abdominal pressure and stabilized by the abdominal muscles anteriorly. When the lumbar spine moves backward, the posterior muscles have to work to counteract the gravity. The contact force (CF) on the spinal column is the addition of forward forces (gravity, abdominal pressure) and the force of the posterior spine muscles. In case of weight bearing, CF increases tremendously. In case of acute back pain, the contracture of the back muscles increases CF and the discs pressure, acting negatively on the pain. In a classical degenerative situation with loss of lordosis and progressive retroverted pelvis, the gravity line moves forward remaining at the level of the femoral heads; the distance of the anterior arrow increases and in this way CF increases (Fig. 6).
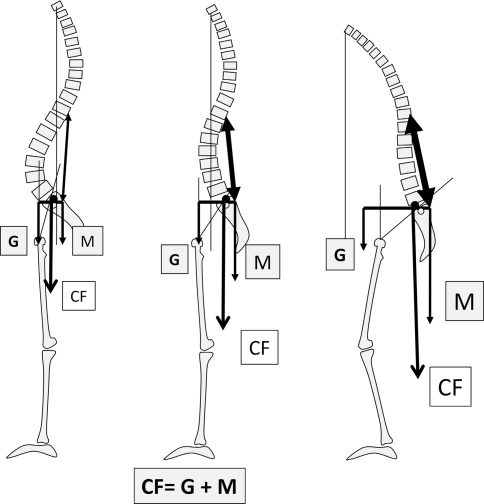
Fig. 6.
Contact force (CF) on the distal lumbar spine is the sum of the gravity force (G) and the force M acting on the posterior muscles to maintain an erect position. The more the system is unbalanced, the more G increases, and the more M has to compensate for increasing CF
When acting on a functional spinal unit, there is a distribution of CF between the intervertebral disc in front and the facet joints behind. The more the lumbar spine is curved, the more is the impact of CF acting on the posterior elements. On the contrary, in case of low curvature or flat back, CF acts mainly on the discs.
At the level of each functional spinal unit and according to its local orientation, CF, which is vertical, may be divided into two resultant forces: one parallel to the vertebral endplate and the other perpendicular to the plate. When the vertebral plate is close to horizontal, as in hypolordosis, the vector perpendicular to the disc increases. In case of a more tilted orientation of the vertebral plate, the resultant of CF parallel to the plate increases, increasing sliding forces (Fig. 7).
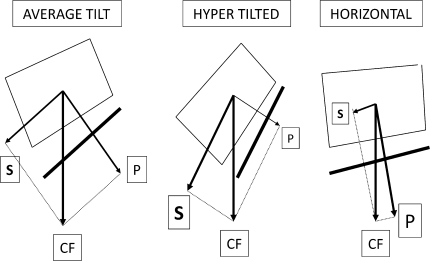
Fig. 7.
Distribution of CF with respect to the local intervertebral tilt. When the tilt increases, the sliding resultant force (S) increases; in case of a horizontal plate orientation, the pressure resultant force (P) increases
When the lumbar spine is hypolordotic and flat, the action of CF is mainly on the anterior column (vertebral bodies and discs) and its distribution favors the resultant force perpendicular to the discs, increasing the disc pressure. On the other hand, if lumbar lordosis is hypercurved, CF acts mainly on the posterior elements (facet joints, spinous processes) and, at the extremities of the curve, the vertebral units are greatly tilted (Fig. 8). The distribution of CF favors the sliding force resultant, increasing the stress on the facets and decreasing the disc pressure. When the tilt is forward, there is a risk of anterolisthesis; if the tilt is posterior, there is a risk of retrolisthesis. If we consider that the mechanical stresses may play a role in degenerative spine progression, hypolordosis may favor degenerative discopathies; inversely, long hyperlordosis may induce posterior facets arthritis, Baastrup disease and listhesis.
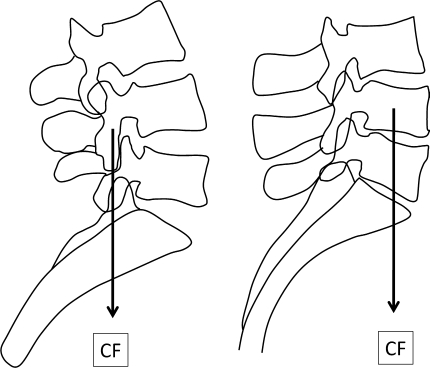
Fig. 8.
CF positioning with respect to the local spine extension. When the spine is in hyperextension (left distal hyperlordosis of a Type 1), CF acts on the posterior arch. If the local lordosis is poor, CF moves forward on the discs and bodies
Biomechanical adaptation of the balance in pathological kyphosis
When the kyphosis occurs acutely, promoting “flexible” deformation on the spine, such as traumatic kyphosis, the compensation is obtained by the “flexible” non-fractured spine below the kyphosis. Generally, there is no compensation at the pelvis level. When the kyphosis is highly located, the lumbar lordosis is able to compensate the balance. When the kyphosis extends into the thoraco-lumbar area, the length of lordosis could be too short to compensate. Compensation is relative to the length of lordosis and the extensibility of the spine.
The flexibility of the lumbar spine is linked to the extension ability. When the lumbar lordosis is greatly curved (Type 4), the posterior arches are thinner as well as the spinous processes. This anatomy allows a better range of motion of the spine, mainly in extension. But the weakness of the posterior arch may induce rupture (spondylolysis) or loosening (degenerative spondylolisthesis). In structural flat back (Type 2 lordosis), the posterior arch is thick and high, as well as the spinous processes, reducing the local ability of extension of the spine (Fig. 9). This could be the cause of a local hyperextension stress in case of compensation of an upper kyphosis. Another similar circumstance occurs when a horizontal pelvis with high PI and SS is associated with a flat rigid lumbar spine.
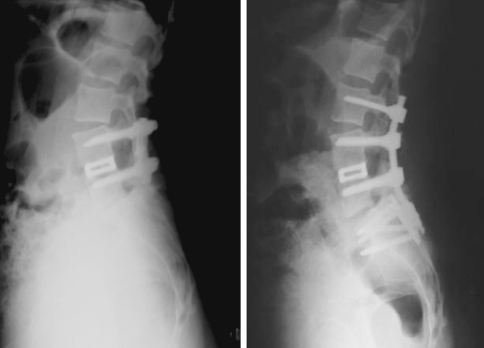
Fig. 9.
Compensation of a local iatrogenic hypolordosis (fusion of L4 L5) by hyperextension of L3 L4 on a flexible spine. Treatment by extension of the fusion to L3 maintaining the segmental hyperextension of L3 L4
When the kyphosis occurs on a rigid spine, such as degenerative spine or ankylosing spondylitis, or in iatrogenic situation such as arthrodesis, the only and very first way of compensation is pelvic tilting, aiming at retroversion. This mechanism increases the horizontal length between the femoral heads and the sacral plate and decreases the SS. Due to the geometrical relation between the PI and the PT, a vertical pelvis with a low PI is less able to compensate for this mechanism than a horizontal pelvis with a high PI.
In case of very severe kyphosis, the flexion of the knees increases the effect of posterior PT and improves the positioning of the head and the gaze direction.
Spino-pelvic assessment in pathology
Which degenerative evolution with which type of spine?
According to the type of spino-pelvic setting, it is possible to suggest the tendency for degenerative evolution and pathological balance [8].
- Type 1 is a combination of kyphosis and hyperextension area:
- In the thoraco-lumbar kyphosis area, there is an increased risk of disc degeneration.
- In the junctional area, between thoraco-lumbar kyphosis and lumbar lordosis, the discs are very tilted with a risk of retrolisthesis.
- In the hyperlordotic area, we see the “kissing” of the spinous processes; there is a risk of facet hyperpressure and L5 spondylolysis by “crack nuts” effect. The discs L4 L5 and L5 S1 are generally protected.
- In case of increasing thoraco-lumbar kyphosis (e.g.,: fracture) the only way to compensate is by increasing the short distal lordosis. Due to a low PI, the range of posterior pelvis tilt is limited. It is mandatory to reduce the thoraco-lumbar kyphosis, if possible, to decrease the hyperlordosis.
Type 2 is the flat back. The orientation of the discs is horizontal; therefore, the disc pressure is maximum. There is an important risk of early disc degeneration with central disc herniation. Barrey showed that the more the patients with disc herniation were young, the more was PI low [15]. The risk of early distal discopathy increases in patients with low PI and flat back. Mechanically, this back is not the one adapted for weight bearing, or sports or activities with high pressure on the back.
A kyphotic evolution at the lumbar level may result in a severe unbalance because of the limitation of pelvis retroversion, but complete retroversion bringing SS to 0° is possible.
Restoration of balance in unbalanced Type 2 is easier because of the small necessary lordosis.
Types 3 and 4 have a bigger lumbar lordosis, mainly Type 4. They are generally associated with a horizontal pelvis with a high-grade PI. The more the increases in PI, the more was SS high, with a risk of spondylolisthesis through L5 isthmic lysis by a “sliding” mechanism.
Due to the big amount of curvature of lumbar lordosis, the stress is mainly posterior on the facet joints. The risk of posterior facet degeneration is significant. A proof of limits of extension is the kissing of the spinous processes. When spinous processes are in contact, the local extension is at its maximum and may be an important cause of pain. Posterior facet arthritis may have different pathological presentations, such as subluxation through the sliding mechanism, osteophytes, synovitis and cyst formation. When the contact between two facets is no more efficient, there is an anterior instability with sliding producing degenerative spondylolisthesis, mainly between L4 and L5 [14, 15].
In aging people, to prevent pain in extension, there is a tendency to decrease lordosis. Progressive degenerative discopathies enhance the loss of lordosis, compensated by an increasing posterior tilt of the pelvis. We may differentiate a true Type 2 with discopathies from a “false” Type 2, resulting in degenerative evolution of a Type 4. The first has a low-grade PI and a small PT, while the second has a high-grade PI and a large PT. Thus, it is important to understand the sagittal spino-pelvic parameters as their knowledge will allow the surgeon to establish the correct surgical strategy regarding the sagittal balance of the spine.
Diagnostic and strategic applications
The only way to assess the global spinal sagittal balance and its eventual consequences is the long-standing lateral X-ray. It is necessary to visualize the whole spine and pelvis, from the skull to the proximal femurs.
A quick diagnosis may be performed on three points:
Pelvic angles: PI, PT and SS
Type of lumbar lordosis
Positioning of C7 PL
Whatever the technique of treatment, the restoration of the sagittal balance is the best way to obtain a good result. In a pathological situation, it is always difficult to recognize how much the present position of the spino-pelvic complex represents its original anatomy and how much it represents its pathological evolution or its functional adaptation (antalgic position, mainly). The only signature of the initial situation is the PI, which remains approximately stable in adult life. When treating a patient with a low-grade PI, it is necessary to restore a Type 1 or 2, without increasing the lordosis. In case of higher PI, the more the PI increases, the more the lumbar lordosis has to be augmented in angle and length, to reduce the posterior tilt of the pelvis.
In case of large PT, hips are forced in extension with an increasing anterior unbalance when walking. This situation may impair a hip arthritis or a total hip prosthesis function due to the more vertical orientation of the acetabulum.
In severe hypolordosis with high-grade PI, a posterior subtraction osteotomy may be used.
Conclusion
Sagittal balance of the spine is not only a matter of positioning the spine over the pelvis. There is a strong correlation in shape and positioning, and form and function, between the pelvis and the spine. The morphology of the pelvis is identified by PI, with consequences on the morphology of the spine. With time, depending of the individual morphology of a person, specific degenerative evolutions may occur. Sagittal parameters may be considered as predictive regarding the respective shape of the spine and pelvis. A better understanding of this relation may lead to improved diagnosis of degenerative spine diseases and a better strategy of treatment.
Conflict of interest
None.
References
- 1.Coppens Y (2010) Estamos em Pé há 10 Milhões de Anos. In: Pinheiro-Franco JL, Vaccaro AR, Benzel EC, Mayer H-M (eds) Conceitos Avançados em Doença Degenerativa Discal Lombar. DiLivros Publisher, Rio de Janeiro, pp 1–11 (in Portuguese)
- 2.Senut B, Devillers M (2008) Et le singe se mit debout. Editions Albin Michel, pp 157–165 (in French)
- 3.Pinheiro-Franco JL, Roussouly P, Vaccaro AR (2010) Importância do Equilíbrio Sagital no Tratamento Cirúrgico da Doença Degenerativa Discal Lombar. In: Pinheiro-Franco JL, Vaccaro AR, Benzel EC, Mayer H-M (eds) Conceitos Avançados em Doença Degenerativa Discal Lombar. DiLivros Publisher, Rio de Janeiro, pp 277–286 (in Portuguese)
- 4.Stagnara P, Mauroy JC, Dran G, Gonon G, Costanzo G, Dimnet J, Pasquet A. Reciprocal angulation of vertebral bodies in a sagittal plane: approach to references for the evaluation of kyphosis and lordosis. Spine (Phila Pa 1976) 1982;7(4):335–342. doi: 10.1097/00007632-198207000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Duval-Beaupère G, Schmidt C, Cosson P. A Barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng. 1992;20:451–462. doi: 10.1007/BF02368136. [DOI] [PubMed] [Google Scholar]
- 6.Duval-Beaupère G, Legaye J. Composante sagittale de la statique rachidienne. Rev Rhum. 2004;71:105–119. doi: 10.1016/j.rhum.2003.09.018. [DOI] [Google Scholar]
- 7.Boulay C, Tardieu C, Hecquet J, Benaim C, Mouilleseaux B, Marty C, Prat-Pradal D, Legaye J, Duval-Beaupère G, Pélissier J. Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J. 2006;15(4):415–422. doi: 10.1007/s00586-005-0984-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roussouly P, Berthonnaud E, Dimnet J. Geometrical and mechanical analysis of lumbar lordosis in an asymptomatic population: proposed classification. Rev Chir Orthop Reparatrice Appar Mot. 2003;89(7):632–639. [PubMed] [Google Scholar]
- 9.Jackson RP, Kanemura T, Kawakami N, Hales C. Lumbopelvic lordosis and pelvic balance on repeated standing lateral radiographs of adult volunteers and untreated patients with constant low back pain. Spine. 2000;25(5):575–586. doi: 10.1097/00007632-200003010-00008. [DOI] [PubMed] [Google Scholar]
- 10.Roussouly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976) 2005;30(3):346–353. doi: 10.1097/01.brs.0000152379.54463.65. [DOI] [PubMed] [Google Scholar]
- 11.Labelle H, Roussouly P, Berthonnaud E, Transfeldt E, O’Brien M, Chopin D, Hresko T, Dimnet J. Spondylolisthesis, pelvic incidence, and spinopelvic balance: a correlation study. Spine (Phila Pa 1976) 2004;29(18):2049–2054. doi: 10.1097/01.brs.0000138279.53439.cc. [DOI] [PubMed] [Google Scholar]
- 12.Mac-Thiong JM, Roussouly P, Berthonnaud E, Guigui P. Sagittal parameters of global spinal balance: normative values from a prospective cohort of seven hundred nine Caucasian asymptomatic adults. Spine (Phila Pa 1976) 2010;35(22):E1193–E1198. doi: 10.1097/BRS.0b013e3181e50808. [DOI] [PubMed] [Google Scholar]
- 13.Debarge R, Demey G, Roussouly P. Radiological analysis of ankylosing spondylitis patients with severe kyphosis before and after pedicle subtraction osteotomy. Eur Spine J. 2010;19(1):65–70. doi: 10.1007/s00586-009-1158-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Le Huec JC, Leijssen P, Duarte M, Aunoble S (2011) Thoracolumbar imbalance analysis for osteotomy planification using a new method: FBI technique. Eur Spine J (in press) [DOI] [PMC free article] [PubMed]
- 15.Barrey C (2004) Equilibre sagittal pelvi-rachidien et pathologies lombaires dégénératives. Etude comparative à propos de 100 cas. Thèse Doctorat, Université Claude-Bernard, Lyon 1 (in French)
- 16.Barrey C, Jund J, Noseda O, Roussouly P. Sagittal balance of the pelvis–spine complex and lumbar degenerative diseases. A comparative study of about 85 cases. Eur Spine J. 2007;16(9):1459–1467. doi: 10.1007/s00586-006-0294-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jang JS, Lee SH, Min JH, Maeng DH. Changes in sagittal alignment after restoration of lower lumbar lordosis in patients with degenerative flat back syndrome. J Neurosurg Spine. 2007;7(4):387–392. doi: 10.3171/SPI-07/10/387. [DOI] [PubMed] [Google Scholar]
- 18.Berthonnaud E, Dimnet J, Roussouly P, Labelle H. Analysis of the sagittal balance of the spine and pelvis using shape and orientation parameters. J Spinal Disord Tech. 2005;18(1):40–47. doi: 10.1097/01.bsd.0000117542.88865.77. [DOI] [PubMed] [Google Scholar]
- 19.Roussouly P, Gollogly S, Noseda O, Berthonnaud E, Dimnet J. The vertical projection of the sum of the ground reactive forces of a standing patient is not the same as the C7 plumb line: a radiographic study of the sagittal alignment of 153 asymptomatic volunteers. Spine (Phila Pa 1976) 2006;31(11):E320–E325. doi: 10.1097/01.brs.0000218263.58642.ff. [DOI] [PubMed] [Google Scholar]