Abstract
Introduction
Many studies suggest the importance of the sagittal sacropelvic balance and morphology in spinal and hip disorders. This study describes the normal age- and sex-related changes in sacropelvic morphology and balance in a prospective cohort of asymptomatic adults without spinal disorder.
Materials and methods
A prospective cohort of 709 asymptomatic adults without spinal pathology was recruited. There were 354 males and 355 females aged 37.9 ± 14.7 and 35.7 ± 13.9 years, respectively. For each subjects, pelvic incidence (PI), pelvic tilt (PT), and sacral slope (SS) were measured from standing lateral radiographs. Ratios of SS to PI (SS/PI), PT to PI (PT/PI), and PT to SS (PT/SS) were also calculated.
Results
There was no significant difference in PI (pelvic incidence), SS (sacral slope), PT (pelvic tilt), PT/PI, SS/PI, or PT/SS between males and females. The mean ± 2 standard deviations (SD) range was 32°–74°, 0°–27°, and 24°–55° for PI, PT and SS, respectively. The mean ± 2 SD range was greater than 0.5 for SS/PI and less than 0.5 for PT/PI. PI was not related to age in either sex group. PT, SS, PT/PI, SS/PI, and PT/SS presented only weak correlation coefficients (r ≤ 0.21) with respect to age.
Conclusion
The current study presents the largest cohort of asymptomatic adults in the literature dedicated to the evaluation of sagittal sacropelvic morphology and balance. The range of values corresponding to the mean ± 2 SD can provide invaluable information to clinicians about the normal range of values expected in 95% of the normal population.
Keywords: Pelvis, Sacropelvic morphology, Sacropelvic balance, Sacrum, Sagittal balance
Introduction
Because of its close relationship with the spine, many studies have investigated the influence of sacropelvic balance and morphology in the evaluation and treatment of spinal disorders, such as developmental spondylolisthesis [1–12], degenerative spondylolisthesis [13, 14], adolescent idiopathic scoliosis [15–17], and adult spinal deformity [18–20]. Some authors have also raised the role of sacropelvic morphology and balance in the pathogenesis and surgical treatment of hip osteoarthritis [21–24]. As a basis for comparison, it is therefore important to document the sacropelvic balance and morphology in the normal population. So far, normal values of sacropelvic parameters have been published for pediatric [25], adult [26–30], and elderly subjects [31].
Boulay et al. [26] and Janssen et al. [28] did not find any significant difference in sacral slope (SS), pelvic tilt (PT), or pelvic incidence (PI) when comparing asymptomatic adult females with males. On the contrary, Vialle et al. [30] found statistically significant differences in SS and PI––but not PT––between 110 females and 190 males. However, the mean differences (3° or less) were marginal when considering the potential measurement errors. They also observed a weak statistical relationship between age and PI (r = 0.14), which is not likely to be clinically significant. The SS and PT were not related to age. Hammerberg and Wood [31] evaluated 50 asymptomatic subjects aged 70–85 years, and did not find any relationship between increasing age and sacropelvic parameters of balance and morphology, but they suggest that the mean PT and PI in their study were higher than those observed previously in younger adult populations.
As there is still some debate concerning the relationships between sacropelvic parameters and sex or age after the end of growth, the current study specifically describes the age- and sex-related changes in sacropelvic morphology and balance in 709 asymptomatic adults without spinal pathology that represent the largest cohort in the literature related to the evaluation of sagittal sacropelvic parameters.
Methods
A prospective cohort of 709 asymptomatic adults without spinal pathology was recruited from January 1st 2000 to December 31st 2008. The study has been approved by the Institutional Review Board of each participating institution. Volunteers were eligible to participate in the study based on the following inclusion criteria: (1) age of 18 years or older, (2) absence of spinal pathology confirmed after evaluation by an orthopedic surgeon, (3) no history of spine, hip, or pelvic disorder, and (4) no contraindication for radiographic exposure (e.g., pregnancy, tumor). All participants were white Caucasians with a mean age of 36.8 ± 14.3 years (range: 18–81). There were 354 males and 355 females aged 37.9 ± 14.7 years (range: 18–81) and 35.7 ± 13.9 years (range: 18–76), respectively.
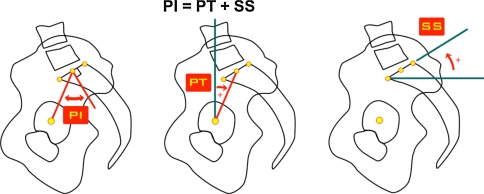
The radiographic protocol was standardized for all participating institutions. For each subject, a standing left lateral radiograph including the spine and pelvis was obtained with a long 36-in cassette placed at 72-in from the X-ray tube. Subjects were instructed to stand in a comfortable position with the hips and knees fully extended. For the two main institutions located in France, hands were positioned on a support, while in North American centers the fist-on-clavicle position was adopted. Plain films were scanned using a VXR8 film scanner (View-Tec, France) in jpg format at 75 dpi when the radiographs were not acquired in digital format. Parameters of sacropelvic balance and morphology (Fig. 1) were then measured by a single observer with the Optispine software (Optispine, France), that has been presented in detail in previous studies of sagittal spinal alignment [32, 33]. The pelvic incidence (PI) was measured in order to assess sacropelvic morphology. It is defined as the angle subtended by the line drawn from the hip axis (center of the line connecting the center of each femoral heads) to the midpoint of the upper sacral endplate and the line perpendicular to the upper sacral endplate. The sacropelvic balance was assessed from the pelvic tilt (PT) and the sacral slope (SS). The PT is defined as the angle subtended by the vertical line and the line drawn from the hip axis to the midpoint of the upper sacral endplate, while the SS is defined as the angle subtended by the horizontal line and the upper sacral endplate. In order to evaluate the relationships between parameters of sacropelvic balance and morphology, the ratios of SS to PI (SS/PI), PT to PI (PT/PI), and PT to SS (PT/SS) were also calculated.
Fig. 1.
Sacropelvic parameters: pelvic incidence (PI), pelvic tilt (PT), and sacral slope (SS)
The data was analyzed using the SPSS 14.0 software (SPSS Inc., Chicago, IL, USA). Descriptive statistics (mean and standard deviation) were provided for all subjects, as well as separately for males and females. In addition, the range of values comprising 95% of the asymptomatic population was estimated from the mean ± 2 SD (standard deviations). The Lilliefors test, which is an adaptation of the Kolmogorov–Smirnov test, was used to assess if the measured sacropelvic parameters (PI, PT and SS) were normally distributed in the female and male cohorts. Comparisons between males and females were performed using bilateral independent Student’s t tests. The relationships between all parameters and with age were assessed using Pearson’s coefficients. In accordance with suggestions from Cohen [34], statistically significant correlation coefficients were considered clinically large if >0.5, moderate if >0.3, and small if >0.1. Two different levels of significance (0.01 and 0.05) were used for the statistical analyses.
Results
The values of PI, PT, and SS are normally distributed in both female and male cohorts. Descriptive statistics for all parameters and comparisons based on sex are presented in Table 1. In particular, Table 1 shows the value ranges that are expected in 95% of the asymptomatic population. There is no significant difference in PI, SS, or PT between males and females, as the mean values varied by <0.5°. PT shows the smallest standard deviation of the three measured parameters, and the results suggest that it is normally positive. The calculated ratios (PT/PI, SS/PI, PT/SS) are not influenced by sex. Of the three ratios, SS/PI seems to be the most stable with the smallest standard deviation and it is normally >0.5, indicating that the SS value is normally at least half of the PI. As for PT/PI, the results show that it is normally positive but <0.5.
Table 1.
Mean and standard deviation [mean ± 2 standard deviations] of sagittal sacropelvic parameters of balance and morphology
| Parameter | All (n = 709) | Females (n = 355) | Males (n = 354) | P value |
|---|---|---|---|---|
| Pelvic incidence (°) | 52.6 ± 10.4 [31.7;73.5] | 52.4 ± 10.8 [30.7;74.1] | 52.7 ± 10.0 [32.7;72.8] | 0.7 |
| Pelvic tilt (°) | 13.0 ± 6.8 [−0.6;26.7] | 12.7 ± 7.0 [−1.3;26.6] | 13.4 ± 6.7 [0.1;26.7] | 0.1 |
| Sacral slope (°) | 39.6 ± 7.9 [23.7;55.4] | 39.8 ± 7.9 [24.0;55.5] | 39.3 ± 8.0 [23.4;55.3] | 0.5 |
| PT/PI | 0.24 ± 0.11 [0.01;0.47] | 0.23 ± 0.11 [0.005;0.46] | 0.25 ± 0.11 [0.02;0.47] | 0.06 |
| SS/PI | 0.76 ± 0.11 [0.53;0.99] | 0.77 ± 0.11 [0.54;1.0] | 0.75 ± 0.11 [0.53;0.98] | 0.06 |
| PT/SS | 0.35 ± 0.21 [−0.07;0.76] | 0.33 ± 0.21 [−0.09;0.75] | 0.36 ± 0.20 [−0.05;0.77] | 0.08 |
P values from the comparison of parameters between males and females are also reported
Results from the correlation analysis are presented in Tables 2 and 3. PI is not related to age in either sex group. On the opposite, PT and SS present small correlation coefficients with respect to age, indicating a tendency for PT and SS to increase and decrease with age, respectively. Similarly, PT/PI and SS/PI tend to increase and decrease with age, respectively. Finally, PT/SS tend to increase with age, again reflecting the tendency of PT to increase and SS to decrease with age. Based on the criteria of Cohen [34], all statistically significant correlations with age are small clinically.
Table 2.
Correlation coefficients between sacropelvic parameters
| Parameter | All (n = 709) | Females (n = 355) | Males (n = 354) |
|---|---|---|---|
| Pelvic incidence–pelvic tilt | 0.65* | 0.69* | 0.61* |
| Pelvic incidence–sacral slope | 0.76* | 0.77* | 0.75* |
| Pelvic tilt–sacral slope | −0.002 | 0.07 | −0.07 |
* Statistically significant correlation coefficient (p < 0.01)
Table 3.
Correlation coefficients between sacropelvic parameters and age
| Parameter | All (n = 709) | Females (n = 355) | Males (n = 354) |
|---|---|---|---|
| Pelvic incidence | 0.03 | 0.06 | 0.005 |
| Pelvic tilt | 0.16* | 0.17* | 0.14* |
| Sacral slope | −0.10* | −0.08 | −0.11† |
| PT/PI | 0.19* | 0.19* | 0.18* |
| SS/PI | −0.19* | −0.19* | −0.18* |
| PT/SS | 0.21* | 0.20* | 0.21* |
†Statistically significant correlation coefficient (p < 0.05)
* Statistically significant correlation coefficient (p < 0.01)
The relationships between PI, PT, and SS are similar between males and females. The statistically significant correlations between PI and PT, as well as between PI and SS are clinically large, based on the criteria proposed by Cohen [34].
Discussion
The current study presents the largest cohort of asymptomatic adults without spinal pathology in the literature dedicated to the evaluation of sagittal sacropelvic morphology and balance. The reported results constitute a strong database that can be used as a comparison for subjects with spinal or hip pathologies, as many clinicians now recognized that assessment of sacropelvic balance and morphology is important in the evaluation and treatment of various spinal and hip disorders. In particular, the range of values provided in Table 1 corresponding to the mean ± 2 SD provides invaluable information to clinicians about the normal range of values expected in 95% of the normal population. In normal adults, PI, PT, and SS are expected to fall between 32° and 74°, between 0° and 27°, and between 24° and 55°, respectively. In addition, PT/PI should be less to 0.5 and SS/PI >0.5. Values outside those ranges could potentially predispose to the development of spinal pathology.
In children and adolescents, PI, PT, and SS are similar between boys and girls [25]. Also, sagittal sacropelvic morphology as measured by the PI tends to change slightly during growth and results in a proportionally slight increase in PT in the presence of a stable SS. In adults, previous reports [26, 28, 30, 31] including smaller cohorts have provided conflicting results concerning the sex- and age-related changes in PI, PT, and SS. However, in accordance with those previous reports, the current study confirms that the influence of age and sex on sagittal sacropelvic morphology and orientation is at most modest (Tables 1, 2, 3). More specifically, PI, PT, and SS are similar between adult males and females. Regarding the ratios between the parameters (PT/PI, SS/PI, PT/SS), the values are not dependent on sex, suggesting that the underlying mechanisms used to control sacropelvic balance (PT and SS) are similar between normal adult males and females.
However, it has to be underlined that previous anthropometric studies [35–39] have shown that there are sex differences in the human pelvis. In the current study, only two parameters of sacropelvic balance and one parameter of sacropelvic morphology are measured from the lateral radiographs. The authors have preferred to limit their analysis to those parameters that are most commonly used by clinicians when evaluating the sagittal sacropelvic balance and morphology in the presence of spinal pathology. It is possible that the measurement of additional parameters could have provided statistically significant differences between males and females, especially for those parameters that could potentially be related to female adaptations for childbearing and delivery. It would also be interesting to assess if PI could be related to dystocia, as it remains unknown if the overall size of the pelvis is related to the PI.
Also of particular significance is the range of values for PT/PI and SS/PI (Table 1), indicating that normally the PT is less than half the value of PI, while the SS is more than half the value of PI. These two specific features of a normal sagittal posture are very important to assess because they can help to detect early compensation from the pelvis—increasing pelvic retroversion with sacral verticalization—in the context of spinal pathology, such as that often found in spondylolisthesis [1, 4] or global sagittal spinal imbalance [18].
With increasing age during adulthood, PI remained stable, as opposed to pediatric subjects [25]. This suggests that, not only does the growth of the pelvis in the sagittal plane between the femoral heads and the upper sacral endplate ceases during adulthood, but also that normal degenerative changes to the hips, sacrum and sacro-iliac joints do not significantly influence the PI. On the opposite, PT and SS, respectively, increased and decreased slightly with aging, indicating an increased retroversion of the pelvis presumably to compensate for degenerative processes (bone and soft tissues) occurring in the spine that tend to decrease the lumbar lordosis and induce a positive spinal balance (forward displacement of the spine) with increasing age, as observed in previous studies [31, 40]. However, changes in PT and SS with age are minor in normal individuals, and therefore an important increase in PT and/or decrease in SS should alert the clinician about the possible presence of underlying spine pathology.
The small increase in PT/PI and PT/SS, as well as the small decrease in SS/PI with advancing age are in agreement with the behavior of PT and SS. Of note, the magnitude of the correlation coefficient is equal but of opposite sign for PT/PI and SS/PI because PT and SS are inversely related due to the mathematical relationship between PT, SS, and PI (PI = PT + SS). In other words, for a given PI, when PT increases SS decreases proportionally and vice versa. This mathematical relationship is very important because it implies that PI depends on both PT and SS. Conversely, it would be impossible and incorrect to attempt predicting PT and/or SS based on PI alone, despite the strong relationships found between PI and PT as well as between PI and SS.
There are two main limitations related to the current study. The first limitation refers to the cross-sectional nature of the study for assessing the influence of age on sacropelvic parameters. A longitudinal study on asymptomatic adults would be preferable and follow-up evaluation of the present cohort is considered. The second limitation is related to the radiographic acquisition. Although we attempted to standardize the radiographic protocol, the exact technique differed between participating centers. In particular, the position of the arms varied in some centers. While most subjects adopted a position with flexed shoulder and hand supports, which is recommended by the recent literature [41], a minority of the subjects were positioned in the fist-on-clavicle position. In addition to the fact that most of the subjects adopted the same arm position, two additional factors tend to minimize the errors associated with the radiographic acquisition. First, only angular parameters (as opposed to distances) were measured in this study, thereby reducing the magnification-related errors. Second, sacropelvic parameters are less likely than spinal parameters to be influenced by the arm position which are distant from the pelvis.
Conclusion
The current study presents the largest cohort of asymptomatic adults without spinal pathology in the literature dedicated to the evaluation of sagittal sacropelvic morphology and balance. The range of values of PI, PT, and SS corresponding to the mean ± 2 SD can provide invaluable information to clinicians about the normal range of values expected in 95% of the normal population. In addition, the presence of PT/PI >0.5 and SS/PI <0.5 could help to identify patients potentially predisposed to developing spinal pathology. PI, PT, and SS were similar between males and females in this study, although it would be interesting to assess whether other sacropelvic parameters are influenced by gender. PI was not related to age, while the correlations between parameters of sacropelvic balance (PT, SS, PT/PI, SS/PI) and age were small.
Acknowledgments
Conflict of interest None.
References
- 1.Hresko MT, Labelle H, Roussouly P, et al. Classification of high-grade spondylolisthesis based on pelvic version and spine balance: possible rationale for reduction. Spine. 2007;32:2208–2213. doi: 10.1097/BRS.0b013e31814b2cee. [DOI] [PubMed] [Google Scholar]
- 2.Jackson RP, Phipps T, Hales C, et al. Pelvic lordosis and alignment in spondylolisthesis. Spine. 2003;28:151–160. doi: 10.1097/00007632-200301150-00011. [DOI] [PubMed] [Google Scholar]
- 3.Labelle H, Roussouly P, Berthonnaud É, et al. Spondylolisthesis, pelvic incidence, and spinopelvic balance. A correlation study. Spine. 2004;29:2049–2954. doi: 10.1097/01.brs.0000138279.53439.cc. [DOI] [PubMed] [Google Scholar]
- 4.Labelle H, Roussouly P, Chopin D, et al. Spino-pelvic alignment after surgical correction for developmental spondylolisthesis. Eur Spine J. 2008;17:1170–1176. doi: 10.1007/s00586-008-0713-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mac-Thiong J-M, Wang Z, Guise JA, et al. Postural model of sagittal spino-pelvic balance and its relevance for lumbosacral developmental spondylolisthesis. Spine. 2008;33:2316–2325. doi: 10.1097/BRS.0b013e318186b236. [DOI] [PubMed] [Google Scholar]
- 6.Mac-Thiong J-M, Labelle H, Parent S, et al. Reliability and development of a new classification of lumbosacral spondylolisthesis. Scoliosis. 2008;3:19. doi: 10.1186/1748-7161-3-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marty C, Boisaubert B, Descamps H, et al. The sagittal anatomy of the sacrum among young adults, infants, and spondylolisthesis patients. Eur Spine J. 2002;11:119–125. doi: 10.1007/s00586-001-0349-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rajnics P, Templier A, Skalli W, et al. The association of sagittal spinal and pelvic parameters in asymptomatic persons and patients with isthmic spondylolisthesis. J Spinal Disord. 2002;15:24–30. doi: 10.1097/00024720-200202000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Roussouly P, Gollogly S, Berthonnaud É, et al. Sagittal alignment of the spine and pelvis in the presence of L5–S1 isthmic lysis and low-grade spondylolisthesis. Spine. 2006;31:2484–2490. doi: 10.1097/01.brs.0000239155.37261.69. [DOI] [PubMed] [Google Scholar]
- 10.Vialle R, Ilharreborde B, Dauzac C, et al. Is there a sagittal imbalance of the spine in isthmic spondylolisthesis? A correlation study. Eur Spine J. 2007;16:1641–1649. doi: 10.1007/s00586-007-0348-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang Z, Parent S, Mac-Thiong J-M, et al. Influence of sacropelvic morphology in developmental spondylolisthesis. Spine. 2008;33:2185–2191. doi: 10.1097/BRS.0b013e3181857f70. [DOI] [PubMed] [Google Scholar]
- 12.Whitesides TE, Jr, Horton WC, Hutton WC, et al. Spondylotic spondylolisthesis. A study of pelvic and lumbosacral parameters of possible etiologic effect in two genetically and geographically distinct groups with high occurrence. Spine. 2005;30(6S):S12–S21. doi: 10.1097/01.brs.0000155574.33693.60. [DOI] [PubMed] [Google Scholar]
- 13.Barrey C, Jund J, Perrin G, et al. Spinopelvic alignment of patients with degenerative spondylolisthesis. Neurosurgery. 2007;61:981–986. doi: 10.1227/01.neu.0000303194.02921.30. [DOI] [PubMed] [Google Scholar]
- 14.Morel E, Ilharreborde B, Lenoir T, et al. Sagittal balance of the spine and degenerative spondylolisthesis [French] Rev Chir Orthop Reparatrice Appar Mot. 2005;91:615–626. doi: 10.1016/s0035-1040(05)84465-4. [DOI] [PubMed] [Google Scholar]
- 15.Mac-Thiong J-M, Labelle H, Charlebois M, et al. Sagittal plane analysis of the spine and pelvis in adolescent idiopathic scoliosis according to the coronal curve type. Spine. 2003;28:1404–1409. doi: 10.1097/01.BRS.0000067118.60199.D1. [DOI] [PubMed] [Google Scholar]
- 16.Tanguay F, Mac-Thiong J-M, Guise JA, et al. Relation between the sagittal pelvic and lumbar spine geometries following surgical correction of adolescent idiopathic scoliosis. Eur Spine J. 2007;16:531–536. doi: 10.1007/s00586-006-0238-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Upasani V, Tis J, Bastrom T, et al. Analysis of sagittal alignment in thoracic and thoracolumbar curves in adolescent idiopathic scoliosis. How do these two curve types differ? Spine. 2007;32:1355–1359. doi: 10.1097/BRS.0b013e318059321d. [DOI] [PubMed] [Google Scholar]
- 18.Gottfried ON, Daubs MD, Patel AA et al (2009) Spinopelvic parameters in postfusion flatback deformity patients. Spine J 9:639–647 [DOI] [PubMed]
- 19.Kim YJ, Bridwell KH, Lenke LG, et al. An analysis of sagittal spinal alignment following long adult lumbar instrumentation and fusion to L5 or S1: can we predict ideal lumbar lordosis? Spine. 2006;31:2343–2352. doi: 10.1097/01.brs.0000238970.67552.f5. [DOI] [PubMed] [Google Scholar]
- 20.Rose PS, Bridwell KH, Lenke LG, et al. Role of pelvic incidence, thoracic kyphosis, and patient factors on sagittal plane correction following pedicle substraction osteotomy. Spine. 2009;34:785–791. doi: 10.1097/BRS.0b013e31819d0c86. [DOI] [PubMed] [Google Scholar]
- 21.Thomasson E, Guingand O, Terracher R, et al. Role of sagittal spinal curvature in early dislocation after revision total hip arthroplasty: prospective analysis of 49 revision procedures [French] Rev Chir Orthop Reparatrice Appar Mot. 2004;90:226–231. doi: 10.1016/s0035-1040(04)70098-7. [DOI] [PubMed] [Google Scholar]
- 22.Lazennec JY, Riwan A, Gravez F, et al. Hip spine relationships: application to total hip arthroplasty. Hip Int. 2007;17:91–104. [PubMed] [Google Scholar]
- 23.Tardieu C, Hecquet J, Boulay C, et al. Two key describers of the sacro-acetabular relationships: the angles of sacral and acetabular incidence (French) Rev Chir Orthop Reparatrice Appar Mot. 2008;94:327–335. doi: 10.1016/j.rco.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 24.Yoshimoto H, Sato S, Masuda T, et al. Spinopelvic alignement in patients with osteoarthrosis of the hip. A radiographic comparison to patients with low back pain. Spine. 2005;30:1650–1657. doi: 10.1097/01.brs.0000169446.69758.fa. [DOI] [PubMed] [Google Scholar]
- 25.Mac-Thiong J-M, Labelle H, Berthonnaud É, et al. Sagittal spinopelvic balance in normal children and adolescents. Eur Spine J. 2007;16:227–234. doi: 10.1007/s00586-005-0013-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Boulay C, Tardieu C, Hecquet J, et al. Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J. 2006;15:415–422. doi: 10.1007/s00586-005-0984-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Berthonnaud É, Dimnet J, Roussouly P, et al. Analysis of the sagittal balance of the spine and pelvis using shape and orientation parameters. J Spinal Disord Tech. 2005;18:40–47. doi: 10.1097/01.bsd.0000117542.88865.77. [DOI] [PubMed] [Google Scholar]
- 28.Janssen MMA, Drevelle X, Humbert L, et al. Differences in male and female spino-pelvic alignment in asymptomatic young adults. Spine. 2009;34:E826–E832. doi: 10.1097/BRS.0b013e3181a9fd85. [DOI] [PubMed] [Google Scholar]
- 29.Kuntz C, Levin LS, Ondra SL, et al. Neutral upright sagittal spinal alignment from the occiput to the pelvis in asymptomatic adults: a review and resynthesis of the literature. J Neurosurg Spine. 2007;6:104–112. doi: 10.3171/spi.2007.6.2.104. [DOI] [PubMed] [Google Scholar]
- 30.Vialle R, Levassor N, Rillardon L, et al. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Joint Surg Am. 2005;87:260–267. doi: 10.2106/JBJS.D.02043. [DOI] [PubMed] [Google Scholar]
- 31.Hammerberg EM, Wood KB. Sagittal profile of the elderly. J Spinal Disord. 2003;16:44–50. doi: 10.1097/00024720-200302000-00008. [DOI] [PubMed] [Google Scholar]
- 32.Berthonaud E, Labelle H, Roussouly P, et al. A variability study of computerized sagittal spinopelvic radiologic measurements of trunk balance. J Spinal Disord Tech. 2005;18:66–71. doi: 10.1097/01.bsd.0000128345.32521.43. [DOI] [PubMed] [Google Scholar]
- 33.Vaz G, Roussouly P, Berthonnaud E, et al. Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J. 2002;11:80–88. doi: 10.1007/s005860000224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cohen J. Statistical power analysis for the behavioural sciences. 2. Hillsdale, New Jersey: Lawrence Erlbaum Associates; (1988). pp. 100–110. [Google Scholar]
- 35.Albanese J. A metric method for sex determination using the hipbone and the femur. J Forensic Sci. 2003;48:263–273. [PubMed] [Google Scholar]
- 36.Bruzek J. A method for visual determination of sex, using the human hip bone. Am J Phys Anthropol. 2002;117:157–168. doi: 10.1002/ajpa.10012. [DOI] [PubMed] [Google Scholar]
- 37.Igbigbi P, Nanono-Igbigbi AM. Determination of sex and race from the subpubic angle in Ugandan subjects. Am J Forensic Med Pathol. 2003;24:168–172. doi: 10.1097/01.paf.0000065149.42423.85. [DOI] [PubMed] [Google Scholar]
- 38.McBride DG, Dietz MJ, Vennemeyer MT, et al. Bootstrap methods for sex determination from the os coxae using the ID3 algorithm. J Forensic Sci. 2001;46:427–431. [PubMed] [Google Scholar]
- 39.Patriquin ML, Steyn M, Loth SR. Metric analysis of sex differences in South African black and white pelves. Forensic Sci Int. 2005;147:119–127. doi: 10.1016/j.forsciint.2004.09.074. [DOI] [PubMed] [Google Scholar]
- 40.Gelb D, Lenke LG, Bridwell KH, Blanke K, McEnery KW. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine. 1995;20:1351–1358. [PubMed] [Google Scholar]