Abstract
Nowadays, conventional or digitalized teleradiography remains the most commonly used tool for the study of the sagittal balance, sometimes with secondary digitalization. The irradiation given by this technique is important and the photographic results are often poor. Some radiographic tables allow the realization of digitalized spinal radiographs by simultaneous translation of X-ray tube and receptor. EOS system is a new, very low dose system which gives good quality images, permits a simultaneous acquisition of upright frontal and sagittal views, is able to cover in the same time the spine and the lower limbs and study the axial plane on 3D envelope reconstructions. In the future, this low dose system should take a great place in the study of the pelvispinal balance. On the lateral view, several pelvic (incidence, pelvic tilt, sacral slope) and spinal (lumbar lordosis, thoracic kyphosis, Th9 sagittal offset, C7 plumb line) parameters are drawn to define the pelvispinal balance. All are interdependent. Pelvic incidence is an individual anatomic characteristic that corresponds to the “thickness” of the pelvis and governs the spinal balance. Pelvis and spine, in a harmonious whole, can be compared to an accordion, more or less compressed or stretched.
Keywords: Spine, Sagittal balance, Teleradiography, Digitalized spinal radiographs, Kyphosis, Lordosis, Posture, Sagittal balance
Introduction
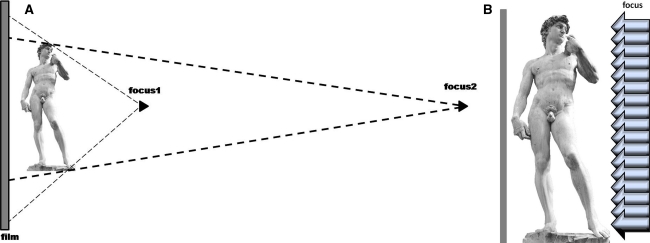
Spine and pelvis shape analysis requires X-ray analysis because the external aspect of the human body is not a good predictor of the spine and pelvis morphology. Except some seldom used techniques (Moiré bands) [1] that are still useful in scoliosis follow up treatment with braces, radiography is the gold standard. This technique for the exploration of the spinopelvic balance has two important disadvantages: a distortion of the studied structures, due to the divergence of the X-rays emitted from a punctual focus and a non-negligible irradiation considering the size of the X-rayed regions (whole spine, pelvis, indeed lower limbs). To the best of our knowledge, only two physical processes can limit the deformation of the spinal structures: move the X-ray source away from the patient to reduce the divergence of the beam and therefore the parallax effect (teleradiography) (Fig. 1a), or give at the focus, coupled to the receptor, a movement of translation to cover all the areas to explore (Fig. 1b).
Fig. 1.
a conventional radiography (focus1): major distortion of the image, Teleradiography (focus 2): less significant distortion. b translation of the focus and the receptor: few vertical distortion of the image
These two techniques are used in actual imaging of spinopelvic balance: Conventional or digitalized teleradiography
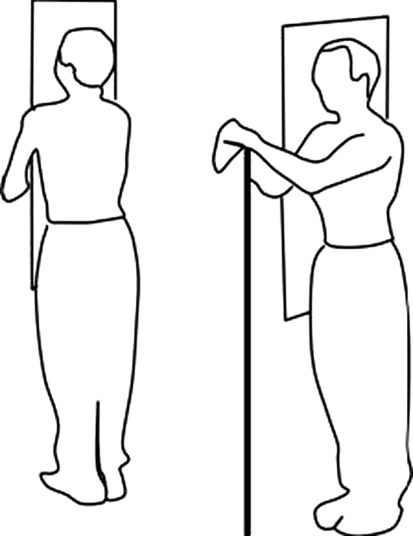
It is still widely utilized technique. A 30 × 90 cm vertical cassette is used. The distance from the radiographic source to the film should be about 2.5 m or, if possible, more. It is advisable to use digressive screens and an attenuation filter placed on the cervicothoracic area. Mean parameters are: 90 kV/100 mA s for the lateral view and 70 kV/160 mA s for the frontal one, meaning a non-negligible X-ray dose. The radiograph is centered on the twelfth thoracic vertebra and made during inhalation. For male, a gonadic lead protection has to be used. For the frontal view (Fig. 2), the patient is asked to stand in a natural erect posture, barefoot, feet gently spread, knees held in extension, stomach against the cassette and hands behind it, or arms hanging. It is also possible to make this radiograph in an anteroposterior direction, especially for female, for whom a breast lead protection can be used. It is usual to present the film in the left anatomical side at the left or the film, in a posterior view. For the lateral view [2] the patient is naturally standing up, looking horizontally, hands resting on a vertical support, upper limbs relaxed, elbows half bent. In this position, the upper limbs do not hide the spine nor change the natural standing position of the spine (Fig. 2) [3]. It is also possible to put the fingertips on both the cheek bones.With this conventional technique, depending on the patient’s size, it is generally possible to visualize from the skull to the pelvis, even sometimes to the cranial part of the femurs.
Fig. 2.
Patient’s position for conventional teleradiography
Above all, in obese patients, the images obtained by this technique are of medium, even poor quality, and it is often necessary on the lateral view to outline with a pencil the anterior borders of the vertebras to correctly show the position of the spine (Fig. 3). Some authors digitalize the conventional radiographs and then study them with dedicated software [2, 4] like Optispine® (SMAIO, Optimage, Lyon, France).
Fig. 3.

Conventional lateral teleradiography
The ability of making radiographs by a simultaneous translation of the X-ray tube and the receptor exists on some radiographic tables of several constructors. The position of the patient is same as described before and the problems are more or less the same than with conventional technique, vertical parallax deformation excluded.
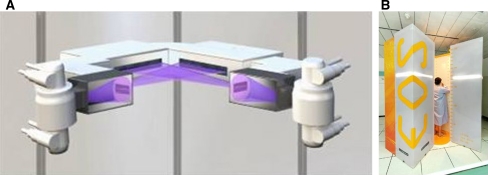
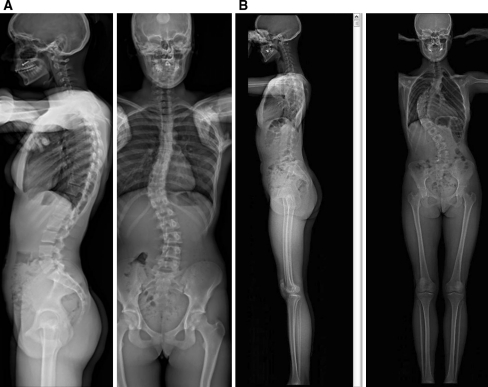
The concept of EOS® system (Biospace, Paris, France) rests on an identical scanning principle, improved by advanced technologies. This system is based on the use of a high sensitive xenon particle detector developed by G. Charpak (Physics Nobel prize winner in 1992) [5, 6]. This collimated detector is mechanically coupled to a X-ray tube in a stiff gantry giving out a fan-shaped strongly collimated X-ray beam. The simultaneous use of two X-ray tubes and two detectors, placed in two orthogonal planes in the gantry allows a simultaneous acquisition of lateral and frontal views. These two devices scan the body of the patient, in a standing position, on a vertical distance varying from 5 to 180 cm, that is to say, more or less, the whole body: skull, spine, pelvis and lower limbs (Fig. 4a, b). This system allows a very important reduction of the X-ray dose of an order of 80–90% versus conventional or digitalized radiographs [7]. This low level of irradiation clearly represents a great advantage, especially for young people. An important dynamic range of 30 000 gray levels (due to an automatic internal gain adjustment) and a pixel size of 250 μm give good quality images [7] with a simultaneous visibility of the thinnest regions (cervical spine) as well as the thickest ones (scapula-thoracic area, lower lumbar spine, pelvis) (Fig. 5a, b). Absence of parallax explains the lack of distortion of the anatomical structures. At last, with an appropriate software and a “bone morphing” technique, the simultaneous acquisition of sagittal and frontal views with identical anatomical landmarks in frontal and sagittal planes, makes possible the construction of a three-dimensional bone envelope weight bearing image of spine, pelvis and lower limbs which can be secondarily extracted and studied in all the planes of the space. Axial plane is particularly useful to visualize and measure the rotational abnormalities (Fig. 6) of spine and pelvis. These different assets (very low dose, good photographic quality, simultaneous acquisition of frontal and sagittal views, possibility to cover at the same time the spine and the lower limbs, study of the axial plane on 3D envelope) represent, in our opinion, a real progress in the imaging of the spine, particularly for the study of its sagittal balance.
Fig. 4.
a Principle of the EOS system with the two orthogonal tubes, their fan-shaped collimated X-ray beams and the two collimated detectors. b EOS system gantry with the patient inside
Fig. 5.
Simultaneous lateral and frontal EOS radiographs. a of the spine. b of the whole body
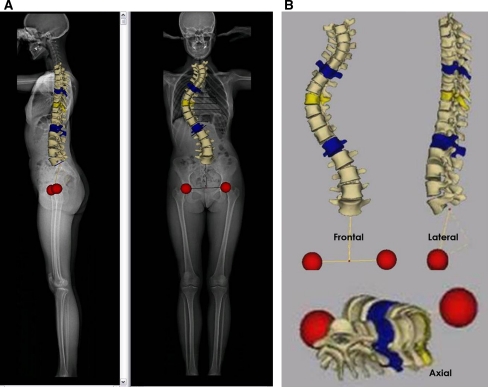
Fig. 6.
a 3D bone envelope reconstruction of the spine in lateral and frontal views. Femoral heads figure as red discs. b extraction of the spine/femoral heads block in frontal, lateral and axial views
In all the cases the patient positioning is crucial to obtain comparable and reproducible images. To decrease the artifacts due to the projection of the humerus on the spine in the lateral view without modifying the spine shape, it has been demonstrated after multiple trials that the best positioning was: standing both feet on the same alignment, 20–25 cm between the two feet, upper arm fingers tip on the clavicle as shown in Figs. 8 and 9.
Fig. 8.
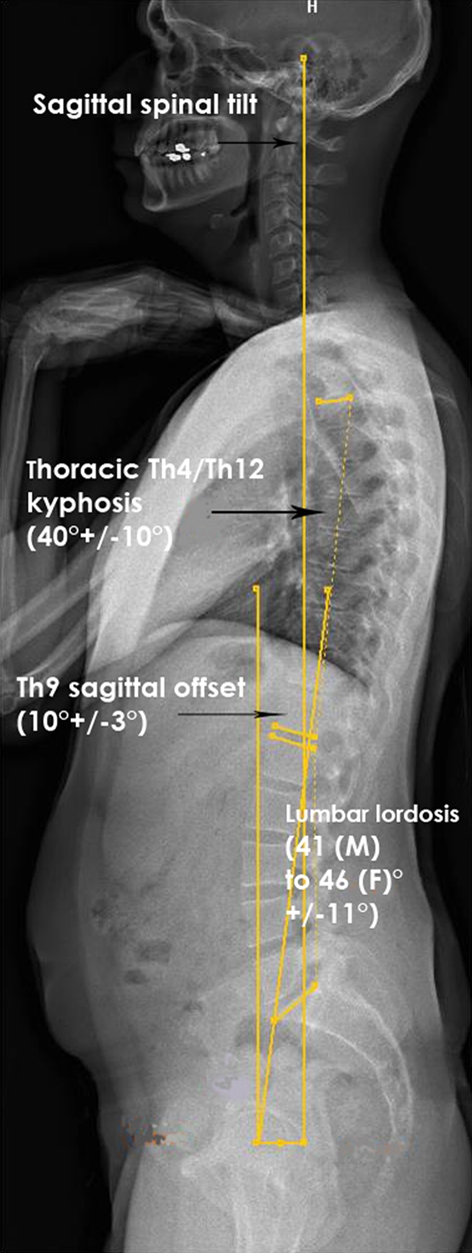
Spinal parameters
Fig. 9.

Spinal imbalance with compensation flexion of hips and knees, and after correction of the position
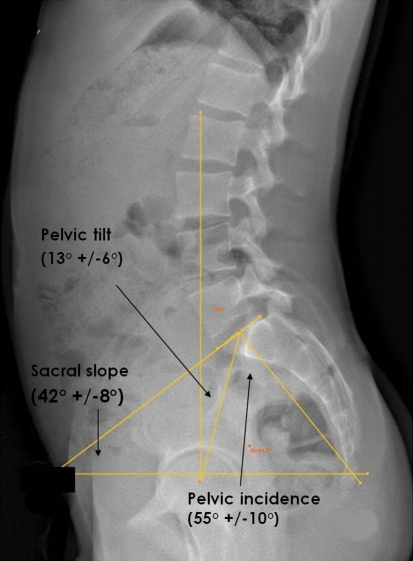
On these documents, conventional or digitalized, it is necessary to draw on sagittal views, manually or semi-automatically (depending on the different application softwares) different points and lines to assess at least three pelvic parameters (Table 1) pelvic incidence, pelvic tilt and sacral slope [8] (Fig. 7): the center of the femoral heads (C point) (or, if the two heads are not exactly superimposed, the middle of the line joining their two centers); the midpoint of the sacral endplate (S point); the C–S line; a vertical line passing through C point; a tangent line to sacral endplate; a perpendicular line to this tangent, passing through S point; an horizontal line cutting this tangent.
Table 1.
Normal value of spinopelvic parameters
| Pelvic tilt | 13° | ±6° |
| Sacral slope | 42° | ±8° |
| Pelvic incidence | 55° | ±10° |
| Lumbar lordosis | 41° (M) to 46° (F) | ±11° |
| Thoracic kyphosis | 40° | ±10° |
| Th 9 sagittal offset | 10° | ±3° |
Fig. 7.
Pelvic parameters
Pelvic tilt is the angle between vertical and CS line (N = 13° ± 6°), sacral slope the angle between the tangent at the sacral endplate and horizontal (N = 42° ± 8°) and pelvic incidence is the angle between CS and the perpendicular to the tangent at the sacral endplate (N = 55° ± 10°) [9]. The pelvic incidence is an anatomical parameter, there is no normal value, the average value is just an information, but does not predict a potential source of problem. Several other parameters have been described, in particular the overhang, defined as the horizontal offset between the midpoint of the sacral plate and the femoral heads center [10].
Then, some spinal parameters must be measured (Fig. 8): lumbar lordosis (angle between tangents at sacral and cranial L1 endplates) (N = 41° (male) to 46° (female) ±11°), thoracic kyphosis (angle between tangent to cranial endplate of Th4 and caudal endplate of Th12)(N = 40° ± 10°), Th9 sagittal offset (angle between vertical and a line joining the C point and the middle of the vertebral body of Th9) (N = 10° ± 3°). It is also possible to draw the vertical line passing through external acoustic meatus or the body of C7. C7 plumb line (C7PL) is defined as the horizontal offset from the postero-superior corner of S1 to the center of the vertebral body of C7.
Patients usually try to compensate sagittal spinal imbalance in hips and knees. It is a classical mistake (Fig. 9). So, rectitude of hips (vertical femurs) or knees and verticality of femurs must be carefully controlled clinically and on the radiographs. On frontal view, in case of scoliosis, Cobb’s angle and rotations of vertebrae (at best on axial 3D reconstructions) must be measured.
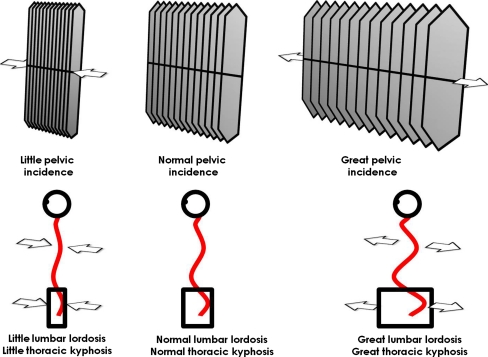
The value of pelvic incidence is an individual anatomical characteristic and corresponds to the “thickness” of the pelvis. Spine and pelvis, in a harmonious spinopelvic whole, can be compared to an accordion (Fig. 10). A normal pelvic incidence normally goes with a lumbar lordosis and a thoracic kyphosis of normal value. A flat pelvis (small pelvic incidence) corresponds at a compress accordion with small spinal curvatures. A stretched accordion corresponds to a thick pelvis (great pelvic incidence) with important spinal curvatures.
Fig. 10.
The spinopelvic accordion
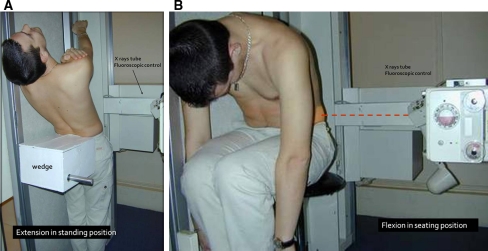
This global imaging of the spinal balance can be completed, if necessary, by localized or dynamic X-ray according to different cases. These dynamic radiographs must be carefully done. Numerous techniques of lateral dynamic X-rays and measurements have been described. The Putto’s technique [11], even if it can be criticized, seems to be the more reliable, its main drawback being the lack of fluoroscopic guiding that damages the precision of the placement of the landmarks. For lateral dynamic views, we used a simple technique derived from the technique of Putto that permits an easy fluoroscopic control: for the extension view, the patient is placed in an upright position on the step of the radiographic table, his buttocks wedged by a posterior support. We asked him to put his arms raised behind his head as in the Putto’s method, his lower limbs extended and to put his lumbar spine in a maximum extension position (Fig. 11a). For the flexion view, the patient is sitting on a rotary stool, thighs raised by a wedge, upper arms hanging along the trunk, lumbar spine in a maximum flexion position. We used the same fluoroscopic guiding for both the positions (Fig. 11b).
Fig. 11.
Patient’s position for extension a and flexion b dynamic radiographs of the lumbar spine
Most of the authors consider that a 3 mm sagittal translation of a vertebral body between flexion and extension X-rays is pathological [12]. For some, 2 mm is sufficient [13] (this number is at the limit of the measurement mistake) and some require 4 mm. Likewise, an angular movement superior to the physiological amplitude between flexion and extension (18° at L3–L4 level, 22° at L4–L5, 20° at L5–S1) for Farfan [12], a little bit less for Allbrook [14], (19° at L4–L5, 18°at L5–S1) means an instability.
Conclusion
Digitalized teleradiography in standing position allows a good evaluation of the sagittal balance and is the most commonly used system today, but the EOS X-rays brought a real progress for the study of the pelvispinal balance avoiding vertical parallax distortion with a very low dose of radiation. A great care must be taken for the protection of the patient against X-rays, patient positioning should be standardized to obtain comparable measurement of the pelvispinal parameters. Dynamic views, of major importance, must be done with the same care to be reliable.
Conflict of interest
None of the authors has any potential conflict of interest.
References
- 1.Legaye J, Saunier P, Dumas R, Vallee C. Correction for patients sway in radiographic biplanar imaging for three-dimensional reconstruction of the spine: in vitro study of a new method. Acta Radiol. 2009;50(7):781–790. doi: 10.1080/02841850903036272. [DOI] [PubMed] [Google Scholar]
- 2.Vialle R, Levassor N, Rillardon L, Templier A, Skalli W, Guigui P. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Joint Surg Am. 2005;87-A:260–267. doi: 10.2106/JBJS.D.02043. [DOI] [PubMed] [Google Scholar]
- 3.Roussouly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine. 2005;30:346–353. doi: 10.1097/01.brs.0000152379.54463.65. [DOI] [PubMed] [Google Scholar]
- 4.Rajnics P, Pomero V, Templier A, Lavaste F, Illes T. Computer-assisted assessment of spinal sagittal plane radiographs. J Spinal Disord. 2001;14:135–142. doi: 10.1097/00002517-200104000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Dubousset J, Charpak G, Dorion I, et al. A new 2D and 3D imaging approach to musculoskeletal physiology and pathology with low-dose radiation and the standing position: the EOS system. Bull Acad Natl Med. 2005;189(2):287–297. [PubMed] [Google Scholar]
- 6.Dubousset J, Charpak G, Skalli W, Kalifa G, Lazennec JY. EOS stereo-radiography system: whole-body simultaneous anteroposterior and lateral radiographs with very low radiation dose. Rev Chir Orthop Reparatrice Appar Mot. 2007;93:141–143. doi: 10.1016/s0035-1040(07)92729-4. [DOI] [PubMed] [Google Scholar]
- 7.Deschênes S, Charron G, Beaudoin G, Labelle H, Dubois J, Miron MC, Parent S. Diagnostic imaging of spinal deformities: reducing patients radiation dose with a new slot-scanning X-ray imager. Spine. 2010;35(9):989–994. doi: 10.1097/BRS.0b013e3181bdcaa4. [DOI] [PubMed] [Google Scholar]
- 8.Duval-Beaupère G, Schmidt C, Cosson P. A barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng. 1992;20(4):451–462. doi: 10.1007/BF02368136. [DOI] [PubMed] [Google Scholar]
- 9.Jackson RP, McManus AC. Pelvic lordosis and pelvic incidence: the relationship of pelvic parameters to sagittal spinal profile. Curr Opin Orthop. 2004;15:150–153. doi: 10.1097/01.bco.0000120643.46244.8a. [DOI] [Google Scholar]
- 10.Schwab F, Lafage V, Boyce R, Skalli W, Farcy JP. Gravity line analysis in adult volunteers. Age-related correlation with spinal parameters, pelvic parameters and foot position. Spine. 2006;31:E959–E967. doi: 10.1097/01.brs.0000248126.96737.0f. [DOI] [PubMed] [Google Scholar]
- 11.Putto E, Tallroth K. Extension-flexion radiographies for motion studies of the lumbar spine a comparison of two methods. Spine. 1990;115:107–110. doi: 10.1097/00007632-199002000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Farfan HJ. Mechanical disorders of the low back. Philadelphia: Lea and Febiger; 1973. [Google Scholar]
- 13.Morgan FP, Kingt T. Primary instability of lumbar vertebra as common cause of low back pain. J Bone Joint Surg Br . 1957;39:6–22. doi: 10.1302/0301-620X.39B1.6. [DOI] [PubMed] [Google Scholar]
- 14.Froning EC, Frohman B. Motion of the lumbosacral spine after laminectomy and spine fusion. Correlation of motion with the result. J Bone Joint Surg Am . 1968;50(5):897–917. [PubMed] [Google Scholar]