Abstract
There is a wide variation in the regional parameters used to describe the spine and sacro-pelvis in children and adolescents. There is a slight tendency for thoracic kyphosis and lumbar lordosis to increase with age. Pelvic incidence and pelvic tilt also tend to increase during growth, while sacral slope remains relatively stable. Strong knowledge of the close relationships between adjacent anatomical regions of the spine and sacro-pelvis is the key when evaluating and interpreting sagittal spino-pelvic alignment. The scheme of correlations between adjacent regional parameters needs to be preserved in order to maintain a balanced posture. The net resultant from these relationships between adjacent anatomical regions is best represented by parameters of sagittal global balance. C7 plumbline tends to move backwards from childhood to adulthood, where it stabilizes or slightly moves forward secondary to degenerative changes. C7 plumbline in front of both hip axis and center of the upper sacral endplate occurs in 29% of subjects aged 3–10 years, 12% of subjects aged between 10 and 18 years, and 14% of subjects aged 18 years or older. Therefore, although most normal subjects stand with a C7 plumbline behind the hip axis, a C7 plumbline in front of both hip axis and sacrum can be seen in normal individuals. However, progressive forward displacement of C7 plumbline should raise a suspicion for the risk of developing spinal pathology.
Keywords: Morphology, Pelvis, Posture, Sagittal alignment, Sagittal balance, Spine
Introduction
Sagittal spinal alignment has been reported in several studies because thorough knowledge of the normal anatomy is the key when evaluating patients with spinal pathologies. More recently, major efforts have also been devoted to the study of sagittal sacro-pelvic alignment, in accordance with the intimate link that exists between the spine and sacro-pelvis. The purpose of this review is to characterize the sagittal spino-pelvic alignment in the normal pediatric population.
Background data
Recently, Kuntz et al. [1] have provided pooled estimates of the mean and variance of parameters used to assess upright sagittal alignment in the normal pediatric population, based on a literature review. They have observed wide variations in the parameters, especially those used to evaluate regional spinal curves. In addition to normal individual variations in sagittal alignment observed in the general population, it is important to realize that the wide variability seen between previous studies is also highly influenced by the use of different measurements techniques.
Sagittal spinal alignment
Thoracic kyphosis (TK) and lumbar lordosis (LL) are usually used to describe sagittal spinal alignment. Voutsinas and MacEwen [2] assessed the sagittal spinal alignment of 670 normal subjects aged 5–20 years by measuring TK and LL using the most tilted vertebrae except for the upper endplate of S1, which was defined as the lower limit for measuring LL. TK was, respectively, 37° ± 7°, 38° ± 8°, and 39° ± 8° in subjects aged 5–9 years, 10–14 years, and 15–20 years. Bernhardt and Bridwell [3] studied the lateral radiographs of the spine in 102 normal subjects aged 4.6–29.8 years (mean: 12.8 years). TK measured from T3 to T12 was 36° ± 10° (range 9°–53°), while LL from T12 to L5 was 44° ± 12° (range: 4°–69°). Boseker et al. [4] evaluated 121 normal children aged 5–19 years and observed a mean TK of 33° (range 17°–51°) measured from the most tilted vertebrae. Using ±2 standard deviations (SD) from the mean as the definition of a normal TK, a normal range of 20°–50° was proposed. Cil et al. [5] assessed TK from T1 to T12 and LL from L1 to S1 in 151 children aged 3–15 years. TK was 45° ± 11°, 48° ± 11°, 46° ± 11°, and 53° ± 9° in 3–6 years, 7–9 years, 10–12 years, and 13–15 years age groups, respectively. LL was 44° ± 11°, 52° ± 12°, 57° ± 10°, and 55° ± 10° in 3–6 years, 7–9 years, 10–12 years, and 13–15 years age groups, respectively. Mac-Thiong et al. [6] used a computer-assisted technique to generate a geometric model of the spine for which TK is calculated from the whole kyphotic segment of the spine while LL is represented by the lordotic segment down to the inferior endplate of L5. Mean TK and LL in 341 normal subjects aged 3–18 years were, respectively, 44° ± 11° and 48° ± 12°. Recent unpublished data from the current authors on 646 asymptomatic children aged 3–18 years provide the range of values for TK (complete kyphotic segment) and LL (lordotic segment down to S1) expected in the normal pediatric population (Table 1). TK and LL values are similar between males and females.
Table 1.
Parameters of sagittal alignment in 646 children and adolescents
| Age group | Number of females:males | Age (years) | Thoracic kyphosis | Lumbar lordosis | Pelvic incidence | Pelvic tilt | Sacral slope |
|---|---|---|---|---|---|---|---|
| 3–10 years | 103:64 | 8.1 ± 2.0 | 42.0° ± 10.6° | 53.8° ± 12.0° | 43.7° ± 9.0° | 5.5° ± 7.6° | 38.2° ± 7.7° |
| >10 and <18 years | 267:212 | 13.6 ± 1.9 | 45.8° ± 10.4° | 57.7° ± 11.1° | 46.9° ± 11.4° | 7.7° ± 8.3° | 39.1° ± 7.6° |
| All | 370:276 | 12.1 ± 3.1 | 44.8° ± 10.6° | 56.7° ± 11.4° | 46.0° ± 10.9° | 5.2° ± 8.2° | 38.9° ± 7.6° |
Sagittal sacro-pelvic alignment
In addition to the spinal alignment, sagittal sacro-pelvic alignment is also recognized as being an important aspect to consider in the evaluation and treatment of spinal pathologies. Appropriate knowledge of sacro-pelvic morphology is also important due to its close relationship with sacro-pelvic alignment. Sacro-pelvic alignment refers to the orientation of the sacro-pelvis in space while sacro-pelvic morphology refers to the anatomical features of the sacro-pelvis and is therefore unaffected by the position of the individual. Sagittal sacro-pelvic alignment is most commonly assessed in children from the pelvic tilt (PT) and sacral slope (SS). As for sacro-pelvic morphology, pelvic incidence (PI) is the most widely used parameter because it is directly related to PT and SS (PI = PT + SS). [7] In their evaluation of 341 normal children and adolescents, Mac-Thiong et al. [6] have found mean values of 49° ± 11° for PI, 8° ± 8° for PT, and 41° ± 8° for SS. Recent unpublished data from the current authors on 646 asymptomatic children aged 3–18 years are provided in Table 1 for PI, PT and SS. PI, PT, and SS values are similar between males and females.
Sagittal alignment and growth
While many studies have attempted to characterize sagittal spinal and sacro-pelvic alignment during growth, the conclusions remain limited since longitudinal studies with prospective cohorts are still lacking. However, it seems that discrete changes in sagittal alignment occur during growth, in order to accommodate for physiological and morphological changes. Vedentam et al. [8] compared the sagittal alignment of 88 asymptomatic adolescents aged 13 ± 8 years with that of 100 asymptomatic adults aged 57 ± 11 years. The adolescent and adult cohorts presented similar LL (64° ± 10° in both groups), but slightly increased TK in adolescents (38° ± 10° vs. 34° ± 11°). Voutsinas and MacEwen [2] reported a slight increase in TK (1.8° mean difference) and LL (4.4° mean difference) from 5 to 20 years old groups. Cil et al. [5] also observed a tendency for increasing TK and LL between different age groups (3–6 vs. 7– vs. 10–12 vs. 13–15 years). However, Mac-Thiong et al. [6, 9] have shown that the correlation between age and TK or LL, although statistically significant, remains modest clinically (r < 0.3).
As for sacro-pelvic morphology, previous studies [10–12] suggested that PI increases after the acquisition of bipedalism in children and stabilizes during adulthood. Accordingly, Mac-Thiong et al. [9] have shown that the increase in PI with age is small and that this trend is similar before and after 10 years of age in the pediatric population after the acquisition of bipedalism. This increase in PI mainly results in a proportional increase in PT, while maintaining a relatively stable SS.
Sagittal spino-pelvic alignment: underlying concepts
A balanced posture is obtained when the spine and sacro-pelvis are aligned so that energy expenditure is minimized and horizontal gaze is preserved. There are two basic concepts underlying this principle. First and foremost, adjacent anatomical regions of the spine and sacro-pelvis are interdependent, and their relationships result in a stable and balanced posture [6, 13]. More important than knowing normative values of regional parameters of the spine and sacro-pelvis, understanding the close relationships between these parameters is the key when evaluating and interpreting sagittal spino-pelvic alignment. Although regional spinal and sacro-pelvic parameters differ between pediatric and adult subjects, the scheme of correlations between parameters is similar in pediatric and adult subjects. Second, the net resultant from these relationships between adjacent anatomical regions is best represented by parameters of sagittal global balance. As shown by Kuntz et al. [1], parameters of global balance are maintained in a narrower range than regional parameters in the normal population. The importance of sagittal global balance is also supported by studies [14, 15] demonstrating its significant relationship with health-related quality of life in spinal deformity.
Relationships in sagittal spino-pelvic alignment
From the correlations between parameters of adjacent anatomical regions of the spine and sacro-pelvis, Mac-Thiong et al. [6] have presented an overview of the sagittal posture in the normal pediatric population (Fig. 1). Based on observations made in the sagittal alignment of children and adolescents with spondylolisthesis [16], it is assumed that this scheme of correlations needs to be preserved in spinal pathology in order to maintain a balanced posture. The most clinically relevant correlation involves PI and LL since this normal relationship needs to be restored or preserved when instrumenting the lumbar spine. PI can be used to estimate the LL that needs to be set intraoperatively because PI is a true morphological parameter (not affected by the positioning). As shown in Fig. 2, the regression line between PI and LL can be used as a guide to estimate the magnitude of LL that should be expected by the surgeon with respect to a specific PI value. Alternatively, the logistic regression equation provided can also be used.
Fig. 1.
Overview of statistically significant correlations between parameters of adjacent anatomical regions of the spine and sacro-pelvis. Moderate (0.3 ≤ r < 0.5) and strong (r ≥ 0.5) correlations are shown in dotted and full arrows, respectively. The mathematical relationship between pelvic tilt and sacral slope is also shown. Thoracic tilt and lumbar tilt refer to the orientation of the kyphotic and lordotic segments of the spine. (Adapted from Mac-Thiong et al. Eur Spine J 2007; 16:227–234)
Fig. 2.
Logistic regression illustrating the relationship between lumbar lordosis and pelvic incidence, based on the study of 646 normal children and adolescents
Assessment of sagittal global balance
Global balance refers to the overall alignment of the spine—generally using center of C7 vertebral body as a reference point—with respect to another landmark on the sacro-pelvis. Assessment of global balance provides information on existing relationships between parameters describing the sacro-pelvis, lumbar spine, thoracic spine, and cervical spine. Clinically, global spinal balance is an important aspect of the evaluation of patients with spinal pathology and of surgical planning, and to minimize complications such as adjacent segment disease, sagittal imbalance, pseudarthrosis, and progressive deformity.
Vedentam et al. [8] compared the sagittal global balance between adolescents and adults based on the assessment of the horizontal distance between C7 plumbline (vertical line from the center of C7 vertebral body) and the antero-superior corner of S1 vertebral body. They observed a significantly forward displacement of C7 plumbline from −5.6 ± 3.5 cm in adolescents to −3.2 ± 3.2 cm in adults. More specifically, Cil et al. [5] noted progressive backward displacement of C7 plumbline with respect to the postero-superior corner of S1 vertebral body during growth, with mean values of 2.5 ± 4.3 cm, 0.7 ± 4.6 cm, −0.1 ± 4.1 cm, and −0.9 ± 4.4 cm, respectively, for 3–6 years, 7–9 years, 10–12 years, and 13–15 years age groups. In comparison, Jackson and McManus [17] reported values of −0.1 ± 2.5 cm for a cohort of 100 asymptomatic adults aged 38.9 ± 9.4 years (range 20–63 years).
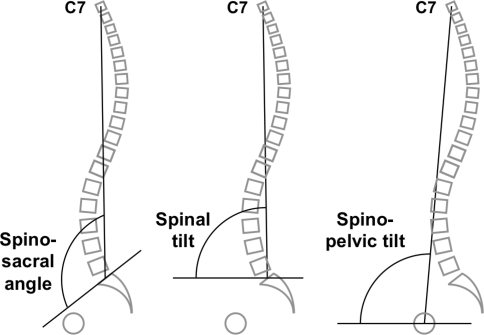
Linear parameters of global balance are, however, subject to measurement errors that can limit comparisons between different studies. Consequently, angular or descriptive parameters of global balance are preferred. Angular parameters also provide the advantage of considering the spinal length. The use of the three following angular parameters of sagittal global balance is suggested (Fig. 3):
Spino-sacral angle or SSA angle subtended by the upper sacral endplate and the line from the center of C7 vertebral body to the center of the upper sacral endplate, as described by Roussouly et al. [18].
Spinal tilt or ST angle subtended by the horizontal line and the line from the center of C7 vertebral body to the center of the upper sacral endplate. A value greater than 90° indicates that the center of C7 vertebral body is behind the center of the upper sacral endplate, while for values less than 90°, the center of C7 vertebral body is in front of the center of the upper sacral endplate.
Spino-pelvic tilt or SPT angle subtended by the horizontal line and the line from the center of C7 vertebral body to the hip axis (midpoint of the line joining the center of the femoral heads). A value greater than 90° indicates that the center of C7 vertebral body is behind the hip axis, while for values less than 90°, the center of C7 vertebral body is in front of the center of the hip axis.
Fig. 3.
Measurement of sagittal global balance. a Spino-sacral angle, b spinal tilt, and c spino-pelvic tilt
Alternatively, a classification system can be used to describe sagittal global balance from the position of C7 plumbline relative to both sacrum and hip axis (Fig. 4) [19]. This technique is easier to use clinically because it does not require any calculation or measurement.
Fig. 4.
Classification system for determining sagittal global balance from the position of C7 plumbline relative to the center of the upper sacral endplate (S1) and to the hip axis (HA). Types 1 to 3 refer to cases for which HA lies in front of the center of the upper sacral endplate, whereas types 4–6 are present when HA is behind the center of the upper sacral endplate
Mac-Thiong et al. [20] recently evaluated sagittal global balance in asymptomatic cohorts of 646 pediatric and 715 adult subjects. SSA and ST were, respectively, 130° ± 10° and 92° ± 6° in subjects aged 3–10 years, 133° ± 8° and 94° ± 4° in subjects between 10 and 18 years, and 131° ± 8° and 91° ± 3° in adults 18 years or older. In accordance with observations from Cil et al. [5], C7 plumbline therefore tends to move backwards until adulthood, where it stabilizes or slightly moves forward secondary to degenerative changes. As for sagittal global balance type (Fig. 4), a C7 plumbline in front of both hip axis and center of the upper sacral endplate (types 3 or 6) occurred in 28.7% of subjects aged 3–10 years, 12.0% of subjects aged between 10 and 18 years, and 14.1% of subjects aged 18 years or older. Therefore, although most normal subjects stand with a C7 plumbline behind the hip axis, a C7 plumbline in front both hip axis and sacrum can be seen in normal individuals. However, progressive forward displacement of C7 plumbline should raise a suspicion for the risk of developing spinal pathology.
Acknowledgments
Conflict of interest None.
References
- 1.Kuntz C, 4th, Shaffrey CI, Ondra SL, Durrani AA, Mummaneni PV, Levin LS, Pettigrew DB. Spinal deformity: a new classification derived from neutral upright spinal alignment measurements in asymptomatic juvenile, adolescent, adult, and geriatric individuals. Neurosurgery. 2008;63:A25–A39. doi: 10.1227/01.NEU.0000313120.81565.D7. [DOI] [PubMed] [Google Scholar]
- 2.Voutsinas SA, MacEwen GD. Sagittal profiles of the spine. Clin Orthop. 1986;210:235–242. [PubMed] [Google Scholar]
- 3.Bernhardt M, Bridwell KH. Segmental analysis of the sagittal plane alignment of the normal thoracic and lumbar spines and thoracolumbar junction. Spine. 1989;14:717–721. doi: 10.1097/00007632-198907000-00012. [DOI] [PubMed] [Google Scholar]
- 4.Boseker EH, Moe JH, Winter RB, Koop SE. Determination of “normal” thoracic kyphosis: a roentgenographic study of 121 “normal” children. J Pediatr Orthop. 2000;20:796–798. doi: 10.1097/01241398-200011000-00019. [DOI] [PubMed] [Google Scholar]
- 5.Cil A, Yazici M, Uzumcugil A, Kandemir U, Alanay A, Alanay Y, Acaroglu RE, Surat A. The evolution of sagittal segmental alignment of the spine during childhood. Spine. 2005;30:93–100. [PubMed] [Google Scholar]
- 6.Mac-Thiong JM, Labelle H, Berthonnaud E, Betz RR, Roussouly P. Sagittal spinopelvic balance in normal children and adolescents. Eur Spine J. 2007;16:227–234. doi: 10.1007/s00586-005-0013-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Duval-Beaupère G, Schmidt C, Cosson P. A barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng. 1992;20:451–462. doi: 10.1007/BF02368136. [DOI] [PubMed] [Google Scholar]
- 8.Vedantam R, Lenke LG, Keeney JA, Bridwell KH. Comparison of standing sagittal spinal alignment in asymptomatic adolescents and adults. Spine. 1998;23:211–215. doi: 10.1097/00007632-199801150-00012. [DOI] [PubMed] [Google Scholar]
- 9.Mac-Thiong JM, Berthonnaud E, Dimar JR, 2nd, Betz RR, Labelle H. Sagittal alignment of the spine and pelvis during growth. Spine. 2004;29:1642–1647. doi: 10.1097/01.BRS.0000132312.78469.7B. [DOI] [PubMed] [Google Scholar]
- 10.Descamps H, Commare-Nordmann MC, Marty C, Hecquet J, Duval-Beaupere G. Modifications des angles pelviens, dont l’incidence, au cours de la croissance humaine. Biom Hum Anthropol. 1999;17:59–63. [Google Scholar]
- 11.Mangione P, Gomez D, Senegas J. Study of the course of the incidence angle during growth. Eur Spine J. 1997;6:163–167. doi: 10.1007/BF01301430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marty C, Boisaubert B, Descamps H, Montigny JP, Hecquet J, Legaye J, Duval-Beaupère G. The sagittal anatomy of the sacrum among young adults, infants, and spondylolisthesis patients. Eur Spine J. 2002;11:119–125. doi: 10.1007/s00586-001-0349-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berthonnaud E, Dimnet J, Roussouly P, Labelle H. Analysis of the sagittal balance of the spine and pelvis using shape and orientation parameters. J Spinal Disord Tech. 2005;18:40–47. doi: 10.1097/01.bsd.0000117542.88865.77. [DOI] [PubMed] [Google Scholar]
- 14.Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine. 2005;30:2024–2029. doi: 10.1097/01.brs.0000179086.30449.96. [DOI] [PubMed] [Google Scholar]
- 15.Mac-Thiong JM, Transfeldt EE, Mehbod AA, Perra JH, Denis F, Garvey TA, Lonstein JE, Wu C, Dorman CW, Winter RB. Can C7 plumbline and gravity line predict health related quality of life in adult scoliosis? Spine. 2009;34:E519–E527. doi: 10.1097/BRS.0b013e3181a9c7ad. [DOI] [PubMed] [Google Scholar]
- 16.Mac-Thiong JM, Wang Z, Guise JA, Labelle H. Postural model of sagittal spino-pelvic balance and its relevance for lumbosacral developmental spondylolisthesis. Spine. 2008;33:2316–2325. doi: 10.1097/BRS.0b013e318186b236. [DOI] [PubMed] [Google Scholar]
- 17.Jackson RP, McManus RP. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients volunteers and patients with low back pain matched for age, sex, and size. A prospective controlled clinical study. Spine. 1994;19:1611–1618. doi: 10.1097/00007632-199407001-00010. [DOI] [PubMed] [Google Scholar]
- 18.Roussouly P, Gollogly S, Noseda O, Berthonnaud E, Dimnet J. The vertical projection of the sum of the ground reactive forces of a standing patient is not the same as the C7 plumb line. A radiographic study of the sagittal alignment of 153 asymptomatic volunteers. Spine. 2006;31:E320–E325. doi: 10.1097/01.brs.0000218263.58642.ff. [DOI] [PubMed] [Google Scholar]
- 19.Mac-Thiong JM, Roussouly P, Berthonnaud E, Guigui P. Sagittal parameters of global balance. Normative values from a prospective cohort of seven hundred nine white asymptomatic adults. Spine. 2010;22:E1193–E1198. doi: 10.1097/BRS.0b013e3181e50808. [DOI] [PubMed] [Google Scholar]
- 20.Mac-Thiong J-M, Roussouly P, Berthonnaud É, Labelle H (2010) Global sagittal spinal balance: normative values from a prospective cohort of 715 asymptomatic adults and 646 asymptomatic children. In: Presented at the Scoliosis Research Society 45th annual meeting & combined course, Kyoto, Japan, September 21–24