Abstract
Introduction
In L5-S1 spondylolisthesis, it has been clearly demonstrated over the past decade that sacro-pelvic morphology is abnormal and that it can be associated to an abnormal sacro-pelvic orientation as well as to a disturbed global sagittal balance of the spine. The purpose of this article is to review the work done within the Spinal Deformity Study Group (SDSG) over the past decade, which has led to a classification incorporating this recent knowledge.
Material and methods
The evidence presented has been derived from the analysis of the SDSG database, a multi-center radiological database of patients with L5-S1 spondylolisthesis, collected from 43 spine surgeons in North America and Europe.
Results
The classification defines 6 types of spondylolisthesis based on features that can be assessed on sagittal radiographs of the spine and pelvis: (1) grade of slip, (2) pelvic incidence, and (3) spino-pelvic alignment. A reliability study has demonstrated substantial intra- and inter-observer reliability similar to other currently used classifications for spinal deformity. Furthermore, health-related quality of life measures were found to be significantly different between the 6 types, thus supporting the value of a classification based on spino-pelvic alignment.
Conclusions
The clinical relevance is that clinicians need to keep in mind when planning treatment that subjects with L5-S1 spondylolisthesis are a heterogeneous group with various adaptations of their posture. In the current controversy on whether high-grade deformities should or should not be reduced, it is suggested that reduction techniques should preferably be used in subjects with evidence of abnormal posture, in order to restore global spino-pelvic balance and improve the biomechanical environment for fusion.
Keywords: Spondylolisthesis, Classification, Sagittal balance, Spino-pelvic alignment
Introduction
Sagittal sacro-pelvic morphology and orientation modulate the geometry of the lumbar spine and consequently, the mechanical stresses at the lumbo-sacral junction. In L5-S1 spondylolisthesis, it has been clearly demonstrated over the past decade that sacro-pelvic morphology is abnormal and that combined with the presence of a local lumbo-sacral deformity and dysplasia, it can result in an abnormal sacro-pelvic orientation as well as to a disturbed global sagittal balance of the spine. These findings have important implications for the evaluation and treatment of patients with spondylolisthesis, and especially for those with a high-grade slip. In the current controversy on whether high-grade deformities should or should not be reduced, they provide a compelling rationale to reduce and realign the deformity, in order to restore global spino-pelvic balance and improve the biomechanical environment for fusion [1]. This has stimulated a renewed interest for the radiological evaluation and classification of spino-pelvic alignment in this condition [2]. The commonly used classification systems from Wiltse et al. [3] and from Marchetti and Bartolozzi [4] are useful to identify the underlying pathology, but they are of little help to guide surgical treatment. Recently, the Spinal Deformity Study Group (SDSG) has proposed a classification system [5] in six different sagittal postures, based on the radiographic measurement of slip grade and spino-pelvic alignment (pelvic incidence, sacro-pelvic and spinal balance). The purpose of this article is to review the work done within the SDSG on this subject over the past decade, which has led to the proposed classification and to illustrate its clinical relevance to guide surgical decision-making in L5-S1 spondylolisthesis. The evidence presented has been derived from the analysis of the SDSG database, a multi-center radiological database of patients with L5-S1 developmental or acquired stress fracture [4] spondylolisthesis, which now contains standing lateral radiographs of the spine and pelvis of 816 subjects with grade 1 to 5 spondylolisthesis, aged between 10 to 40 years and collected from 43 spine surgeons in North America and Europe.
Evidence for abnormal sagittal spino-pelvic alignment
When compared to a control population, Pelvic Incidence (PI), Sacral Slope (SS), Pelvic Tilt (PT), and Lumbar Lordosis were shown by Labelle et al. [6] to be significantly greater in a cohort of 214 subjects with spondylolisthesis. Furthermore, the differences between the two populations increased in a direct linear fashion as the severity of the spondylolisthesis increases. Although the correlation between PI and spondylolisthesis is evident, there is still no clear data in the literature that has demonstrated a cause/effect relationship between the two. However, since PI is a morphological parameter describing the shape of the pelvis, an abnormally high PI is typically associated with a high lumbar lordosis predisposing to altered mechanical stresses in the lumbar spine and lumbo-sacral junction, suggesting a higher risk of presenting spondylolisthesis.
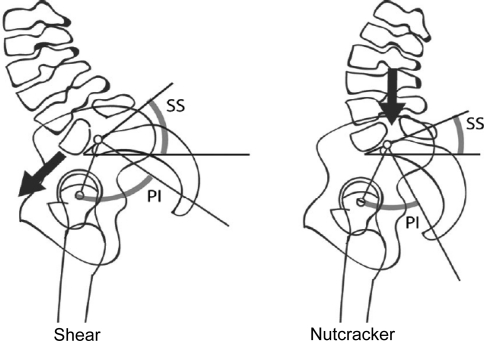
Not all patients with L5-S1 spondylolisthesis do, however, present with a higher than normal PI. Roussouly et al. [7] noted two different subgroups of sacro-pelvic balance and shape in 82 subjects with low-grade spondylolisthesis that might be affected by a different pathogenic mechanism. In their opinion, patients with high PI and sacral slope have increased shear stresses at the lumbo-sacral junction, causing more tension on the pars interarticularis at L5: the shear type (Fig. 1). On the opposite, patients with a low PI and a smaller sacral slope would have impingement of the posterior elements of L5 between L4 and S1 during extension, thereby causing a ‘‘nutcracker’’ effect on the pars interarticularis at L5 (Fig. 1). Based on K-means cluster analysis, Labelle et al. [5]. have confirmed the existence of distinct subgroups of sacro-pelvic balance in a larger SDSG cohort of 540 low-grade isthmic spondylolisthesis: a subgroup with normal PI and SS values averaging respectively 52 ± 7° and 41 ± 7°, and a subgroup with high PI and SS values averaging respectively 74 ± 10° and 53 ± 7°, thereby strongly supporting the existence of the shear type spino-pelvic posture with high PI and high SS. In a further analysis of the same first subgroup of subjects with normal PI values, using this time an unsupervised two-step cluster analysis, Mac-Thiong et al. [8] were able to recognize two further significantly different spino-pelvic alignment postures: a smaller specific subgroup with low PI (42 ± 5°) and SS (35 ± 4°), thereby corresponding to the nutcracker type, and another larger group with normal PI (54 ± 4°) and SS (45 ± 4°) with a similar spino-pelvic alignment to the one found in a normal control population.
Fig. 1.
The shear and nutcracker spino-pelvic postures reported by Roussouly et al. [7] in low grade spondylolisthesis
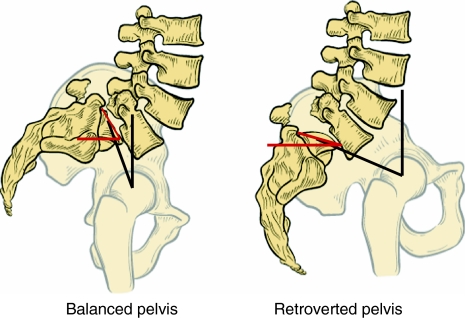
As for high-grade spondylolisthesis, Hresko et al. [9] have identified two subgroups of sacro-pelvic alignment using K-means cluster analysis in an initial cohort of 133 patients: balanced versus unbalanced pelvis (Fig. 2). The ‘‘balanced’’ group includes patients standing with a high SS and a low PT, a posture similar to a control subgroup of individuals with high PI but no evidence of spondylolisthesis, while the “unbalanced” group includes patients standing with a retroverted pelvis and a vertical sacrum, corresponding to a low SS and a high PT. More recently, a similar study [5] on a larger cohort of 276 subjects has confirmed the existence of these 2 different sacro-pelvic alignments, and has demonstrated that almost all subjects with high-grade slips have above average PI values ≥ 60º. This is in distinct contrast with subjects having low-grade spondylolisthesis in which low, normal or above average PI values are noted.
Fig. 2.
The balanced and retroverted pelvic postures reported by Hresko et al. [9] in high grade spondylolisthesis.
Furthermore, it was found that global spinal balance, as measured with the C7 plumb line, was significantly higher (>3 cm) in subjects with a retroverted (unbalanced) posture[5], thereby suggesting that positive sagittal spine imbalance can be associated with this type of spino-pelvic alignment. In support of this last finding, using a postural model of spino-pelvic balance showing the relationships between parameters of each successive anatomical segment from the thoracic spine to the sacro-pelvis, Mac-Thiong et al. [10] have observed in a study comparing 120 controls to 131 subjects with spondylolisthesis that a relatively normal global trunk posture was maintained in low-grade spondylolisthesis, while it was abnormal in high-grade spondylolisthesis. Again, in high-grade spondylolisthesis, the spino-pelvic balance was particularly disturbed in the subgroup with an unbalanced sacro-pelvis.
Spinal deformity study group classification
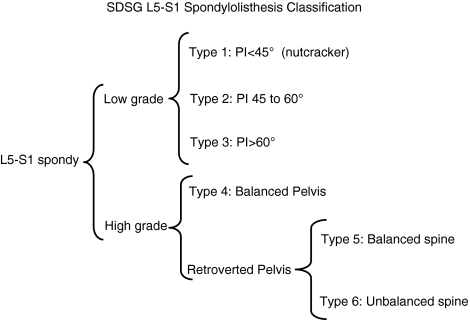
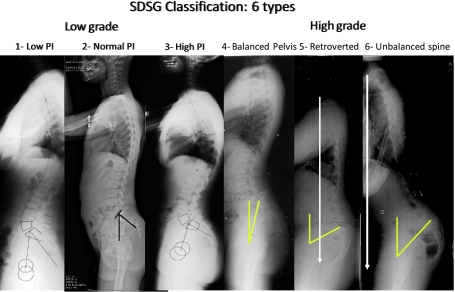
Based on a systematic review of the literature, Mac-Thiong and Labelle [11] have presented a classification system incorporating this recent knowledge in sagittal spino-pelvic balance and intended to guide surgical treatment of developmental spondylolisthesis in children, adolescents and young adults. In addition to slip grade and spino-pelvic balance, this first attempt at classification also incorporated the degree of bony dysplasia and proposed eight different types of deformity. Unfortunately, in a subsequent variability study [12], the authors found only fair overall inter-observer reliability (kappa: 0.49) for this classification system, mainly due to the difficulty in accurately determining the degree of dysplasia (inter-observer kappa: 0.43) on radiographs. Consequently, the SDSG has decided to exclude assessment of dysplasia and the classification has been further refined and simplified. It is based on three important characteristics that can be assessed on sagittal radiographs of the spine and pelvis: (1) the grade of slip (low or high), (2) the pelvic incidence (low, normal or high), and (3) the spino-pelvic balance (balanced or unbalanced). Accordingly, six different subtypes can be identified (Fig. 3).
Fig. 3.
Classification of spondylolisthesis based on spino-pelvic posture
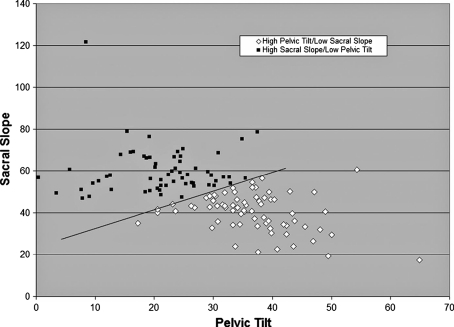
To classify a patient, the degree of slip is quantified first from the lateral radiograph, in order to determine if it is low-grade (grades 0, 1 and 2, or <50% slip) or high-grade (grades 3, 4 and spondyloptosis, or ≥50% slip). Next, the sagittal balance is measured by determining sacro-pelvic and spino-pelvic alignment, using measurements of PI, SS, PT and the C7 plumb line. For low-grade spondylolisthesis, three types of sacro-pelvic balance can be found: type 1, the nutcracker type, a subgroup with low PI (< 45°), type 2, a subgroup with normal PI (between 45 and 60°), and type 3, the shear type, a subgroup with high PI (≥60°). For high-grade spondylolisthesis, three types are also found. Each subject is first classified as having a balanced or an unbalanced sacro-pelvis using PI and SS values and the nomogram provided by Hresko et al. [9] (Fig. 4). When SS and PT are located above the threshold line, the subject is classified as high SS/low PT. On the other hand, when SS and PT are located below the threshold line, the subject is classified as low SS/high PT. Next, spino-pelvic balance is determined using the C7 plumb line. If this line falls over or behind the femoral heads, the spine is balanced, while if it lies in front of the femoral heads, the spine is unbalanced. In our experience, the spine is almost always balanced in low-grade and in high-grade spondylolisthesis [10] with a balanced sacro-pelvis and therefore, spinal balance needs to be measured mainly in high-grade deformities with an unbalanced pelvis. Therefore, the three types in high grade spondylolisthesis are: type 4 balanced pelvis, type 5 retroverted pelvis with balanced spine and type 6 retroverted pelvis with unbalanced spine. Figure 5 illustrates clinical examples of theses six postures.
Fig. 4.
Nomogram reported by Hresko et al. [9] to classify balanced vs retroverted pelvic posture using SS and PT values
Fig. 5.
Lateral radiographs demonstrating the 6 types of spino-pelvic postures
In a recent clinical assessment of this refined version of the classification system, Mac-Thiong et al. [13] found improved and substantial intra- and inter-observer reliability similar to other currently used classifications for spinal deformity, with an overall intra- and inter-observer agreements of 80% (kappa: 0.74) and 71% (kappa: 0.65), respectively. Further improvements in reliability are expected with a computer-assisted classification technique.
Clinical relevance for treatment of spondylolisthesis
Currently, most treatment protocols proposed in the literature for developmental spondylolisthesis have focused mainly on the abnormalities noted at the L5-S1 junction, mostly the slip grade. Surgery is usually recommended for patients with low-grade deformities, which are unresponsive to conservative management, and for all high-grade slips. While slip grade is an important component of the deformity, the evidence presented above demonstrates that sacro-pelvic morphology and balance are strong determinants of sagittal spino-pelvic alignment and that they should be considered in any treatment algorithm. The presence of different patterns of sagittal spino-pelvic balance suggests that the biomechanics involved in spondylolisthesis may differ from one patient to the other. Accordingly, the specific pattern of sagittal spino-pelvic balance for each patient should influence the risk of progression and the treatment outcome. In support of this concept [14], a cohort of 397 adolescents with L5-S1 spondylolisthesis has been compared to an aged-matched control population: health-related quality of life measures were found to be clearly abnormal in spondylolisthesis, with significant differences according to various types of spino-pelvic alignment, thus supporting the value of a classification based on spino-pelvic alignment.
Abnormal spino-pelvic balance alters the biomechanical stresses at the lumbo-sacral junction and the compensation mechanisms used to maintain an adequate posture. Since PI is always much greater than normal in high-grade spondylolisthesis, this suggests that the risk of progression in types 1 and 2 with lower or normal PI may be lower than in the shear type 3 with abnormally high PI and SS values imposing higher shear stresses at the L5-S1 junction. In these subjects as well as those with type 4 alignment, there is an increased lumbar lordosis in order to keep the center of gravity and C7 plumb line behind the hips to maintain a balanced posture. This first compensation mechanism occurs by increasing the intervertebral segmental lordosis and/or by including more vertebrae in the lordotic segment. For each patient, there is a maximal attainable lumbar lordosis beyond which the patient will then attempt to maintain a balanced posture by progressive retroversion of the pelvis. This second compensation mechanism corresponds to the abnormal posture found in types 5 and 6 with a retroverted pelvis/vertical sacrum. Because each patient has a fixed pelvic incidence, since it is an anatomic parameter, SS decreases along with the retroversion of the pelvis and PT increases as the sacrum becomes vertical. When the limit of these two compensation mechanisms is reached, the patient develops sagittal trunk imbalance, most often characterized either by compensatory hip flexion, by forward leaning of the trunk with positive sagittal imbalance of the spine, or a combination of both, as seen in type 6 posture.
The SDSG classification is the first that organizes subgroups of spondylolisthesis in an ascending order of severity according to prognosis and/or spino-pelvic alignment. Because the classification is designed so that subgroups are in an ascending order of severity, it becomes easier and more intuitive to develop an associated surgical algorithm because the complexity of the surgery should increase, as the severity of the spondylolisthesis increases.
While the need for reduction in the surgical treatment of spondylolisthesis is still debated, three studies provide some insight for the decision-making process. Hresko et al. [9] stated that the failure to analyze sacro-pelvic balance and therefore to distinguish between a balanced and an unbalanced sacro-pelvis could account for the variability found in the literature regarding the outcome of reduction for high-grade spondylolisthesis. Accordingly, they suggest that reduction techniques might preferably be considered in types 5 and 6 with an unbalanced sacro-pelvis. Mac-Thiong et al. [10] also suggested attempting reduction of high-grade spondylolisthesis in types 5 and 6 with an unbalanced sacro-pelvis since these patients present with an abnormal spino-pelvic balance, as compared to the normal population. Finally, in a retrospective multi-center study analysis of spino-pelvic alignment after surgical correction of 73 subjects with high grade slips, Labelle et al. [15] have shown that while sacro-pelvic shape (PI) is unaffected by attempts at surgical reduction, proper repositioning of L5 over S1 significantly improves sacro-pelvic balance and the shape of the lumbar spine in developmental spondylolisthesis. Their results also emphasize the importance of sub-dividing subjects with high-grade spondylolisthesis into types 4, 5 and 6, and further support the contention that reduction techniques might preferably be considered for types 5 and 6 of the classification.
In summary, the proposed classification emphasizes that subjects with L5-S1 spondylolisthesis are a heterogeneous group with various adaptations of their posture and that clinicians need to keep this fact in mind for evaluation and treatment. Although outcome studies are obviously needed before a definitive treatment algorithm can be established for each subtype, it is suggested that for subjects with a type 4 spino-pelvic alignment, forceful attempts at reduction of the deformity may not be required and that simple instrumentation and fusion after postural reduction may be sufficient to maintain adequate sagittal alignment. For subjects with type 5 posture, reduction and realignment procedures should preferably be attempted, but in difficult cases, instrumentation and fusion after postural reduction may also be sufficient to achieve adequate sagittal alignment, since spinal alignment is maintained. Reduction and realignment procedures would appear mandatory in type 6 deformities where sagittal alignment is severely disturbed.
Acknowledgments
This research was assisted by support from the Spinal Deformity Study Group. This research was funded by an educational/research grant from Medtronic Sofamor Danek. The authors would like to acknowledge the other members of the Spondylolisthesis section of the Spinal Deformity Study Group: Eric Berthonnaud, PhD, Courtney Brown, MD, John Dimar, MD, Timothy Hresko, Serena Hu, Julie Joncas, RN, Stefan Parent, MD, Mark Weidenbaum, MD.
Conflict of interest None.
References
- 1.Mardjetko S, Albert T, Andersson G, Bridwell K, DeWald C, Gaines R, Geck M, Hammerberg K, Herkowitz H, Kwon B, Labelle H, Lubicky J, McAfee P, Ogilvie J, Shufflebarger H, Whitesides T (2005) Spine/SRS Spondylolisthesis Summary Statement. Spine, 30(6 Suppl):S3 [DOI] [PubMed]
- 2.Labelle H, Roussouly P, Berthonnaud E, et al. The importance of spinopelvic balance in L5-S1 developmental spondylolisthesis: a review of pertinent radiologic measurements. Spine. 2005;30(suppl):27–34. doi: 10.1097/01.brs.0000155560.92580.90. [DOI] [PubMed] [Google Scholar]
- 3.Wiltse LL, Newman PH, Macnab I. Classification of spondylolysis and spondylolisthesis. Clin Orthop. 1976;117:23–29. [PubMed] [Google Scholar]
- 4.Marchetti PC, Bartolozzi P (1997) Classification of spondylolisthesis as a guideline for treatment. In: Bridwell KH, DeWald RL, Hammerberg KW, et al., (eds) The textbook of spinal surgery, 2 edn. Lippincott-Raven, Philadelphia pp 1211–1254
- 5.Labelle H, Roussouly P, Berthonnaud E, Mac-Thiong JM, Hresko T, Dimar, J, Parent S, Weidenbaum M, Brown C, Hu S (2009) Spondylolisthesis classification based on spino-pelvic alignment, Podium presentation at the 2009 Scoliosis Research Society Annual Meeting, San Antonio, USA
- 6.Labelle H, Roussouly P, Berthonnaud E, Transfeldt E, O’Brien M, Hresko T, Chopin D, Dimnet J. Spondylolisthesis, pelvic incidence and sagittal spino-pelvic balance: a correlation study. Spine. 2004;29(18):2049–2054. doi: 10.1097/01.brs.0000138279.53439.cc. [DOI] [PubMed] [Google Scholar]
- 7.Roussouly P, Gollogly S, Berthonnaud E, Labelle H, Weidenbaum M. Sagittal alignment of the spine and pelvis in the presence of L5–S1 isthmic lysis and low-grade spondylolisthesis. Spine. 2006;31(20):2484–2490. doi: 10.1097/01.brs.0000239155.37261.69. [DOI] [PubMed] [Google Scholar]
- 8.Mac-Thiong JM, Roussouly P, Hresko MT, Labelle H (2010) The importance of sagittal spino-pelvic alignment in low grade spondylolisthesis. Identification of subgroups based on Pelvic Incidence and Sacral Slope, Podium presentation at the Scoliosis Research Society Annual Meeting, Kyoto, Japan, September 2010
- 9.Hresko MT, Labelle H, Roussouly P, Berthonnaud E. Classification of high grade spondylolisthesis based on pelvic version and spinal balance: possible rationale for reduction. Spine. 2007;32(20):2208–2213. doi: 10.1097/BRS.0b013e31814b2cee. [DOI] [PubMed] [Google Scholar]
- 10.Mac-Thiong JM, Labelle H, Wang Z, Guise JA. Postural model of sagittal spino-pelvic balance and its relevance for lumbosacral developmental spondylolisthesis. Spine. 2008;33(21):2316–2325. doi: 10.1097/BRS.0b013e318186b236. [DOI] [PubMed] [Google Scholar]
- 11.Mac-Thiong JM, Labelle H. A proposal for a surgical classification of pediatric lumbosacral spondylolisthesis based on current literature. Eur Spine J. 2006;15:1425–1435. doi: 10.1007/s00586-006-0101-4. [DOI] [PubMed] [Google Scholar]
- 12.Mac-Thiong JM, Labelle H, Parent S, Hresko MT, Deviren V, Weidenbaum M (2008) Reliability and development of a new classification of lumbosacral spondylolisthesis. Scoliosis 3:19 [DOI] [PMC free article] [PubMed]
- 13.Mac-Thiong JM, Duong L, Parent S, Hresko MT, Dimar J, Weidenbaum M, Labelle H. Reliability of the SDSG classification of lumbosacral spondylolisthesis, Submitted to Spine, April 2010 [DOI] [PubMed]
- 14.Labelle H, Roussouly P, Mac-Thiong JM, Parent S, Hresko MT (2010) Relationship between HRQL measures and spino-pelvic alignment in adolescent spondylolisthesis compared to a control population, Podium presentation at the Scoliosis Research Society Annual Meeting, Kyoto, Japan, September 2010
- 15.Labelle H, Roussouly P, Chopin D, Berthonnaud E, Hresko T, O’Brien M. Spino-pelvic alignment after surgical correction for developmental spondylolisthesis. Eur Spine J. 2008;17:1170–1176. doi: 10.1007/s00586-008-0713-y. [DOI] [PMC free article] [PubMed] [Google Scholar]