Abstract
Introduction
Aging of the spine is characterized by facet joints arthritis, degenerative disc disease and atrophy of extensor muscles resulting in a progressive kyphosis. Recent studies confirmed that patients with lumbar degenerative disease were characterized by an anterior sagittal imbalance, a loss of lumbar lordosis and an increase of pelvis tilt. The aim of this paper was thus to describe the different compensatory mechanisms which are observed in the spine, pelvis and/or lower limbs areas for patients with severe degenerative spine.
Methods
We reviewed all the compensatory mechanisms of sagittal unbalance described in the literature.
Results
According to the severity of the imbalance, we could identify three different stages: balanced, balanced with compensatory mechanisms and imbalanced. For the two last stages, the compensatory mechanisms permitted to limit consequences of lumbar kyphosis on the global sagittal alignment. Reduction of thoracic kyphosis, intervertebral hyperextension, retrolisthesis, pelvis backtilt, knee flessum and ankle extension were the main mechanisms described in the literature. The basic concept of these compensatory mechanisms was to extend adjacent segments of the kyphotic spine allowing for compensation of anterior translation of the axis of gravity.
Conclusions
To avoid underestimate the severity of the degenerative spine disorder, it thus seems important to recognize the different compensatory mechanisms from the upper part of the trunk to the lower limbs. We propose a three steps algorithm to analyse the balance status and determine the presence or not of these compensatory mechanisms: measurement of pelvis incidence, assessment of global sagittal alignment and analysis of compensatory mechanisms successively in the spine, pelvis and lower limbs areas.
Keywords: Sagittal balance, Pelvis, Spinal alignment, Lumbar lordosis, Degenerative disc disease, Lumbar kyphosis
Introduction
Recent studies support the concept that analysis of sagittal balance is an important step for optimizing the management of lumbar degenerative pathologies, especially when surgery with spinal fusion and instrumentation are intended [9, 15, 17, 26].
Aging of the spine is characterized by facet joints arthritis, degenerative disc disease and atrophy of extensor muscles resulting in a progressive kyphosis and sagittal balance disorder [7, 12, 26]. Similarly, patients with chronic low back pain and lumbar degenerative disease are characterized by an anterior sagittal imbalance, a loss of lumbar lordosis and an increase of pelvis tilt [1–3, 10]. The anterior imbalance is directly secondary to the loss of lumbar lordosis even if the part of structural loss of lordosis and the antalgic postural part are difficult to differentiate. Except the loss of lordosis and the anterior imbalance which are related to the degenerative process, other changes in spino-pelvic parameters (for example decrease of sacral slope, reduction of thoracic kyphosis or increase of lordosis in upper lumbar spine) correspond to compensatory mechanisms. To optimize the management of lumbar degenerative disorders and to avoid underestimating the severity of the disease, it seems important to recognize these different mechanisms.
Considering that in the normal population, correlations between the pelvic incidence (morphological parameter), the sacral slope and sagittal curves (especially lumbar lordosis) have been well documented [4–8, 13, 22, 24, 25], it is much easier now to understand the changes for patients with severe degenerative spine. The compensatory mechanisms permit to limit the consequences of lumbar kyphosis in terms of sagittal anterior imbalance and occur in the spine, pelvis and/or lower limb areas.
The objective of this paper is thus to describe these different compensatory mechanisms in patients with severe degenerative spine and sagittal balance disorders.
Global balance evaluation
In the normal population, a standard sagittal balance does not exist. The most important thing to have is optimal congruence between pelvic and spinal parameters to achieve an economic posture placing the axis of gravity in a physiologic position [4, 6, 16, 18, 20].
One of the most important step is to evaluate the global balance of the patient. This can be done optimally using force plate and measuring positioning of the gravity axis in the sagittal plane [25]. In clinical practice, however, global balance is appreciated more simply by describing the relative positioning of the spine in reference with the pelvis on standing full spine radiographs. Global sagittal alignment is typically determined by calculated the offset between the posterior corner of the sacrum and the vertical line passing through the mid-vertebral body of C7. Instead of measuring a linear distance, we advise to use angular and/or ratio parameters: spino-sacral angle and C7plumbline/sacro-femoral distance ratio (C7/SFD), respectively [1, 23].
The SSA was defined as the angle between the sacral plate and the line connecting the centroid of C7 vertebral body and the midpoint of the sacral plate (Fig. 1a). In the normal population, the mean value of this angle is 135° ± 8 [23].
Fig. 1.
Evaluation of global sagittal alignment using the spino-sacral angle (a) and the C7/SFD ratio (b). The SSA is defined as the angle between the sacral plate and the line connecting the centroid of C7 vertebral body and the midpoint of the sacral plate [23]. Sacro-femoral distance (SFD) is the horizontal distance between the vertical bi-coxo-femoral axis and the vertical line passing through the posterior corner of the sacrum. The horizontal distance between C7 PL and the posterior corner of the sacrum (that is SC7 D) was also measured. Then we calculated the C7/SFD ratio corresponding to the ratio between SC7 Distance and SF Distance [1]
The method to measure C7/SFD ratio is presented in Fig. 1b. This ratio is equal to zero, when C7 plumb line projects exactly on the posterior corner of the sacrum, and to one, when C7 plumb line projects exactly on the bicoxo-femoral axis. It is negative when C7 plumb line projects posteriorly to the sacrum and more than one when C7 plumb line projects from anterior to the femoral heads. In the normal population the value of this ratio is −0.9 ± 1 [1].
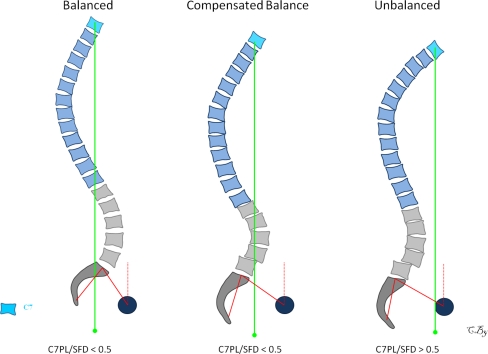
The spino-sacral angle and the C7/SFD ratio permit to evaluate the global sagittal alignment of the spine above the pelvis. According to the severity of the imbalance, we can identify three different stages: balanced, balanced with compensatory mechanisms and imbalanced (Fig. 2). The two last stages are characterized by the presence of compensatory mechanisms which are not enough efficient to maintain sagittal balance in the last stage.
Fig. 2.
Classification of global sagittal alignment in 3 stages with respect to the severity of the imbalance: stage 1 balanced, stage 2 balanced with compensatory mechanisms, stage 3 unbalanced (C7PL/SFD ratio superior to 0.5)
Compensatory mechanisms
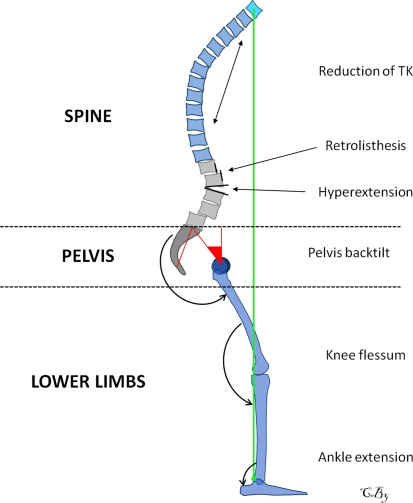
Compensatory mechanisms can occur in spine, pelvis and/or lower limb areas and are summarized and presented in Fig. 3. Although these mechanisms are not observed all together in the same patient, they are usually associated at different degree depending mainly on the stiffness of the spine, the musculature status and the severity of the imbalance.
Fig. 3.
Sagittal imbalance and the different compensatory mechanisms in the spine, pelvis and lower limbs areas
Their basic concept is to extend the adjacent segments of the kyphotic spine allowing for the compensation of anterior translation of the axis of gravity.
To understand the variations of positional parameters such as SS, PT, LL and TK (thoracic kyphosis) in the patients’ population, we previously published the values of six different classes of pelvic incidence in a normal control group of 154 subjects. Values of positional parameters for each class of PI (from I to VI corresponding to a progressively increase of the PI value) are summarized in Table 1. Otherwise, to analyze the segmental changes, we have to keep in mind that the L4-S1 segment provides the 2/3 of the total lumbar lordosis [8, 22].
Table 1.
Classes of pelvic incidence and corresponding values of spino-pelvic positional parameters from a group control of 154 subjects [2]
| n | PI | PT | SS | LL | TK | |
|---|---|---|---|---|---|---|
| I 28° < PI < 37.9° |
12 | 35.4 ± 1.3 (33.7–37.9) | 3.9 ± 4.5 (−1.5–13.3) | 31.5 ± 5.2 (21.2–38.5) | 53.3 ± 6.6 (41.2–62) | 43.8 ± 9.1 (22.5–51.5) |
| II 38° < PI < 47.9° |
44 | 42.7 ± 2.8 (37.9–47.6) | 8.9 ± 4.8 (−5.1–18.2) | 33.8 ± 4.8 (23.1–48.4) | 55.5 ± 8 (41.5–76.5) | 48 ± 8.8 (24–64.7) |
| III 48° < PI < 57.9° |
59 | 52.6 ± 2.8 (48.2–57.4) | 12.5 ± 5.6 (−1.2–23.2) | 40.1 ± 5.5 (28.2–52.9) | 61.5 ± 8.4 (43.1–81.9) | 47.4 ± 10.7 (24–70.3) |
| IV 58° < PI < 67.9° |
26 | 62.6 ± 2.8 (58.2–67.6) | 15.8 ± 4.3 (7.1–26.8) | 46.8 ± 4.2 (37.9–58.5) | 68.3 ± 5.1 (60.9–76.3) | 47.6 ± 7.8 (34.7–64.7) |
| V 68° < PI < 77.9° |
11 | 72.6 ± 2.8 (69.6–77.4) | 19.7 ± 5.5 (12.6–27.9) | 52.9 ± 5.2 (46.2–59.6) | 74.9 ± 6.8 (62.2–81.6) | 46 ± 10.2 (29.7–62) |
| VI 78° < PI < 87.9° |
2 | 81.4 ± 3.3 (79.1–81.4) | 21.9 ± 12.3 (13.2–30.6) | 59.5 ± 9 (53.1–65.9) | 76 ± 8.3 (70.1–81.9) | 44.6 ± 12.2 (36–53.3) |
Spine area
Reduction of thoracic kyphosis
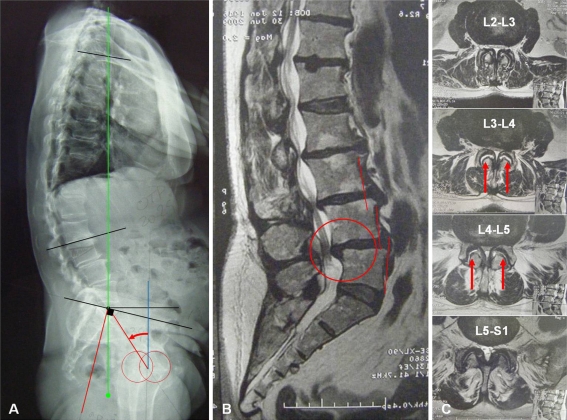
Reduction of thoracic kyphosis permits to limit anterior translation of the axis of gravity and can be observed in young patients with flexible spine (Fig. 4). In a previous work, we found that patients with degenerative disc disease and disc herniation were characterized by flat spine with significant reduction of both lumbar lordosis and thoracic kyphosis. This profile was more marked for patients with disc diseases below 45 years old [2]. Our findings were concordant with those reported by Rajnic et al. [21] through a similar study. When the spine is rigid (aging is kyphotic and ankylosis), there is no possibility for the patient to reduce the magnitude of the thoracic curve.
Fig. 4.
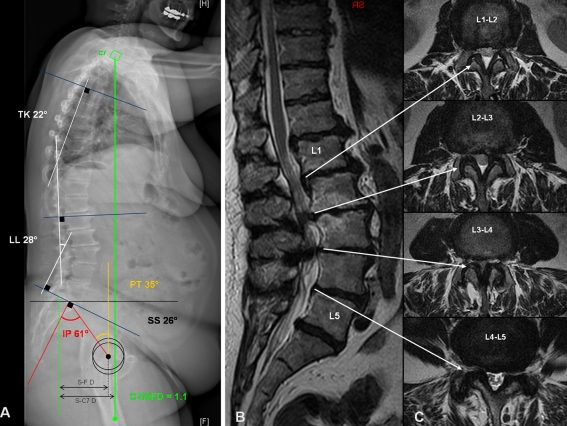
Patient with lumbar kyphosis and severe multilevel stenosis from L2–L3 to L4–L5: full spine radiographs (a), sagittal T2-weighted (b) and transverse T2-weighted (c) MRI sequences. The patient is still balanced (C7PL/SFD is 0.25), but balance is compensated by three main mechanisms: pelvis back tilt (curved arrow), multilevel retrolisthesis (red circles) and reduction of thoracic kyphosis (calculated to 25°). PI was measured to 47°, PT was 34° and SS was 13°. Compared to group control from normal and asymptomatic population, we should expect value of PT around 10°. On MRI axial slices, retrolisthesis at L3–L4 and L4–L5 are associated with fluid collection in facet joints (straight arrows)
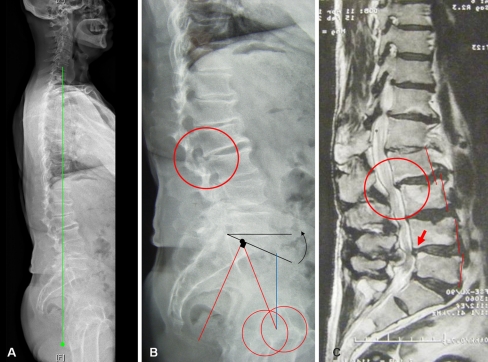
Hyperextension of adjacent segments
Hyperextension of adjacent segments is a very common compensatory mechanism to limit the consequences of lumbar kyphosis on axis gravity shift (Fig. 5). Previous studies demonstrated that low back pain subjects were characterized by less distal lordosis, a more vertical sacrum and more proximal lumbar lordosis [10, 14]. More proximal lumbar lordosis signified more extension in the upper lumbar spine. Hyperextension can be global (multi-segmental) or local (mono/bi-segmental). Local hyperextension is efficient to place posteriorly the upper spine, however, this generates increase of stresses on posterior structures (Fig. 5), exposes to the risk of retrolisthesis and may result in accelerated facet joints arthritis, inter-spinous hyperpressure (Baastrup’s disease) and sometimes isthmic lysis.
Fig. 5.
Patient with lumbar stenosis from L2–L3 to L4–L5 and thoraco-lumbar kyphosis: full spine radiographs (a), X-rays focused on lumbo-pelvic zone (b) and sagittal T2-weighted MRI sequence (c). The patient is well-balanced (C7PL/SFD is −0.3) however, some compensatory mechanisms are present in the lumbar area. Hyperextension is observed at L5–S1 (curvedblack arrow) (local lordosis was measured to 24°) and there are multilevel retrolisthesis at L2–L3 (red circles) and L4–L5 (large arrow). The pelvis tilt was quite normal as it was calculated to 22° and the PI to 46°
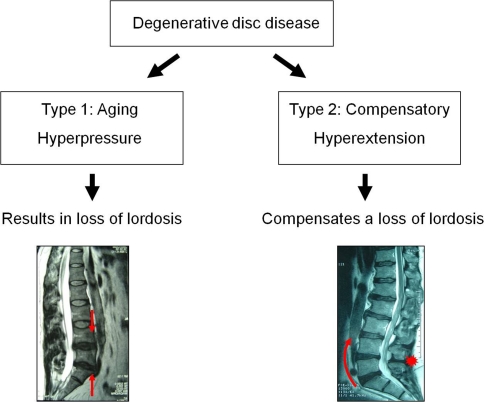
From a biomechanical point of view, we assume that compensatory discopathy has to be differentiated from classical aging discopathy (Fig. 6). Compensatory discopathy is characterized by hyperextension compensating a loss of lordosis whereas aging discopathy (the most frequent type) is characterized by disc narrowing with parallel endplates resulting in loss of lordosis.
Fig. 6.
Classification of degenerative disc diseases into aging discopathy and compensatory discopathy
Retrolisthesis
Retrolisthesis is typically limited to 2–3 mm slippage in the lumbar spine and result in severe foraminal stenosis and more rarely in central stenosis (Figs. 4, 5). They are observed at lower or upper adjacent segments of the kyphotic degenerative disease: L5-S1 is a common site. Retrolisthesis is typically underestimated on lying down radiological imaging techniques (MRI and CT scan). They can be suspected on MRI imaging with the presence of loss of coaptation of facet joints with fluid collection and frequent synovial facet cysts (Fig. 4).
Pelvis area
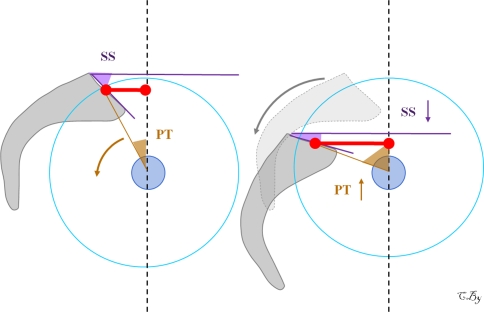
The only compensatory mechanism in the pelvis area is pelvis back tilt (also called pelvis retroversion) defined by the increase of the pelvis tilt and corresponds to posterior rotation of the pelvis around the femoral heads similarly than during hip extension (Fig. 7). This motion is permitted by hypolordotic spine stiffness transmitted to the pelvis and results in posterior placement of sacrum related to the coxo-femoral heads. Bringing back the sacral plate related to the coxo-femoral heads and increasing the sacro-femoral distance, this mechanism permits the compensation of anterior translation of the axis of gravity. The pelvis incidence determines the global capacity of pelvis retroversion, which is easily achieved for patients characterized by a great pelvic incidence. Considering that PI = SS + PT and that SS cannot be a negative number in standing position, the pelvis can tilt more with a high PI than a low PI, since there is a much wider range through which adaptation can occur. Numerous studies reported that patients with chronic low back pain and lumbar degenerative disease were characterized by decrease of sacral slope and increase of pelvis tilt [2, 3, 10, 11, 14] as demonstrated in our illustrated case in Figs. 4 and 8.
Fig. 7.
Pelvis back tilt mechanism. Increase of pelvis tilt results in posterior placement of sacrum related to the coxo-femoral heads thus increasing the sacro-femoral distance (red lines)
Fig. 8.
Patient with multilevel lumbar stenosis from L1–L2 to L4–L5: full spine radiographs (a), sagittal T2-weighted MRI sequence (b) and axial T2-weighted MRI sequences from L1–L2 to L4–L5 (c). The patient is clearly unbalanced (SC7D/SFD is more than 1) with C7 plumbline in front of femoral heads. The sagittal unbalance is because of the lumbar kyphosis, which is secondary to the severe degenerative disc diseases from T12 to S1. Seeing that PI is measured to 61° and compared to group control, we should expect value of LL around 70° (only measured to 28° on full spine radiographs). To limit sagittal unbalance, this patient undergoes pelvis retroversion (increase of PT which is calculated to more than 30°), reduction of thoracic kyphosis (only 22°) and knee flessum
Lower limbs area
Knee flexion
Knee flexion can be evaluated by the pelvi-femoral angle described by Mangione et al. [19]. This is a well-known compensatory mechanism for patients with severe degenerative spine and has already been widely reported [12, 26].
Ankle extension
Through a prospective study, Lafage et al. [16] recently underlined that the pelvis translation was a parameter as important as the pelvis rotation (measured by the pelvis tilt) and probably induced by extension in ankle joint. They suggested that our patients should be analyzed from head to feet.
Finally, we propose three main steps to achieve analysis of sagittal balance and to determine the presence or not of compensatory mechanisms perfectly demonstrated in Fig 8.
What is the value of the pelvis incidence? The knowledge of the pelvis incidence permits to determine the expected theoretical values for spino-pelvic positional parameters (Table 1).
Is the patient balanced? Global sagittal alignment is evaluated by analysing the positioning of C7 using measurement of SSA and C7PL/SFD ratio.
- Are there compensatory mechanisms?
- Analysis of the spine zone consists of measurement of lumbar lordosis and thoracic kyphosis and looking for the presence of compensatory discopathy(ies) and retrolisthesis.
- Analysis of the pelvic parameters: is the pelvis tilt adequate with respect to the pelvis incidence? The presence of horizontal sacral plate is highly suspected of pelvis back tilt mechanism.
- In lower limbs area: are the knee flexed? One must care to this point considering that knee flessum minimizes the importance of sagittal imbalance on full spine radiographs.
Conclusion
Meticulous analysis of spino-pelvic parameters allows for the identification of the main compensatory mechanisms observed in patients with sagittal balance disorders. These mechanisms have to be considered prior to therapeutic options. This may probably optimize the management of patients with severe degenerative spine especially when surgical treatment is planned.
Conflict of interest
No funds were received in support of this study.
Abbreviations
- LL
Lumbar lordosis
- PI
Pelvic incidence
- PT
Pelvic tilt
- SS
Sacral slope
- TK
Thoracic kyphosis
References
- 1.Barrey C (2004) Equilibre sagittal pelvi-rachidien et pathologies lombaires dégénératives. Etude comparative à propos de 100 cas (in French). Thèse de Médecine. Université Claude Bernard, Lyon
- 2.Barrey C, Jund J, Noseda O, Roussouly P. Sagittal balance of the pelvis–spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur Spine J. 2007;16:1459–1467. doi: 10.1007/s00586-006-0294-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barrey C, Jund J, Perrin G, Roussouly P. Spinopelvic alignment of patients with degenerative spondylolisthesis. Neurosurg. 2007;61:981–986. doi: 10.1227/01.neu.0000303194.02921.30. [DOI] [PubMed] [Google Scholar]
- 4.Berthonnaud E, Dimnet J, Roussouly P, Labelle H. Analysis of the sagittal spine and pelvis using shape and orientation parameters. J Spinal Disord Tech. 2005;18:40–47. doi: 10.1097/01.bsd.0000117542.88865.77. [DOI] [PubMed] [Google Scholar]
- 5.During J, Goudfrooij H, Keessen W, Beeker TW, Crowe A. Towards standards for posture. Postural characteristics of the lower back system in normal and pathologic conditions. Spine. 1985;10:83–87. doi: 10.1097/00007632-198501000-00013. [DOI] [PubMed] [Google Scholar]
- 6.Duval-Beaupère G, Legaye J. Composante sagittale de la statique rachidienne (in French) Rev Rhum. 2004;71:105–119. doi: 10.1016/j.rhum.2003.09.018. [DOI] [Google Scholar]
- 7.Gelb DE, Lenke LG, Bridwell KH, Blanke K, MacEnery KW. An analysis of sagittal spinal aligment in 100 asymptomatic middle and older aged volunteers. Spine. 1995;20:1351–1358. [PubMed] [Google Scholar]
- 8.Guigui P, Levassor N, Rillardon L, Wodecki P, Cardinne L. Valeur physiologique des paramètres pelviens et rachidiens de l’équilibre sagittal du rachis. Analyse d’une série de 250 volontaires (in French) Rev Chir Orthop. 2003;89:496–506. [PubMed] [Google Scholar]
- 9.Izumi Y, Kumano K. Analysis of sagittal lumbar alignment before and after posterior instrumentation: risk factor for adjacent unfused segment. Eur J Orthop Surg Traum. 2001;1:9–13. doi: 10.1007/BF01706654. [DOI] [Google Scholar]
- 10.Jackson RP, MacManus AC. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex and size. Spine. 1994;19:1611–1618. doi: 10.1097/00007632-199407001-00010. [DOI] [PubMed] [Google Scholar]
- 11.Jackson RP, Kanemura T, Kawakami N, Hales C. Lumbopelvic lordosis and pelvic balance on repeated standing lateral radiographs of adult volunteers and untreated patients with constant low back pain. Spine. 2000;25:575–586. doi: 10.1097/00007632-200003010-00008. [DOI] [PubMed] [Google Scholar]
- 12.Kobayashi T, Atsuta Y, Matsuno T, Takeda N. A longitudinal study of congruent sagittal spinal alignment in an adult cohort. Spine. 2004;29:671–676. doi: 10.1097/01.BRS.0000115127.51758.A2. [DOI] [PubMed] [Google Scholar]
- 13.Korovessis PG, Stamatakis MV, Baikousis AG. Reciprocal angulation of vertebral bodies in the sagittal plane in a asymptomatic Greek population. Spine. 1998;23:700–704. doi: 10.1097/00007632-199803150-00010. [DOI] [PubMed] [Google Scholar]
- 14.Korovessis PG, Dimas A, Iliopoulos P, Lambiris E. Correlative analysis of lateral vertebral radiographic variables and medical outcomes study short-form health survey: a comparative study in asymptomatic volunteers versus patients with low back pain. J Spinal Disord Tech. 2002;15:384–390. doi: 10.1097/00024720-200210000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Kumar MN, Baklanov A, Chopin D. Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur Spine J. 2001;10:314–319. doi: 10.1007/s005860000239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lafage V, Schwab F, Skalli W, Hawkinson N, Gagey PM, Ondra S, Farcy JP. Standing balance and sagittal plane spinal deformity: analysis of spinopelvic and gravity line parameters. Spine. 2008;33:1572–1578. doi: 10.1097/BRS.0b013e31817886a2. [DOI] [PubMed] [Google Scholar]
- 17.Lazennec JY, Ramare S, Arafati N, Laudet CG, Gorin M, Roger B, Hansen S, Saillant G, Maurs L, Trabelsi R. Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Eur Spine J. 2000;9:47–55. doi: 10.1007/s005860050008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Legaye J, Duval-Beaupère G, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7:99–103. doi: 10.1007/s005860050038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mangione P, Senegas J. L’équilibre rachidien dans le plan sagittal (in French) Rev Chir Orthop. 1997;83:22–32. [PubMed] [Google Scholar]
- 20.Marnay T (1988) Equilibre du rachis et du bassin. Cahiers d’enseignement de la SOFCOT. Elsevier, Paris, pp 281–313
- 21.Rajnics P, Templier A, Skalli W, Lavaste F, Illes T. The importance of spinopelvic parameters in patients with lumbar disc lesions. Int Orthop. 2002;26:104–108. doi: 10.1007/s00264-001-0317-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roussouly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine. 2005;30:346–353. doi: 10.1097/01.brs.0000152379.54463.65. [DOI] [PubMed] [Google Scholar]
- 23.Roussouly P, Gollogly S, Noseda O, Berthonnaud E, Dimnet J. The vertical projection of the sum of the ground reactive forces of a standing patient is not the same as the C7 plumbline: a radiographic study of the sagittal alignment of 153 asymptomatic volunteers. Spine. 2006;31:E320–E325. doi: 10.1097/01.brs.0000218263.58642.ff. [DOI] [PubMed] [Google Scholar]
- 24.Stagnara P, Mauroy JC, Dran G, Gonon G, Costanzo G, Dimnet J, Pasquet A. Reciprocal angulation of vertebral bodies in a sagittal plane: approach to references for the evaluation of kyphosis and lordosis. Spine. 1982;7:335–342. doi: 10.1097/00007632-198207000-00003. [DOI] [PubMed] [Google Scholar]
- 25.Vaz G, Roussouly P, Berthonnaud E, Dimnet J. Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J. 2002;11:80–87. doi: 10.1007/s005860000224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vital JM, Gille O, Gangnet N. Equilibre sagittal et applications cliniques (in French) Rev Rhum. 2004;71:120–128. doi: 10.1016/j.rhum.2003.09.020. [DOI] [Google Scholar]